![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
178 Cards in this Set
- Front
- Back
|
where is the heart located 1. in the 2. superior to the 3. anterior to the 4. posterior to the 5. between the |
1. mediastinum 2. diaphram 3. vertebral column 4. sternum 5. lungs |
|
|
1. weight of the heart 2. length in cm of the heart 3. where is the heart on the ribs |
1. 250-350 grams 2. 12-14 cm 3. 2nd rib to the 5th intercostal space |
|
|
what is the heart inclosed in |
a double walled sac
|
|
|
what are the layers of the CT linings of the heart |
1. outer fibrous pericardium 2. inner serous pericardium 3. parietal layer 4. visceral layer
|
|
|
fibrous pericardium |
outer 1st layer of the heart that protects, anchors, and prevents over filling |
|
|
serous pericardium |
2nd layer of the heart that contains the parietal layer and visceral layer |
|
|
parietal layer |
underlines the fibrous layer and folds over to form the visceral layer
|
|
|
visceral layer |
also called the epicardium, contains 2 layers with stuff in between them. It's directly over the heart tissue |
|
|
pericardial cavity |
found in between the parietal layer and the visceral layer that contains serous fluid for lubrication |
|
|
serous fluid |
found in the pericardial cavity for lubrication during contraction |
|
|
pericarditis 1. what is it 2. what does it lead to 3. how is it found 4. what can it cause |
1. inflammation of the pericardial cavity 2. reduced serous fluid and friction 3. able to be heard w/ a stethoscope 4. adhesions, fluid retention, and pressure or restriction of movement |
|
|
define cardiac tamponade |
when the heard cannot properly move because of pressure or restriction |
|
|
What are the cardiac layers |
1. epicardium (visceral layer) 2. myocardium 3. endocardium
|
|
|
myocardium |
made of cardiac fibers connected by a CT fibrous skeleton made of collagen and elastin |
|
|
CT skeleton |
made of collagen and elastin and acts as anchors for cardiac fibers
|
|
|
what does the myocardium functionally do |
insulates atria and ventricles |
|
|
Endocardium |
inner most lining of the heart/ touches the heart tissue |
|
|
atria |
one of the 2 types of chambers in the heart, the top 2 chambers
|
|
|
inreratrial septum |
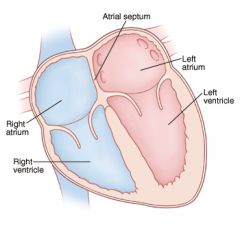
internally separates the 2 atria and is electrically conductive |
|
|
inner posterior surface |
somewhat smooth in appearance |
|
|
pectinate muscles |
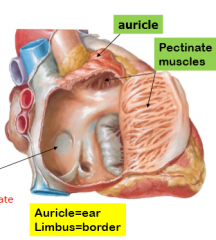
rigid muscles on the anterior wall of the heart |
|
|
cristae terminalis |
separates the regions in the heart |
|
|
fossa ovalis |
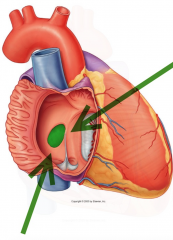
the depression in the interatrial septum
|
|
|
fossa ovalis in a fetus |
called the foramen ovale |
|
|
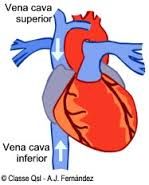
right atrium |
receives de-oxgenated blood from the superior and inferior vena cava and the coronary sinus |
|
|
location of superior vena cava |
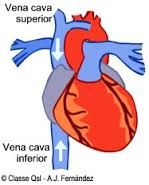
superior to the the diaphragm |
|
|
location of the inferior vena cava |
inferior to the diaphragm |
|
|
coronary sinus |

vein coming from the myocardium |
|
|
left atrium |
receives oxygenated blood from the 4 pulmonary veins |
|
|
interventricular septum |
separates the 2 ventricles |
|
|
atriovetricular groove/coronary sulcus |
marks the boundaries of the atria from the ventricles and by circling the heart and contains the coronary arteries |
|
|
define coronary arteries |
veins that go to the myocardium |
|
|
anterior and posterior inter-ventricular sulci |
marks the boundaries between the left and right ventricles and contain the inter ventricular arteries/veins |
|
|
papillary muscles |
valves that project into the cavity and discharge blood |
|
|
Pulmonary circuit |
the right side carries deoxygenated blood rom tissues to the heart to the lungs |
|
|
pulmonary circuit route |
venules, veins, superior and inferiour vena cava, right atria, right ventricle, pulmonary arteries, capillaries, lungs
|
|
|
systematic circuit |
left side carries oxygenated blood from the alveoli to the heart to the body tissues |
|
|
systematic circuit route |
venules, pulmonary veins, left atrium, left ventricle, aorta, material tree, capillaries, cells |
|
|
why is the left ventricle larger? |
to accommodate for the larger requirements |
|
|
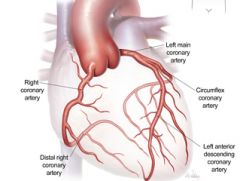
coronary arteries 1. comes from what 2. lies where |
1. the systematic circuit 2. atrioventricular grove |
|
|
left coronary |
runs left and divides into the anterior inter ventricular artery and the circumflex artery |
|
|
anterior interventricular artery |
supplies interventricular septum and anterior walls of ventricles |
|
|
circumflex artery |
supplies left atrium and posterior left ventricle q |
|
|
right coronary |
runs right and divides into marginal artery and posterior interventriular artery |
|
|
marginal artery |
supplies the lateral right |
|
|
posterior interventrical artery |
runs toward the apex, supplies the posterior ventricles, and connects with the anterior inter ventricular artery |
|
|
cardiac veins |
collect the venous blood and forms the coronary sinus |
|
|
coronary sinus |
delivers blood into the right atrium via the great cardiac vein, middle cardiac vein, small cardiac vein, and anterior cardiac vein
|
|
|
anterior cardiac veins |
empties directly into the atrium
|
|
|
what is/ causes ischemia |
a reduced coronary supple that causes the symptoms of angina pectoris |
|
|
ischemia in males |
pain in the left pectorals with radiation into the left axilla and arm |
|
|
ischemia in females |
similar to males or stomach pain with nausea |
|
|
what can ischemia cause |
blockages, cell death, infarct, and the heart attack |
|
|
treatment for ischemia |
by pass surgery and stints |
|
|
by pass surgery |
allows closed and blocked arteries to be replaced by veins taken from a patient thighs |
|
|
stints |
mesh like structures inserted into closed arteries which expand and restore normal lumen and flow |
|
|
atrioventricular valve |
prevent backlash of blood into the atria during ventricular contraction |
|
|
right atrioventricular valve |
called the tricuspid valve and has 3 flaps |
|
|
left atrioventricular valve |
called the bicuspid/mitral valve and has 2 flaps |
|
|
chordae tendinae |
anchors atrioventricular valve to the papillary muscles to prevent flaps from folding into the atria |
|
|
Mitral Valve Prolapse |
fluttering dysfunction of the valve flaps (chords tendinae) that is associated with stress |
|
|
semilunar valve function |
prevents backlash into the ventricles |
|
|
semilunar valves |
pulmonary and aortic |
|
|
flaps during contraction |
open in to the pulmonary artery and aorta |
|
|
flaps during relaxation |
the back flow of blood closes them |
|
|
cardiac muscle |
striated, a-mitotic, brach, uninucleate |
|
|
intercalated discs
|
how cardiac muscle cells are connected |
|
|
desmosome |
type of intercalated disc that prevent separation |
|
|
gap junction |
type of intercalated disc that allows the passage of ions and facilitates the contraction of cells in the same chamber |
|
|
endomysium |
connects cells to CT skeleton acting as an origin and insertion for cells to anchor to |
|
|
does cardiac muscle have capillaries |
yes an extensive network intermeshed |
|
|
mitchondria |
large ones branched in myofibrils |
|
|
functional syncytium |
describing cardiac muscle because it acts as a single unit |
|
|
autorythmic/ automatic cardiac fibers |
the 1% of cardiac cells that are self excitable and can initiate their own depolarizations to help pace the heart |
|
|
define nerve stimulation |
the skeletal requirement of having all the cells in a chamber to contract as an organ or not at all |
|
|
refractory period |
as long as contract to ensure claim is cleared from the sarcomeres |
|
|
effects of ischemia 1. cannot function properly in __ 2. rising levels of __ 3. low level of ___ 4. inhibited ____ synthesis |
1. anaerobic conditions 2. lactic acid 3. pH 4. ATP
|
|
|
effects of ischemia 1. ___pump fails 2. ___ and ___ levels rise 3.___ junctions close 4. cells |
1. calcium 2. calcium and H+ 3. gap 4. electrically isolating |
|
|
effects of ischemia 1. ischemia areas 2. ___ of electrical conduction 3. chamber failure 4. injured cells release |
1. infarcts 2. irregularities 3. heart attack 4. creatine kinase
|
|
|
is heart contraction intrinsic or extrinsic? |
intrinsic
|
|
|
is heart contraction independent or dependent of the CNS?
|
independent |
|
|
what is the heart controlled by? |
the extrinsic factors of the CNS and ANS |
|
|
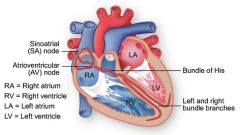
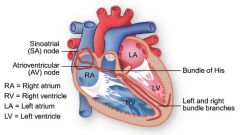
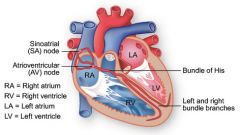
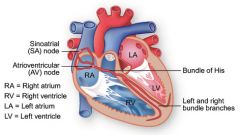
intrinsic cardiac conduction system components |
composed of the 1% authrythmic cells (senatorial node, atrioventricular node, atriavetrcular bundle of his, left and right bundle, purkinje fibers) |
|
|
autorythmic cells |
has their own rate of depolarization |
|
|
sinoatrial node |
to the right of the atria wall and inferior to the vena cava |
|
|
atriovenricular node |
inferior to the interatrial septum and above the bicuspid |
|
|
atrioventricular bundle of his |
inferior to the interatrial septum and splits into left and right |
|
|
right and left bundle branches |
interventricular septum towards apex |
|
|
purkinje fibers |
interventricular septum into the apex and superior into the ventricular walls |
|
|
function of the intrinsic cardiac condition system |
initiate and distribute impulses through out the heart to ensure proper depolarization and contractions |
|
|
pacemaker potential (pre potential) |
sine the autorythmic cells have an unstable resting potential, K+ and Na+ leak into the channels allowing the membrane to drift towards threshold |
|
|
what does the pacemaker potential cause |
a drop in electronegativity which opens the Ca+ gates |
|
|
what is the dominant autorythmic group |
the sinoatrial node |
|
|
when does the sinoatrial node depolarize |
100/min |
|
|
what does the sinoatrial node create? |
the sinus rhythm |
|
|
what role does the sinoatrial node play in the sequence |
depolarization wave spreads via the gap junctions and the inernodal pathway to the atria and atrioventricular node |
|
|
what role does the atrioventricular node play in the sequence |
its the place where impulse delay allows for the atria to contract |
|
|
what role does the atrioventricular bundle of his play in the sequence?
|
since the atria and ventricles aren't connected by gap junctions, the electrical connection conducts the depolarization wave to the right and left bundle branches |
|
|
what role do the purkinje fibers play in the sequence? |
they contract papillary muscles prior to ventricular contraction |
|
|
how long does the intrinsic conduction system take? |
220 ms |
|
|
define arrythias |
uncoordinated atrial and ventricular contractions |
|
|
types of arrhythmias |
fibrillation, ectopic focus, and heart block |
|
|
define fibrillation |
where there is a rapid, irregular phase of contractions resulting in no pumping and defibrillation depolarizes the myocardium by shocking to reset the sinoatrerial node establish a sinus rhythm |
|
|
define ectopic focus |
when an abnormal pacemaker takes control making the nodes junction rhythm at 40-60/min and having small excitable regions |
|
|
define premature ventricular contractions |
when the heart has small excitable regions due to caffeine or nicotine and generating impulses faster than the nodes rhythm |
|
|
what is a heart block |
damage to the atrioventricular node preventing impulses from reaching the ventricles causes them to beat on their own at about 30/min |
|
|
what is the treatment for a heart block |
an artificial fixed rate pacemaker |
|
|
what is a partial heart block |
when the heart stop transmitting on its own requiring a pace maker |
|
|
what 2 components make up the extrinsic controls of the heart |
the sympathetic and parasympathetic |
|
|
sympathetic sequence |
cardioaccelatory center of medulla > lateral horn of T1-T5 > cervical and thoracic chain > postganlionic fibers > senatorial node and atrioventricular node |
|
|
parasympathetic |
cardioinhibitory center of the medulla > vagus CN X > postganglionic > sinoatrial node and atrioventricular node |
|
|
EKG |
composite of all action potentials generated by nodes and contractile cells |
|
|
leads of EKG |
creates picture of electrical conductivity noted as deflection waves |
|
|
P wave |
senatorial through the atria creating depolarization followed by atrial contraction that takes .08 seconds |
|
|
increase in the p wave |
an enlarged atrium |
|
|
QRS complex |
ventricular depolarization and atrial depolarization that takes .08 seconds |
|
|
Increased Q wave |
infarct
|
|
|
Increased R wave |
enlarged vent |
|
|
T wave |
ventricular depolarization that takes .16 seconds |
|
|
increased T wave |
hyperkalemia |
|
|
T wave indication |
ischemia |
|
|
P-Q interval |
start of atrial excitation through ventricular excitation that takes .16 seconds |
|
|
lengthened P-Q interval |
coronary artery disease |
|
|
S-T interval |
action potential plateau and the entire myocardium is depolarized |
|
|
S-T interval elevated above base line |
infarct |
|
|
S-T interval depressed below base line |
ischemia |
|
|
Q-T interval |
ventricular depolarization through repolarization |
|
|
lengthened Q-T interval |
ischemia |
|
|
systole |
contraction |
|
|
diastole |
relaxation |
|
|
ventricular filling |
refers to mid-late diastole |
|
|
steps in ventricular filling |
1. open atrioventricular valves for 70% of ventricular filing allowing passive flow through atria 2. atria depolarizes and contacts allowing final 30% into ventricles 3. atria distole and ventricles depolarize |
|
|
ventricular systole |
ventricular contraction
|
|
|
steps in ventricular systole |
1. ventricles contract 2. pressure builds in the atrioventricular valves until it exceeds the pressure of the arteries 3. semilunar valves are forced open |
|
|
isovolumetric contraction phase |
when the pressure builds in the atrioventricular valves |
|
|
ventricular ejection phase |
when the semilunar valves are forced open giving the normal blood pressure of 120 mmHg |
|
|
isovolumetric relaxation |
early diastole/ ventricular repolarization |
|
|
steps in isometric relaxation |
1.the pressure drops to allow arterial blood to back lash 2. the pressure increases to shut the semilunar valves 3. atrial fillings build pressure until it exceeds the pressure of the ventricles pressure 4. atrioventricular valves open 5. ventricular filling beings
|
|
|
total time for a heart to beat/complete a full cycle |
.8 seconds |
|
|
what are the heart sounds created by? |
the closing of the valves |
|
|
what is the 1st sound the heart makes |
the atrioventricular valves shutting in the beginning of systole during the QRS |
|
|
what is the 2nd sound the heart makes |
the semilunar valves shutting in the beginning go the ventricular diastole during the T wave
|
|
|
define cardiac output |
the total amount of blood propelled by the heart per minute |
|
|
stroke volume equation |
=total volume after filling-residual volume after contraction
=end diastolic volume - end systolic volume
|
|
|
what should the stroke volume equal |
70 ml (60% of the blood being ejected)
=120ml - 50ml
|
|
|
how many liters per minute does the heart pump out |
50 L/minute |
|
|
what 3 factors can affect stroke volume |
1. preload 2. contractility 3. afterload
|
|
|
define preload |
also called the frank starling law, is the ventricular stretch |
|
|
steps in preload |
1. increase in venous blood return 2. increase in end diastolic volume 3. increased cardiac stretch 4. increased actin-myosin cross bridging 5. muscle contraction tension |
|
|
contractility |
an increase in contractile strength as a function of enhanced Calcium influx resulting from sympathetic stimulation |
|
|
what is after load |
arterial resistance |
|
|
afterload volumes |
8mmHg in the pulmonary 80mmHg in the aortic |
|
|
epinephrine |
comes from the adrenal medulla and is part of the sympathetic nervous system |
|
|
thyroxine |
effects are longer and are sustained |
|
|
ions found in the heart |
calcium, potassium, and sodium |
|
|
hypocalcemia |
low levels of calcium in the body that reduces heart function |
|
|
hypercalcemia |
high levels of calcium in the blood that causes spastic heart contractions |
|
|
hypernatremia |
high levels sodium that inhibits calcium transport and muscle contraction |
|
|
hyperkalemia |
high level of potassium that lowers resting potential leading to heart block and cardiac arrest |
|
|
hypokalemia |
low level of potassium that leads to weakness and abnormal rhythm |
|
|
tachycardia |
describes a heart that beats more than 100 beats per minute |
|
|
bradycardia |
describes a heart that beats less than 60 beats per minute |
|
|
congestive heart failure |
reduction in cardiac output caused by various things causing dysfunction and degeneration of the myocardium |
|
|
pulmonary congestion |
left side heart failure when blood backs up engorging the pulmonary capillary bed causing pulmonary edema |
|
|
peripheral congestion |
right side heart failure when blood backs up in the venous system causing edema in ankles and organs |
|
|
digitalis |
medicine that is a diuretic and reduces heart rate and blood pressure |
|
|
23rd day of fetus |
the 2 tubes fuse into a single pumping chamber |
|
|
25th day of fetus |
4 primitive chambers differentiate 1. sinus venosus 2. atrium 3. ventricle 4. bulbus cordis |
|
|
2nd month of fetus |
fully developed expect for foramen oval and ductus arteriosus |
|
|
foramen ovale |
pushes blood from right atrium to left atrium skipping the pulmonary circulation and closes after birth leaving the fossa ovale |
|
|
ductus arteriosus |
pushes blood from the pulmonary trunk to the aorta and closes after birth leaving the ligamentum arteriosum |
|
|
what are some congenital defects |
atrial septal defects, patent ductus, ventricle septal defects, coarctation of the aorta, tetralogy of fallot, and cyanosis |
|
|
atrial septal defects |
when the foramen ovale doesn't close causing mixed blood |
|
|
patent ductus |
when the ductus arteriosus doesn't close causing mixed blood |
|
|
ventricular septal defect |
when the septum doesn't form causing mixed blood |
|
|
coarctation of the aorta |
the narrowing of the aorta (stenosis) causing the heart to pump the blood harder |
|
|
tetralogy of fallot |
4 defects of the heart all occuring at once |
|
|
cyanosis |
bluish color of the skin resulting from poor circulation of blood/ common symptom |

