![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
73 Cards in this Set
- Front
- Back
|
Analog- programmable
|
Computer interface: adjusted with interface + computer software or stand-alone programmer.
More precise that analog non-programmable. Disadvantages: adjustments not as precise as digital. Limited adjustments available. Advanced processing not available. |
|
|
Digital- programmable
|
Analog transducers (mic, receiver, t-coil).
Digital processing: converts electrical voltages to digital (numbers). Advantages: potentially the best precision (if mid- to high- end). Advanced processing available. Limitations: low-end digital has limited adjustments (but cheap!) Additional distortion if not well designed. |
|
|
Feedback strategy: notch filter
|
Aid detects oscillation and then puts in a notched filter at the frequency of the oscillation (feedback).
Disadvantage: reduces gain of input signal (e.g. speech). |
|
|
Feedback strategy: feedback cancellation
|
Aid detects oscillation (feedback). Aid generates signal 180-degrees out of phase. Partially cancels feedback. Allows for an additional gain of approx 10 dB without feedback.
|
|
|
Expansion
|
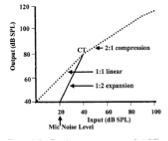
Minimizes amount of amplification below compression threshold.
Why use expansion? Reduces microphone noise and low-level environmental noise. Expansion is for very low inputs (e.g. 20 dB). |
|
|
Modulation-based noise reduction
|
Speech= slower rate, larger depth (deeper)
Noise= faster rate, smaller depth (shallower) |
|
|
Fitting range for skeleton earmolds
|
Less than 60-65 dB
|
|
|
Fitting range for full shell earmolds
|
Greater than 60-65 dB
|
|
|
Hard (Acrylic) earmolds
|
Advantages: durable, easy to modify, inexpensive.
Disadvantages: may be more prone to feedback, slight risk of harm from breakage (especially kids). |
|
|
Soft earmolds
|
Advantages: comfortable when tight fit needed, less prone to feedback than hard, no risk of breakage in the ear.
Disadvantages: difficult to modify and change tubing, discolors, hardens, less durable than hard - more frequent replacement. |
|
|
Hypoallergenic earmolds
|
Silicone (semi-soft): low incidence of allergic reactions, very difficult to modify, cannot glue tubing.
Poly-ethylene (hard): best choice for hypoallergenic application, easy to modify (grind, drill), ugly! |
|
|
Earmold acoustics: venting
|
Venting: some of the amplified sound escapes through the vent (mostly low frequencies) smaller vent --> less sound gets out. Some sound comes trough the vent (mostly high frequencies) smaller vent --> less high frequencies get in.
Diagonal (side branch) vents: decrease high frequencies - up to 10 dB above 1 kHz. Intersection close to outside worse b/c increase likelihood of feedback. |
|
|
Earmold acoustics: dampers
|
Dampers: "to decrease gain and max output at frequencies corresponding to resonances in sound bore."
Placement: earmold tubing (BTE), earhook (BTE), sound bore (ITE). |
|
|
Earmold acoustics: sound bore
|
Varying diameter of sound bore affects high frequency response > 2 kHz (primairly 3-6 kHz). The larger the diameter, the more gain in the high frequencies.
Two ways: Acoustic horn- maximum 9 dB better than standard tubing. Large diameter bore- maximum 6 dB better than standard tubing. |
|
|
Candidacy factors
|
Communication problems: ***self perceived***, perceived by friends/family.
Hearing loss: thresholds, speech recognition. Lifestyle/communication demands. Motivation/expectations. |
|
|
Determining Candidacy: Data Used
|
Audiometric data: thresholds and speech recognition.
Information from interview. |
|
|
The interview
|
Communication difficulties?
-Situations, frequency, severity. -Open-ended or probing questions: Why are you here today?" "Tell me about situations in which you have trouble hearing." -Watch for signs of denial. Listening environments encountered? -Leading questions: Do you socialize much? In what setting? Environments? -Ability and support -Motivation. Self vs. others. |
|
|
COSI
|
Client Oriented Scale of Improvement. Disability-based. Evaluate the extent to which the patient is having difficulty hearing in different situations. Nominate communicative situations targeted for improvement. After fitting: measure BENEFIT (i.e. improvement with aid), evaluate final disability.
|
|
|
GHABP
|
Glasgow Hearing Aid Benefit (or Difference) Profile. Evaluates both disability and handicap. Advantages: short and standardized. Includes "goals" section like COSI.
|
|
|
Disability Measures
|
Evaluate the extent to which a patient has difficulty hearing in different situations.
|
|
|
Handicap Measures
|
Evaluates the patients feeling about the hearing loss (how much is patient prevented from doing what he/she WANTS to DO). Emotional aspect of hearing loss.
|
|
|
What is the significance of an average hearing loss (PTA) of 40 dB HL in terms of the frequency of reported problems (based on HHIE)?
|
Most with average hearing losses of 40 dB HL or more report communication problems. Of those with averages losses below 40 dB HL some will report communication problems and some won’t. Depends on the role of communication demands/lifestyle. If the PTA is 40 or more and patient does NOT report communication problems consider possible reasons.
|
|
|
Palmer et al. (2009) used one simple question to predict hearing aid uptake. What was this question? Describe the predictive value of different ratings in the prediction of uptake.
|
“On a scale from 1 to 10, 1 being the worst and 10 being the best, how would you rate your current overall hearing ability?”
Results: 75-100% of those with ratings of 1-5 will pursue amplification. 80-100% of those with ratings 8-10 will NOT pursue amplification. Ratings of 6-7 are somewhere in the middle. The may need more information, counseling, demo ect. Uptake not well predicted by audiogram. |
|
|
Choosing styles and processing/circuit options
|
Choosing styles: driven by priorities and practical considerations (e.g. dexterity)
Choosing processing/circuit options: match to communicative complaints and communication demands. |
|
|
Early approach to amount of gain used.
|
Mirroring the audiogram.
Knudson & Jones, 1935 Every 1 dB increase in hearing loss requires 1 dB of additional gain. |
|
|
Problems with "Mirroring the audiogram"
|
Tolerance levels exceeded for higher level sounds.
Excessive gain, particularly for Hz with greatest loss. Why? Increase HL = decreased DR |
|
|
Two general approaches to gain
|
1) Threshold-based approaches
-Gain and maximum output based on pure-tone thresholds. -e.g. NAL, DSL, POGO ect. 2) Loudness-based approaches -Gain and maximum output based on loudness (MCL, UCL, full scales) -e.g. Pascoe, 1978 |
|
|
Prescriptive fitting
|
Should be considered a "starting point"
"Fine tuning" is sometimes necessary to optimize quality |
|
|
Linear prescriptions
|
Appropriate for compression limiting and linear aids
|
|
|
NAL
|
"Loudness equalization"
Goal: to maximize speech intelligibility at the preferred listening level of the hearing aid user. Assumptions: Intelligibility maximized when all frequency regions at equal loudness. Preferred listening levels of real patients correspond to MCL. NAL perscriptions -- based on pure-tone threshold. |
|
|
What is the difference between speech levels in dB HL and dB SPL when presented though speakers? headphones?
|
dB SPL is 12.5 dB higher than HL levels is presented through speakers.
dB SPL is 20 dB higher than HL levels presented through earphones. |
|
|
Frequency response shaping considerations
|
-Shape of normal loudness curve (mid-level)
-Shape of speech spectrum -Shape of hearing loss |
|
|
Describe the essentials of the original NAL prescriptive approach
|
For mild-moderate HL – roughly based on half gain rule. Gain at 1000 Hz is equal to 0.46 times the loss at 1000 Hz
For severe-profound loss – need more gain (2/3 gain) at 1000 Hz |
|
|
Describe the research evidence demonstrating validation of NAL-R (Byrne and Cotton, 1987; 1988)
|
Approximately ¾ of listeners judged NAL-R to be as good as or better than the alternative frequency responses and the average preferred listening levels were within 1 dB of prescribed.
|
|
|
Describe of how and why NAL-R was modified further for severe-profound hearing losses
|
Went from NAL-R to NAL-RP because they needed more gain. 2/3rds instead of ½.
|
|
|
Why can't you use half gain rule to estimate NAL-RP?
|
The ½ gain rule substantially overestimates NAL-RP in low frequencies – that is, the ½ gain rule prescribe TOO MUCH low frequency gain.
|
|
|
Explain the concept of loudness equalization as it applies to the goals of the NAL prescription
|
You need different phon magnitude to equal the same level of dB SPL.
Example: 40 phon curve (standard = 1000 Hz @ 40 dB SPL Mid frequencies require approximately equal intensity level for equal loudness to a 1000 Hz 40 dB tone. Lower frequencies e.g. 100 Hz, intensity must be raised by approximately 10 dB in order to produce equal loudness to a 1000 Hz 40 dB tone. As the phons increase (i.e. dB SPL for 1000 Hz increases), the equal loudness contours flatten out more. |
|
|
LTASS
|
Long-term average speech spectrum.
The level of speech across different frequencies when averaged over a long period of time (e.g. 30 seconds or more). Characteristics: The LTASS has more energy in the low frequencies. 6 dB/octave drop above 500 Hz. |
|
|
Goals underlying the NAL-NL prescription (for WDRC aids)
|
1) Amplify relative loudness of different speech band to maximize intelligibility.
2) Loudness control: amplify so that sounds are no louder than normal hearing person perceives at same level. 3) Does not attempt to "normalize" loudness. |
|
|
Loudness normalization
|
Amplify sound so that at any input level and frequency, the hearing aid wearer would report loudness to be the same as that which a person with normal hearing person would report.
|
|
|
Similarities between NAL-NL1 and NAL-NL2
|
Note: NAL-NL2 not yet fully released.
Same prescription of maximum output. Same allowance for number of channels. |
|
|
5 main changes made in NAL-NL2 (compared to NL1)
|
1) Less gain than NAL-NL1 above 65 dB (people prefer less gain)
2) Gender correction (females prefer 4 dB less gain) 3) Acclimatization (experience) correction (-2 dB on average for new users) 4) Binaural correction changed (less than NAL-NL1) 5) Greater gain for children with congenital HL at low input levels |
|
|
The empirical basis (research studies) for the DSL gain targets.
|
These targets were based on a study by Erber and Witt conducted to determine how sensation level affected speech understanding for a group of children with severe hearing loss. They determined the sensation levels that maximized the ability to understand speech. The DSL developers based their "desired sensation levels" on the levels that were found to maximize speech understanding in the Erber and Witt study. They then determined that the target levels were within the comfort range based on a study of preferred listening levels of children with hearing loss.
|
|
|
How did DSL developers arrive at their maximum output targets?
|
The developers based MPO targets on the adult norms for loudness discomfort levels. They set the targets 1 standard deviation below the adult norms for loudness discomfort and then made slight additional adjustments for upward spread of masking.
|
|
|
Describe differences between frequency responses prescribed by DSL and DSL[i/o] v.5 and NAL-NL1 (linear/compression limiting Rx)
|
Flat losses: DSL and DSL[i/o] prescribe more in the high and low frequencies than NAL-NL1.
Sloping: DSL and DSL[i/o] prescribe more gain in the high frequencies than NAL-NL1. The steeper the slope, the larger the difference in HF gain between DSL and NAL prescriptions. |
|
|
Loudness control:
|
Amplify so that sounds are no louder than normal hearing person perceives at same level.
|
|
|
Loudness scale
|
Give the patient a list and tell them to identify which category the sounds presented fall into (usually use bottom 7 categories)
Painfully loud Extremely uncomfortable Uncomfortable loud Loud, but OK Comfortable, but slightly loud Comfortable Comfortable, but slightly soft Soft Very soft |
|
|
Consequences of setting OSPL90 too high or too low
|
Too high: loudness discomfort and further damage to hearing.
Too low: HA user does not receive sounds at adequate SL and excessive saturation. |
|
|
Approaches to setting max output level: approach 1
|
Based on direct measurements UCL.
Decide on a loudness procedure: categorical rating of loudness, ascending procedure, practice effects associated with loudness measures - stabilize by 3rd trial. Otherwise people underestimate. |
|
|
Approaches to setting max output level: approach 2
|
Prescriptive method.
There are consequences for setting OSPL too high or low. NAL OSPL prescription: best value of OSPL should consider both discomfort and saturation. |
|
|
The maximum output controversy
|
Position 1: Must base MPO on individually measured LDLs.
LDLs variable. Cannot be predicted by PT thresholds. Implications: HAs problems (discomfort) if LDLs not used. Position 2: Aid MPO can be prescribed using PT threshold. LDLs are variable but range of acceptability can be predicted. Must way risk/benefit of prediction vs. LDL measures. |
|
|
NAL OSPL validation study "Pro-Rx"
|
Storey et al. 1998: prescription validated with real subjected wearing aids. Tested aided loudness discomfort to make sure Rx settings did not exceed LDL. Adding LDLs did not substantially improve accuracy of OSPL procedure (only 0.4 dB)
Mackersie (2007): fittings based on NAL OSPL Rx PLUS aided loudness validation at fitting. Unaided LDL measures. Max output (ear canal) exceeded LDL for only 1/29 and this person did not want his aid adjusted. Conclusion - LDL not worth the time. |
|
|
NAL OSLP validation study "Pro-LDL"
|
Shi et al. (2007): fewer adjustments (average 1 less) when LDLs measured. BUT used (unvalidated) DSL [i/o] Rx, not NAL.
Munro & Patel (1998): Correlation between amount by which max output exceeded LDL and reported loudness problems. BUT no information about how MPO determined - NAL Rx not yet developed. |
|
|
How do you modify gain/frequency response targets for a conductive/mixed HL.
|
Gain frequency response prescriptions: prescribe 1/2 gain for SN part of the loss. Prescribe additional gain at each frequency equal to 75% of the conductive loss (ABG).
OSLP: prescribe OSLP for SN part of loss. Increase OSLP by adding 87.5% of the ABG. |
|
|
Four general binaural effects that enhance hearing
|
Localization
Loudness Summation Diffraction Noise |
|
|
Binaural effects: Localization
|
Horizontal localization: depends on time and intensity differences between ears. Impaired localization may contribute to difficulty in noise. Won't be able to change listeners quickly or follow moving sound.
Vertical localization: depends on high frequency spectral cues. Binaural hearing is less important for vertical localization. |
|
|
Binaural effects: Loudness Summation
|
Loudness greater when using two ears compared to one. Near thresholds loudness summation = 3 dB. At comfortable level loudness summation = 5-6 dB.
|
|
|
Binaural effects: Diffraction
|
Head diffraction. The head is getting in the way of sounds coming at the head from an angle other than directly in front or behind. High frequencies are less able to travel around the head than the low frequencies are. High frequencies more affected by diffraction. For binaural hearing you must simply attend to the ear with the better SNR. For unilateral hearing there is a disadvantage if good ear is on side of noise.
|
|
|
Binaural effects: Noise
|
Squelch effect in background noise. Understanding speech is easier with 2 ears due to the central auditory system effect. "Binaural masking level difference" - subtracts sound from side with poorer SNR. May be due to squelch effect.
|
|
|
Binaural advantages
|
Speech perception (speech in noise)
Localization Tinnitus relief Avoid late onset auditory deprivation |
|
|
Binaural advantages: Speech Perception
|
It has been demonstrated that people with binaural hearing aids have better speech understanding than those with a monaural fitting (depending on how speech intelligibility is measured). Speech intelligibility effected by: head diffraction affect and binaural squelch effect.
Ross (1980) review of laboratory studies: found that 15/19 studies showed bilateral speech advantage. 4 showed no difference. None showed unilateral advantage. Bilateral advantage- robust for moderate HL or greater. For mild HL the advantages of binaural hearing aids are less obvious because they are getting some speech signal without aids. |
|
|
Binaural advantages: Localization
|
Horizontal localization: greater advantage for moderate to severe loss than for mild loss.
Vertical localization: no binaural advantage with BTE, ITE or ITC. There may be some advantage with CIC because the pinna, which helps with localization, is not filled with an earmold. |
|
|
Binaural advantages: Tinnitus relief
|
Brooks & Bulmer (1981) found that 66% reported tinnitus decrease with 2 aids. Only 13% reported tinnitus decrease with 1 aid. More sound from the outside may distract from tinnitus,
|
|
|
Binaural advantages: Avoid late onset auditory deprivation
|
Unilateral fittings: the ability to understand speech may decrease in the unaided ear overtime. May be accompanies by small increase in speech recognition in aided ear. Magnitude of reduction varies by study, mean = 7%. Recovery following bilateral amplification in many (2/3), but not all patients.
|
|
|
Potential disadvantages of bilateral hearing aids
|
Cost
Binaural interference: small portion of elderly. Possibly due to inter-hemispheric transfer of information across the corpus collosum. Self-image: people think they look twice as disabled with two hearing aids. Usually people who are more resistant to wearing hearing aids to begin with. |
|
|
Four goals to consider for a monaural fitting
|
1) Maximize range of sounds audible to person.
2) Maximize range of sounds available to binaural interaction. 3) Send high quality signals to the brain. 4) Try to make overall hearing as “normal” as possible. |
|
|
Monaural "rule-of-thumb"
|
Fit the ear that has four frequency average (.5, 1, 2, 4 kHz) closer to 60 dB HL.
|
|
|
Which HA configuration is best?
|
Bilateral except for:
Small number of people with binaural interference. Small number with unaidable hearing in poorer ear. |
|
|
How much benefit does binaural provide?
|
Moderate to severe loss: substantially more benefit than monaural. A person with two aids can tolerate 5 dB more noise to the the same speech understanding as with one HA.
Mild in at least one ear: small benefit. |
|
|
Describe the general research findings comparing compression limiting and linear (peak clipping) output limiting for profound losses. What general recommendations does Dillon make in light of this research?
|
Earlier evidence against CL for profound
Preference: Half subject with PTA > 90 dB preferred linear over compression (Dawson et al., 1991) Recent evidence in favor of CL Most with profound HL prefer compression over linear (Barker et al., 2001) Conclusions: peak clipping if Hx use with max volume. Dillon recommends using peak clipping if the patient has a history of preferring maximum volume control settings or complains that the aid does not make sounds loud enough. Otherwise use compression limiting. |
|
|
Describe the general findings of research comparing findings for linear, compression limiting and WDRC at average input levels. Include both speech recognition and preference results.
|
Speech recognition at average conversations levels
No difference between speech recognition for linear, compression limiting, WDRC Preferences No difference between preferences for linear, compression limiting, WDRC at average input levels (65 dB SPL) |
|
|
Describe the general findings of research comparing speech recognition for linear/compression limiting vs. WDRC at low input levels.
|
Speech recognition at soft input levels is better for WDRC than for CL or linear
Why? WDRC -- increased gain for soft inputs compared to CL or linear Exception: If listeners adjust VC (linear, CL) to increase gain. Compensates for soft input level |
|
|
Describe general research findings (e.g. quality ratings – Dillon, 1988) comparing linear vs compression limiting at high input levels.
|
Increased listening comfort compared to linear (true of any type of compression)
Quality: HI listeners gave CL aids higher ratings for “clarity” judgments than linear aids (Dillon, 1988) |

