![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
72 Cards in this Set
- Front
- Back
|
2 basic types of grafts:
|
pedicle grafts, free grafts
|
|
|
Pedicle graft:
|
remains connected to the donor site, permanently or temporarily, to sustain the graft and ensure viability
|
|
|
Free graft:
|
skin that has been removed from its blood suplly and transferred to another site and must establish new vascular connections to ensure viability
|
|
|
Types of free grafts:
|
autografts, allografts or xenografts
|
|
|
Autografts:
|
grafts taken from the same individual
|
|
|
Allografts:
|
grafts taken from a different individual of the same species
|
|
|
Xenograft:
|
graft taken from a different individual of a different species
|
|
|
Categories of free skin grafts:
|
Full thickness, partial thickness
|
|
|
Full thickness free skin grafts:
|
include the epidermis and all of the dermis
|
|
|
Partial thickness free skin grafts:
|
epidermis and a variable portion of the dermis
|
|
|
What effect does the amount of dermis in the graft affect?
|
acceptance, durability, and cosmesis at the recipient site
|
|
|
What effect does thicker dermis have?
|
durability and cosmetic appearance but decreases survivability
|
|
|
How are free skin grafts applied?
|
sheets or islands
|
|
|
Types of sheet grafts:
|
solid or meshed
|
|
|
Types of island grafts:
|
pinch, punch, or tunnel grafts
|
|
|
Requirements for a graft acceptance:
|
recipient bed should be vascular and not be infected or devitalized
|
|
|
Phases of graft acceptance:
|
adherence, serum imbibition, and revascularization
|
|
|
How does initial adherence of the graft to the recipient bed occur?
|
by fibrin
|
|
|
How does firm adherence of the graft occur?
|
fibroblast and vessel invasion
|
|
|
What provides nourishment to the graft?
|
Plasmatic imbibition or plasmatic circulation
|
|
|
What is plasmatic imbibition?
|
Plasma-like fluid is taken up into open vessels by capillary action.
|
|
|
When does revascularization begin?
|
about 48 hours
|
|
|
How does revascularization occur?
|
Inosculation, neovascularization, vascular bridging
|
|
|
Inosculation:
|
generation of new capillaries by the anastomosis of existing vessels in the recipient bed to those in the graft
|
|
|
Neovascularization:
|
invasion of new vessels in the recipient bed to existing vessels in the graft
|
|
|
Vascular bridging:
|
Vessels in the recipient bed adjacent to the avascular portion bridge the avascular portion to enter the graft overly it
|
|
|
What occurs after the graft is accepted?
|
undergoes organization and contraction
|
|
|
What occurs during organization?
|
epidermis either becomes hyperplastic to double in thickness or it may slough, exposing the underlying dermis
|
|
|
When does pigmentation occurs?
|
approximately 4 weeks after grafting for split thickness grafts
|
|
|
When does hair appears?
|
4 to 6 weeks
|
|
|
When does reinnervation occur?
|
should appear by 7-9 weeks post grafting but may occur earlier
|
|
|
Primary contraction:
|
occurs when the graft is harvested because of recoil of the elastic fibers in the dermal layers
|
|
|
Reasons for grafts failure:
|
fluid accumulation, movement or infection
|
|
|
What occurs with fluid accumulation?
|
prevents fibrin from attaching the graft to the recipient bed and prevents ingrowth of vessels
|
|
|
When does infection generally results?
|
surface of the wound has greater than 10^5 bacteria per gram of tissue but pathogenic bacteria may cause graft failure with smaller numbers
|
|
|
Common pathologic wound bacteria:
|
Beta hemolytic streptococci and pseudomonas species
|
|
|
Detrimental effects of pathologic wound bacteria:
|
Beta-strep release proteolytic enzymes, such as streptokinase or staphylokinase, and pseudomonas produce elastases
|
|
|
What is preparation of the recipient site is aimed at?
|
improving vascularity and decreasing bacterial contamination
|
|
|
How can vascularity be improved in the recipient bed?
|
Fibrous granulation tissue should be trimmed to below the level of the skin edges to allow a healthy vascular bed of granulation tissue to form prior to grafting, in fresh wounds, grafting can be delayed several days to allow sprouting capillaries to develop
|
|
|
Methods to reduce bacterial numbers:
|
topical application of antimicrobial drugs
|
|
|
What are the benefits of full thickness grafts?
|
Resistant to trauma, best cosmetic outcome, and better functional outcome compared with split thickness grafts
|
|
|
Disadvantages of full thickness grafts:
|
poorer acceptance because of the greater need from nourishment and fewer exposed blood vessels
|
|
|
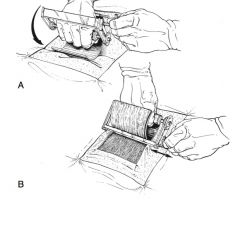
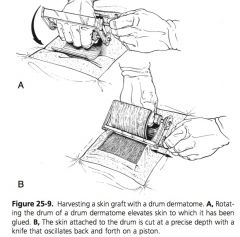
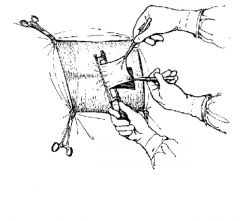
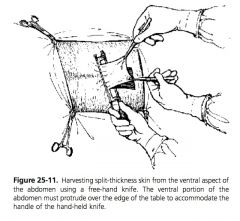
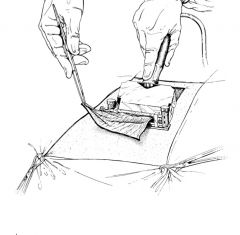
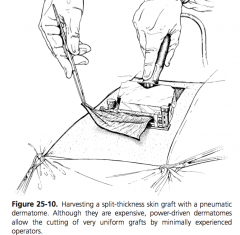
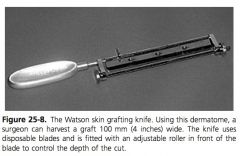
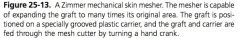
How can split thickness grafts can be harvested?
|
hand instruments, drum dermatomes, and power driven dermatomes
|
|
|
Advantages of hand dermatomes vs drum or power dermatomes:
|
Hand dermatomes provide a graft that is more uniform, larger, can be used on the ventral abdomen, is less expensive, requires less maintenance, and is easier to sterilize
|
|
|
How is graft thickness is assessed?
|
translucency and pattern of bleeding
|
|
|
Advantages of split thickness grafts:
|
they can be used to cover large defects, improved survivability, and better cosmetic appearance than island grafts
|
|
|
Disadvantages of split thickness grafts:
|
poorer cosmetic appearance than full thickness grafts and more difficulty in obtaining the graft
|
|
|
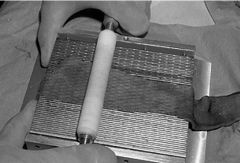
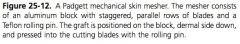
How can sheet grafts can be meshed?
|
manual fenestration with a scalpel blade or through a meshgraft dermatome
|
|
|
Advantages of meshing:
|
uniform coverage of a wound larger than the graft harvested, prevention of fluid accumulation under graft, application of topical antimicrobials, improve conforming to the wound bed, and improved stability or attachment to the wound bed
|
|
|
Punch grafts:
|
performed with biopsy punches, graft generally 2 cm larger than the recipient bed punch
|
|
|
Pinch grafts:
|
small (3mm) discs of skin which are split thickness at the narrow end and full thickness at the wider end, and are inserted into pockets made into the granulation tissue
|
|
|
Tunnel grafts:
|
full or split thickness strips of skin imbedded under granulation tissue, that are exposed 6-10 days later
|
|
|
Benefits of tunnel grafts:
|
are not affected by movement and can be used over highly mobile areas
|
|
|
Modified meek grafting technique:
|
combination of island grafting and split thickness sheet grafting, graft cut with circular blades to produce 196 3mm x 3mm grafts, epidermal side of grafts adhered to stretchable gauze that can separate grafts, gauze attached to wound, removed once the grafts have adhered
|
|
|
Advantages of the modified meek micrograft:
|
better acceptance on poorer quality wounds with a higher concentration of grafts on the wound than for other island graft, failure of one graft does not affect all the grafts
|
|
|
Disadvantages of the modified meek micrograft:
|
graft harvest is done under general anesthesia and the equipment is expensive
|
|
|
Supply of cutaneous allografts:
|
harvested from refrigerated cadavers
|
|
|
Survival of cutaneous allografts:
|
2 to 3 weeks
|
|
|
Benefits of allografts:
|
promote epithelialization, angiogenesis, retard exuberant granulation tissue, and are a bacterial barrier to infection
|
|
|
How are grafts stored?
|
refrigerated, in saline or lactated ringer’s solution for several weeks, or longer if placed in medium
|
|
|
Most common medium graft storage medium:
|
McCoy’s 5A and serum
|
|
|
What does McCoy’s 5A contain?
|
balanced electrolyte solution, amino acids, vitamins, dextrose, and a pH indicator
|
|
|
What should the concentration of serum be in storage medium?
|
10-33%
|
|
|
What occurs with higher concentration of serum in storage medium?
|
greater than 33% stimulate metabolic activity in the graft
|
|
|
Benefits of stored grafts:
|
Grafts stored for at least 24 hours are more readily accepted than fresh grafts because release of anaerobic metabolites stimulates revascularization of the graft
|
|
|
|
|
|
|
|
|
|
|

|
|
|

|

|
|
|
|
|

|
|

