![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
109 Cards in this Set
- Front
- Back
|
Speech Awareness Threshold
|
SAT
Lowest level at which the presence of a speech signal can be heard 50% of the time |
|
|
Speech Detection Threshold
|
SDT
Same as SAT and SRT Lowest level at which a speech signal is intelligible enough to be recognized or identified 50% of the time. |
|
|
Speech Reception/Recognition Threshold
|
SRT
Speech Reception Threshold is the older term Speech Recognition Threshold is the current preferred term |
|
|
Spondee Threshold
|
ST
SRT when measured with spondees |
|
|
Speech/word recognition scores
|
SRS, WRS
Measure of speech understanding or intelligibility at suprathreshold (above threshold) levels Trying to assess the listeners best or maximum understanding capabilities |
|
|
Most comfortable loudness level
|
MCL
Hearing level at which the patient experiences speech (or tonal) stimuli to be most comfortable (i.e. where the person prefers to listen to the speech or tonal materials) |
|
|
Conversational Speech Levels
|
Soft, average, loud
Long term output level of speech at various conversational effort levels by the speaker. Soft = 20-30 dB HL Average = 35-55 dB HL Loud = >55 dB HL |
|
|
Uncomfortable Loudness Level
|
UCL
Hearing level at which the patient considers speech (or tonal) stimuli to be uncomfortably loud |
|
|
Dynamic range for speech
|
DR
Range in decibels between the patient's SRT and UCL Patient's usable listening range DR may be reduced in SNHL |
|
|
What does SRT serve to corroborate?
What does it help us decide? |
Pure tune thresholds
It serves as a reference point for deciding on the level to perform suprathreshold speech recognition testing |
|
|
What is the rationale for doing SRT?
|
Corroborate pure tone thresholds
Determine hearing aid/amplification needs and performance Ascertain the need for aural (re)hab and progress in management Determine hearing sensitivity for young children and others who are difficult to test. |
|
|
What is the rationale for doing SDT/SAT testing?
|
A measure of speech audibility (less complex skill than speech recognition)
Obtained when SRT cannot be established |
|
|
What is the rationale for doing suprathreshold SRS/WRS testing?
-2 reasons |
Determine the extent of hearing loss and how it affects speech understanding
Aids in differential diagnosis of auditory disorders |
|
|
What are the general considerations for instrumentation with threshold testing?
|
Audiometer controls
Input options Output options Interrupter switch "on" Equipment calibrated (re: ANSI standards) so that 0 dB HL has a specific SPL value (depends on the transducer) |
|
|
What are the stimulus choices with threshold testing?
|
Recorded vs. Monitored Live Voice
|
|
|
What are the considerations when choosing recorded vs. monitored live voice?
|
Recorded is the preferred method
CD better than tape (no noise/distortion) Better control of intensity than MLV Consistency in speech pattern of speaker MLV more flexible & can save time (i.e. kids, geriatrics, "special clients") MLV allows for rate of presentation manipulation MLV allows for selection deletion of specific "trouble words" |
|
|
What test materials (types of words) used for threshold and suprathreshold testing?
|
Threshold: spondees (e.g. Central Institute of the Deaf W-1) most common
Suprathreshold: phonetically or phonemically balanced monosyllabic word lists (e.g. CID W-22 and NU 6 most common) |
|
|
Open Set Stimuli
-What is it? -What can results be influenced by? |
Patient has no prior knowledge of what the possible words/alternatives will be
"Fill in the blank" Influenced by language skills, vocabulary, familiarity with words, etc. Most traditional word lists are "open" (W-1, W-22, NU6, PAL 50, etc.) |
|
|
Closed Set Stimuli
|
Patient is provided with a choice of several possible response alternatives
"multiple choice" Ex: Spondee Picture Board, WIPI, SSI |
|
|
Why might you want to use a picture board?
|
Children may not be able to repeat the words coming through the loudspeaker because they are shy or uncomfortable
People with articulation problems |
|
|
Carrier Phrase
|
"Say the word" or "You will say"
Threshold testing: carrier phrase often omitted for MLV and recorded Research has shown no effect for SRT Suprathreshold testing: carrier phrase used for most traditional monosyllabic word presentations for both MLV and recorded. |
|
|
General Considerations: Stimulus Calibration
Recorded |
Typically a 1000 Hz tone at the onset which must be set to 0 on the VU meter
Ensures equipment/stimuli is "calibrated" Must re-calibrate when changing recording stimuli |
|
|
General Considerations: Stimulus Calibration
Monitored Live Voice |
When doing MLV, clinician must ensure that his vocal effort and input to the microphone is "peaking" at 0 dB on the voltage/volume unit (VU) meter
|
|
|
What is the purpose of SRT?
|
Determination of the level at which 50% of a presented speech test list is understood and repeated back correctly
|
|
|
What is the purpose of SRS/WRS?
|
To assess the patient's ability to understand speech stimuli presented at suprathreshold levels.
|
|
|
How should instructions be given?
|
Phrased in language appropriate to the patient
Orient the patient to the nature of the task Specify what type of test material will be presented Specify what type of response is required (point to, circle, repeat) |
|
|
Response mode
|
Usually repetition
Can adapt if needed: writing, picture board pointing, ID of body parts, objects, answering questions, etc. |
|
|
Should you encourage guessing for threshold testing?
|
Yes, you should encourage guessing for both threshold and suprathreshold testing
|
|
|
Familiarization
-How is it done? -Why is it done? |
Patient is familiarized with the words at a suprathreshold level (e.g. MCL)
-Test vocabulary (make sure it is familiar) -Make sure patient can be understood by clinician -Difficult words can be eliminated from the test |
|
|
Interpretation of threshold testing
|
SRT/PTA agreement - if they don't agree, need to evaluate why not.
Should be +/- 5-10 dB or +/- 8 dB (if doing 2 dB steps) |
|
|
What must you consider when interpreting threshold tests?
|
"audiometric configuration" effect
Use 3 speech frequencies or Fletcher best 2-frequency average Look at audiogram configuration to determine which one to use. Discrepancies warrant explanation |
|
|
SDT/PTA agreement
|
7 to 0 dB better (smaller dB) than SRT
Speech can be detected at lower intensities than it can be recognized and repeated back |
|
|
What influences threshold testing?
|
MLV vs. recorded
Familiarity of words Homogeneity of words (is the list a good representation of available words with both voiced and unvoiced phonemes?) Set size |
|
|
How can you interpret suprathreshold tests?
|
Maximum Performance (e.g. PB-Max)
If normal hearing, then expect high scores If conductive hearing loss, then expect high scores as long as the presentation level covers the degree of HL Wide range of scores possible for sensorineural HL Abnormally low scores indicative of retrocochlear |
|
|
What is the main effect of mild HL on word recognition?
|
In quiet situations, mostly unaffected
In noise, may decrease to 50% Mostly miss consonants |
|
|
What is the main effect of mild to moderate HL on word recognition?
|
Quiet environment, face to face, topic known, vocabulary constrained - will understand most of it
|
|
|
What is the main effect of moderate HL on word recognition?
|
May miss most or all of the message if no hearing aid is used
Difficulty in group situations |
|
|
Severe
|
May not hear voices, unless speech is loud
With amplification, may recognize some speech & detect environmental sounds |
|
|
Profound
|
May perceive sound as vibrations
Rely on vision as primary sense of speech recognition May even need amplification for loud sounds |
|
|
Performance-Intensity Function
|
Scores differ as a function of presentation level
|
|
|
Why should you do more than 1 level for suprathreshold
|
Scores may differ as a function of disorder site. For conductive, the performance line follows the normal curve, it just requires higher SPL. For Cochlear, the performance line plateaus at a lower %words correct rate. With retrocochlear, there is a rollover of performance.
|
|
|
Rollover of the PI Function
|
Reduction of speech recognition scores that occurs above the level where maximum score is obtained
|
|
|
Rollover Index
|
Number which describes the rollover pattern
|
|
|
What does significant rollover indicate?
|
Retrocochlear disorder
|
|
|
How do you calculate the Rollover Index?
|
Best Score (PB Max) - Worst score (after PB Max) / PB Max
|
|
|
What is considered a significant rollover index?
|
>0.45
|
|
|
What are the influencing factors for suprathreshold testing?
|
MLV vs. Recorded
Type of speech material -CV, Monosyllables, Sentences, Synthetic Sentences, High Freq. Word Lists Equivalency of test forms Familiarity of Words Homogeneity of words Presentation level Reliability depends on the set size of the test -Reducing test makes the test less reliable |
|
|
What is the primary reason for obtaining MCL and UCL?
|
For rehabiliatation and amplification purposes
|
|
|
What type of presentation can you use for MCL and UCL?
|
Can use recorded or monitored live voice speech material
-Lists, cold running speech Can also use narrow bands of noise or pure tones |
|
|
What are the categories of loudness (from loud to soft)?
|
Uncomfortably loud
Loud but okay Comfortable but slightly loud Comfortable Comfortable but slightly soft Soft Very soft |
|
|
Ipsilateral Ear
|
Test ear
Same side as stimulus |
|
|
Contralateral Ear
|
Non-test ear
Opposite side from stimulus |
|
|
Can the terms "ipsilateral ear" and "test ear" be used interchangably?
|
Not always
It is not always the case that the ear the clinician wants to test is the ear that is being stimulated. Results may be invalid |
|
|
What are the problems requiring the use of masking?
|
Unilateral hearing loss (may be shown on case history)
Asymmetrical bilateral hearing loss |
|
|
What questions should you ask when you have unilateral or asymmetrical bilateral HL?
|
Can this be a dead ear?
Which ear is hearing the sound" Is this a valid audiogram? |
|
|
Cross over
|
The passage of sound from the test ear to the non-test ear
|
|
|
Is bone conduction or "around the head" air conduction cross over the more significant problem? Why?
|
Bone conduction because there is no attenuation. The bone conductor is vibrating the entire skull
|
|
|
What is a situation when you may have "around the head" cross over?
|
If the earphone doesn't fit correctly, sound may escape
|
|
|
Cross hearing
|
Sound which arrived at the non-test ear by cross over is heard by the non-test ear
|
|
|
Through the head crossover
|
Bone conduction crossover due to a signal presented via earphone or a bone vibrator
|
|
|
Around the head crossover
|
Air conduction crossover
|
|
|
Why doesn't crossover always mean cross hearing?
|
The sound may not be intense enough by the time it crosses over to stimulate the other ear
|
|
|
Interaural attenuation
|
the difference between a signal's intensity at the ipsilateral/test ear and the contralateral/non-test ear
A measure of how much the signal is reduced between the ipsilateral and contralateral ear |
|
|
Minimum intensity needed to set the skull into vibration can vary depending on what factors?
|
Frequencies, listeners, type of air conduction earphones used (supra-aural or insert)
|
|
|
What is a conservative estimate for how much energy that can be lost due to interaural attenuation?
|
40 dB for all frequencies and listeners for pure tone signals presented through supra aural type earphones
|
|
|
What must happen for a signal to be cross heard in the non-test ear?
|
The test tone level must equal or exceed interaural attenuation
|
|
|
Interaural attentuation for speech signals are slightly _______ than for pure tones.
What is a conservative estimate for speech signals presented through supra aural type earphones? |
higher
Still 40 dB |
|
|
What is the interaural attenuation value for bone conduction?
|
0 dB
Nothing is lost during the crossover |
|
|
During unmasked BC testing, which ear will respond to the signal if the vibrator is placed on the right mastoid? Left mastoid?
|
The better ear
If SN hearing is equal in both ears, both will pick up the signal. |
|
|
Masking
|
The interference of one sound by another in the same ear
|
|
|
When to mask: Rule 1
|
For pure tone air conduction testing
Mask when there is a difference of 40 dB or greater between the air conduction thresholds of the right and left ears |
|
|
When to mask: Rule 2
-What is it? -What kind of masking do you need to do if it applies? |
For pure tone air conduction testing
Mask when there is a difference of 40 dB between the bone conduction threshold in the better ear and the air conduction threshold in the poorer ear. |
|
|
When to mask: Rule 3
|
During pure tone bone conduction testing
Mask when there is a difference of 10 dB or greater between the BC thereshold of the better ear and the AC threshold of the poorer ear |
|
|
Central Masking Effect
|
Elevation of the test ear's threshold as a result of masking noise in the other non-test ear
A threshold shift that occurs as a function of perceptual disruption rather than because of peripheral masking Usually minimal (5 dB) but in some people it could be 15-20 dB |
|
|
Types of Masking Noise
|
White Noise
Narrow Band Noise Speech Noise |
|
|
White Noise
|
A noise that covers a broad band of frequencies at approximately equal intensities
|
|
|
Narrow band noise
|
White noise which has been filtered into limited bands of frequencies
Each band consists of frequencies surrounding a center frequency which corresponds to the pure tone being masked. |
|
|
Speech Noise
|
White noise filtered so that it approximates the overall spectrum of speech
|
|
|
What is the best masking choice for pure tone signals?
|
Narrow band noise
|
|
|
What is the best masking choice for speech signals?
|
Speech noise
|
|
|
Why don't we just do masking all the time?
|
Central Masking Effect
Children or people with cognitive difficulties may not be able to attend to the tones Occlusion effect |
|
|
Minimum Effective Masking
|
The noise level (dB HL) needed to just effectively mask a test signal in the non-test ear
The lowest masker intensity required to prevent the non-test ear from responding to the test signal |
|
|
Maximum Effective Masking
|
The noise level (dB HL) just below that sufficient to mask the test signal in the test ear
|
|
|
Overmasking
|
A condition in which the masking noise level is sufficient to cross the head and affect threshold in the test ear
|
|
|
Occlusion Effect
|
Increase in loudness when the ears are occluded during bone conduction testing
Seen in people with normal hearing and SNHL but absent in patients with CHL |
|
|
What contributes to the loudness increase with the occlusion effect?
|
The intensity increase of sound delivered by bone conduction vibrator to the inner ear via osseotympanic bone conduction
|
|
|
Masking Plateau
|
Threshold level that does not change as the masking level increases from minimum to maximum
|
|
|
At plateau, threshold is being determined by _________.
|
The test ear
|
|
|
What do we use to determine plateau?
|
The Hood Plateau Seeking Method
|
|
|
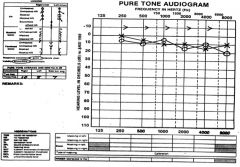
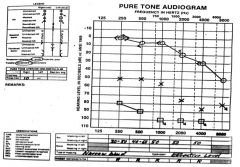
Hearing is within normal limits but there is an air-bone gap indicating that the patient may not be hearing to his/her potential.
Rule 1: No: There is not a 40 dB or greater difference between the air conduction thresholds of the right and left ears. Rule 2: No: There is not a 40 dB or greater difference between the bone conduction threshold of the better ear and the air conduction threshold of the worse ear. Masking for air conduction is not needed at any frequency in either ear. Rule 3: Yes: There is a 10 dB difference between the bone conduction threshold of the better ear and the air conduction threshold of the worse ear. Therefore, you need to do bone conduction masking to see which ear has (or if both ears have) an air-bone gap. |
|
|
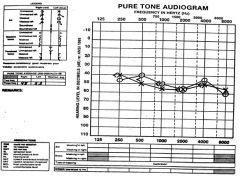
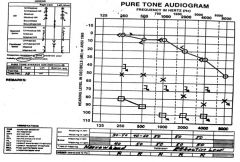
Bilateral, symmetrical moderate hearing loss.
Rule 1: No: There is not a 40 dB or greater difference between the right and left ears. Rule 2: No: There is not a 40 dB or greater difference between the bone conduction threshold in the better ear and the air conduction threshold in the poorer ear. You do not need to do air conduction masking. Rule 3: No: There is not a 10 dB or greater difference between the bone conduction threshold of the better ear and the air conduction threshold of the poorer ear. No masking is needed. |
|
|
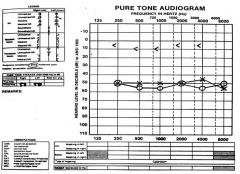
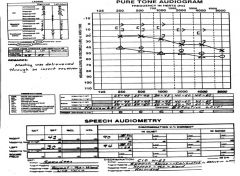
Rule 1: No: There isn't a 40 dB or greater difference between right and left AC scores.
Rule 2: Yes: There is a 40 dB or greater difference between the BC threshold of the better ear and the AC threshold in the poorer ear. -We don't know which AC scores are accurate (since the signal could have been picked up in the other ear by BC). Rule 3: Yes: There is a sufficient gap between the BC and AC scores. We need to do air conduction masking but this could cause cross-hearing of the masking noise. We also need to do bone conduction masking. This is a "masking dilema" |
|
|
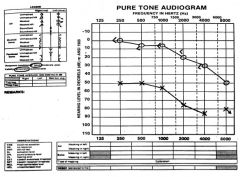
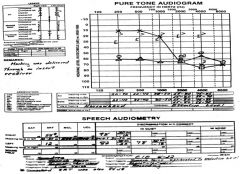
Rule 1: Yes: There is a 40 dB or greater difference between the air conduction thresholds of the right and left ear.
Rule 2: Yes: There is a 40 dB or greater difference between the bone conduction threshold in the better ear and air conduction threshold in the poorer ear. Rule 3: Yes: There is a 10 dB or greater difference between the bone conduction threshold of the better ear and the air conduction threshold of the poorer ear. All three rules apply and there is a classic shadow curve, indicating that the left ear may have thresholds that are considerably poorer than those shown. |
|
|
When masking was used in the right ear, the left ear air conduction thresholds became considerably poorer. Responses could not be obtained at 1000, 2000 or 4000 Hz.
We conclude that the unmasked left ear air conduction threshold represented a shadow curve or cross hearing of the right ear. Since we do not have masked bone conduction thresholds for the left ear, we do not know what type of loss exists in that ear. The loss may be sensorineural or it may be mixed. |
|
|
No air/bone gap between the AC threshold in the right ear and unmasked BC thresholds so we can assume the unmasked BC thresholds represent the actual threshold of the right ear.
Large air/bone gaps exist between air conduction results of the left ear and unmasked bone conduction thresholds so we don't know the actual bone conduction thesholds for the left ear unless we do contralateral masking. Right ear has hearing w/in normal limits through 2000 Hz and a sensorineural hearing loss in the higher frequencies. Left ear also has a sensorineural hearing loss. |
|
|
Masking not needed when obtaining SRT in either ear.
Right ear: SRT of 42 dB HL is less than 40 dB above the SRT of the left ear or the best BC threshold in the left ear (10 dB at 250 Hz and 500 Hz Left ear: SRT of 30 dB HL is less than 40 dB above the best BC threshold of the right ear (5 dB at 250, 500, 1000 Hz) and is less than the SRT of the right ear Masking is required for both ears for suprathereshold speech recognition testing. |
|
|
In suprathreshold speech testing, masking is needed whenever the presentation level of the words in the test ear is:
40 dB or more above the BC threshold of the opposite ear, or 40 dB or more above the SRT of the opposite ear In this case, the presentation level of the PB words in the right ear is 88 dB HL (30 dB SL re: SRT) which is 71 dB above the BC threshold of 15 dB at 250 Hz, 500 Hz and 1000 Hz in the left ear and 74 dB above the left ear's SRT |
|
|
What are the steps of the Hood Plateau Method?
|
When a tone seems to be heard by the nontest ear, a noise is delivered to that ear and the level of noise is increased in 5 dB increments until the tone is no longer audible. Then the threshold for the tone is measured again in the presence of the contralateral noise. If the tone is heard, raise the masking noise by 5 dB. If not heard, raise the tone by 5 dB. Do this until the masking noise can be raised 3 times and the tone is still heard without needing to raise it.
|
|
|
What three variables determine the width of the masking plateau?
|
The AC threshold of the nontest (masked) ear
The BC threshold of the test ear The patient's interaural attenuation |
|
|
The _____ the AC threshold of the masked ear, the ______ must be the initial masking level. This causes the chances that the noise will cross to the test ear to be _____.
|
higher
greater greater |
|
|
The _____ the BC threshold of the ______, the ______ the likelihood that a noise reaching the cochlea of that ear from a masking receiver on the opposite ear will exceed its threshold, producing a ______ in the test ear.
|
lower
test ear greater threshold shift |
|
|
The smaller the interaural attenuation, the _____ the level of the noise that reaches the test ear.
|
higher
|
|
|
What is the formula for calculating the efficient masking level for bone conduction?
|
EM = AC (nontest ear) + 10 dB + OE
|
|
|
What is the initial amount of masking you want to put into the nontest ear?
|
AC of the nontest ear + 10 dB
|
|
|
What can be interpreted from high scores on suprathreshold testing?
|
Normal or conductive HL
|
|
|
What can be interpreted from low scores on suprathreshold testing?
|
Sensorineural or central HL
|
|
|
How do you determine the level for masking for suprathreshold speech testing?
|
EM = plateau(test ear) - IA + largest A/B gap(nontest ear)
|
|
|
How can you tell if overmasking has occured?
|
If the masking level used minus interaural attenuation is greater than the best BC threshold of the test ear
EM(nontest ear) - IA > BC(test ear) |
|
|
What is the Occlusion Effect at various frequencies?
|
250 Hz = 15 dB
500 Hz = 10 dB 1000 Hz = 5 dB |

