![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
11 Cards in this Set
- Front
- Back
|
Basic epi of babesia
|
common tick-borne parasite of domestic and wild animals
rare zoonotic human infection serological surveys suggests higher prevalence of asymptomatic cases more severe in immunocompromised persons (ie, opportunistic) several species infecting humans |
|
|
What are the 2 most common species of babesia?
|
B. divergens
B. microti |
|
What is the life cycle of babesia?
|
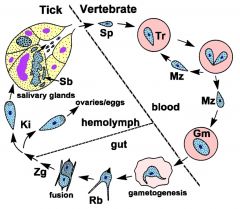
Sp= sporozoite
Tr= trophozoite Mz= merozoite Gm= gamont Rb=Ray body (gamete) Zg= zygote Ki= kinete The infection is acquired by the reservoir and human hosts when sporozoites are transferred from the salivary glands during tick feeding. The sporozoites invade erythrocytes utilizing a mechanism of invasion that is similar to other apicomplexa. In contrast to Plasmodium and many other apicomplexa, the parasitophorous vacuolar membrane disintegrates after invasion and the parasite is in direct contact with the host erythrocyte cytoplasm. Babesia trophozoites divide by binary fission and produce merozoites. In the large Babesia species paired trophozoites connected at the pointed end are often observed. The small Babesia species sometimes form a mini-schizont with four merozoites. This tetrad is often referred to as the Maltese cross form. The merozoites escape from the infected erythrocyte and reinvade other erythrocytes to reinitiate the replicative cycle. Some of the trophozoites will, instead of replicating, develop into gamonts (or gametocytes), which are responsible for initiating the infection in the ixodid tick vector. The gametocytes undergo morphological changes within the tick’s gut and develop into ray bodies (aka Strahlenkörper). Two ray bodies (i.e., gametes) will fuse to form a zygote which then develops into a kinete. The kinete is a mobile form that penetrates the peritrophic membrane and intestinal epithelium of the tick to gain access to the hemolymph. The kinetes invade various organs and undergo a few cycles of asexual replication. Large Babesia species can invade the ovaries and eggs leading to a transovarial (i.e., vertical) transmission to the tick’s offspring. The small Babesia species are not capable of this vertical transmission. Sporogony is initiated when kinetes invade the salivary glands. The parasite expands and fills a hypertrophied host cell and develops into a multinucleated sporoblast, or sporont. Mature sporozoites, possessing apical organelles, will bud from this undifferentiated sporoblast when the tick feeds again on a new host. A single sporoblast can produce 5000–10 000 sporozoites. The sporozoites are then injected into the host with the saliva, thus completing the life cycle. |
|
|
What are the clinical manifestations of Babesia?
|
asymptomatic to fatal
more severe symptoms in splenectomized, elderly, or immunocompromised persons characterized by fever, chills, sweating, myalgia, fatigue mild to severe hemolytic anemia (→ jaundice, hemoglobinuria) more severe and rapid progression in B. divergens than B. microti |
|
|
How do you diagnose babesia?
|
parasite detection in thin or thick blood smear
Diagnosis is confirmed by detecting the parasite in Giemsastained blood smears. Three basic blood stage morphologies are observed: ring forms, tetrads, and paired piriforms. The tetrads are more common in small Babesia and paired piriforms are more common in large Babesia. B. microti expresses primarily ring forms and tetrads are quite rare, whereas tetrads are more common in B. duncani. Paired piriforms can be observed in addition to the rings and tetrads in B. divergens. In general, speciating Babesia infections based on blood stages can be difficult because of the similar morphologies exhibited by the species. |
|
|
What are the factors distinguishing Babesia and falciparum malaria?
|
Presence of tetrads and paired piriforms
Lack of travel to malaria endemic area Lack of response to anti-malarials Infection of rodents Serology Molecular analyses |
|
|
Summary and key points:
|
Babesiosis is a rare zoonotic infection transmitted by ticks.
l The most predominant species in humans are Babesia microti in northeastern United States and B. divergens in Europe. l The infection can produce a wide range of symptoms from asymptomatic to an acute febrile illness to hemolytic anemia to death. l Splenectomy and other immunocompromising conditions are risk factors for severe disease. l Diagnosis is made by detecting the parasite in blood smears and can be confused with malaria due to morphological similarities. l Treatment involves chemotherapy and in severe cases exchange transfusion. |
|
|
How do you treat babesia?
|
no generally effective drugs
clindamycin + quinine is recommended atovaquone +azithromycine blood transfusions for severe anemia |
|
|
how does clindamycin + quinine help treat babesia?
|
reduces duration of parasitemia
high level of adverse side affects |
|
|
how does atovaquone + azithromycin help treat babesia?
|
as effective as clindamycin + quinine
fewer adverse affects |
|
|
how do you control babesia?
|
avoid tick bites
|

