![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
33 Cards in this Set
- Front
- Back
|
What is Intrapleural Pressure (Pip)
|
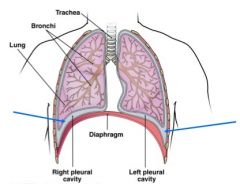
pressure in space between parietal & visceral pleura (also fluctuates with breathing) (~ slight vacuum)
• Should be ~ −4 mm Hg at rest ** remains below atmospheric pressure (Patm) throughout respiratory cycle |
|
|
Pressure Relationships
|
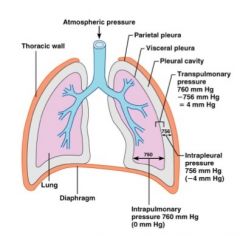
• Intra-alveolar pressure and intrapleural pressure fluctuate with the phases of breathing
• Intra-alveolar pressure always eventually equalizes itself with atmospheric pressure |
|
|
What is lung collapse?
|

caused by equalization of intrapleural pressure with intra-alveolar pressure
• without negative intrapleural pressure → lungs recoil and collapse |
|
|
pneumothorax
|
air enters intrapleural space
|
|
|
Gas exchange in the lungs occurs because of partial pressure differences...
Concentration gradient causes: |
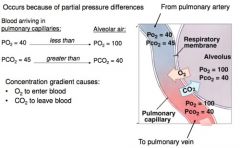
• O₂ to enter blood
• CO₂ to leave blood |
|
|
Gas exchange at the tissues occurs because of partial pressure differences...
Concentration gradient causes: |

• O₂ to enter tissues
• CO₂ to enter blood |
|
|
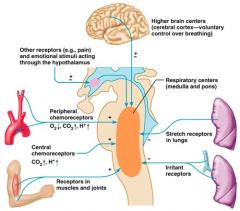
Control of Respiration involves neurons in the:
|
medulla and pons
|
|
|
Control of Respiration in the medulla .....
|
sets respiratory rhythm
|
|
|
Control of Respiration in the pons .....
|
influences and modifies activity of medullary neurons
|
|
|
What are the two respiratory groups of the Medullary Respiratory Centers?
|

Ventral Respiratory Group & Dorsal Respiratory Group
|
|
|
Ventral Respiratory Group (VRG)
|

• Rhythm generating
• Integrative center • Excites "quiet" inspiratory muscles & sets normal respiratory rate & rhythm • Inspiratory neurons (2 seconds) • signal contraction of diaphragm & external intercostals • Expiratory neurons (3 seconds) • output stops, inspiration ceases • passive expiration |
|
|
Dorsal Respiratory Group (DRG)
|

• Integrates input from:
• Peripheral Stretch receptors • Peripheral chemoreceptors to modify rhythms generated by VRG |
|
|
Pons Respiratory Center
|

• influences & modifies activity of medullary respiratory center
• "smooths out" inspiration and expiration transitions • e.g. modifies breathing rhythm set by VRG during vocalization, sleep & exercise • DRG & pons respiratory centers receive info from peripheral receptors & higher brain centers |
|
|
DRG & pons respiratory centers receive info from _____ & _____
|
DRG & pons respiratory centers receive info from peripheral receptors & higher brain centers
|
|
|
Breathing rate
|
determined by how long inspiratory center is active (breaths per minute)
|
|
|
Breathing depth
|
more stimulation → more motor units excited → greater force of breath
|
|
|
Factors that include breathing rate & depth are:
|
• Chemical****
• CO₂ • O₂ • pH • Reflexes • Higher Brain Centers • Exercise • Pain, emotional stimuli |
|
|
Chemoreceptos
|
sensors that respond to chemical flucuations
|
|
|
What are the two chemoreceptors?
|
central chemoreceptors & peripheral chemoreceptors
|
|
|
What are the two locations of the chemoreceptors?
|
• central chemoreceptors - medulla
• peripheral chemoreceptors - aortic arch & carotid arteries |
|
|
Factors influencing breathing rate and depth: PCO₂
|
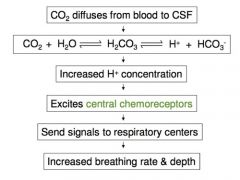
• CO₂ - most potent and closely controlled chemical
• Mediated mainly be central chemoreceptors detecting rising CO₂ |
|
|
Hyperventilation
|
increased depth and rate of breathing
• Quickly flushes CO₂ from blood • Occurs in response to high CO₂ ➤ Though a rise in CO₂ act as original status → control of breathing is actually regulated by H+ concentration in the brain |
|
|
Hypoventilation
|
slow and shallow breathing due to abnormally low PCO₂ levels
• Apnea (breathing cessation) - may occur until PCO₂ levels rise |
|
|
Apnea (breathing cessation)
|
may occur until PCO₂ levels rise
|
|
|
Peripheral chemoreceptors
|
in aortic bodies & carotid bodies
• Sensitive to O₂ changes (and CO₂) • Usually only respond to large changes in O₂ (vs very sensitive CO₂ receptors) • ok because we have large O₂ reservoir bound to Hb • drop in pH results in an increase in respiratory and breathing rate |
|
|
Factors influencing breathing rate and depth: arterial pH
|
central chemoreceptors and peripheral chemoreceptors
|
|
|
Central chemoreceptors
|
insignificantly affected by H+ from arterial blood
• little H+ diffuses from blood into CSF |
|
|
CO₂ and H+ are _____ → but they are distinct stimuli
|
• Drop in pH may reflect an increase in CO₂ but...
• Can reflect other acid accumulation (e.g. lactic acid) |
|
|
Body compensates for low pH by eliminating _____ by increasing breathing & respiratory rate.
|
CO₂
|
|
|
Body compensates for low pH by eliminating CO₂ by increasing breathing & respiratory rate.
Why does this make sense? |
CO₂ + H₂O ⇋ H₂CO₃ ⇋ H+ + HCO₃-
|
|
|
Inflation reflex (Hering-Breuer reflex)
|
stretch receptors in airways respond to changes in lung volume
• lungs stretched during inspiration • send signal to control center to inhibit inspiration • lungs recoil during expiration • send signal to control center to stimulate inspiration Thought to be a protective response (to prevent excessive stretching of lungs) |
|
|
Pulmonary irritant reflex
|
irritating physical/chemical stimuli in nasal cavity, larynx, and bronchial tree
• stimulate cough in trachea or bronchi • stimulate sneeze in nasal cavity |
|
|
Factors influencing breathing rate and depth
|
enter here
|

