![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
135 Cards in this Set
- Front
- Back
|

|
|
|
|
|

|
|
|

|
penile hematoma
|
|
|

|
|

|
persistent frenulum
|
|

|
preputial avulsion
|
|

|
preputial prolapse
|
|
|
|
|

|

|
|

|
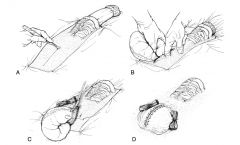
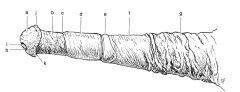
segmental posthectomy
|
|
|

|
|

|
urethra rent
|
|
|
|
|
|
|
|
|

|
|
|
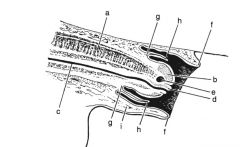
Location of the urethra:
|
passes over the ischial arch at the root of the penis, and becomes incorporated into the shaft of the penis. The urethra is located more ventral in the shaft of the penis
|
|
|
What forms the root of the penis?
|
a left and right crura originating on the lateral aspect of the ischial arch and converging below the arch, forming the shaft
|
|
|
How is the proximal portion of the shaft attached?
|
to the ventral aspect of the ischium by the suspensory ligaments of the penis
|
|
|
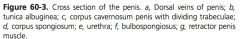
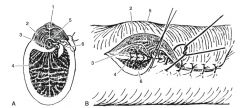
Location of corpus cavernosum penis (CCP):
|
dorsal to the urethra, begins at the union of the crura and ends distally in 3 projections, 1 centrally located, and 2 ventrolateral
|
|
|
What is the urethral groove?
|
ventral surface of the CCP
|
|
|
Location of corpus spongiosum penis:
|
surrounds the urethra and is located within the urethral groove of the CCP.
|
|
|
What is the glans penis?
|
CSP expands distally, covering the distal projections of the CCP
|
|
|
Location of bulbospongiosus muscle:
|
covers the ventral aspect of the CSP, the entire length of the penis
|
|
|
What is the bulbospongiusus continuous with?
|
Proximally with the urethralis muscle
|
|
|
What surrounds the CCP and CSP?
|
tunica albuginea, which is a thick, fibroelastic capsule, sending trabeculae into the spaces to form a supporting framework within the spaces
|
|
|
What are the CCP and CSP lined with?
|
endothelial cells and longitudinal bundles of smooth muscle
|
|
|
What maintains the non-erect penis in the prepuce?
|
Tone in smooth muscles of the CSP and CCP and the retractor penis muscle
|
|
|
What is the corona glandis?
|
circular edge of the glans penis
|
|
|
What is the collum glandis?
|
constriction behind the corona glandis
|
|
|
What is the fossa glandis?
|
deep depression in the glans penis from which the urethra protrudes
|
|
|
What is the urethral sinus?
|
dorsal diverticulum in the fossa glandis
|
|
|
Describe erection:
|
Parasympathetic input dilates and straightens the coiled branches of the deep artery of the penis and relaxes smooth muscle, enabling blood to flow into the spaces within the CCP and CSP. Engorgement of the CCP and CSP is restricted by the tunica albuginea and the trabeculae. Venous return is restricted to maintain engorgement of the CCP and CSP. Contraction of the ischiocavernosus muscle, stimulated by the pudendal nerves, elevates the penis and compression against the ischium forces blood into the CCP and impedes venous return from the CCP. During peak erection, the arterial supply is also occluded in the manner, making the CCP a completely closed space. Increased arterial flow into the CSP and contraction of the bulbospongiosus muscle increase pressure in the CSP. The CSP remains an open system during erection because vessels entering are not compressed against an osseous structure and blood can exit out of the dorsal veins. Contraction of the ischiourethral muscle impedes venous return by compressing the dorsal veins.
|
|
|
Location of the ischiocavernosus muscle:
|
arise from the tuber ischii and attach to the crura and the proximal aspect of the shaft
|
|
|
Location of the ischiourethral muscle?
|
extends from the ventral surface of the ischium, goes around the ischial arch, and end at the ventral aspect of the urethralis muscle
|
|
|
Describe ejaculation:
|
Contraction of the urethralis muscle forces release of seminal fluids. Contraction of the bulbospongiosus muscle causes a pressure wave down the CSP expelling semen from the urethra.
|
|
|
Location of the retractor penis muscle:
|
arise on the floor of the coccygeal vertebra, forming a loop under the rectum and anus, but extending distally with the bulbospongiosus muscle to end at the glans penis
|
|
|
Arterial supply to the penis:
|
from the internal and external pudendal arteries and the obturator artery
|
|
|
What does the external pudenal supply?
|
the dorsal artery of the penis, the major source of blood during erection and supplies the caudal superficial epigastric artery, which is the arterial supply to the prepuce
|
|
|
What does the obturator artery supply?
|
deep arteries of the penis, which supplies blood to the CCP
|
|
|
What does the internal pudendal supply?
|
pelvic urethra and the CSP
|
|
|
What are the accessory glands?
|
paired seminal vesicles, bulbourethral, and ampulla of the ductus deferens and the unpaired prostate
|
|
|
Where is the ampulla of the ductus deferens?
|
widen portion with walls thickened with secretory glands, located near the midline of the pelvic floor
|
|
|
Where are the seminal vesicles located?
|
on the dorsal surface of the neck of the bladder, lateral to the ampullae
|
|
|
Where do the seminal vesicles and ampullae drain?
|
open with or near the ampulla on the colliculus seminalis through the ejaculatory duct, a rounded prominence on the dorsal aspect of the urethra
|
|
|
Wher is the prostate located?
|
dorsal aspect of the neck of the bladder, caudal to the seminal vesicles
|
|
|
Where do prostratic secretions exit?
|
through small slit-like prostatic ducts, located lateral to the colliculus seminalis
|
|
|
Where are the bulbourethral glands located?
|
dorsolateral to the urethra at the level of the ischial arch, 2-3 cm caudal to the prostate
|
|
|
What supports the prepuce?
|
suspensory ligament, within the external lamina, the is derived from the abdominal tunic
|
|
|
What is the plica preputialis/ preputial fold?
|
When the penis is retracted, the internal lamina doubles on itself
|
|
|
What is the preputial ring?
|
opening of the plica preputialis
|
|
|
How is the pudendal nerve blocked?
|
3 to 5mL lidocaine is injected 2cm dorsal to the ischial arch and 2 cm lateral to the anus
|
|
|
Treatment of Preputial lacerations:
|
sutured to prevent infection and cellulitis
|
|
|
Treatment of penile wounds?
|
Fresh penile wounds should be sutured. Chronic infected wounds should be cleaned and treated with topical antimicrobials without repair
|
|
|
Treatment of urethral lacerations?
|
should be reapposed or if complete, penile amputation should be considered
|
|
|
Consequences of untreated urethral injuries?
|
cutaneous-urethral or cavernourethral fistulas
|
|
|
Consequences of laceration into cavernous regions?
|
may result in shunt and lead to impotence
|
|
|
Treatment of lacerations into CCP or CSP?
|
tunica should be repaired
|
|
|
Treatment of Penile hematomas:
|
compression wrapping repeatedly until the maximal decrease in size is achieved. The penis is then supported within the prepuce or against the abdomen until resolution of swelling
|
|
|
Paraphimosis:
|
inability to retract the protruded penis
|
|
|
Causes of paraphimosis:
|
Trauma leads to edema, the weight of the edema tires the smooth muscles that maintain the penis within the prepuce or administration of phenothiazine tranquilizers blocking motor innervation to the retractor penis muscle
|
|
|
What is balanoposthitis?
|
inflammation of the penis and prepuce
|
|
|
What complicates paraphimosis?
|
Pooling blood within the CCP of the protruded penis occurs within 2-5 hours, leading to further edema, impaired venous drainage, and fragility to exposed tissues. Exposed tissues become excoriated, leading to further inflammation and cellulitis. Chronic inflammation results in fibrosis of the penile skin and permanent impairment of the normal telescoping action of the penis and prepuce. The weight of the penis can cause damage to the pudendal nerves
|
|
|
Treatment of acute paraphimosis:
|
controlling edema and preventing further trauma. The penis can be retained within the prepuce or if too swollen to be retained in the prepuce, it can be retained against the abdomen with a support or within a bandage
|
|
|
Treatment of chronic paraphimosis:
|
fibrosed preputial ring can be incised longitudinally (preputiotomy), cicatrical tissue can be resected with segmental posthectomy, or the horse salvaged for non-breeding purposed with bolz procedure, extensive posthectomy, or partial phallectomy
|
|
|
Phimosis:
|
inability to protract the retracted penis from the prepuce due to stricture of the preputial orifice or the preputial ring
|
|
|
Consequences of phimosis:
|
Urine exposure in the preputial cavity exacerbates inflammation leading to further scarring
|
|
|
Treatment of preputial orifice phimosis:
|
wedge of the external preputial lamina can be resected and the internal and external lamina are joined with a row of interrupted sutures
|
|
|
Treatment of preputial ring phimosis:
|
wedge is removed from the internal preputial lamina and segmental posthectomy is performed
|
|
|
Priapism:
|
persistent erection without sexual excitement, from disturbance of wither arterial inflow or venous outflow to the CCP
|
|
|
Causes of priapism:
|
after administration of phenothiazine (alpha anatagonist) medication, general anesthesia, EPM, and pelvic canal neoplasia
|
|
|
What is high flow priapism?
|
occurs when arterial flow into the CCP is increased, likely from arteriocavernosal shunt, with inability of the venous drainage to compensate for the increase
|
|
|
What is low flow priapism?
|
result of altered neural impulses controlling venous drainage, results in blood stasis within the CCP, with arterial flow continuing in the early phases of formation, which becomes static with formation of blood clots, edema, and chronically, fibrosis
|
|
|
What flow of priapism affects horses?
|
Low flow
|
|
|
Consequences of priapism:
|
penis and internal lamina will become edematous resulting in paraphimosis. Chronic priapism results in damage to the pudendal nerves from compression against the ischium, resulting in paralysis of the penis
|
|
|
Medication treatment of acute priapism:
|
topical therapies aimed at preventing preputial edema, support against the abdomen, and re-establishing normal circulation to the erectile tissue
|
|
|
Drugs administered to affect circulation to erectile tissues in acute priapism:
|
benztropine mesylate, a combination of atropine and diphenhydramine, working through anticholinergic effects. Terbutaline and clenbuteral, both beta-2 adrenergics. Alpha adrenergic agents into the CCP or CSP such as phenylephrine, ephedrine, or epinephrine by promoting contraction of cavernous and arterial smooth muscles
|
|
|
Most common alpha agonist used in acute priapism:
|
Phenylephrine
|
|
|
Options for acute priapism if medical therapies are unsuccessful:
|
CCP should be lavaged with heparin containing saline
|
|
|
Describe lavage of the CCP:
|
12 gauge needle is inserted distally and 1-2 12 gauge needles are inserted caudal to the scrotum. The lavage is continued until fresh blood appears. Phenylephrine can be instilled into the CCP at the end of lavage
|
|
|
What is indicated if fresh blood does not appear after lavage of CCP?
|
arterial supply to the CCP is permanently damaged
|
|
|
What are the options in acute priapism if lavage and medical therapies fail?
|
shunt created between the CCP and the CSP, or phallectomy
|
|
|
Benefits of CCP CSP shunt in priapism:
|
Since the CSP is not a closed system, shunt will allow outflow of blood from the CCP through the CSP
|
|
|
Describe creation of CCP CSP shunt:
|
15 cm incision is made along the perineal raphe, 4-8 cm caudal to the base of the scrotum. The retractor penis muscle is retracted, the bulbospongiosus muscle is elevated to exposed the edge of the urethral groove. A 3cm incision is made into the tunica albuginea of the CCP, allowing stagnant blood to be evacuated. A second 3 cm incision is made into the tunica albuginea of the CSP. The medial edge of the CCP tunica albuginea is sutured to the lateral edge of the CSP tunica albuginea and the lateral edge of the CCP tunica albuginea is sutured to the medial edge of the CSP tunica albuginea to create the shunt. The bulbospongiosus is sutured to is origin on the CCP tunica albuginea and the SQ and skin are closed
|
|
|
Complications of surgically created cavernous shunt:
|
urethrocavernous or urethrocutaneous fistulas, penile necrosis, infection, or pain during erection
|
|
|
Hypospadias:
|
congenital defect in which the urethral opening is on the ventral aspect of the penis, proximal to its normal location
|
|
|
Cordee:
|
abnormal curvature to the penis
|
|
|
Treatment of hypospadias or cordee:
|
amputation of the deformed portion of the penis
|
|
|
Most common location of SCC:
|
glans penis and the internal lamina of the prepuce
|
|
|
Most common location of habronemiasis:
|
preputial ring and the urethral process
|
|
|
Causes of hemospermia:
|
bacterial urethritis, habronemiasis, neoplasia, seminal vesiculitis, trauma, or urethral rents
|
|
|
Surgical treatment for hemospermia:
|
Temporary perineal urethrostomy or incision into the convex surface of the tunica albuginea of the CSP, repair of urethral rent through a perineal incision
|
|
|
Causes of hematuria:
|
urinary origin calculi, urinary origin neoplasia, pyelonephritis, and urethral rents
|
|
|
Treatment for urethral rents:
|
temporary urethrostomy, incision into the convex surface of the tunica albugina of the CSP, or repair through a perineal incision
|
|
|
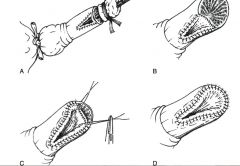
Synonyms for Segmental posthectomy:
|
posthioplasty or reefing
|
|
|
Describe segmental posthectomy:
|
Parallel circumferencial incision are made through the epithelial layer, proximal and distal to the lesion. A longitudinal incision connects the 2 circumferential incisions. 4 equidistant sutures are placed around the penis to appose the proximal and distal epithelial edges. The tissue between the 2 circumferencial incisions is undermined circumferentially and removed. The portions of the unopposed epithelium are apposed in an interrupted or continuous pattern.
|
|
|
Where are incisions made if segmental prosthectomy is to retain the penis in the prepuce:
|
proximal incision is made close to the prepuce orifice and the distal incision is made where the internal preputial lamina inserts on the free body of the penis
|
|
|
How is apposition of the proximal and distal incision of segmental posthectomy modified is they are of different sizes?
|
2 triangular portions of the proximal incision can be removed, with the base of the triangle the proximal circumferential incision. The sides of the triangle are closed, making the proximal circumferential incision smaller and easier to appose to the distal circumferential incision
|
|
|
Indications for Boltz phallopexy:
|
permanently retract the penis in the prepuce
|
|
|
When is the Boltz phallopexy technique not indicated?
|
If the internal lamina of the prepuce is damaged, unless it is first removed with a segmental posthectomy, or if the horse is still capable of maintaining an erection
|
|
|
Describe boltz phallopexy:
|
10 cm incision is made on the preputial raphe caudal to the scrotum. The penis is bluntly separated from fascia and retracted through the incision until the reflection of the internal preputial lamina is seen through the incision. The penis is anchored with heavy, non-absorbable suture on either side of the incision, from the skin, through the annular ring of the lateral surface of the penis, back through the skin. A roll of gauze is place over the pexy site and the suture is tied. The SQ and skin are closed in separate layers. Post-operative the pexy sutures can be adjusted so that the glans penis is just flush with the preputial orifice. The pexy sutures can be removed in 10-12 days after adhesion formation maintains the new position of the penis.
|
|
|
Describe Amputation of the urethral process:
|
urinary catheter is placed in the urethra and the urethral process is retracted out of the fossa. Small gauge needles are placed at 90 degree angles through the urethra and the urinary catheter proximal to the site of amputation to maintain traction on the urethra. A circumferential incision is made around the base of the urethra process proximal to the lesion and distal to the anchoring needles. The mucosa of the urethra is apposed to the epithelium of the stump in a simple interrupted or continuous pattern, compressing the tissue of the CSP
|
|
|
Complications of amputation of the urethral process:
|
Hemorrhage can be seen from the stump for several days after amputation
|
|
|
options for partial phallectomy:
|
vinsot’s technique, the william’s technique, the scott technique, en bloc resection with retroversion, and en bloc resection without retroversion
|
|
|
early complications of partial phallectomy:
|
hemorrhage from CSP of the penile stump especially with urination for several days post-operatively, dehiscence, hematoma formation, pain, infection, edema, and urinary obstruction for edema or inflammation of the urethra
|
|
|
Long term complications of partial phallectomy:
|
chronic recurrent cystitis, urine induced dermatitis, dysuria from stricture, and recurrence of neoplasia
|
|
|
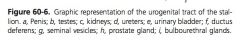
Describe Vinsot’s technique:
|
2.5 cm by 4 cm triangular section of the ventral penis is created proximal to the intended amputation, with the base of the triangle proximally. The urethra is incised and sutured to the epithelial border of the triangle, including the tunica albuginea of the CSP. The penis is amputated in a wedge shaped incision 4-5 cm distal to the triangle incision. Dorsal vessels are ligated. The CCP and the CSP are compressed with suture through the tunica albuginea, and the stump is closed with suture through the penile or preputial skin
|
|
|
How can vinsot’s technique be modified?
|
placement of a fixation ligature or a tight latex calf banding loop at the site of amputation and allowing the segment to necrosis and heal by second intension. Triangular incision can be replaced with a linear incision, with apposition of the urethral mucosa to the epithelium, incorporating the tunica albuginea of the CSP for compression
|
|
|
Advantages of the William’s technique over Vinsot’s:
|
urethral stricture and urine dermatitis
|
|
|
Describe william’s technique?
|
triangular incision is made on the ventral surface of the penis but the base of the triangle is part of the amputation incision. The mucosa of the urethra on the sides of the triangle are sutured to the penile epithelium, in a simple continuous or interrupted pattern, incorporating the tunica albuginea of the CSP. The penis is amputated and large vessels ligated. At the base of the amputation, the tunica albuginea of the CSP is compressed by suturing to the urethra mucosa. The remainder of the stump is closed by suturing the urethral mucosa at the base to the epithelium, incorporating the tunica albuginea of the urethral groove and the CCP, in 2 or 3 layers. 3 layers through the mucosa ensures good compression on the canvernous tissue
|
|
|
describe scott’s technique:
|
circumferential incision is made through the epithelium to the level of the urethra. A 4 cm segment of the urethra distal to the circumferential incision is freed from the stump before transection. The CCP is closed by suturing the outer CCP tunica albuginea to the inner CCP tunica albuginea with interrupted sutures. The CSP is closed with suture from the CSP tunica albuginea to the submucosa of the urethra in a continuous or interrupted pattern. The urethral stump is divided into 3 equal triangular segements and sutures to 3 similarly prepared segments of preputial or penile epithelium in a simple interrupted pattern or the urethral mucosa can be folded back over and sutured circumferentially to the penile or preputial epithelium and tunica albuginea
|
|
|
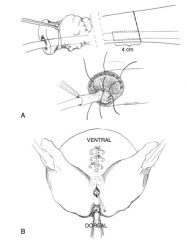
describe en bloc partial phallectomy with penile retroversion:
|
elliptical incision is made around the preputial orifice starting 6 cm cranial and extending 10 cm caudal, to the level of the abdominal tunic. The penis is amputated 6-8 cm caudal to the fornix of the prepuce in the scott method, so that there is a 4 cm segment of urethra protruding from the penile stump. A 6 cm subischial incision is made 20 cm ventral to the anus and the penile stump is retroverted through this incision. The tunica albuginea of the CCP and the fascia of the penis are sutured to the subcutaneous tissue of the subischial incision. The urethra is incised longitudinally on the ventral surface and the urethra is sutured to the subischial skin. Penrose drains are applied deeply through the cranial incision before closure of the SQ and skin
|
|
|
describe Partial phallectomy without retroversion:
|
A similar elliptical incision is created around the prepuce, and dissection is continued to exposed at least 10 cm of the shaft of the penis. The penis is amputated similar to the William’s technique, with a triangular segment from the ventral aspect of the penis, closing and compressing the cavernous layers but not the urethral layer. The penile stump is sutured to the body wall. The SQ tissue cranial to the stump is apposed. Skin is sutured to the tunica albuginea and the cranial aspect of the urethra. The caudal sides of the urethra are sutured to the skin and skin caudal to the orifice is closed
|
|
|
benefits of partial phallectomy without penile retroversion:
|
maintains the ventral position of the penile stump, has smaller incisions, and alters the horse’s normal appearance less
|
|
|
describe temporary perineal urethrostomy:
|
6-8 cm vertical incision 2-3 cm ventral to the anus, tunneled down to an incision through the urethra
|
|
|
Complications of temporary PU:
|
hemorrhage from the external pudendal vessels if the incision is off midline
|
|
|
How does the ruminant penis differ from the horse?
|
has a sigmoidal flexure located just caudal to the scrotum, the urethra has a dorsal diverticulum, there is an apical ligament, and in the ram and buck the urethral process extends 4-5 cm beyond the glans penis
|
|
|
What is the consequence of the ruminant urethral dorsal diverticulum?
|
makes catheterization difficult or impossible
|
|
|
What is the function of the apical ligament?
|
holds the penis straight for intromission
|
|
|
What provides diagnostic or surgical anesthesia?
|
blocking either the pudendal nerve or the dorsal nerve of the penis
|
|
|
How is the ruminant pudendal nerve blocked?
|
approached between the caudal fold of the tail and the caudal extent of the sacrosciatic ligament, guided per rectum, for injection at the level of the lesser ischiatic formen
|
|
|
Surgical treatment of ruminant seminal vesiculitis:
|
removal of gland by either ischiorectal approach or an approach through the floor of the rectum
|
|
|
Describe ischiorectal seminal vesicular gland removal:
|
crescent shaped incision can be made in the ischiorectal fossa, with blunt dissection to the gland, blind blunt freeing of the gland, and ecraseur transection
|
|
|
Complications of ischiorectal seminal gland removal:
|
severe hemorrhage from the large vessels adjacent to the surgical approach and iatrogenic damage to nerve that control erection and ejaculation within in the surgical area
|
|
|
Where do penile hematomas occur in ruminants?
|
just distal to the distal aspect of the sigmoid curve of the penis
|
|
|
Complications of hematomas in ruminants:
|
abscess +/- adhesion formation
|
|
|
Treatment of penile hematomas in ruminants:
|
larger than 15 cm should be approached surgically to remove blood and clot to reduce the risk of adhesion formation
|
|
|
When does corkscrew or deviation of the penis occur?
|
when the apical ligament slips before intromission occurs, preventing intromission
|
|
|
Surgical options for corkscrew penis?
|
anchoring the apical ligament to the tunica albuginea or augmentation of the ligament with strips of fascia lata
|
|
|
Options for production of teaser bulls:
|
epididyectomy or vasectomy, preputial relocation, preputial obliteration, penile tiedown, or phallectomy
|
|
|
Approaches to penile tie down:
|
tacking the dorsal aspect of the penis to the ventral body wall or by attaching the penis to the skin between the scrotum and the anus
|
|
|
What does relocation of the prepuce involve?
|
resection of the skin and tissue surrounding the prepuce, removal of an area of skin laterally near the flank fold, tunneling from the preputial incision to the flank incision, and replacement of the prepuce in the flank incision
|
|
|
When does preputial avulsion occur?
|
injury common to bulls used for semen collection
|
|
|
What is preputial avulsion?
|
penile skin at the point of reflection of the internal preputial laminia is torn
|
|
|
Treatment options for preputial prolapse:
|
resection of stricture by either preputiotomy or segmental posthectomy
|

