![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
61 Cards in this Set
- Front
- Back
|
What is the rectal ampulla?
|
retroperitoneal rectum forming dilation
|
|
|
Muscular content of the anus:
|
composed of the internal and external anal sphincters. The internal sphincter is smooth muscle and the external sphincter has striated muscle.
|
|
|
Function of levator ani muscle:
|
overcomes anal prolapse during defecation
|
|
|
Origin & insertion of the levator ani muscle:
|
originats from the ischiatic spine and sacrotuber ligaments and inserts under the external sphincter
|
|
|
How are most rectal tears created?
|
rectal wall contracts around the examiners hand or forearm, enemas, meconium extraction with forceps, sadism, dystocia, parturition, animal bites, chronic impaction at stricture, misdirection of the stallion’s penis, rectal thrombosis, or sand impactions
|
|
|
Grades of rectal tears:
|
Grade 1 tears involved only the mucosa and submucosa. Grade 2 tears involved only the muscle, causing the mucosa/ submucosa to prolapse through the muscle defect, creating a pocket for fecal impaction. Grade 3a tears involve the mucosa, submucosa, and muscular layers but do not involve the serosa, 3b tears are similar expect that they do not involve the mesorectum or retroperitoneal tissue. Grade 4 tears involve all layers with gross contamination of the peritoneal cavity.
|
|
|
Where do most tears occur?
|
dorsally and parallel to the long axis, however idiopathic tears tend to be oriented in a transverse direction
|
|
|
What cause of rectal tears affects the size of the tear?
|
Dystocia
|
|
|
Initial treatment of rectal tears:
|
reducing the activity of the rectum, gentle removal of feces, treatment for shock and peritonitis, epidural analgesia, and rectal packing, anus is closed with towel clamps or a purse string.
|
|
|
When are bypass procedures used with rectal tears?
|
grade 3 and 4 tears
|
|
|
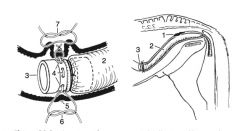
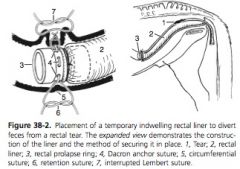
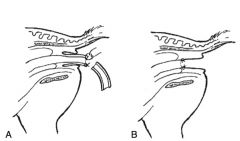
Describe placement of temporary indwelling rectal liner:
|
prolapse ring with Dacron loop lacing around the outer circumference , rectal sleeve or arthroscopy sleeve is glued to the ring, in dorsal recumbency the liner is passed through the rectum until the surgeon can manipulate the ring and liner through a ventral midline celiotomy, past the tear. First a circumferential suture is placed around the small colon, fitting into the groove of the rectal prolapse ring, using 3 gut. Retention sutures are then placed on the dorsal, ventral, medial, and lateral aspects of the small colon, incorporating the circumferential suture, all layers of the rectum, and the Dacron loop. The circumferential suture and the retention suture is then covered by apposing the serosal surface using a Lembert pattern
|
|
|
How is a temporary indwelling rectal liner removed?
|
circumferential suture will cut through the rectal wall and the liner will pass in 9-12 days
|
|
|
Complications of temporary indwelling rectal liners:
|
sleeve tears or retraction and formation of a rectoperitoneal fistula
|
|
|
Types of colostomy techniques:
|
loop colostomy and end colostomy
|
|
|
Why is loop colostomy preferred over end colostomy?
|
easiest, quickest to create and reverse, and does not have concern for incomplete diversion of feces
|
|
|
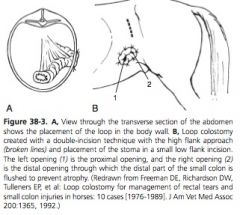
Approaches to loop colostomy:
|
single incision or double incision technique
|
|
|
How do single and double incision loop colostomy techniques differ?
|
Single incision techniques use the exploratory incision for stoma placement and double incision technique has separate incisions for the exploration and the stoma placement
|
|
|
What are the disadvantages of the single incision loop colostomy?
|
colostomy is at closure weakens the closure and increases risk of prolapse or herniation
|
|
|
What are the approaches to single incision loop colostomy?
|
High flank approach with high flank stoma placement, low flank approach with low flank stoma placement, and ventral midline approach with ventral midline stoma placement
|
|
|
What are the advantages of single incision high flank loop colostomy?
|
Can be done standing
|
|
|
What are the disadvantages of single incision high flank loop colostomy?
|
Can’t explore abdomen or empty colon, fecal soiling of incision & skin
|
|
|
What are the disadvantages of a single incision low flank loop colostomy?
|
Can’t do standing, can’t explore abdomen or empty colon, risk of prolapse & herniation
|
|
|
What are the advantages of single incision VMC for loop colostomy?
|
Can explore abdomen and empty colon
|
|
|
What are the disadvantages of single incision VMC for loop colostomy?
|
GA, prolapse, herniation
|
|
|
Disadvantages of performing the colostomy under general anesthesia:
|
include difficulty placing the stoma because of recumbency, additional expense of inhaled anesthesia compared with standing, and risk of stoma dehiscence during recovery
|
|
|
What are the approaches to double incision loop colostomy?
|
High flank approach with low flank stoma placement, ventral midine approach with low flank stoma placement
|
|
|
What is the advantage of a double incision high flank/ low flank loop colostomy?
|
Can be done standing
|
|
|
What are the disadvantages of a double incision high flank/ low flank loop colostomy?
|
Can’t explore abdomen or empty colon, construction is difficult
|
|
|
What are the advantages of a double incision VMC/ low flank loop colostomy?
|
Can explore abdomen and empty colon
|
|
|
What are the disadvantages of a double incision VMC/ low flank loop colostomy?
|
GA, construction is difficult
|
|
|
Where is the low flank incision made?
|
between the flank fold and the costal arch, angled dorsally about 20-30 degrees
|
|
|
What location in the small colon is used for the stoma?
|
1 meter oral to the rectum
|
|
|
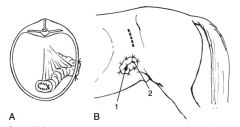
Describe loop colostomy:
|
small colon is folded into a loop and the loop arms are sutured together with a lambert pattern ½ way between the mesenteric and antimesenteric teniae for 8 to 10 cm. The loop is inserted into the flank incision with the proximal loop located more ventral to the distal loop and the antimesenteric teniae exposed beyond the skin edge by 3 cm. The seromuscular layer is sutured to the abdominal muscles with interrupted sutures. An 8 cm incision is made through the tenia to created the stoma, the edges are everted and sutured to the skin edges in a simple, interrupted pattern using nylon or polypropylene. An alternative is to suture the colon loop directly to the skin. At 14 days the loop is detached and oversewn at the stoma
|
|
|
Why are end colostomies chosen?
|
some felt there was not complete fecal diversion with loop colostomies
|
|
|
Describe end colostomy:
|
stoma is created by transecting the small colon, closing the aboral segment with Parker-Kerr method. Oral segment is passed through incision, the mucosa is cuffed by suturing it to the serosa, then attached to the skin
|
|
|
Disadvantage of the end colostomy:
|
aboral segment will atrophy which makes the reversal more difficult and predisposes to anastomosis impaction or dehiscence
|
|
|
How is atrophy of the aboral portion of the loop colostomy prevented?
|
flushed daily with 20L of warm water
|
|
|
Why is flushing the aboral segment of the loop colostomy better than infusing luminal nutrients?
|
nutrients effect only the mucosa with no effects on stretching or exercising the muscle
|
|
|
When is the colostomy reversed?
|
at least 6 weeks post-operatively
|
|
|
Complications of colostomy:
|
dehiscence, abscessation, peristomal hernia, prolapse with or without mesenteric vessel rupture, infarction, colostomy rupture, stoma obstruction or closure reversal complications
|
|
|
When is liner placement selected?
|
small tears
|
|
|
When is colostomy considered?
|
large tears
|
|
|
How do liner placement and colostomy compare?
|
colostomy is more expensive, is a staged procedure, and has more life threatening risks, however there is better deviation of fecal material and comparable success rates to liners
|
|
|
How is suture repair performed?
|
Suture repair can be undertaken by prolapsing grade 4 tears through the anus, accessing grade 4 tears through a VMC, or non-visual standing technique
|
|
|
What can improve access when performing primary suture repair with rectal tears?
|
Long handle instruments with pistol grips and rectal speculums are available to easy suturing. Cutting the anal sphincter and improve access and the resulting wound can be partially closure after repair of the tear or can be left open to heal by second intention
|
|
|
When should primary suture repair be selected?
|
best for grade 3 tears that are half or less of the rectal circumference or for grade 4 tears with very small serosal perforation only
|
|
|
What qualities should suture have in repairing rectal tears?
|
Suture should be long, have little memory, and resist stretch and fecal digestion
|
|
|
What rectal tears can be managed with nonsurgical management?
|
grade 1 and 2 tears and maybe suitable for grade 3 tears
|
|
|
Complications related to rectal tears:
|
stricture, diverticulum, perirectal abscess formation, mucosal or submucosal herniation, or rectoperitoneal fistula
|
|
|
Survival rates for rectal tears:
|
excellent for grade 1 and 2 tears, good to fair for horses with grade 3 tears and poor for horses with grade 4 tears (Claes’ paper, survival rate 100% for horses with grade 1 and 2 tears, 38% for grade 3 tears, and 2% for grade 4 tears)
|
|
|
Rectal prolapse causes:
|
straining due to diarrhea, dystocia, parasitism, colic, proctitis, tumor, or foreign body
|
|
|
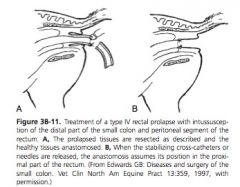
Types of rectal prolapse:
|
Type 1 prolapse involves the mucosa and submucosa, type 2 is a full thickness prolapse with all or a portion of the rectal ampulla. A type 3 prolapse is a type 2 plus in addition to small colon intussusception into the rectum. With a type 4 prolapse the peritoneal portion of the rectum as well as the small colon form an intussusception through the anus
|
|
|
How are type 1 and 2 rectal prolapse treated?
|
educe edema with glycerin, sugar, MgSO4, lidocaine, or a mixture, Epidural anesthesia reduces straining. Purse string is performed to prevent recurrence
|
|
|
How are type 3 and 4 prolapse treated?
|
manual reduction, submucosal resection, or resection and anastomosis
|
|
|
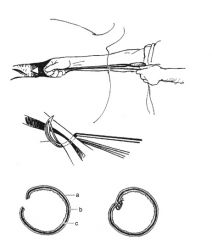
Describe submucosal resection of rectal prolapse:
|
2- 6 inch spinal needles or IV catheters are placed at right angles to each other through the external anal sphincter and healthy mucosa to keep the prolapse in place during the dissection. Circumferential incision through healthy mucosa is made in healthy tissues cranial and caudal to the tissue to be resected. after the circumferential incision is made, a longitudinal incision is made to connect the 2 circumferential incisions, and then the abnormal tissue is resected away circumferentially, in 1/3 segments. Mucosa and submucosa is apposed in an interrupted pattern. Once all the abnormal tissue is removed the mucosa is apposed
|
|
|
When is submuscosal resection of rectal prolapse performed?
|
prolapse is devitalized, the prolapse recurs with medical management, or the horse continues to strain
|
|
|
Described rectal prolapse RA:
|
Instead of partial thickness circumferential incisions, full thickness incisions are made, again in 1/3 segments. The exposed healthy tissues are first apposed in a full thickness interrupted horizontal pattern, again in 1/3 segments, until all necrotic tissue is removed. Mucosa is then apposed
|
|
|

|
|
|
|
|
|
|
|
|
|

