![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
78 Cards in this Set
- Front
- Back
|
What organ does Epinephrine and glucagon work on? What are their roles?
|
Epi works on muscle and liver for quick energy.
Glucagon works on muscle for maintaining blood glucose levels when you're fasting. |
|
|
What are two common problems associated with too much glucose as seen in uncontrolled diabetes? (1 related to kidney 1 related to tissues)
|
Glucose is excreted and causes weight loss. Too much also causes non-enzymatic glycation rxns that increase HbA1C and other tissues that cause problems
|
|
|
Despite having its own nucleus and energy-generating machinery, why is brain tissue so dependent on glucose? (What is the exception?)
|
Bc it's the only substrate that it uses to get energy (with the exception of ketone bodies if it has enough time to adapt)
|
|
|
Why is the renal medulla so dependent on glucose?
|
Bc it has few mitochondria.
|
|
|
Why are RBCs so dependent on glucose?
|
Bc it does not have any nucleus or mitochondria for alternative energy sources - glucose is the only one it uses.
|
|
|
What are the three tissues most dependent on plasma glucose?
|
Brain, RBCs, renal medulla
|
|
|
Beware of the GLUT transporters. How many are there and do they require energy? In what direction does glucose flow through them?
|
There are 5 and they do not require energy. They simply travel down the concentration gradient.
|
|
|
What is the Km for GLUT1/3, 2 and 4?
|
GLUT1/3 = 1mM
GLUT 2 = 15-20mM GLUT 4 = 5mM |
|
|
Where are the following found:
1. GLUT1/3 2. GLUT2 3. GLUT4 5. GLUT5 |
1. RBC's, brain
2. Liver, pancreatic B-cells, basolateral side of intestinal cells 3. Adipose and skeletal tissue 4. Enterocites |
|
|
Don't forget to review your GLUT proteins summary
|
Don't forget to review your GLUT proteins summary
|
|
|
What does hexokinase do? Which C does it work on?
|
It phosphorylates glucose - this prevents it from passing back through the GLUT transporters. It phosphorylates glucose carbon 6
|
|
|
Interesting fact: Plasma glucose concentration is about 5mM and as it diffuses into cell, it encounters hexokinase with a Km of about 0.1mM. What does that mean, really? Can it be inhibited?
|
That nearly all glucose molecules that enter the cell are going to be trapped by the phospohorylation mechanism of hexokinase. This enzyme is inhibited by feed back inhibition.
|
|
|
What is the liver equivalent to hexokinase? Is its Km higher or lower? Why?
|
Glucokinase has a much higher Km. Higher bc the liver's job is to maintain glucose levels at fasting times. If the Km was low, then it would absorb/trap glucose-6-phosphate during fasts and that would be counter productive. Thus, the liver traps glucose only when it is in abundance.
|
|
|
In glycogen, glucose units are linked by __a__ bonds with interspersed __b__ branch points.
|
a. alpha 1,4 glycosidic bonds
b. alpha 1,6 branch points. |
|
|
In terms of osmotic potential, what is the advantage to storing glucose as glycogen?
|
A typical glycogen molecule contains up to 500K glucose monomers and equivalent to only one molecule. This means a difference between 0.01 uM glycogen and 400 mM free glucose.
|
|
|
Remember osmotic pressure concepts. I.e. if you have a high concentration of solute on one side of a membrane, you'd have high osmotic pressure and water would rush in.
|
This is important bc if a liver cell did not store glucose as glycogen, its cells would have a very high osmotic pressure and the cells would explode.
|
|
|
What kind of cleavage does glycogen phosphorylase put glycogen through? What bond does it break? What monomer does it make?
|
Phosphorolytic cleavage of the alpha 1,4 bond. It makes a monomer of Glucose 1-phosphate.
|
|
|
What is odd about the co-factor for glycogen phosphorylase?
|
It uses PLP (pyridoxyl phosphate) - an odd thing (see pg 79 and 9/19 8:15 lecture 50:00 and less. He said we don't need to know but if you care...
|
|
|
What role does phosphoglucomustase play?
|
Since phosphorylization of glycogen yields, G-1-P monomers, something has to covert it to the metabolically relevant G-6-P...that's what this enzyme does. see pg 80
|
|
|
Review how hepatocytes convert glycogen to glucose and release it into the plasma.
|
Glucose conversion in Hepatocyte:
1. In CYTOSOL, Glycogen phosphorylase converts glycogen to G-1-P. 2. In CYTOSOL Phosphoglucomutase converts G-1-P to G-6-P 3. G-6-P is transported from cytosol to ER lumen 4. In ER LUMEN, glucose-6-phosphatase converts G-6-P to Glucose (enzyme is on lumenal surface of ER) 5. Glucose is transported from ER LUMEN to CYTOSOL via GLUT2 6. Glucose is transported from CYTOSOL to plasma via GLUT2 |
|
|
What does debranching enzyme do? What does it yield and how does that product differ from glycogen phosophorylase?
|
Remember: Glycogen phosphorylase is hindered by branches. Debranching enzyme takes care of the remaining 4 or so residues by first moving 3 to a linear end and converting the remaining branched residue directly to G-6-P (vs G-1-P.) See pg 81
|
|
|
Review the role of UDP-Glucose Pyrolphosphorylase starting on pg 81. General pathway on back
|
1. G-6-P is converted to G-1-P with our friend Phosphoglucomutase.
2. UTP is added to G-1-P via UDP-glucose pyrophosphorylase to make an "activated" glucose or UDP-glucose (PPi is instantly degraded by pyrophosphatase to drive rxn to the right) 3. Glycogen synthase takes this UDP-glucose and adds it to the non-reducing termini of glycogen, forming alpha(1-4) linkages only and adds them to chains that are already at least 4 glucose units long. 4.After glucose is added to chain and UDP is released, UDP is converted back to UTP via Nucleoside diphosphate kinase. |
|
|
Re Glycogenin:
1. Where does it add first glucose unit (and in what form is the glucose)? 2. What catalyzes this rxn? 3. How many units are added? 4. Once those are added, what enzyme takes over? |
1. Glycogenin adds a UDP-glucose to a tyrosine residue
2. This rxn is catalyzed by subunits of glycogenin itself 3. About 8 s.u. are added before... 4. Glycogen synthase takes over. |
|
|
What does branching enzyme do? (p83)
|
When a chain becomes at least 11 glucose residues long, branching enzyme transfers 7 unites to a 6 position on a nearby chain. (see p83)
|
|
|
Epinephrine, glucagon, AMP (muscle), Ca2+ are factors that increase or decrease glycogen breakdown?
|
Increase p.83
|
|
|
Insulin, ATP, G-6-P, glucose are factors the increase or decrease glycogen breakdown?
|
Decrease p.83
|
|
|
Of these enzymes, which promote phosphorylation and which promote dephosphorylation?
1. Epinephrine 2. Glucagon 3. Insulin |
1. Phosphorylation
2. Phosphorylation 3. Dephosphorylation |
|
|
Review 9/19 8:15 1:12:00 -ish, p 84 re glycogen phosphorylase activity
|
Review 9/19 8:15 1:12:00 -ish, p 84 re glycogen phosphorylase activity
|
|
|
What is a synonym for Protein Kinase A?
|
cAMP-dept Protein Kinase
|
|
|
In aerobic glycolysis, glucose is metabolized to ?
Anaerobic? |
1. Aerobic = Pyruvate
2. Anaerobic = Lactate |
|
|
How many ATPs does glycolysis yield? Although this is small, what make glycolysis an extremely useful pathway?
|
2 ATP - Useful bc it can run anaerobically and very quickly.
|
|
|
What is the irreversible step in glycolysis?
|
F-6P to F-1,6-BP via Phosphofructokinase (p 94)
|
|
|
Beware that PFK-1 exhibits sigmoidal kinetics and has different activity depending on the level of ATP in the cell. Review p 94
|
Beware that PFK-1 exhibits sigmoidal kinetics and has different activity depending on the level of ATP in the cell. Review p 94
|
|
|
Citrate, ATP, and Protons act as inhibitors of PFK-1. AMP, ADP, and inorganic P act as activators of PFK-1. Why would citrate act as an inhibitor when it is a central component of the TCA cycle that proceeds glycolysis?
|
If TCA is rolling, there's lots of energy and glycolysis isn't necessary. Citrate is a component of this cycle and induces glycolysis to slow down.
|
|
|
What is a more sensitive energy marker of a cell? ATP or AMP?
|
AMP
|
|
|
Draw the PFK activity vs F6P concentration curve when 1) no inhibitor 2) 1mM ATP + 0.1mM AMP and 3) 1 mM ATP
(There's a figure on the back that you're trying to match) |
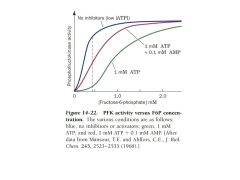
Note that each has a sigmoidal shape (subtle as some may be)
|
|
|
Review slide 14 of the 6_Glycolysis and... ppt showing how/why F1,6BP is regulated according to ATP, AMP, ADP, etc. Gluconeogenesis with F1,6BP is an energy requiring step so it doesn't make sense to do that if energy is low (it AMP is high)
|
Review slide 14 of the 6_Glycolysis and... ppt showing how/why F1,6BP is regulated according to ATP, AMP, ADP, etc. Gluconeogenesis with F1,6BP is an energy requiring step so it doesn't make sense to do that if energy is low (it AMP is high)
|
|
|
Under fasting conditions:
1. Glucagon is high or low? 2. F2,6BP is activated or inactivated? 3. Is liver glycolysis up or down? 4. Is liver gluconeogenesis up or down? |
1. Glucagon is high
2. F2,6BP is low (bc making F1,6BP would commit to glycolysis, which is not what you need right now) 3. Liver glycolysis is down bc it needs to pump glucose into the blood, not break it down) 4. Liver gluconeogenesis is up (via glucogen break down) to increase blood glucose level in blood. |
|
|
After meal:
1. Glucagon is high or low? 2. F2,6BP is activated or inactivated? 3. Is liver glycolysis up or down? 4. Is liver gluconeogenesis up or down reg'd? |
1. Glucagon is down, Insulin is up.
2. F2,6BP is up to break down glucose (too much in blood after meal) 3. Liver glycolysis is up to help remove glucose from blood 4. Liver gluconeogensis down bc not needed. |
|
|
He wants us to know/understand that the oxidative step from GAP to 1,3BPG is an important step that stores energy in NADH and in the high energy phosphate bond of 1,3-BPG
(see p97, 9/20 lecture, 8:15a, 1:10-ish) |
He wants us to know/understand that the oxidative step from GAP to 1,3BPG is an important step that stores energy in NADH and in the high energy phosphate bond of 1,3-BPG
(see p97, 9/20 lecture, 8:15a, 1:10-ish) |
|
|
How is arsenic bad for you, metabolically speaking?
|
It forms arsenate, a high energy compound similar to Phosphate. However, instead of releasing its energy to other metabolic rxns, it spontaneously hydrolyzes and falls apart.
|
|
|
The last enzyme in glycolysis, Pyruvate Kinase, is subject to feedforward activation by what molecule? What does this allow in terms of regulating glycolysis?
|
Pyruvate is subjected to feedforward activation by F1,6BP. This allows for coupled regulation of the two irreversible steps of glycolysis: PFK-1 and pyruvate kinase.
|
|
|
Review p 100 9/20 8:15 at about 1:25 re how a RBC deals with the accumulation of NADH made during glycolysis. In other cells, NADH is sent to mitochondria where it can be sent through electron transport chain. RBC do not have this mechanism and is instead reacted with an alcohol.
|
Review p 100 9/20 8:15 at about 1:25 re how a RBC deals with the accumulation of NADH made during glycolysis. In other cells, NADH is sent to mitochondria where it can be sent through electron transport chain. RBC do not have this mechanism and is instead reacted with an alcohol.
|
|
|
As you should know, oxidation (i.e. burning) is how energy is released. It must always be coupled to a reduction reaction. How can these steps be easily identified in a pathway?
|
Whenever you see something like NAD+ being REDUCED to NADH
|
|
|
See 9/21 8:15a at about 18:00 where he wants us to know Lactose Intolerance features (p 102)
|
See 9/21 8:15a at about 18:00 where he wants us to know Lactose Intolerance features (p 102)
|
|
|
In liver, insulin stimulates phospho- or dephosphorylation?
What about glucagon? |
Dephosphorylation. Glucagon stimulates phosphorylation.
|
|
|
Attempt to understand what's happening on pt 103. In lecture, it's at about 23:00 on 9/21, 8:15a
|
Attempt to understand what's happening on pt 103. In lecture, it's at about 23:00 on 9/21, 8:15a
|
|
|
Nearly all glycolysis pathway enzyme diseases are either lethal or affect these cells? Why?
|
RBCs. Bc RBCs do not have a nucleus to compensate for defective enzymes - they also live only on glycolysis and if screwed up, they die.
|
|
|
The pentose phosphate pathway is the main source of...?
|
NADPH and Ribose-5-phosphate (for nucleotide synthesis - especially important for growing tissues).
|
|
|
The pentose pathway makes this tri-peptide that is the key component that combats oxidative stress. What is odd about its structure? What part of it does all of the work to combat the oxidative stress in cells?
|
Glutathione Reductase - the Glu residue to connected to Cys via Glu's side chain vs standard a-chain connection (Gly is the 3rd residue). It's a very stable structure. The Sulfhydryl group does all of the work.
|
|
|
Note that, two molecules of GSH combine when being oxidized (and therefore reducing) by an oxidative radical. How is the GSSG product regenerated to GSH then?
|
Is regenerated by NADPH:
GSSG + NADPH --> 2 GSH + NADP+ (mediated by glutathione reductase) |
|
|
How many NADPH does the oxidative step of the pentose phosphate pathway produce? How many CO2?
|
2 NADPHs and 1 COs (you start out with a 6-C molecule and end up with 5-C).
|
|
|
What is the commitment step of the Pentose Phosphate pathway?
|
Glucose-6-phosphate dehydrogenase.
|
|
|
He said it's worth memorizing the oxidative branch of the pentose pathway. So, what are the four molecules involved starting with Glucose-6-Phosphate? What are three enzymes involved at each step and what is left behind at each step? (see p114, 8:15a lecture at 1:14 and earlier)
|
Molecules
1. G-6-P 2. 6-Phosphoglucono-lactone 3. 6-Phosphogluconate 4. Ribulose-5-Phosphate Enzymes 1/2. Glucose-6-phosphate dehydrogenase. Converts NADP+ to NADPH 2/3. Lactonase. Consumes water 3/4. 6-phosophogluconate dehydrogenase. Produces NADPH and CO2 |
|
|
So, the pentose phosphate pathway makes a 5-carbon sugar - ribulose-5-phosphate - that can be used to make amino acids and nucleotides. But to convert it back to something useful if that's not needed, the 5-C sugar needs to be converted back to a 6-sugar. What two enzymes in the pentose pathway accomplish this? (See p 114 and 9/21 8:15 at 1:16)
|
Transketolase and transaldolase.
|
|
|
How is the pentose phosphate regulated?
|
It is regulated NOT by an allosteric enzyme but by substrate availability of NADP+ and competitive inhibition by the NADPH product (see p115)
|
|
|
What does transketolase do in terms of movement of carbons?
|
It transfers a 2-C piece from one sugar to another - usually this results in a 5-C that is useless to a 6-C sugar that can be shuttled through one of the glycolysis pathways.
|
|
|
How does Transaldolase work in terms of moving carbons around?
|
It transfers a 3-carbon piece between a ketose donor and an aldose acceptor. It DOES NOT require a cofactor like transketolase does (see pg 118)
|
|
|
Overall, what is the purpose of the pentose pathway - i.e. what does it make that's necessary for the cell?
|
It makes NADPH to deal with oxidative stress and it makes ribulose-5-phosphate for nucleotide synthesis.
|
|
|
What tissue is most reliant on the pentose pathway?
|
RBC - it is the most oxidatively stressed tissue in the body and it relies on the NADPH made by this pathway to replenish all of the GSH RBCs use to combat oxidative stress.
|
|
|
Note that in the pentose pathway, x ribulose-5-P is converted to y G-6-P.
|
x = 6
y = 5 |
|
|
He asked to know re Transketolase and Transaldolase that:
1. Transketolase moves 2-C piece and requires a cofactor thiamine pyrophosphate 2. Transaldolase transfers a 3-C piece and DOES NOT require a cofactor. |
He asked us to know re Transketolase and Transaldolase that:
1. Transketolase moves 2-C piece and requires a cofactor thiamine pyrophosphate 2. Transaldolase transfers a 3-C piece and DOES NOT require a cofactor. |
|
|
What is Thiamine Pyrophosphate?
|
It's the co-factor required by Transketolase to move a 2-C piece.
|
|
|
The pentose pathway has a common genetic deficiency - what is it, what sxs does it cause, and what is its inheritability?
|
It is an X-linked deficiency in the G-6-P dehydrogenase enzyme that causes hemolytic anemia.
|
|
|
In pts with G-6-P dehydrogenase deficiency, oxidative stress caused by triple A (two other things) is the only way to identify that they have the disorder. What is the Triple A and the two other factors?
|
Triple A = Antibiotics (sulfa drugs), Anitmalarials (primaquin) and Antipyretics.
The other factors include viral or bacterial infections and/or ingestion of fava beans. |
|
|
If a pt shows sxs of hemolytic anaemia after taking primaquin, what genetic disorder might this pt have?
|
X-linked G-6-P dehydrogenase mutation.
|
|
|
Pyruvate can be sent down 5 different pathways according to the body's needs. All but one are reversible - which one?
|
Pyruvate to Acetyl-CoA is irreversible.
|
|
|
What three things does ALT accomplish that's good for the cell? (p. 126)
|
1. NADH is oxidized allowing glycolysis to continue
2. L-Alanine, a "pyruvate equivalent" is made that can be converted back to glucose 3. Ammonia (NH3) a toxic product of aa degradation, is converted to a safe derivative |
|
|
What is hydride (he said he wants us to know this)
|
It's hydrogen with two electrons
(H = H:) |
|
|
What does lactate dehydrogenase do?
|
It catalyzes the direct transfer of a hydride species bn NAD+ and C-2 of pyruvate.
|
|
|
Review p128 and how lipoic acid functions as a swinging arm that cycles between being a dithiol and disulfide form. 9/22 8:15a, 1:04
|
Review p128 and how lipoic acid functions as a swinging arm that cycles between being a dithiol and disulfide form. 9/22 8:15a, 1:04
|
|
|
I don't get what he's talking about on pg 129. 9/22 1:08
|
I don't get what he's talking about on pg 129. 9/22 1:08
|
|
|
Alcoholic polyneuropathy is a condition due to what?
|
Thiamine/VitB1 deficiency
|
|
|
If you're thiamine/vitB1 deficient, what would you expect re pyruvate?
|
Pyruvate and alpha-ketoglutarate levels in the blood would go up.
|
|
|
Clinically, how is thiamine/VitB1 deficiency evaluated?
|
By measuring thiamine activity in RBCs. Thiamine is required for Transketolase enzyme and measuring its activity from a patient sample will give you an idea of the status of this vitamin.
|
|
|
Pyruvate dehydrogenase enzyme deficiencies due to genetics are pretty rare bc of the importance of this enzyme. However, if it happens, what are sxs?
|
Patients exhibit psychomotor retardation and ataxia.
|
|
|
What role does biotin play in pyruvate carboxylase? (p130)
|
Biotin activated CO2 using ATP and then transfers it to pyruvate to make oxaloacetate. (p130)
|
|
|
Name the coenzyme the pair with the following vitamin:
1. Panothenate 2. Thiamine 3. Riboflavin (Vit B2) 4. Nicotinate (Niacin) 5. Biotin (vitamin H) 6. Pyridoxin (vitamin B6) |
1. Panothenate = Coenzyme A
2. Thiamine = Thiamine Pyrophosphate 3. Riboflavin (Vit B2) = Flavin Adenine Dinucleotide 4. Nicotinate (Niacin) = NAD+/NADH; NADP+NADPH 5. Biotin (vitamin H) = Biotin 6. Pyridoxin (vitamin B6) = Pyridoxal Phosphate |

