![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
70 Cards in this Set
- Front
- Back
|
Capacity of the stomach:
|
5 to 15L
|
|
|
Stomach location:
|
left side of the abdomen with the pyloric region just to the right of midline
|
|
|
Most caudal portion of stomach:
|
fundus, at the level of the 14th and 15th ICS
|
|
|
Regions of the stomach:
|
cardia, fundus, body, and pylorus
|
|
|
Stomach attachments:
|
Cardia portion attached to diaphragm by gastrophrenic ligament; greater omentum attaches to greater curvature; hepatogastric and hepatoduodenal ligaments (lesser omentum), connecting the stomach and the duodenum to the liver
|
|
|
What is the gastrophrenic ligament a continuation of?
|
phrenicosplenic ligament and gastrosplenic ligament
|
|
|
What is the greater omentum contiguous with?
|
gastrophrenic ligament
|
|
|
What does the greater omentum form?
|
blind potential space called omental bursa
|
|
|
Opening of omental bursa:
|
epiploic foramen
|
|
|
Borders of epiploic foramen:
|
between caudate process of the liver & right lobe of the pancreas, caudal vena cava (dorsal) and portal vein (ventral.)
|
|
|
Blood supply to stomach:
|
celiac artery
|
|
|
Venous drainage from stomach:
|
gastric veins to portal vein
|
|
|
Regions of the stomach based on mucosal lining:
|
from oral to aboral, nonglandular stratisfied squamous epithelium, cardiac epithelium, proper gastric (glandular) mucosa, and pyloric mucosa
|
|
|
Cells of proper glandular mucosa:
|
parietal, zymogen, enterochromaffin-like
|
|
|
Product of parietal cells:
|
hypochloric acid (HCl)
|
|
|
Product of zymogen cells:
|
pepsinogen
|
|
|
Product of enterochromaffin-like cells:
|
histamine
|
|
|
Function of histamine:
|
amplifies secretion of HCl by parietal cells
|
|
|
Function of pepsinogen:
|
converted to pepsin, break down protein
|
|
|
Cells of pyloric mucosal region:
|
G & D cells
|
|
|
Products of G cells:
|
gastrin
|
|
|
Products of D cells:
|
somatostatin
|
|
|
Function of gastrin:
|
increased gastric acid secretion
|
|
|
Function of somatostatin:
|
decreased gastric acid secretion
|
|
|
Protective mechanisms of proper gastric mucosa:
|
high transepithelial electrical resistance, secretion of mucus and HCO3, and Na/H exchangers
|
|
|
What is transepithelial resistence?
|
Measure of ion permeability, high resistance indicates impermeability of ions
|
|
|
How is gastric mucosa healed?
|
Superficial ulcer repair by epithelial restitution; deeper ulceration healed by granulation tissue, proliferation of epithelium from wound edges, budding and migration of gastric glands, facilitated by a mucoid cap
|
|
|
Function of mucoid cap:
|
retains healing factors and maintains a neutral pH
|
|
|
What is epitheliam restitution?
|
epithelial cells migrate to cover defect
|
|
|
Normal barium transport in the stomach:
|
reaches the small intestine in 10 minutes and is cleared in 35 minutes
|
|
|
How is gastric emptying measured?
|
nuclear scintigraphy, acetaminophen absorption, or breath testing after administration of C-octanoic acid
|
|
|
What region does neonatal ulcers affect?
|
glandular mucosa
|
|
|
How do weanling and adult ulcers differ?
|
affect the squamous epithelium at the margo plicatus, but weanling associated with diarrhea and not in adults
|
|
|
Causes of gastric rupture:
|
primary, due to gastric impaction or unknown cause, or secondary to aboral obstruction
|
|
|
Most common site of gastric rupture:
|
greater curvature
|
|
|
Most common form of gastric neoplasia:
|
SCC
|
|
|
Most common location of gastric neoplasia:
|
cardia
|
|
|
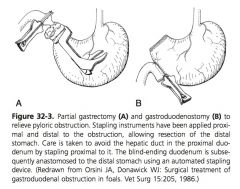
Cause of gastric outflow obstruction:
|
pyloric stenosis caused by congenital hypertrophy or pyloric mass development
|
|
|
When is surgery indicated for gastric outflow obstruction?
|
medical management is not successful in a short period of time
|
|
|
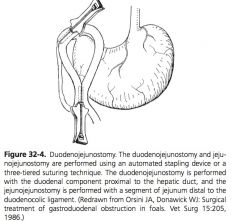
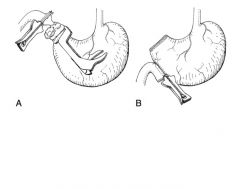
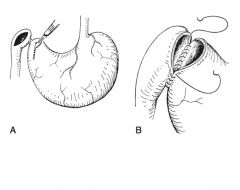
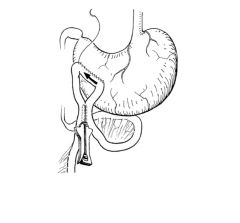
Surgical approaches to gastric outflow obstruction:
|
gastrojejunostomy, gastroduodenostomy, duodenojejunostomy with jejunojejunostomy, or gastrojejunostomy with jejunojejunostomy
|
|
|
Why is jejunojejunostomy is performed with gastrojejunostomy or duodenojejunostomy?
|
allow outflow from the proximal small intestine
|
|
|
How is the jejunum is aligned for gastrojejunostomy ?
|
left to right (oral to aboral) along the caudal ventral aspect of the stomach
|
|
|
How are anastomoses created for pyloric bypass?
|
stapling devices, which can be difficult to maneuver in foals, or hand sewn in 2 to 3 layers
|
|
|
Complications of pyloric bypass?
|
duodenal obstruction, duodenal adhesions, and ileus
|
|
|
Spleen location:
|
left mid-dorsal abdomen, Base is most dorsal and extends past 18th rib into the paralumbar fossa, Apex is most ventral and located near costochondral junctions of the 9-11th ribs
|
|
|
Parietal surface of spleen contacts:
|
diaphragm
|
|
|
Visceral surface of spleen contacts:
|
Cranial to hilus the spleen contacts the stomach, caudal to the hilus the spleen contacts colon and small intestine
|
|
|
What suspends the spleen from the dorsal abdomen?
|
nephrosplenic ligaments, composed of phrenicosplenic and renosplenic ligaments
|
|
|
Spleen attachment to stomach:
|
gastrosplenic ligament
|
|
|
Arterial supply to the spleen:
|
splenic artery, branch of the celiac artery
|
|
|
Spleen innervation:
|
celiac plexus, which has both sympathetic and parasympathetic supply, major splanchnic nerve, and parasympathetic input from the vagus nerve
|
|
|
Splenic tissue organization:
|
red pulp and white pulp
|
|
|
Red pulp:
|
arterial capillaries, small venules, and reticulum housing macrophages and blood
|
|
|
White pulp:
|
lympathic tissue organized as lymphatic nodules
|
|
|
Splenic reticulum:
|
lymphocytes and macrophages supported by a scaffolding of extracellular fibers
|
|
|
Splenic functions:
|
storage of RBC & platelets, removal of aged or damaged RBC & platelets, fetal hematopoiesis, Fe recycling, and immunologic functions
|
|
|
Immunologic function of spleen:
|
production of IgM, homing of B cells, and reservoir for immunocompetent lymphocytes
|
|
|
Indications for splenectomy:
|
research, splenomegaly with or without splenic infarction or thrombosis, splenic rupture, or primary tumors without metastases
|
|
|
Primary splenic neoplasia:
|
Lymphosarcoma, metastatic melanoma, and hemangiosarcoma
|
|
|
When does splenic thrombosis or infarction occur?
|
when the spleen is enlarged
|
|
|
Where does splenic rupture occurs?
|
visceral surface
|
|
|
Splenectomy approaches:
|
Original descriptions are through paralumbar fossa, currently described are in the 17th ICS or with resection of either the 16, 17, 18th rib, or the distal aspect of all 3
|
|
|
Why is splenectomy not performed through paralumbar fossa approach?
|
difficulty accessing the base & primary vessels
|
|
|
What complications are associated with splenectomy approaches involving the 16th or 17th rib?
|
opening the plueral cavity due to proximity to the diaphragmatic line of plueral reflection
|
|
|
Describe splenectomy through 17th rib resection:
|
RLR, incision made over 17th rib, periostium elevated circumferentially, rib transected proximally, disarticulated distally at costochondral junction, dorsal spleen elevated from incision, nephrosplenic ligament transected, vessels triple ligated, remainder of ligamentous structures transected near hilus, ligation of short gastric vessels, separated from greater omentum
|
|
|
Complications of splenectomy:
|
hemorrhage, incisional complications, and complications associated with penetration of the plueral cavity
|
|
|
|
|
|
|
|
|

|
|
|

|

