![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
27 Cards in this Set
- Front
- Back
|
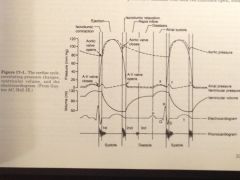
The cardiac cycle
|
– The succession of atrial and ventricular events, which comprises a period of contraction, or systole, followed by a period of relaxation, diastole
– Systole and diastole are further divided into phases |
|
|
What is the first phase of systole?
|
isovolumetric contraction
|
|
|
Isovolumetric contraction
|
– The ventricle contracts with all valves closed
|
|
|
What is the second phase of systole?
|
– the ejection phase
|
|
|
Ejection phase of systole
|
– A rapid rise in ventricular pressure causes opening of the semi lunar valves as ventricular pressure exceeds aortic pressure
|
|
|
What are the phases of diastole?
|
– Isovolumetric relaxation
– Rapid inflow – Diastasis and atrial systole |
|
|
Diastole
|
-begins with isovolumetric relaxation, when the aortic valve closes; the AV valves open as atrial pressure exceeds ventricular pressure during the phase of rapid inflow, which is followed by diastasis and the phase of atrial systole, which completes ventricular diastole
|
|
|
The cardiac cycle (figure)
|
|
|
|
Initiation of normal cardiac cycle
|
– Is done by spontaneous generation of an action potential (AP) in the sinoatrial (SA) node
|
|
|
Where is the SA node located?
|
In the posterior wall of the right atrium near the superior vena caval opening
|
|
|
What is rhythmicity of the cardiac cycle related to?
|
– The less negative resting potential (-55 mV), and threshold potential of SA nodal fibers compared with ventricular muscle cells, as well as the inactivation of fast Na channels
|
|
|
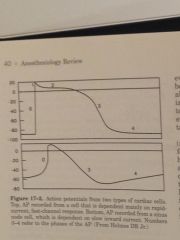
Action potentials from SA nodal cells and vebtricular cells
|
|
|
|
SA nodal fibers cycle
|
– SA fibers slowly leak sodium into cells and potassium out of cells, causing the resting potential to gradually rises during phase 4 depolarization until it reaches a threshold voltage of -40 mV, at which point slow calcium and sodium channels open, leading to an action potential
– A state of hyperpolarization then follows as K defuses out of fibers, dropping the resting membrane potential down to -55 mV at the termination of the action potential – Finally K channels close with inward leaking Na correcting outward flux of K, thus the resting potential drifts upward to threshold level (-40 mV), eliciting another cycle |
|
|
What allows the SA node to control the hearts rhythmicity?
|
– The depolarization rate of the SA node exceeds that of other parts of the cardiac conduction system, thus the SA node, or cardiac pacemaker, loses its state of hyperpolarization more rapidly than other parts
|
|
|
Rate of the SA node, AV node, and Purkinje fibers
|
– SA Node: 70 – 80 per minute
– AV node: 40 – 60 per minute – Purkinje fibers: 15 – 40 per minute |
|
|
Sympathetic nerve distribution in the heart
|
– Sympathetic nerves are distributed to all parts of the heart, especially the ventricular muscle
|
|
|
Effects of sympathetic stimulation on the heart
|
-increase the rate of SA nodal discharge
-increase the rate of conduction and excitability throughout the heart -increase the force of contraction of all cardiac musculature (max sympathetic outflow can triple the heart rate and double the strength of contraction) |
|
|
Mechanism of sympathetic activity on the heart
|
– Norepinephrine release at sympathetic nerve endings, which is thought to increase membrane permeability to Na and Ca, increasing the tendency of the membrane potential to drift upwards toward the threshold for excitation
-the increased Ca also causes increased chronotropic effect |
|
|
Distribution of parasympathetic nerves in the heart
|
– Mainly distributed via the vagus nerve to the SA and AV nodes, and to a lesser extent the age Rihanna and an even lesser extent the ventricles
|
|
|
Effect of parasympathetic's on the heart
|
– Cause release of acetylcholine which:
1. decreases the rate of SA nodal discharge 2. decreases the excitability of AV junctional fibers, thus slowing the impulse transmission into the ventricles |
|
|
What can strong vagal stimulation due to the heart?
|
– Can completely stop SA nodal discharge, leading to eventual ventricular escape beats from Purkinje fiber discharge
|
|
|
Effect of acetylcholine on cardiac fibers
|
– Increases the permeability of muscle fibers to K, producing hyperpolarization (increased negativity inside the cells, -70 – -75 mV), thus conduction tissue is much less excitable and takes longer to reach threshold potential
|
|
|
Central nervous system control of the cardiac cycle
|
– The vasomotor center, medullary – pontine area, contains neurons that affect chronotropic and inotropic responses from the heart
– Vagal activity is reflex in origin and is due to impulses from carotid and aortic baroreceptors -the nucleus ambiguous contains vagal motor neurons that travel to the SA and AV notes, and impulse activity depends mainly on baroreceptor |
|
|
Last way the CNS affects the heart
|
– From phasic input from the inspiratory center which causes sinus arrhythmias: increased heart rate with inspiration, decreased heart rate with expiration
|
|
|
Synchronized cardiac conduction
|
– An action potential originates in the SA node, And spreads through the atrium at 0.3 m/s, terminating in the AV node (1 m/s); the impulse reaches the AV node 0.04 s after originating in the SA node; Purkinje fibers then lead from the AV node and divide into left and right bundle branches, spreading into the apex of the respective ventricles and then back toward the base of the heart
|
|
|
What is the purpose of the delay at the AV node?
|
– It allows time for the atria to empty before the ventricle contracts
– it also helps prevent dysrhythmias which can occur if a second cardiac impulse is transmitted into the ventricle too soon after the first |
|
|
Purkinje fiber conduction velocity
|
-large fibers with a conduction velocity of 1.5-4 m/s (6 times that of cardiac muscle and 150 times that of junction all fibers); this allows almost immediate transmission of cardiac impulses throughout the entire ventricle, allowing almost all portions of the ventricle to contract simultaneously, with the first ventricular muscle fibers being excited only 0.06 seconds I had of the last ones
|

