![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
111 Cards in this Set
- Front
- Back
|
Case Control Study
|
Observational and RETROspective. Compares a group of people with disease to a group WITHOUT a disease. Asks the question, "what happened?"
Associated with Odds Ratio Ex: Patients with COPD had higher odds of a history of smoking than those without COPD. |
|
|
Cohort Study
|
Observational and PROspective
Compares a group of people with a given RISK FACTOR to a group of people without risk factor to assess whether the risk factor increases the likelihood of a disease. Asks the question, "what will happen?" Associated with Relative Risk Ex: Smokers had a higher risk of developing COPD than did nonsmokers |
|
|
Cross-Sectional Study
|
Observational and Acute
Collects data from a group of people to assess frequency of disease(and related risk factors) to a particular point in time. Asks the question, "What is happening?" Associated with Disease Prevalence. Important to note that you can show risk factors association with disease but DOES NOT establish causality. |
|
|
Twin Concordance Study
|
Compares the frequency for which monozygotic or dizygotic twins develop a disease. This measures heritability.
|
|
|
Adoption Study
|
Compares siblings raised by biologic vs adoptive parents. Measures heritability and influence of environmental factors.
|
|
|
Clinical Trials
|
Experimental Studies involving humans. Compares therapeutic benefits of 2 or more treatments, or of treatment and placebo. Study quality improves when study is randomized, controlled, and double-blinded.
|
|
|
Phase I Clinical Trials
|
Small number of healthy volunteers. This assesses the safety, toxicity, and pharmacokinetics of the drug.
|
|
|
Phase II Clinical Trials
|
Small number of patients with disease of interest. Assesses the treatment efficacy, optimal dosing, and adverse side effects.
|
|
|
Phase III Clinical trials
|
large number of patients randomly assigned either to treatment under investigation or the best available accepted treatment(or if no treatment, placebo).
This compares the new treatment to the current standard of care. |
|
|
Phase IV Clinical Trials
|
Postmarketing surveillance trial of patients after approval.
Purpose: Detects rare or long-term adverse effects. |
|
|
Evaluation of diagnostic tests
|
Uses 2x2 table comparing test results with the actual presence of disease. TP = True Positive; FP = False Positive; TN= True Negative; FN = False Negative
Sensitivity and Specificity are fixed properties of test; however, PPV and NPV vary with prevalence or pretest probability. |
|
|
Sensitivity (true-positive rate)
|
Proportion of all people with disease who test positive, or the probability that a test detects disease when a disease is present.
Value approaching 100% is desirable to rule OUT a disease(SNOUT) and indicates a low false negative rate(FN/FN+TP). Used for screening in diseases with low prevalence. Sensitivity = TP/(TP + FN) If 100% sensitivity = 1 FN = 0, and all negatives must be TN's |
|
|
Specificity (true-negative rate)
|
Proportion of all people without disease who test negative, or the probability that a test indicates non-disease when disease is absent. Value approaching 100% is desirable for ruling in disease and indicates a low false positive rate. Used as confirmatory test after a positive screening test
Specificity = TN/(TN+FP) Example: HIV testing. You screen with ELISA which is very sensitive, high FPR, and low threshold and then after that you confirm with Western Blot which is specific, high FNR and a high threshold. |
|
|
Positive Predictive Value(PPV)
|
Proportion of positive test results that are true positive.
Probability that a person actually has the disease after being given a positive result. PPV = TP/(TP+FP) |
|
|
Negative Predictive Value(NPV)
|
Proportion of negative test results that are true negative.
Probability that a person is disease free after being given a negative test result. NPV = TN/(TN+FN) |
|
|
Incidence vs. prevalence
|
Incidence rate = # of new cases / population at risk
Incidence looks at new incidents prevalence looks at all current incidents Prevalence = # of existing cases/population at risk |
|
|
Quantifying Risk
|
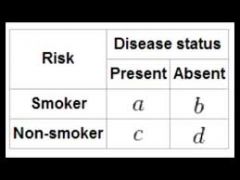
Disease can be (+) or (-)
Risk can be (+) or (-) a = (+) disease (+) risk b = (-) disease (+) risk c = (+) diease (-) risk d = (-) disease (-) risk |
|
|
Odds Ratio (OR)
|
Typically used in case control studies.
Odds that the group with the disease (cases) was exposed to a risk factor (a/c) divided by the odds that the group without the disease (controls) was exposed (b/d) Odds Ratio = (a/b)/(c/d) = ad/bc |
|
|
Relative Risk (RR)
|
Typically used in cohort studies.
Risk of developing disease in the exposed group. Relative Risk = Probability of disease in exposed / Probability of disease in unexposed Relative Risk = a/(a+b) / c/(c+d) |
|
|
Attributable Risk
|
The difference in risk between exposed and unexposed groups, or the proportion of disease occurrences that are attributable to the exposure
Attributable Risk = a/(a+b) - c/(c+d) |
|
|
Absolute Risk Reduction (ARR)
|
Absolute risk in the risk associated with a treatment as compared to a control
|
|
|
Number needed to Treat
|
Number of patients who need to be treated for 1 patient to benefit.
Calculated as 1/absolute risk reduction |
|
|
Number needed to Harm
|
Number of patients who need to be exposed to a risk factor for 1 patient to be harmed.
Calculated as 1/attributable risk |
|
|
Precision
|
The consistency and reproducibility of a test(Reliability) as well as the absence of random variation.
|
|
|
Accuracy
|
The trueness of test measurements (validity).
The absence of systematic error or bias in a test. |
|
|
Random Error
|
Reduces precision
|
|
|
Systematic Error
|
Reduces accuracy
|
|
|
Bias
|
PARCIALIDAD
Occurs when there is a systematic error or favor in a particular direction. To Reduce: Blind Studies, Placebo control groups, crossover studies, randomization and matching |
|
|
Selection bias
|
non-random assignment to study group.
|
|
|
Recall bias
|
knowledge of presence of disorder alters recall by subjects; common in retrospective studies
|
|
|
Sampling bias
|
subjects are not representative of the general population; therefore results are not generalizable. A type of selection bias.
|
|
|
Late-look bias
|
information gathered at an inappropriate time.
e.g. using a survey to study a fatal disease(only those subjects still alive will be able to answer survey) |
|
|
Procedure bias
|
subjects in different groups are not treated the same.
e.g. more attention is paid to the experimental group, stimulating greater compliance. |
|
|
Confounding bias
|
Occurs when factor is related to both exposure and outcome, but is not on the casual pathway; factor distorts or confuses effects of exposure on outcome
|
|
|
Lead-time bias
|
early detection confused with increased survival; seen with improved screening.(natural history of disease is not changed, but early detection makes it seem as though survival increased).
|
|
|
Observer - expectancy effect
|
Occurs when a researchers belief in the efficacy of a treatment changes the outcome of that treatment
|
|
|
Hawthorne Effect
|
Occurs when the group being studied changes its behavior owing to the knowledge of being studied.
|
|
|
Statistical Distribution
|
Measures of central tendency = mean, median, mode
Measures of dispersion = standar deviation (SD), Standard Error of the mean (SEM), Z-score, confidence interval |
|
|
Normal Distribution
|
Gaussian, also called bell-shaped
Mean = Median = Mode |
|
|
SD and SEM
|
The standard deviation of a sample of means from a given population.
SEM = σ/√n |
|
|
Positive Skew
|
mean > median > mode
Asymmetry with tail on the right. |
|
|
Negative Skew
|
mean < median < mode
Asymmetry with tail on the left. |
|
|
The Null Hypothesis(H0)
|
There is no statistical difference between the disease and the risk factor. Hypothesis of no difference.
|
|
|
The Alternative Hypothesis(H1)
|
There is some association between the disease and the risk factor.
|
|
|
Type I Error(α)
|
Stating that there is an effect or difference when none exists. In other words, to mistakenly accept the alternative hypothesis when the null hypothesis is true.
p = the probability of making a type I error. p is judged against α, a preset level of significance, usually less than 0.05. "False-positive error" Similar to convicting an innocent man. Related to specificity. |
|
|
Type II Error(β)
|
Stating that there is NOT an effect or difference when one exists.(To accept the null hypothesis when the alternative hypothesis is true. In other words, failing to reject the null hypothesis.)
β is the probability of making a Type II error. "False-negative error". Similar to setting a guilty man free. Related to sensitivity. |
|
|
Statistical Power(1-β)
|
Probability of rejecting the null hypothesis when it is in fact false, or the likelihood of finding a difference if one in fact exists. It depends on:
1.) Total number of end points experienced by population 2.) Difference in compliance between treatment groups(differences in the mean values between groups) 3.) Size of expected effect(preset level of significance for p. Raises likelihood of Type I error but reduces likelihood of Type II error) Notably, if you increase sample size, you increase power. There is power in numbers. Again, related to sensitivity since it is dependent on β. |
|
|
Meta-analysis
|
Pools data and integrates results from several similiar studies to reach an overall conclusion.
Increase statistical power. Limited by quality of individual studies or bias in study selection |
|
|
Confidence Interval
|
An interval in which you can say contains the true parametric mean with 95% certainty.
CI = mean ± 1.96(SEM) If the 95% CI for a mean difference between 2 variables includes 0, then there is no significant difference and the null hypothesis cannot be rejected. If the 95% CI for the odds ratio or relative risk includes 1, then the null hypothesis cannot be rejected. If the CI between 2 groups overlaps, then these groups are not significantly different. |
|
|
T-Test
|
T-test checks difference between the means of two groups.
Mr.T is mean |
|
|
ANOVA
|
ANOVA checks the difference between the means of 3 or more groups.
ANOVA = Analysis of Variance of 3 or more variables. |
|
|
χ²(Chi-squared Test)
|
χ² checks difference between 2 or more percentages or proportions of categorical outcomes.(not mean values).
χ² = compare percentages or proportions. |
|
|
Pearson's Correlation Coefficient(r)
|
r is always between -1 and + 1. The closer the absolute value of r is to 1, the stronger the linear correlation between 2 variables.
Coefficient of determination = r2 |
|
|
Disease Prevention
|
1° - Prevent disease occurrence(Vaccination)
2° - Early detection of disease(Pap smear) 3° - Reduce disability from disease(chemotherapy) PDR - Prevent, Detect, Reduce Disability |
|
|
Medicare and Medicaid
|
Federal program that originated form amendments to the Social Security Act.
Medicare is available to patients over 65 years of age and under 65 with certain disabilities, and those with end of stage renal disease. MedicarE is for Elderly Medicaid is a joint federal and state health assistance for people with very low income. MedicaiD is for Destitute |
|
|
Core Ethical Principles -
Autonomy |
Obligation to respect patients as individuals and to honor their preferences in medical care.
|
|
|
Core Ethical Principles -
Beneficence |
Physicians have special ethical(fiduciary) duty to act in the patient's best interest. May conflict with autonomy. If the patient can make an informed decision, ultimately the patient has the right to decide.
|
|
|
Core Ethical Principles -
Non-maleficence |
"Do no harm." However, if the benefits of an intervention outweigh the risks, a patient may make an informed decision to proceed(most surgeries)
|
|
|
Core Ethical Principles -
Justice |
To treat persons fairly.
|
|
|
Informed Consent legally requires...
|
Legally requires:
1.) Discussion of pertinent information 2.) Patient's agreement to the plan of care 3.) Freedom from coercion In other words, the patient must understand the risks, benefits, and alternatives, which include no intervention. |
|
|
Exceptions to Informed Consent
|
1.) Patient lacks DMC or is legally incompetent
2.) Implied consent in an emergency 3.) Therapeutic Privilege - withholding information when disclosure would severely harm the patient or undermine informed DMC 4.) Waiver - patient waives the right of informed consent. |
|
|
Consent for minors
|
Minor is generally any person <18 years of age. Parental consent must be obtained unless minor is emancipated(married, self-supporting, has children or is in military)
Parental consent is not required in (1) emergency situations (2) prescribing contraceptive (3)treating STD's (4) medical care of pregnancy, and (5) treatment of drug addiction |
|
|
Decision-making Capacity -
5 requirements and common problem associated with family. |
Physician must determine whether the patient is psychologically and legally capable of making a particular healthcare decision.
Components 1.) Patient makes and communicates a choice 2.) Patient is informed 3.) Decision remains stable over time. 4.) Decision is consistent with the patient's values and goals. 5.) Decision is not a result of delusions or hallucinations The patient's family CANNOT require that a doctor withhold information from a patient if the patient can demonstrate decision-making capacity. |
|
|
Advance Directives
|
Instructions given by a patient in anticipation of the need for a medical decision. State-specific.
|
|
|
Oral Advance Directive -
discuss validity |
Incapacitated patient's prior oral statement commonly used as a guide. Problems arise from variance in interpretation. If the patient was informed, directive is specific, patient made a choice, and decision was repeated over time, the oral directive is more valid.
|
|
|
Written advance directive -
Living Will |
Living Will
describes treatments the patient wishes to receive or not receive if he/she becomes incapacitated and cannot communicate about treatment decisions. Usually, patient directs physician to withhold or withdraw life-sustaining treatment if he/she develops a terminal disease or enters a persistent vegetative state. |
|
|
Written advance directive -
Durable Power of Attorney |
Durable Power of Attorney
patient designates a surrogate to make medical decisions in the event that he/she loses DMC. Patient may also specify decisions in clinical situations. Surrogate retains power unless revoked by patient. More flexible than a living will. |
|
|
Surrogate decision-maker
|
If an incompetent patient has not prepared an advance directive, individuals (surrogates) who know the patient must determine what the patient would have done if he/she were competent. Priority of surrogates: spouse, adult children, parents, adult siblings, other relatives.
|
|
|
Confidentiality
|
Confidentiality respects patient privacy and autonomy. Disclosing information to family and friends should be guided by what the patient would want. The patient may waive the right to confidentiality(e.g. insurance companies)
|
|
|
Exceptions to Confidentiality -
List 4 common exceptions and 5 common examples |
1.) Potential harm to others is serious
2.) Likelihood of harm to self is great 3.) No alternative means exist to warn or to protect those at risk 4.) Physician can take steps to prevent harm Examples include: -- Infectious diseases: Physicians may have a duty to warn public officials and identifiable people at risk. -- The Tarasoff decision: law requiring physicians to inform and protect potential victim from harm; may involve breach of confidentiality. -- Child and/or elder abuse -- Impaired automobile drivers -- Suicidal/homicidal patients: physicians may hold patients involuntarily for a period of time. |
|
|
Examples of Exceptions to Confidentiality
|
Reportable Disease (STD's, TB, Hepatitis, food poisoning)
The Tasaroff decision - California Supreme Court decision requiring physician to directly inform and protect potential victim of harm; may involve breach of confidentiality. Child and/or elder abuse Impaired automobile drivers Suicidal/homicidal patients |
|
|
Ethical Situations -
Patient is not adherent |
Appropriate Response:
Attempt to identify the patient's reason for nonadherence and determine his/her willingness to change; do not attempt to coerce the patient into adhering or refer the patient to another physician. |
|
|
Ethical Situations -
Patient desires an unnecessary procedure |
Appropriate Response:
Attempt to understand why the patient wants the procedure and address underlying concerns Do not refuse to see the patient or refer him/her to another physician. Avoid performing unnecessary procedure. |
|
|
Ethical Situations -
Patient has difficulty taking medications |
Appropriate Response
Provide written instructions; attempt to simplify treatment regimens; use teach-back method to ensure patient comprehension. |
|
|
Ethical Situations -
Family member asks for information about patient's prognosis |
Appropriate Response:
Avoid discussing issues with relatives without the permission of the patient. |
|
|
Ethical Situations -
A child wishes to know more about his illness |
Appropriate Response And Action:
Ask what the parents have told the child about the illness. Parents of a child determine what information can be relayed about the illness. |
|
|
Ethical Situations -
A 17-year old girl is pregnant and requests an abortion |
Appropriate Response
Many states require parental notification or consent for minors for an abortion. Unless she is at medical risk, do not advise a patient to have an abortion regardless of here age or the condition of the fetus. |
|
|
Ethical Situation -
A 15 year old girl is pregnant and wants to keep the child. Her parents want you to tell her to give the child up for adoption. |
Appropriate Response or Action:
The patient retains the right to make decisions regarding her child, even if her parents disagree. Provide information to the teenager about the practical issues of caring for a baby. Discuss the options, if requested. Encourage discussion between the teenager and her parents to reach the best decision. |
|
|
Ethical Situations -
A terminally ill patient requests physician assistance in ending own life |
Appropriate Response:
In the overwhelming majority of states, refuse involvement in any form of physician assisted suicide. Physicians may, however, prescribe medically appropriate analgesics that coincidentally shorten the patient's life. |
|
|
Ethical Situations -
Patient states that he/she finds you attractive |
Appropriate Response or Action:
1. Ask direct, closed-ended questions and use a chaperone if necessary. Romantic relationships with patients are NEVER appropriate(excluding the smoking hot women). Never say, "there can be no relationship while you are a patient" because that implies that a relationship may be possible if the individual is no longer a patient. |
|
|
Ethical Situation -
Patient is Suicidal |
Appropriate Response or Action:
Assess the seriousness of the threat; if it is serious, suggest that the patient remain in the hospital voluntarily; Patient can be hospitalized involuntarily if he/she refuses. |
|
|
Ethical Situations -
Patient is angry about the amount of time spent in the waiting room |
Appropriate Response or Action:
Acknowledge the patients anger, but do not tale a patient's anger personally. Apologize for any inconvenience. Stay away from efforts to explain the delay. |
|
|
Ethical Situations -
Patient is upset with the way he/she was treated by another doctor |
Appropriate Response or Action:
Suggest that the patient speak directly to that physician regarding his/her concerns. If the problem is with a member of the office staff, tell the patient you will speak to that individual. |
|
|
Ethical Situation-
A woman who has a mastectomy says she feels "ugly" when she is undressed |
Appropriate Response or Action:
Find out why the patient feels this way. Do not offer falsely reassuring statements (e.g. you still look good) |
|
|
Ethical Situations -
A drug company offers a "referral fee" for every patient a physician enrolls in a study. |
Appropriate Response or Action:
Eligible patients who may benefit from the study may be enrolled, but it is never acceptable for a physician to receive compensation from a drug company. Patients must be told about the existence of the referral fee. |
|
|
Ethical Situation -
A physician orders an invasive test for the wrong patient |
Appropriate Response or Action:
No matter how serious or trivial a medical error, a physician is ethically obligated to inform a patient that a mistake has been made. |
|
|
Ethical Situation -
A patient requires a treatment not covered by his/her insurance |
Appropriate Response or Action:
Never limit or deny care because of the expense in time or money. Discuss all treatment options with patients, even if some are not covered by the insurance companies. |
|
|
APGAR score
|

Assessment of newborn vital signs following labor via a ten point scale evaluated at 1 minute and 5 minutes.
Appearance, Pulse, Grimace, Activity and Respiration |
|
|
Low Birth Weight
|
Defined as <2500 grams.Caused by prematurity or intrauterine growth retardation. Associated with risk of SIDS and with rise in overall mortality. Complications include infections, Respiratory Distress Syndrome, necrotizing enterocolitis, intraventricular hemorrhage, and persistent fetal circulation.
|
|
|
Early Developmental Milestones -
Birth - 3 months |
Motor - Rooting reflex, holds head up, Moro reflex disappears
Social - Social Smile Verbal/ Cognitive - Orient and Responds to voice |
|
|
Early Developmental Milestones -
7 - 9 months |
Motor - Sit alone, crawls, transfers toys from hand to hand.
Social - Stranger anxiety Verbal/ Cognitive - Responds to name and simple instructions, uses gestures, plays peekaboo. |
|
|
Early Developmental Milestones -
12 - 15 months |
Motor - Walks, Babinski sign disappears
Social - Separation Anxiety Verbal/ Cognitive - Few Words |
|
|
Early Developmental Milestones -
12 - 24 months |
Motor - Climbs stairs, stacks 3 blocks at 1 yrs, 6 blocks at 2 years (age x 3 = no. of blocks)
Social - Rapprochement (moves away from and then returns to mother) Verbal/ Cognitive - 200 words and 2 word phrases at age 2 |
|
|
Early Developmental Milestones -
24 - 36 months |
Motor - Feed self with fork and spoon, kicks ball
Social - Core gender identity, parallel play. Verbal/ Cognitive - Toilet training (pee at age 3) |
|
|
Early Developmental Milestones -
3 years |
Motor - Rides tricycle(rides 3-cycle at age 3); copies line or circle drawing
Social - Comfortably spends part of day away from mother Cognitive/Social Milestone - 900 words and complete sentences |
|
|
Early Developmental Milestones -
4 years |
Motor - Uses buttons and zippers, grooms self (brushes teeth), hops on 1 foot, makes simple drawings (stick figures).
Cognitive/Social Milestone - Cooperative play, imaginary friends Cognitive - Can tell detailed stories and use prepositions. |
|
|
Changes in the elderly -
|
1.) Sexual changes - Men have slower erection/ejaculation with a longer refractory period while Women have vaginal shortening, thinning and dryness.
2.) Sleep patterns - decreased REM, slow-wave sleep, increased latency and awakenings. 3.) Common medical conditions are arthritis, HTN, heart disease, osteoporosis 4.) decreased incidence of psychiatric disorders 5.) increased suicide rate(males 65-74 years of age have the highest suicide rate in the US) 6.) decreased vision, hearing, immune response, and bladder control. 7.) decreased renal, pulmonary and GI function 8.) decreased muscle mass, increased fat NOTABLY sexual interest does NOT decrease and intelligence does NOT decrease. |
|
|
Grief
Normal vs pathological |
Normal bereavement characterized by shock, denial, guilt and somatic symptoms, typically lasts 6 months to a year. May experience illusions.
Pathologic grief includes extensively intense or prolonged grief or grief that is delayed, inhibited or denied. May experience depressive symptoms, delusions and hallucinations. |
|
|
Sexual Dysfunction Differential Diagnosis
|
Includes secual desire disorders, orgasmic disorders and secual pain disorders
Differential Diagnosis includes: 1.) Drugs(antihypertensives, neuroleptics, SSRIs, ethanol) 2.) Diseases(depression, diabetes) 3.) Psychological(performance anxiety) |
|
|
Body Mass Index(BMI)
|
BMI is a measure of weight adjusted for height.
BMI = weight in kg/(height in meters)² Measure of weight adjusted for height <18.5 underweight 18.5 - 24.9 normal 25.0 - 29.9 overweight\ >30.0 obese >40.0 morbidly obese >45.0 super obesity |
|
|
Sleep Stages -
Awake |
Awake(eyes open),alert, active mental concentration
EEG Waveform - Beta(highest frequency, lowest amplitude) Awake(eyes closed) EEG Waveform - Alpha |
|
|
Sleep Stages -
Stage N1 |
(5%) light sleep
EEG waveform - Theta |
|
|
Sleep Stages -
Stage N2 |
(45%) Deeper sleep; bruxism
EEG waveform - sleep spindles and K complexes |
|
|
Sleep Stages -
Stage N3 |
(25%) Deepest, non-REM sleep; sleepwalking, night terrors, bedwetting(slow-wave sleep0
EEG waveform - Delta(lowest frequency, highest amplitude) |
|
|
Sleep Stages -
REM |
(25%) Dreaming, loss of motor tone, possibly a memory processing function, erections, increased brain O2 use.
EEG waveform - Beta At night, BATS Drink Blood |
|
|
Key Points to remember about sleep
|
1.) Serotonergic predominance of raphe nucleus key to initiating sleep.
2.) Sleep enuresis is treated with oral desmopressin acetates (DDAVP), which mimes vasopressin; preferred over imipramine because of the latter's effects 3.) Alcohol, benzodiazepines, and barbiturates are associated with reduced REM and delta sleep. 4.) Benzodiazepines shorten stage 4 sleep; thus useful for night terrors and sleepwalking |
|
|
REM Sleep
|
increase and variable pulse, REM, increase and variable blood pressure, penile/clitoral tumescence. Occurs every 90 minutes; duration increases through the night. ACh is the principal neurotransmitter involved in REM sleep. REM sleep decreases with age.
REM sleep is like sex: increase pulse, penile/clitoral tumescence, decrease with age because rem has the same EEG patterns as wakefulness, it has been termed "paradoxical sleep" and "desynchronized sleep" |
|
|
Sleep patterns of depressed patients
|
Patients with depression typically have the following changes in their sleep stages:
Low slow wave sleep Low REM latency High REM early in sleep cycle High total REM sleep Repeated nighttime awakenings Early-morning awakenings (important screening question) |
|
|
Narcolepsy
|
Disordered regulation of sleep/wake cycles. May include hypnagogic(just before sleep) or hypnopompic(just before awakening) hallucinations. The patients nocturnal and narcoleptic sleep episodes start off with REM sleep. Cataplexy(loss of all muscle tone following a strong emotional stimulus) in some patients. Strong genetic component. Treat with stimulants(amphetamines and modafinil) and night time sodium oxybate (GHB)
|
|
|
Circadian Rhythm
|
Driven by suprachiasmatic nucleus(SCN) of hypothalamus; controls ACTH, prolactin, melatonin, nocturnal NE release, SCN --> NE release --> pineal gland --> melatonin. SCN is regulated by environment (i.e. light).
|
|
|
Sleep terror disorder
|
Periods of terror with screaming in the middle of the night; occurs during slow-wave sleep. Most common in children. Occurs during non-REM sleep (no memory of arousal) as opposed to nightmares that occur REM sleep (memory of a scary dream). Cause unknown, but triggers may include emotional stress during the previous day, fever, or lack of sleep. Usually self limited.
|

