![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
74 Cards in this Set
- Front
- Back
|
ANTIINFLAMMATORY AGENTS
|
• inhibit release and/or synthesis of proinflammatory mediators
• prevent migration/activation of inflammatory cells • decrease airway hyperreactivity by decreasing inflammation • used prophylactically |
|
|
Corticosteroid drug names
|
beclomethasone (Beclovent®), flunisolide (Aerobid®), fluticasone (Flovent®),
triamcinolone acetanide (Azmacort®), prednisolone |
|
|
what do corticosteroids do to airway inflammation
|
decrease airway inflammation therefore decrease airway hyperreactivity
|
|
|
indications for corticosteroids
|
• severe asthma
- oral preparations • mild to moderate - aerosol |
|
|
issues with oral corticosteroids
|
lot of side effects
use for a short duration at the lowest dose possible |
|
|
aerosol corticosteroids are good becasue
|
a high concentration of drug administered locally to minimize systemic SE and they are safe
|
|
|
what size of particle are the aerosol corticosteroids
|
1-10 microns so the do not get absorded systemically
|
|
|
side affects and considerations for oral corticosteroids
|
peptic ulcer, Cushings syndrome, fluid retention, linear growth in children,
osteoporosis, cataracts can cause adrenal supression |
|
|
side affects and considerations for aerosol corticosteroids
|
oral candidiasis, dysphonia
prevented by rinsing the mouth after use or using a spacer to decrease particle deposition in the oropharyngeal cavity |
|
|
prophylaxis use of corticosteroids
|
therapeutic effect occurs slowly days
|
|
|
when using corticosteroids to treat asthma is the disease or symptoms being treated
|
disesase
|
|
|
peak flow measurements(flow meter)
|
• simplest measure of expiratory flow
• may be used for self-evaluation and documentation of lung ventilatory function • patient inhales completely (to TLC) and then exhales rapidly and completely into a peak flowmeter-> measures maximal flow rate of expiration |
|
|
when using corticosteroids to treat asthma are both the early and late phase inhibited
|
yes
|
|
|
Forced expiratory flow measurements(spirometer)
|
• involves the use of a spirometer
• same maneuvers are used as in peak flow measurements, except that the patient exhales into the spirometer (instead of the peak flow meter) • FEV1.0 (forced expiratory volume in one second) and FVC (forced vital capacity) are determined from the spirometer trace FEV1.0 is normalized to age, gender and body weight FEV1.0/FVC is a useful measure of pulmonary function |
|
|
mast cell stabilizer drug names
|
cromolyn sodium (Intal®), nedocromil sodium (Tilade®)
|
|
|
FEV1/FVC pulmonary function
(normal, restricted, obstructed) |
80% normal
90% restricted 50% obstructed |
|
|
what do mast stabilizers do to inflammation in asthma
|
decrease airway inflammation and therefore decrease hyperreactivity and bonchoconstriction
|
|
|
mast cell stabilizers decrease airway inflammation by...
|
i. stabilizing mast cells
→ decrease mediator release from mast cells ii. ↓ activation of eosinopils, neutrophils and monocytes--> decrease airway hyperreactivity (preventing the late response) iii. ↓ sensory nerve activation (mechanism not well understood) |
|
|
indications for mast cell stabilizers
|
• exercise-induced asthma
• asthma associated with current exposure to allergen • useful in children • NOTE: not effective in everyone |
|
|
side effects and considerations of mst cell stabilizers
|
• coughing/irritation
• unpleasant taste (nedocromil) • therapeutic effects occur slowly 4-6 weeks to maximally given prophylactically nausea, diarrhea, dyspepsia |
|
|
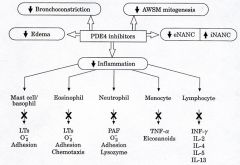
PDE4 inhibtiors for asthma acts by
|
• acts by inhibition of phosphodiesterase 4 → ↑ intracellular cAMP
→ ↓ inflammatory mediator release from mast cells & inflammatory cells ↓ bronchoconstriction |
|
|
drug names of PDE4 inhibitors for asthma
|
cilomilast
|
|
|
inddications of PDE4 inhibitors
|
• not FDA-approved
• moderate efficacy in COPD; unsubstantiated efficacy in asthma |
|
|
effects of PDE4 inhibitors
|
|
|
|
side effects and considerations fo PDE4 inhibitors
|
nausea (CNS affect), diarrhea, dyspepsia
|
|
|
LEUKOTRIENE RECEPTOR ANTAGONISTS/5-LIPOXYGENASE INHIBITORS drug names
|
zafirlukast (Accolate®), montelukast (Singulair®)
zileuton (Zyflo®) |
|
|
how do zafirlukast (Accolate®), montelukast (Singulair®) work
|
inhibit luekotriene C4 and D4 receptors (cys-LT1)
acts by inhibition of leukotriene C4/D4 receptors (cys-LT1) or of leukotriene synthesis → ↓ bronchoconstriction ↓ edema ↓ airway reactivity |
|
|
how does zileuton work
|
block 5-lipoxygenase so there are not any leukotirenes produced
|
|
|
what happens with arachidonic acid when mast cells are activated
|
it is shunted from making COX so there is a decrease in PG and 5-lipoxygenase is the prodominant enzyme in mast cells which converts arachidonic acid to leukotrienes
|
|
|
side effects and considerations of LEUKOTRIENE RECEPTOR ANTAGONISTS/5-LIPOXYGENASE INHIBITORS
|
• oral or aerosol administration
• side effects being defined zafirlukast: headache, nausea, hepatotoxicity (monitor LFTs) montelukast: dyspepsia zileuton: dyspepsia, nausea, hepatotoxicity • zafirlukast - 99% protein bound (can be an issue with displacement) - metabolized by hepatic P450 enzymes ⇒ PK interacations zileuton - microsomal CYP3A4 inhibitor ⇒ inhibits metabolism of warfarin and theophylline (PK interactions) - contraindicated in acute liver disease |
|
|
IgE BINDING ANTIBODIES drug names
|
omalizumab (Xolair®)
|
|
|
IgE BINDING ANTIBODIES
|
• humanized murine monoclonal antibody
• acts by binding to the Fc epsilon R-1 portion of circulating antibodies → prevents binding of IgE to mast cells → ↓ antigen-induced release of inflammatory mediators → ↓ asthma (and allergy) symptoms • also inhibits IgE synthesis → ↓ asthma (and allergy) symptoms |
|
|
side effects and consideration of IgE BINDING ANTIBODIES
|
• prophylaxis
• subcutaneous administration → pain and bruising at injection site • anaphylaxis (0.2%) • injected q 2-4wks very expensive ($10 K/year) |
|
|
what group of drugs decrease airway hyperreactivity in asthma
|
anti-inflammatory
|
|
|
what agents are used acutely in asthma
|
bronchodlators
|
|
|
what agents are used prophylactically for asthma
|
anti-inflammatory
|
|
|
in the central airways, airway defense comprises:
|
mucociliary escalator
ventilatory response |
|
|
ventilatory responses
|
- Δ rate - Δ depth (decrease volume)
- ↓ lung penetration (because particles in airways move more quickly, so deposition of particles in central airways are more likely to be deposited where mucus is, preventing particles from getting deep into the airways) - facilitates mucus removal [- reflex parasympathetic nerve activation]-->bronchoconstirction increases airflow which increases particle deposition because increase in particle velocity |
|
|
ICS Side Effects
|
oropharyngeal candidiases (thrush)
dysphonia(dose related) reflex cough/bronchospasmq |
|
|
prevention of ICS side effects
|
use spacer
rinse mouth after ICS lowest dose possible slow inspiration |
|
|
long term high dose ICS side effects?
|
osteoporosis, ccataracts, bruising, glaucoma
*these effects based on cumulative doses |
|
|
Therapeutic Issues with ICS
|
|
|
|
PATIENT CASE: MJ has been using a low-dose ICS for 3 months. In the last month, she has
used her albuterol approximately 3x/day when she has wheezing, 2x/week at night, and her peak flow has been about 70% of her personal best. She has had some limitations in her normal activities in the last month and she has not required oral steroids for any exacerbations. You have verified that her inhaler technique, compliance, and environmental controls are appropriate. How would you classify her asthma control? What parameters were used to make this classification? What other information would you like to have? How should MJ be treated? |
1. Not Well Controlled
2. nighttime/daily sx, activity levels, peak flow, ICS use 3. How often is wheezing happening? 4. Treatment: 1 step up to step 3. ICS, add LABA ...OR increase ICS dose from low to medium |
|
|
How to you select a classification if patient criteria fall into more than one category?
|
Classify based on WORST symptom!
Ex: 3 criteria in "not well controlled" category and 1 criterion in "very poorly controlled" category...classify patient as Very poorly controlled |
|
|
OCS role in asthma therapy
|
|
|
|
Therapeutic issues with OCS
|
|
|
|
LABA Role in asthma therapy
|
|
|
|
What is the max daily dose of LABAs?
|
salmeterol 100 mcg daily
formoterol 24 mcg daily |
|
|
can LABA be used for quick relief in asthma?
|
NO! Don't use acutely, use a SABA
|
|
|
Which asthma therapy has a warning in regards to incraeased risk of asthma related death?
|
LABA.
WARNING: Long-acting beta2-adrenergic agonists may increase the risk of asthma-related death. Therefore, when treating patients with asthma, FORADIL AEROLIZER should only be used as additional therapy for patients not adequately controlled on other asthma-controller medications (e.g., low- to medium-dose inhaled corticosteroids) or whose disease severity clearly warrants initiation of treatment with two maintenance therapies, including FORADIL AEROLIZER. Data from a large placebo-controlled US study that compared the safety of another long-acting beta2- adrenergic agonist (salmeterol) or placebo added to usual asthma therapy showed an increase in asthma-related deaths in patients receiving salmeterol. This finding with salmeterol may apply to formoterol (a long-acting beta2-adrenergic agonist), the active ingredient in FORADIL AEROLIZER (see WARNINGS). |
|
|
When do you consider step up in therapy?
|
2-6 weeks if current therapy not effective
|
|
|
when do you consider step down in therapy?
|
> or = 3 months if improvement seen
|
|
|
mast cell stabilizers in asthma:
|
cromolyn, nedocromil
|
|
|
mast cell stabilizers role in therapy in asthma
|
ALTERNATIVE
|
|
|
mast cell stabilizers therapeutic issues in asthma
|
Therapeutic Issues
|
|
|
LT modifiers role in asthma therapy
|
ALTERNATIVE Role in Therapy
|
|
|
Which LT modifier is the most likely one to recommend?
|
montelukast b/c less side effects
hepatotoxicity with Ziluten and zafirlukast, ziluten QID dosing |
|
|
LT Modifier therapeutic issues
|
|
|
|
theophylline role in asthma therapy
|
|
|
|
what is the most common theophylline dosage formulatoin?
|
sustained release tablets and capsules ( slowest absorption, but ok b/x long term treatment)
|
|
|
How to counsel pt. on eating and theophylline...
|
BE CONSISTENT to keep serum levels in range 5-15
food also help decrase stomach upset |
|
|
How does smoking effect theophylline CL?
|
increase CL by 60%.
when quit smoking, theophylline levels increase(toxicity), dose needs to be decrased when quite smoking |
|
|
how do P450 inducers effect theophylline CL?
|
incraese theophylline CL (need to increase the dose)
30% increase: phenobarbital, rifampin, charbroiled foods 60% incrase: phenytoin |
|
|
theophylline drug interactions:
|
|
|
|
what is the therapeutic theophylline range for asthma?
|
5-15 mg/L to balance SE and effectiveness
|
|
|
Theophylline dosing:
|
• Usually based on clinical judgment
• Initial: 400 mg/24 hrs (adult; lower for children) • Titration: titrated to therapeutic range of 5-15 mg/L – usually 900 mg/24 hrs |
|
|
When should a patient be referred to an asthma specialist?
|
• Difficulties achieving or maintaining control
• Step 4 care or higher is required (step 3 care or higher for children 0-4 years) • Immunotherapy or omalizumab is considered • Additional testing is indicated • Patient required 2 bursts or oral systemic corticosteroids in the past year • Patient required hospitalization in the past year |
|
|
ideal candidate for ICS:
|
any pt. w/ persistent asthma
|
|
|
ideal candidate for OCS:
|
exacerbations, severe asthma
|
|
|
ideal candidate for LABA:
|
not well controlled on low or med dose ICS, but only give LABA in combo WITH ICS
|
|
|
ideal candidate for mast cell stabilizer:
|
children, alternative tx
|
|
|
ideal candidate for LT modifier
|
alternative, ALLERGY
|
|
|
ideal candidate for theophylline
|
alternative, cost, nocturnal sx
|
|
|
asthma lecture conclusions
|
|

