![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
131 Cards in this Set
- Front
- Back
|
Relation of The cricoid in the larynx:
|
most caudal, connected to the first tracheal ring by the cricotracheal membrane
|
|
|
Relation of the thyroid to the cricoid:
|
rostral, connected by the cricothyroid membrane
|
|
|
Relation of the arytenoid cartilages to the cricoid:
|
rostral, right and left arytenoid cartilages articulate with the cricoid at the cricoarytenoid joints
|
|
|
Relation of the arytenoid and thyroid cartilages:
|
arytenoid dorsal to the thyroid
|
|
|
Function of the cricoarytenoid joint:
|
allow the arytenoid cartilages to rotate dorsolaterally during abduction
|
|
|
Location of the cricoarytenoid articulation:
|
caudal aspect of the arytenoid
|
|
|
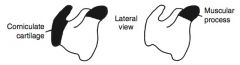
Cartilage composition of the laryngeal cartilages:
|
body of the arytenoid is composed of hyaline cartilage, as is the thyroid and cricoid cartilage. The corniculate processes of the arytenoid is composed of elastic cartilage, as is the epiglottis
|
|
|
Relation of the epiglottis in the larynx:
|
most rostral cartilage
|
|
|
Relation of the epiglottis to the thyroid cartilage:
|
epiglottis sits on the dorsal surface of the thyroid cartilage, connected by the thyroepiglottic ligament
|
|
|
Function of Intrinsic laryngeal muscles:
|
are responsible for movement of the cartilages in relation to each other, changes the diameter of the rima glottis, either by abducting or adducting the corniculate processes of the arytenoids or by increasing or decreasing tension placed on the vocal folds
|
|
|
Function of Extrinsic laryngeal muscles:
|
are responsible for movement or stabilization of the larynx as a whole unit
|
|
|
What are The vocal folds?
|
mucous membrane covered vocal ligaments
|
|
|
Location of vocal ligament:
|
extends from the ventral aspect of the arytenoid to the caudal body of the thyroid and the cricothyroid membrane
|
|
|
What are the Intrinsic laryngeal muscles?
|
cricoarytenoideus dorsalis, thyroarytenoideus, cricothyroideus, cricoarytenoideus lateralis, and the tranverse arytenoid
|
|
|
How does the transverse arytenoid differ from the other intrinsic laryngeal muscles?
|
It is the only non-paired (right & left)
|
|
|
What are the portions of the thyroarytenoideus?
|
rostral portion called the ventricularis, caudal portion called the vocalis muscle
|
|
|
What is the major abducting muscle?
|
cricoarytenoideus dorsalis
|
|
|
Function of the cricoarytenoideus dorsalis?
|
abduct the corniculate processes and tensing the vocal folds
|
|
|
What are the adducting muscles?
|
thyroarytenoideus, transverse arytenoid, and cricoarytenoideus lateralis
|
|
|
What is the function of the cricothyroideus?
|
tenses the vocal folds during vocalization
|
|
|
What is the innervation to the cricothyroideus?
|
external branch of the cranial laryngeal nerve, which is a branch of the vagus nerve
|
|
|
Innervation of cricoarytenoideus dorsalis:
|
recurrent laryngeal nerve, which is a branch of the vagus nerve
|
|
|
Innervation of thyroarytenoideus:
|
recurrent laryngeal nerve, which is a branch of the vagus nerve
|
|
|
Innervation of cricoarytenoideus lateralis:
|
recurrent laryngeal nerve, which is a branch of the vagus nerve
|
|
|
Innervation of tranverse arytenoid:
|
recurrent laryngeal nerve, which is a branch of the vagus nerve
|
|
|
What are the Extrinsic laryngeal muscles?
|
thyrohyoideus, hyoepiglotticus, cricopharyngeus, thyropharyngeus, and sternothyroideus
|
|
|
What is the aryepiglottic fold?
|
mucous membrane of the epiglottis reflects off the lateral, caudal aspect of the epiglottis to continue with the mucous membrane of the corniculate processes
|
|
|
Where is the laryngeal saccule?
|
between the medial wall of the thyroid cartilage and the lateral wall of the ventricle
|
|
|
What is the laryngeal ventricle?
|
broad band of tissue that extends from ventral aspect of the arytenoid cartilage to the caudal, lateral border of the epiglottis
|
|
|
Laryngeal arterial supply:
|
caudal laryngeal artery and branches of the ascending pharyngeal artery
|
|
|
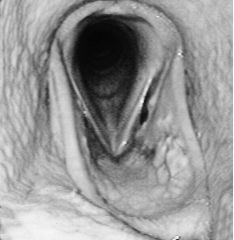
What is Recurrent laryngeal neuropathy?
|
progressive loss of large myelinated axons in the left recurrent laryngeal nerve, resulting in neurogenic atrophy of the intrinsic laryngeal muscles. Paralysis of the cricoarytenoid dorsalis causes loss of abduction, there is increase in the negative inspiratory pressure, reducing the size of the rima glottis
|
|
|
Grade 1 laryngeal movement:
|
all arytenoid movement synchronous and symmetrical, and full abduction of the corniculate process can be achieved and maintained
|
|
|
Grade 2A laryngeal movement:
|
transient asynchrony, flutter, or delay in movements
|
|
|
Grade 2B:
|
asymmetry of the rima glottis most of the time because of reduced mobility of the arytenoid or vocal fold, but with after swallowing or nasal occlusion, full abduction is seen and maintained
|
|
|
Grade 3A laryngeal movement:
|
asymmetry of the rima glottis most of the time because of reduced mobility of the cartilage but occasionally after swallowing or nasal occlusion, full symmetrical abduction is achieved but can not be maintained
|
|
|
Grade 3B:
|
abductor muscle deficit and cartilage asymmetry and full abduction is never achieved
|
|
|
Grade 3C:
|
marked but not total abductor muscle deficit and cartilage asymmetry with little cartilage movement and full abduction is never achieved
|
|
|
Grade 4:
|
complete immobility of the cartilage and vocal fold
|
|
|
Surgical options for RLN:
|
prosthetic laryngoplasty, ventriculectomy, ventriculocordectomy, reinnervation of the CAD muscle, and partial arytenoidectomy
|
|
|
What can be performed in conjuction with PL or reinnervation:
|
VE and VCE
|
|
|
Why are VE and VCE performed with PL or reinnervation?
|
reduce noise and scar formation may improve airflow mechanics
|
|
|
When is Partial arytenoidectomy performed?
|
congenital malformation of the cartilages, when PL has failed and there is fracture of the cartilage, arytenoid chondropathy
|
|
|
Goal of PL:
|
suture is used as a prosthesis between the cricoid and arytenoid cartilages, to have some degree of permanent abduction of the arytenoid
|
|
|
Describe PL:
|
10-12 cm incision is made ventral to the linguofacial vein starting 4 cm rostral to the ramus of the mandible. The vein is separated from the omohyoideus muscle, and with retraction of the vein, a plane is evident between the sternocephalicus and cricothyroideus muscles, which is digitally opened. The thyropharyngeus and cricopharyngeus muscles are separated from each other to allow better exposure of the muscular process of the arytenoid. Suture needle is walked off the caudal dorsolateral aspect of the cricoid and the suture is passed in a cranial direction. Suture ends are drawn rostrally under the cricopharngeus muscle and a second suture is placed 1 cm lateral to the first. Suture is passed through the muscular process in a caudomedial to craniolateral direction, with the second suture placed 5 cm more caudal than the first. Suture is tied, leaving 1.5-2cm tails.
|
|
|
What procedure can prevent loss of abduction post- PL?
|
tendon of insertion of the CAD can be cut and the cricoarytenoid articulation can be opened and curetted to facilitate ankylosis of the joint
|
|
|
When is the tendon of insertion of the CAD cut and the CAJ opened during PL?
|
Prior to placement of suture in the muscular process of the arytenoid
|
|
|
What degree of abduction should be the end result of PL?
|
approximately 88% of the maximal rima glottis area for adequate airflow
|
|
|
When does training resume after PL?
|
approximately 45 days post-operatively
|
|
|
Intra-operative complications of PL:
|
hemorrhage, needle break, perforation of the mucosa, and suture cut through
|
|
|
When is perforation of the mucosa during PL most likely to occur?
|
placing the suture in the cricoid cartilage
|
|
|
Post-operative complications of PL:
|
seroma, wound infection, dehiscence, dysphagia, coughing, suture infection and contamination of the lower airway resulting in lower airway disease
|
|
|
What is initial coughing and dysphagia after PL a result of?
|
excessive abduction or inflammation from retraction on the cricopharyngeus and thyropharyngeus
|
|
|
What is the cause of chronic pharyngeal dysfunction after PL?
|
may be due to surgical trauma to nerves or overabduction of the cartilage
|
|
|
When should infected PL suture be removed?
|
delayed until at least 4 months after the initial surgery to prevent failure of arytenoid abduction
|
|
|
When is repeat PL indicated?
|
overabduction or loss/ failure of abduction
|
|
|
Complications of repeat PL:
|
Formation of dense scar tissue makes visualization difficult and transection of scar tissue causes hemorrhage
|
|
|
Prognosis after PL:
|
50-70% in racehorses and higher in non-racehorses
|
|
|
What is Ventriculectomy (VE)?
|
removal of the mucosal lining of the ventricle/ saccule to help reduce noise and potentially airflow
|
|
|
Approaches of VE:
|
laryngotomy approach in either dorsal recumbency after PL or standing
|
|
|
Describe VE:
|
laryngotomy is performed, a burr is introduced into the saccule, engaging the mucosa, then everted. The everted saccule is clamped prior to transection with metzenbaum scissors
|
|
|
What is VCE?
|
removal of the ventricle and the leading edge of the vocal fold
|
|
|
Indications for VCE:
|
sport horses with primary complaint of respiratory noise, with racehorses with grade 3 laryngeal movement caused by vocal fold collapse during exercise, or racehorses that have had PL but have performance limiting issues related to vocal fold collapse
|
|
|
Approaches to VCE:
|
laryngotomy approach or through nasal endoscopic laser assisted approach
|
|
|
Describe VCE:
|
With laryngoplasty approach, after eversion and removal of the saccule, a 2 cm by 2-3 cm cresent shaped wedge of tissue is removed from the leading edge of the vocal fold. Mucosal edeges are sutured.
|
|
|
What is the benefit of suturing the mucosal edges in VCE?
|
decrease hemorrhage, decrease formation of cicatrix, and result in smoother airway surface
|
|
|
Describe Laryngotomy:
|
incision is made on ventral midline from just rostral to the thyroid cartilage to just caudal to the cricoid cartilage. The sternothyroideus muscle is separated, and loose adventitia over the larynx is bluntly separated. The cricothyroid membrane is incised
|
|
|
What can improve exposure with laryngotomy?
|
cricoid and/ or thyroid can be split
|
|
|
Ideal candidates for laryngeal reinnervation:
|
younger horses with grade 3 movement, or those in which performance is not necessary within a year of surgery
|
|
|
Source of reinnervation graft:
|
first cervical nerve and the omohyoideus muscle
|
|
|
Benefit of 1st cervical nerve and omohyoideus for reinnervation graft:
|
muscle and nerve are active during inspiration
|
|
|
Describe reinnervation:
|
laryngotomy, first cervical nerve is identified and followed to insertion in the omohyoideus. Dorsal, surface branches of the nerve are used, and 3 mm grafts are created with tenotomy scissors. Longitudinal separation of fibers in the CAD are made with vascular forceps to create pockets for the grafts. The graft is sutured to the pocket, mainly at the junction of the dorsal and lateral muscle bellies at the caudal aspect of the muscle
|
|
|
When does training resume after reinnervation?
|
rested for 16 weeks then return to training for 6 weeks before assessment
|
|
|
Reflexes used to determine function after reinnervation:
|
stretching the head and neck to an elevated position and observing a flicker or a single abduction, applying sudden pressure on the commissure of the mouth and observing an abduction
|
|
|
What stabilizes The vocal fold?
|
contraction of the cricothyroideus
|
|
|
Treatment of Axial deviation of the vocal fold:
|
bilateral VCE
|
|
|
Treatment of Bilateral laryngeal paralysis:
|
aimed at the underlying disease, but in unresponsive cases a unilateral PL can be performed as a salvage procedure in non-performance horses or trachestomy can be considered in horses that need to have some athletic capabilities
|
|
|
Portions of larynx derived embryologically from the 4th branchial arch:
|
Lateral wings of the thyroid, cricoarytenoid articulation, crcithyroideus, thyropharyngeus, and cricopharyngeus muscles
|
|
|
What is the side predilection for 4BAD?
|
Right side is more commonly affected than the left and bilateral involvement is more common than left sided disease
|
|
|
What palpable abnormalities occur with 4BAD?
|
thyroid wing is absent or decreased in size, and there is a gap between the cricoid and thyroid cartilage because there is absence or atrophy of the cricothyroideus muscle
|
|
|
What is often observed endoscopically with 4BAD?
|
rostral displacement of the palatopharyngeal arch, where the caudal pharynx is displaced rostral to the dorsal aspect of the corniculate processes
|
|
|
Treatment for Axial deviation of the aryepiglottic folds:
|
transendoscopy laser transection or laryngotomy resection of a 2 cm section of tissue that is collapsing into the airway
|
|
|
What is Arytenoid chondropathy?
|
abnormal enlargement in 1 or 2 arytenoid cartilages, usually due to mucosal injury and subsequent infection, but may be multifactorial
|
|
|
Why is abduction restricted with ACC?
|
lateral position of the thyroid cartilage and inflammation in the CAJ and/ or CAD
|
|
|
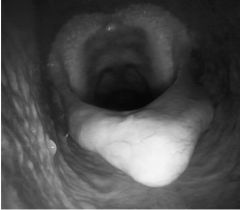
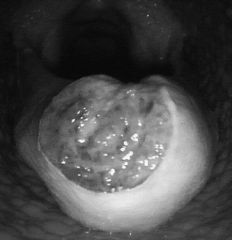
Endoscopy signs of ACC:
|
granulation tissue, fistulas or sinus tracts, and ulceration or granulation opposite to the original granulation lesion
|
|
|
Types of arytenoidectomy:
|
Subtotal arytenoidectomy removes all of the cartilage except for the muscular process and the corniculate process. Partial arytenoidectomy is removal of all of the arytenoid except for the muscular process
|
|
|
Which type of arytenoidectomy is preferred and why?
|
Partial is preferred because subtotal has been shown to not improve upper airway function
|
|
|
What approach to arytenoidectomy should be taken with bilateral ACC?
|
worst side is removed with partial arytenoidectomy
|
|
|
When is Bilateral arytenoidectomy performed?
|
salvage procedure.
|
|
|
Describe partial arytenoidectomy:
|
laryngotomy, U shaped incision is made on the axial surface of the arytenoid and the mucosa is undermined off of the cartilage. The cartilage is elevated and transected with Mayo scissors or a scalpel.
|
|
|
What is a modified partial arytenoidectomy approach?
|
removal of the portion of the arytenoid in 2 pieces with its overlying mucosa. The defect is closed by suturing the remaining mucosa and the aryepiglottic fold
|
|
|
Benefits of modified partial arytenoidectomy?
|
easier dissection, shorter surgery time, reduces soft tissue in the airway, and is equal in post-operative complications and airflow mechanics achieved with the traditional approach
|
|
|
Complications of partial arytenoidectomy:
|
Dyspnea and dysphagia are the most common, Intraluminal granulation and advanced mineralization of the cartilages
|
|
|
Disorders of the epiglottis:
|
entrapment in the aryepiglottic fold, acute epiglottitis, subepiglottic cyst or granulomas, dorsal epiglottic abscesses, hypoplasia, and retroversion
|
|
|
When does Epiglottic entrapment occur?
|
loose subepiglottic tissue becomes displaced dorsal to the soft palate
|
|
|
What is associated with epiglottic entrapment?
|
entrapment is persistent, and usually the tissue is thickened. Epiglottic entrapment may be associated with epiglottic hypoplasia
|
|
|
Treatment options for EE:
|
transnasal endoscopic guided laser, bistoury, or electrocautery axial resection of the membrane, bistoury transection through an oral approach or excision through a laryngotomy or pharyngotomy
|
|
|
Recurrence rate Laser assisted EE transection:
|
4-10%
|
|
|
Complications Laser assisted EE transection:
|
thermal trauma to the epiglottis
|
|
|
recurrence rate bistoury EE transection:
|
5-15%
|
|
|
Complications bistoury EE transection:
|
laceration of the soft palate, epiglottis, or pharynx
|
|
|
Recurrence rate Transnasal endoscopic guided electrosurgical EE transection:
|
40%
|
|
|
When is laryngotomy EE transection used?
|
reserved for very thickened, ulcerated, and fibrotic appearing entrapments
|
|
|
Possible sequella of relief of epiglottic entrapment, regardless of surgical approach taken:
|
DDSP
|
|
|
Endoscopic appearance of acute epiglottitis:
|
thickened, reddened, edematous mucous membrane of the epiglottis
|
|
|
Origin of Subepiglottic cysts:
|
submucosal in origin
|
|
|
Histology of subepiglottic cysts:
|
stratisfield and pseudostratisfied columnar epithelium with mucous glands, ducts, and eosinophilic mucous
|
|
|
Treatment options for subepiglottic cysts:
|
removed through a laryngotomy approach, transorally using a laser or a cyst snare, and transnasally using laser or electrosurgery. A single report of cyst injection of 10% formalin resulting in resolution.
|
|
|
When is transnasal approach to subepiglottic cyst chosen?
|
small cysts that are easily manipulated
|
|
|
Location of Subepiglottic granulomas:
|
form on the ventral aspect of the epiglottis
|
|
|
Cause of subepiglottic granulomas:
|
inflammation and ulceration of the aryepiglottic fold
|
|
|
What is the most important aspect of treating subepiglottic granulomas?
|
extended periods of rest are mandatory
|
|
|
Treatment of Epiglottic hypoplasia:
|
epiglottic augmentation, submucosal injection of polytetrafluoroethylene (Teflon)
|
|
|
How does Augmentation affect the epiglottis?
|
increased thickness but not increased length
|
|
|
What is the cause of Epiglottic retroversion?
|
Trauma or inflammation of the geniohyoid or hypoglossal nerves
|
|
|
Treatment options for epiglottic retroversion?
|
attempts have been with epiglottic augmentation, placement of a prosthetic suture between the epiglottis and thyroid cartilage
|
|

|
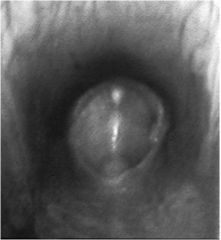
vocal fold collapse
|
|

|
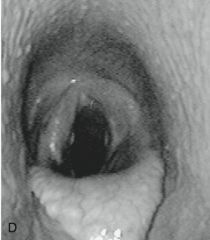
rostral displacement of palatopharyngeal arch in 4bad
|
|

|
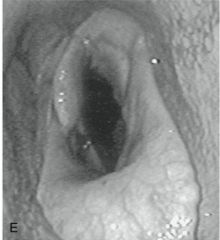
axial deviation of aryepiglottic folds
|
|

|
after resection of aryepiglottic folds
|
|

|
arytenoid chondritis
|
|

|
arytenoid chondritis
|
|
|
left = subtotal right = partial
|
|
|
epiglottic entrapment
|
|

|
epiglottic entrapment
|
|
|
ulcerated epiglottic entrapment
|
|
|
epiglottic hypoplasia
|
|
|
epiglottic retroversion
|
|

|
grade 4 RLN
|
|
|
moderate abduction (grade 2) after prosthetic laryngoplasty
|
|
|
excessive abduction (grade 1) after prosthetic laryngoplasty
|
|

|
exercise videoendoscopy grade 4 RLN with vocal fold collapse
|

