![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
67 Cards in this Set
- Front
- Back
|
What does capnography rely on?
|
infrared absorption (function of molecular weight)
|
|
|
How does infrared absorption interpret the N20 in the presence of CO2?
|
amount of N2O is artificially higher due to CO2 having the same molecular weight
|
|
|
What is the cause of a sudden drop but not to 0 of the CO2 waveform?
|
leakage or partial obstruction of the airway
|
|
|
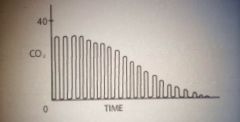
what is the cause of an exponential decrease of the CO2 waveform?
|
increased alveolar dead space such as PE or cardiac arrest
|
|
|
What does a gradual increase of the CO2 waveform indicate?
|
decreased minute ventilation, prolapse of the expiratory valve
|
|
|
What is the cause of a sudden increase in CO2 on the CO2 waveform?
|
release of a tourniquet (sudden increase in CO2)
|
|
|
in general what do peripheral and central chemoreceptors modulate?
|
-peripheral: ventilatory response to arterial hypoxemia (PaO2<60mm Hg, they do not respond to low O2 content);
-central: response to pH and pCO2 (CO2 actually cross the BBB and then in the CSF, H+ is formed and acidosis occurs) |
|
|
What is the afferent and efferent limb of the carotid and aortic bodies response to hypoxemia?
|
afferent CN IX (glossopharyngeal)
efferent CN X (vagus) |
|
|
where is the chemosensitive area in the brainstem that controls ventilation located?
|
medulla, in close proximity to CN IX (glossopharyngeal) and X (vagus)
|
|
|
How does CO2 rise during apnea?
|
6mm Hg the 1st minute and 3mm Hg for each minute thereafter
|
|
|
what is the ventilatory response to increased CO2?
|
increased tidal volume and increased RR
|
|
|
Where is hypoxic ventilatory drive primarily regulated?
|
carotid bodies
|
|
|
what is the slope of the carbon dioxide response curve?
|
0.5-0.7 liters/min/mm Hg(when CO2>100 slope is 2 L/m/mmHg)
|
|
|
When does carbon dioxide act as a ventilatory depressant?
|
PaCO2>100mmHg
|
|
|
What causes a left shift of the CO2 response curve (increased sensitivity to CO2)?
|
1. arterial hypoxemia,
2. metabolic acidemia, 3. central causes (increased ICP, anxiety, fear, cirrhosis), 4. drugs (doxepram, strychnine, picrotoxin (analeptics) |
|
|
what is the x and y axis of the CO2 response curve?
|
X-PaCO2, Y-alveolar ventilation
|
|
|
What causes a right shift of the CO2 response curve (decrease sensitivity to CO2)?
|
1. catecholamines,
2. metabolic alkalemia, 3. denervation of peripheral chemoreceptors, 4. normal sleep, 5. drugs - aminophylline, salicylates 6. hypothermia) |
|
|
What causes a down and to the right shift of the CO2 response curve?
|
1. high doses of opioids,
2. potent anesthetics (with increasing dose curve becomes more horizontal-not responsive to CO2, (greatest to least ventilatory depression is enflurane>halothane>isoflurane), 3. neuromuscular blockade |
|
|
How does 0.1MAC affect the ventilatory response to hypercarbia versus hypoxemia?
|
greater effect on the ventilatory response to hypoxemia than hypercarbia
|
|
|
What are the physiologic effects of hypoventilation-hypercarbia?
|
A RIPE:
A = acidosis, arrhythmias, R = right shift of oxy-hemoglobin curve, I = intracerebral steal, P = PA pressure increase, E = Epi-norepi release |
|
|
what are the physiologic effects of hyperventilation-hypocarbia?
|
AVCO:
A = apnea, alkalosis, airway constriction, V = V/Q mismatch, C = cardiac output, CBF, coronary blood flow and calcium all decrease, O = oxyhemoglobin curve shifted to the left |
|
|
How is CO2 carried in the blood?
|
1. carbaminohemoglobin,
2. bicarb - 70% 3. hydrated carbonic acid, 4. dissolved in solution - 7% |
|
|
what is the haldane effect?
|
affinity of hemoglobin for CO2 increases with deoxygenation
|
|
|
why is endobronchial intubation not detected by capnography?
|
- CO2 is more than 20x more diffusible than O2,
- as shunt increases the PaO2 progressively decreases but PaCO2 does not increase until the shunt is >50% |
|
|
What is the cause of a sudden drop to zero in the CO2 waveform?
|
technical defect such as a disconnect
|
|
|
What are the peripheral chemoreceptors? What do they respond to?
|
Aortic and carotid bodies which respond to arterial hypoxemia
|
|
|
What are the central chemoreceptors? What do they respond to?
|
found in the brainstem and modulate the response to pH and PaCO2
|
|
|
Activation of the aortic bodies result primarily in...
|
circulatory changes
|
|
|
What is the apneic threshold? What is the value?
|
The higher arterial or alveolar CO2 at which a pt will remain apneic.
-in humans is 5 mmHg below the resting PaCO2 |
|
|
What causes no effect upon CO2 response?
|
1. droperidol
2. diazepam (at 0.15 mg/kg) 3. midazolam (at 0.075 mg/kg) |
|
|
What is the Bohr effect?
|
the oxy-hemoglobin dissociation curve is impacted by PCO2 and pH
|
|
|
Which is more diffusible, CO2 or O2?
|
CO2 by more than 20x
|
|
|
what are the prototypical lesions that cause a shunt?
|
Shunt = perfused but not ventilated
1. pnuemothorax |
|
|
What is the normal shunt percentage?
|
<10% therefore over 90% of CO participates in gas exchange
|
|
|
What happens as the shunt fraction increases?
|
PaO2 progressively falls
PaCO2 does not increase until Qs/Qt exceeds 50% |
|
|
What are 2 examples of dead space problems?
|
dead space = ventilated but not perfused
1. PE 2. severe hypotension |
|
|
In what conditions is end tidal PCO2 not a valid measure of PaCO2? In what conditions is it valid?
|
Not valid:
1. pulmonary emphysema - shunt and dead space problem 2. PE - dead space problem 3. hypotension - dead space problem Valid: exhaused CO2 absorbent - there will be no uptake and no excretion so alveolar concentration will equilibrate with arterial and venous concentrations |
|
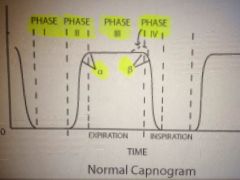
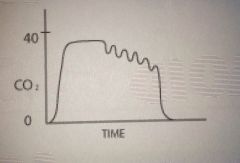
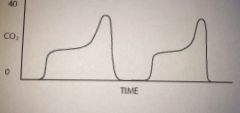
Describe the 4 phases of the capnogram.
|
Phase I: first portion of expiration, anatomic and apparatus dead space, low CO2
Phase II: mixing of dead space and alveolar gas, CO2 rises Phase III: CO2 rich alveolar gas, almost always has positive slope indicating rising CO2, highest point is PETCO2 Phase IV: beginning inspiration, CO2 free fresh gas, inhaled concentration falls to 0. |
|
|
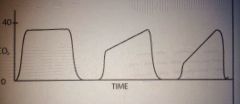
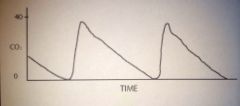
Partially obstructed ETT or airway
|
|
|
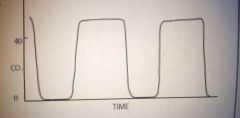
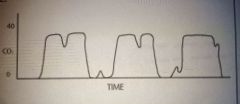
Re breathing of CO2 from one if several causes:
1. incompetent expiratory valve, 2. exhausted absorbent, 3. insufficient fresh gas flow |
|
|
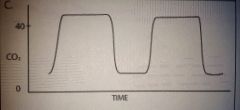
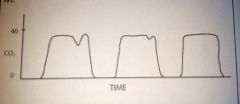
Side stream sampling too low
|
|
|
Contamination of expired sample - sampling may be too near fresh gas inflow or excessive rate of fresh gas inflow
|
|

|
Low end tidal CO2 indicative of hyperventilation
|
|
|
Elevated end tidal CO2 indicative of hypo ventilation
|
|

|
Release of tourniquet, unclamping of major vessel
|
|
|
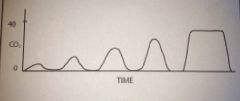
Exponential decrease in end tidal CO2 - large embolus or cardiopulmonary arrest
|
|
|
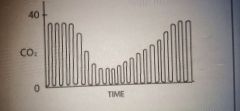
Small air embolus
|
|
|
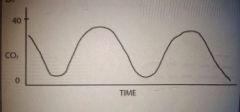
Cardiogenic oscillations
|
|
|
Spontaneous respiratory efforts
|
|
|
Curare cleft
|
|
|
Return to spontaneous ventilation
|
|
|
Leak in sampling line during PPV
|
|
|
What is the alpha angle?
|
The angle between phases II and III, an increased slope and larger alpha angle indicates increases airway obstruction
|
|
|
What is the beta angle?
|
The angle between phase III and IV, increase in this angle from 90 degrees indicates re breathing
|
|
|
Define capnometry vs capnography.
|
Capnometry - measurement of co2,
capnography - graphic display of co2 waveform |
|
|
What is the CO2 response curve?
|
A curve that measures minute ventilation in response to varying levels of CO2
|
|
|
Does 50% nitrous oxide depress the CO2 response curve?
|
No
|
|
|
What do benzos do to the CO2 response curve?
|
shift the curve down but not to the right
|
|
|
What is the effect of combined doses of halothan and nitrous oxide on the CO2 response curve?
|
depress the response less than halothane alone
|
|
|
How does hypoxia effect the CO2 response curve?
|
normally shifts the curve up and to the left ie stimulating ventilation
|
|
|
When does hypoxic ventilatory drive normally become strong?
|
when PO2 <50
|
|
|
What is the normal gradient between PaCO2 and PACO2? What factors increase this gradient?
|
<3 mmHg in healthy pts
1. V/Q mismatching - supine position, atelectasis, PE 2. increased dead space 3. rapid RRs with inadequate time for expiration 4. high sampling rate of side stream monitor, in the face of an elevated fresh gas flow rate 5. excessive PEEP causing overdistention of alveoli and impaired perfusion 6. decreased pulmonary blood flow caused by circulatory arrest, PE, sudden hypotension 7. Other - kinked ETT, partial disconnect, defective CO2 analyzer |
|
|
What can create a pneumoperitoneum during laparoscopy? What is the pressure target?
|
CO2 or nitrous oxide
- 20 mmHg |
|
|
Why is CO2 usually chosen for laparoscopy?
|
High solubiliity, it would offer some protection in case of accidental intravascular injection
|
|
|
What would be the advantages of choosing nitrous oxide for pneumoperitoneum during laparoscopy?
|
1. less diaphragmatic or peritoneal irritation
2. less shoulder pain 3. less risk of arrhythmia bc less hyhpercarbia |
|
|
What are the risks of using CO2 for pneumoperitoneum during laparoscopy?
|
1. gas embolism - signaled by hypotension or hypoxemia
2. pneumothorax or pneumomediastinum 3. arrhythmia from hypercarbia 4. reflux due to increased intraabdominal pressure 5. cardiovascular depression w/ pressures >30 - lead to hypotension, tachycardia, and decreases in CVP, pulse pressure, and CO |
|
|
What should MV be increased to during CO2 pneumoperitoneum?
|
1-1.5x the normal requirement
|

