![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
48 Cards in this Set
- Front
- Back
|
What is the most common signalment for dens fracture with atlantoaxial subluxtion?
|
Foal younger than 6 months of age
|
|
|
What is the embryologic origin of the dens?
|
Body of the atlas
|
|
|
When does closure of the dens-axis physis close?
|
8-12 months
|
|
|
What is the most common location of dens fracture?
|
Cranial physis of the axis which separates the dens from the body of the axis (remains attached to the atlas, axis displaces ventrally)
|
|
|
What is the goal of surgery to fix dens fracture?
|
Decompression at fracture site by realignment of the vertebrae and providing stability with fixation
|
|
|
What surgical techniques have been described for dens fracture fixation?
|
External fixation with Steinman pins, ventral compression plating with DCP, ventral atlantoaxial fusion with cancellous bone screws, dorsal laminectomy of caudal atlas
|
|
|
What is the etiology of atlantoaxial subluxtion without concurrent dens fracture?
|
Congenital or traumatic
|
|
|
What is the anatomical result of complete atlantoaxial luxation?
|
Complete disruption of the ligamentous attachment to the dens with displacement of the dens ventral to the atlas
|
|
|
Surgical option for atlantoaxial subluxation:
|
subtotal dorsal laminectomy of the caudal 2/3 of the dorsal arch of the atlas, leaving a portion of the dorsal atlantoaxial ligament intact
|
|
|
What are the possible sequella of fractures of the ventral arch of the atlas?
|
Healing with a bony callus that impinges the spinal cord, inducing ataxia at a later time frame than the original injury
|
|
|
Recent approach to vertical fracture of the axis:
|
reduction of fracture with Steinman pins and bone reduction forceps then plate fixation with a 7 hole narrow 4.5mm DCP on the dorsal rim of the axis with 4.5 mm cortical screws
|
|
|
When does caudal cervical vertebral physis closure occur?
|
4-5 years however likely functionally closed around 2 years
|
|
|
What can occur with caudal articular process fractures?
|
Pedicle elevates resulting in deroofing of the spinal canal
|
|
|
What maintains stability after deroofing of the spinal canal?
|
Dorsal portion of the intervertebral disc
|
|
|
What imaging modalities have recently been described for diagnosis of cervical vertebral fracture in the standing horse?
|
Radiography, ultrasonography, nuclear scintigraphy, fluoroscopy
|
|
|
What is a possible sequella of caudal cervical vertebral fracture?
|
Worsening of neurologic signs after natural or surgical fusion because of compression at intervertebral sites adjacent to the fusion
|
|
|
What are the most common locations for thoracolumbar vertebral body fractures?
|
T1-3, T12, all L
|
|
|
What is the most common location for fracture of the dorsal spinous processes?
|
T6
|
|
|
Who are candidates for thoracolumbar laminectomy & fracture stabilization?
|
Foals with deep pain recognition or some voluntary movement of the hind limbs
|
|
|
What is a minimally invasive approach to dorsal spinous process impingment?
|
Endoscopic subtotal resection of processes and interspinous ligament
|
|
|
Where is the anatomical location of the supraspinous bursa?
|
Between the dorsal spinous processes of T2-5 and the nuchal ligament
|
|
|
What are the clinical signs of compressive sacral fracture?
|
Neurologic deficits related to manure and urine retention
|
|
|
What is the approach to surgical decompression of the sacrum?
|
Removal of spinous processes and dorsal laminae of sacrum
|
|
|
Recent approach to sacral fracture fixation in heifers:
|
reduction with strong distraction on dorsal spinous processes with repositioning forceps combined with transrectal pressure. Internal fixation with 4.5 LCP with 5.0 locking screws
|
|
|

|
|
|
|
|
|

|
|
|

|
|
|
How is intravertebral sagittal ratio calculated?
|
Dividing the minimal sagittal diameter of the vertebral canal by the height of the vertebral body
|
|
|
How is the minimal sagittal diameter of the vertebral canal obtained?
|
Narrowest diameter measured from the dorsal aspect of vertebral body to the ventral border of the dorsal laminae
|
|
|
How is the vertebral body width obtained?
|
Perpendicular to the vertebral canal at the widest point of the cranial aspect of the vertebral body
|
|
|
Normal intervertebral sagittal ratio:
|
>52% from C4-C6, >56% at C7 in horses >320 kg
|
|
|
What is intervertebral sagittal ratio?
|
Measurement from caudal aspect of dorsal lamina of the vertebral arch to the dorsocranial aspect of the body of the next caudal vertebra divided by the vertebral body width
|
|
|
Normal intervertebral sagittal ratio:
|
>0.485
|
|
|
Classifications of sagittal ratios:
|
low (<48% at C4-C6), moderate sagittal ration (48%-56%), high (>56%)
|
|
|
What is indicated with low sagittal ratio?
|
Perform myelogram to identify sites of cord compression and classify as static or dynamic
|
|
|
What is indicated with moderate sagittal ratio?
|
Perform myelogram to confirm or exclude CSM as a differential
|
|
|
What is indicated with high sagittal ratio?
|
No CSM
|
|
|
What factors are important for surgical success with cervical cord compression?
|
# of sites of compression, static or dynamic compression, severity of clinical signs, duration of clinical signs, temperament, age, and use of horse
|
|
|
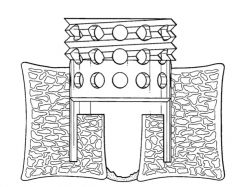
Approaches to ventral interbody fusion:
|
kerf cut cylinder, LCP
|
|
|
Complications of ventral interbody fusion:
|
seroma, infection, fractures of the adjacent vertebral body, ventral migration of implant, laryngeal hemiplegia, horner's syndrome, if fixed with LCP screws can migrate if there is a gap between plate and bone at fixation
|
|
|
Post-op care for ventral interbody fusion:
|
45 days stall rest, 45 days hand walking, reradiograph at 60 days, turn out for at least 6 months or until clinical signs resolve
|
|
|
How long can complete interbody fusion take?
|
Up to a year
|
|
|
When do clinical signs resolve after ventral interbody fusion?
|
Can take up to a year
|
|
|
Types of nerve injury:
|
type 1 (neuropraxia) is compression of myelin sheath or alteration in cell membrane function; type 2 (axonotmesis) is disruption of the axon and myelin sheath; type 3 (neurotnesis) is disruption of axon, myelin sheath, endoneurium; type 4 is disruption of axon, myelin sheath, endoneurium, perineurium; type 5 is disruption of axon, myelin sheath, endoneurium, perineurium, epineurium
|
|
|
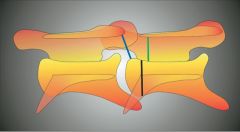
characteristics of CSM
|
flare of the caudal epiphysis of the vertebral body, abnormal ossification of the articular processes, subluxation between adjacent vertebrae, extension of the dorsal laminae, OA of articular processes
|
|
|
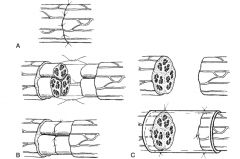
ways to define myelographic spinal cord compression:
|
50% or greater decrease in sagittal diameter of dorsal and ventral contrast columns or 20% reduction in dural diameter at C6-C7
|
|

|
|

