![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
48 Cards in this Set
- Front
- Back
|
What is plasminogen? |
is a circulating protein with a high affinity for fibrin of a developing clot |
|
|
What is APC and where is it located? |
1. Activated Protein C 2. It is on platelets |
|
|
What does APC do? (3) |
Turns off the following: 1. Pro-coagulation factors V and VIII 2. Stimulate release of tPA and scu-PA, which binds to the clot 3. Inhibits plasminogen activator inhibitor (PAL-1) |
|
|
What is the function plasminogen activators (tPA) |
convert plasminogen to active plasmin |
|
|
T/F tPA is an endogenous single-chain urokinase |
False it is an endogenous tissue plasminogen activator |
|
|
T/F scu-PA is an endogenous single-chain urokinase |
True |
|
|
Streptokinase: _______ beta-hemolytic streptococci |
Exogenous |
|
|
Plasmin degrades ______ |
Fibrin |
|
|
What 2 components activate plasmin? |
1. tPA 2. scu-PA |
|
|
PAI-1 does what? |
Inhbits clot bound plasmin |
|
|
What is α2-antiplasmin and what does it do? |
1. α2-antiplasmin is a circulating protease inhibitor 2. It inhibits plasmin that has been released from clots |
|
|
What are 3 inhibitors of eicosanoids synthesis? |
1. Aspirin 2. NSAIDS 3. Glucocorticoids |
|
|
What specifically does aspirin and NSAIDs inhibit? |
Inhibit thromboxane and prostaglandin synthesis |
|
|
What do glucocorticoids specifically inhibit? |
cortisol, hyrodocortisol inhibit all eicosanoid synthesis |
|
|
What are the 2 nonspecific Thrombin inhibitors? |
1. Antithrombin III (ATIII) activators 2. Vitamin K antagonists |
|
|
What are 2 examples of ATIII activators |
•Heparin (soluble & used as an injectable drug) & Heparin sulfate (membrane bound) |
|
|
What is a specific vitamin K antagonist? |
Warfarin |
|
|
How does warfarin work? |
decrease activity of coagulation proteins (II,VII,IX,X) by inhibiting their activation in the liver by g-carboxylation |
|
|
What are 2 specific thrombin (II) inhibitor |
1. Fondaparinus 2. Bivalirudin |
|
|
How does Fondaparinus work? |
inactivates Factor Xa, thus Factor II activation |
|
|
How does Bivalirudin work? |
–reversibly binds to Factor II (thrombin) |
|
|
Describe the specific MOA of Aspirin and NSAIDs |
•inhibit the cyclo-oxygenase that converts arachidonic acid to prostaglandin H2, a precursor to thromboxanes and other signal molecules involved in fibroblast recruitment |
|
|
Describe the specific MOA of glucocorticoids (hydrocortisol) |
•Inhibit the release of arachidonic acid from its storage site on plasma membrane phospholipids |
|
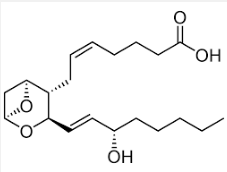
What is this structure? |
Thromboxane |
|
|
What are heparins? |
–Glycosaminoglycans (repeating disaccharides, GAGs) of varying molecular wt |
|
|
Heparin can induce ______ and _______ |
1. Clotting 2. Thrombocytopenia |
|
|
Heparins bind to and activate what? |
Antithrombin III (ATIII) |
|
|
What is the function of ATIII (2) |
1. Inactivates thrombin 2. ATIII inactivates Factors VIIIa, IXa, Xa and Xla |
|
|
T/F Heparin treatment can induce excessive clotting and thrombocytopenia in patients that develop antibodies to the platelets |
True |
|
|
Heparin binds to ______ changing its conformation |
platelet factor 4 (PF4) |
|
|
_____ recognize the heparin-PF4 complex as foreign material and binds to the ______ |
1. IGgs 2. Platelet |
|
|
_____ activates the platelet increasing _____ |
1. IGg 2. thrombosis |
|
|
IGg tagged platelets are removed by the _______ producing _______ |
1. spleen 2. thrombocytopenia |
|
|
Warfarin is structurally similar to _____ |
Vitamin K |
|
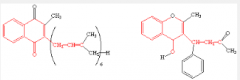
Which is vitamin k and which is warfarin? |
Left is vitamin K Right is warfarin (3 rings) |
|
|
What is the specific MOA of warfarin? |
•Acts as a competitive inhibitor to Vit K epoxide reductase blocking the reduction of Vit K epoxide (KO) to active reduced Vit K (KH2) |
|
|
Reduced vitamin K is required for what? |
•is required for the formation of g-carboxylated glutamate residues in all of the Vit K dependent coagulation factors II (thrombin), VII, IX and X |
|
|
What is needed to bind to calcium and what does this binding do? |
•gamma-carboxylated glutamate residues are needed to bind calcium (Ca) which links the coagulation factors to the negatively charged phospholipids (PL) in the platelet membrane |
|
|
Warfarin also blocks activity of _______ activity of proteins ____ and _____ |
1. antithrombogenic 2. S 3. C |
|
|
what is an indirect inhibitor of thrombin? |
Fondaparinus |
|
|
Heparin and warfarin lack what? |
specificity |
|
|
T/F Fundaparinus is a disaccharide |
False it is a pentasaccharide |
|
|
Fundaparinus is a specific inhibitor of ______ |
Factor Xa |
|
|
T/F Fondaparinus enhances the binding of ATIII to Factor Xa by 300 fold, thus preventing Factor Xa activation of thrombin |
True |
|

What is this drug? |
Fondaparinus (pentasaccharide, 5 rings) |
|
|
Bivalirudin was developed based on what? |
•Bivalirudin, 20 aa peptide, was developed based on hirudin which is secreted by leeches. |
|
|
What is the advantage of bivalirudin over hirudin? |
High binding affinity and specificity for thrombin yet the binding is reversible, whereas, hirudinbinds irreversibly |
|
|
T/F Hirudin is safer to use than bivalirubin in that the anticlotting activity of hirudin is more easily controlled |
False Bivalirubin is safer to use than hirudin in that the anticlotting activity of bivalirubin is more easily controlled |

