![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
41 Cards in this Set
- Front
- Back
|
What two compartments do the pelvic floor separate? |
Main pelvic cavity superiorly and perineum inferiorly |
|
|
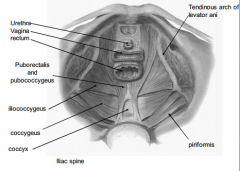
What is the pelvic floor composed of? |
The diaphragm is formed by levator ani
Incomplete anteriorly – urethra and vagina |
|
|
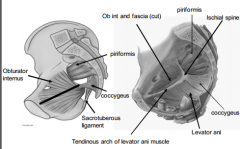
Remember this diagram |
|
|
|
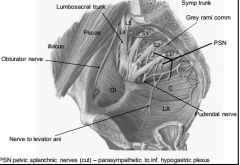
Remember the sacral plexus in relation to the pelvic floor. |
|
|
|
What are the anatomical components of the levator ani and their origins and insertions? |
• Sphincter vaginae |
|
|
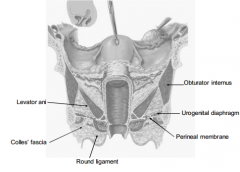
Describe the female pelvic floor when viewed superiorly. |
|
|
|
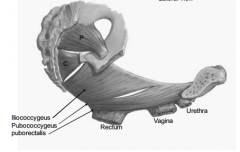
Be able to describe the order from superior to inferior of the pelvic floor muscles when viewed laterally - female. |
|
|
|
What is the function of the levator ani? |
• Supports and maintains pelvic viscera in |
|
|
What are the anatomical features of the ureter? |
• Retroperitoneal, muscular tubes |
|
|
What are the anatomical features of the bladder? |
• Extraperitoneal
|
|
|
What is the clinical relevance of the pouch of Douglas? |
– Accumulation of blood or pus |
|
|
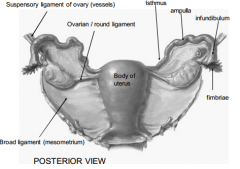
Describe the ligaments of the female reproductive system. |
|
|
|
What are the remnants of the gubernaculum in females and what do they connect? |
• Ovarian ligament (cranial gubernaculum) – Ovary to uterus • Round ligament of uterus - can be source of pain in pregnancy if tight - caudal gubernaculum). – Uterus to labium majorum via inguinal canal |
|
|
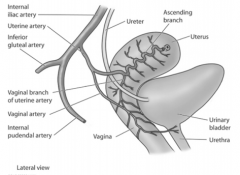
Describe the anatomy of the blood vessels supplying the uterus. |
|
|
|
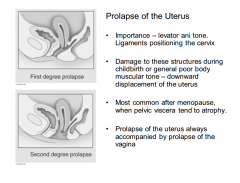
What supports does the uterus have? |
• Levator ani muscles and the perineal body |
|
|
What are anatomical features of the vagina? |
• Thin muscular tube extending backwards from the vulva to the uterus |
|
|
What are the anatomical relations of the vagina? |
Relations of the Vagina |
|
|
Describe the pelvic floor when viewed sagitally. |
|
|
|
What is in the female superficial perineal pouch? |
• 3 masses of erectile tissue |
|
|
Describe the deep and superficial dissections of the perineum. |

|
|
|
What is the anatomical relevance of the perineal body in females? |
• Perineal Body
|
|
|
What occurs upon injury to the pevlic floor during pregnancy? |
• Difficult childbirth – levator ani muscles fail |
|
|
Describe first and second degree prolapse of the uterus and the muscles that resist this. |
|
|
|
What enters the pudendal canal? |
• Pudendal nerve branch of the sacral plexus
|
|
|
Describe the nerves that cover the pubic area in women. |
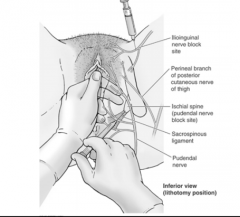
Remember ischial spine is site of pudendal nerve blockade |
|
|
What are general visceral afferents? |
• Visceral afferents conduct impulses from
|
|
|
How do GVA impulses reach the spinal cord? |
• GVA impulses reach the spinal cord through |
|
|
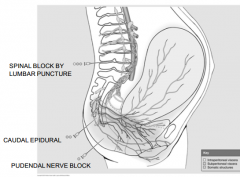
What are the characteristics of spinal anaesthesia? |
– Subarachnoid space L4-5. Complete anaethesia
|
|
|
What are the characteristics of pudendal nerve block? |
– Peripheral nerve block S2-4 – perineum and lower ¼ vagina – mother can feel/assist contractions |
|
|
What are the characteristics of caudal epidural block? |
– Anaesthetic administered to catheter in sacral canal (but must be done in advance). More anesthetic can be administered if necessary, limbs still unaffected
Affects the pelvic SPLANCHNIC nerves - during childbirth still have abdominal muscles and can move leg as legs - lumbar and upper sacral |
|
|
Describe the sites of administration of the above mentioned anaesthetic blocks. |
|
|
|
What is the function of the obturator internus? |
Lateral rotation of the hip - attachment to greater troch
+ fascia allows attachment tendinous arch of levator ani to ischial spine - pelvic floor attachment |
|
|
Where does the sciatic nerve emerge? |
Inferior to the pirirformis |
|
|
Where does the sciatic nerve emerge? |
Inferior to the pirirformis |
|
|
What is the route of the pudendal nerve? |
Deep to the pelvic floor |
|
|
What is the broad ligament? |
Double folded sheet of peritoneum. Aka mesometrium Connects uterus to walls and floor of pelvis |
|
|
What is the suspensory ligament of the ovary? |
Carries ovarian vessels Ovary to walls of pelvis |
|
|
Describe the blood vessels of the pelvis. |
Bifurcation of abdo aorta Bifurcation int and ext iliac. Lots of lumbar venous plexi cf sacral fracture |
|
|
Where does the ovarian artery come from? |
L2 near renal arteries Nb anastomoses with uterine artery |
|
|
What is the relevance of water under the bridge? |
0.5-2% of hysterectomies/routine uterine surgeries damage Ureter - only covered by slight amount of peritoneum Check for extravasation of urine |
|
|
What is the clinical significance of a retroverted/retroflexed uterus? |
Painful intercourse - cervix is directly facing vagina |

