![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
117 Cards in this Set
- Front
- Back
|
What are the 5 functions (processes) of the digestive system?
|
Ingestion
Mechanical processing Digestion Absorption Excretion |
|
|
ingestion
|
taking in of liquid or solid food
|
|
|
mechanical processing
|
crushing or shearing of food that does NOT change it chemically
|
|
|
digestion
|
chemical breakdown of food via catabolic reaction
|
|
|
absorption
|
moving nutrients from digestive tract to the blood and/or lymph
|
|
|
excretion
|
removal of waste materials
|
|
|
What are the 4 layers of the digestive wall, starting from the innermost layer?
|
Mucosa
Submucosa Muscularis externa Serosa |
|
|
Describe this digestive layer: mucosa. (2)
|
Touches food
Primary epithelium (nonvascular) |
|
|
Describe this digestive layer: submucosa. (4)
|
Dense, irregular connective tissue
Blood vessels Sensory neurons Glands (exocrine) |
|
|
Describe this digestive layer: muscularis externa. (4)
|
Thick bunch of muscle fibers
Smooth muscle (involuntary) Circular and longitudinal layer Performs peristalsis |
|
|
Describe this digestive layer: serosa.
|
Visceral serous membrane
|
|
|
What are the 2 accessory organs of the small intestine?
|
Liver
Pancreas |
|
|
Are the salivary glands digestive organs or accessory organs?
|
Accessory organs
|
|
|
peristalsis
|
combined circular and longitudinal smooth muscle contraction used to move bolus
|
|
|
mesenteries
|
folded sheets of peritoneum that hold intestines together and anchor them to body wall
|
|
|
peritonitis
|
inflammation of the peritoneal membrane; life-threatening and most common killer
|
|
|
peritoneum
|
transparent tissue that lines abdominal cavity
|
|
|
Extrinsic regulation of the digestive system is controlled by what two systems?
|
Nervous system
Endocrine system |
|
|
What does the hard palate allow us to do?
|
Breathe and chew simultaneously
|
|
|
What is the purpose of chewing?
|
Increase surface area by breaking food down into smaller pieces
|
|
|
deglutition
|
moving a bolus from the oral cavity into esophagus; act of swallowing, esp. food
|
|
|
What kind of epithelia is the oral cavity lined with?
|
Stratified squamous epithelia
|
|
|
gomphosis
|
peg joint that holds teeth in place
|
|
|
periodontal ligament
|
group of specialized connective tissue that hold tooth inside its bony socket
|
|
|
cementum
|
bony matrix that helps to hold teeth in place at the root
|
|
|
What is the hardest biologically-made substance?
|
Enamel
|
|
|
Where are dentin and enamel made?
|
From living cells in pulp cavity
|
|
|
dentin
|
mineralized matrix, like bone, that surrounds pulp cavity; below enamel
|
|
|
enamel
|
hard, white outer layer of the tooth; crystallized version of calcium phosphate
|
|
|
gingiva
|
tissue of the jaws that surround the base of teeth; gums
|
|
|
What are the 3 types of teeth discussed in class?
|
Incisors
Canines (cuspids) Molars |
|
|
incisors
|
made to cut or bite off food
|
|
|
canines
|
human teeth with deepest root; made for tearing
|
|
|
molars
|
flat tops for chewing and grinding
|
|
|
bolus
|
already chewed up and salivated on food
|
|
|
What are 3 phases of deglutition?
|
Buccal phase
Pharyngeal phase Esophageal phase |
|
|
Identify what occurs during the following phase of deglutition.
Buccal |
Push bolus against hard palate, past soft palate, and back (into pharynx)
|
|
|
Identify what occurs during the following phase of deglutition.
Pharyngeal |
Swallowing reflex from swallowing center (of brain) pushes bolus into esophagus
|
|
|
Identify what occurs during the following phase of deglutition.
Esophageal |
Peristalsis moves bolus toward stomach
|
|
|
How long is the esophagus?
|
25 cm (10 in.)
|
|
|
What kind of epithelium is the esophagus made of?
|
Stratified squamous epithelium
|
|
|
What is the volume of a stomach, generally?
|
1.5 liters
|
|
|
fundus
|
large, hollow dome top of an organ
Note: Uterus and stomach both have a fundus. |
|
|
cardiac sphincter
|
the circular muscle that precedes the stomach
|
|
|
TRUE or FALSE
Every entrance and exit to the digestive system has a sphincter. |
TRUE
|
|
|
What are the 3 muscular layers of the stomach?
|
Circular
Longitudinal Oblique (*) |
|
|
rugae
|
folds in the stomach muscosa that allow it to expand
Note: Also found in the bladder |
|
|
gastric pit
|
deep, narrow crevices that make up the opening of a gastric gland
|
|
|
What is the stomach lining made of?
|
Gastric pits with glands in them line the stomach and secrete gastric juice
|
|
|
What are the 3 types of cells that line the gastric pit (gland)?
|
Parietal cells
Endocrine cells Chief cells Tip: PEC |
|
|
What type of cell are those that line the gastric pit (gland)?
A. Simple cuboidal B. Simple columnar C. Stratified squamous D. Stratified columnar |
Simple columnar
|
|
|
In the gastric pit (gland), what function does the following cell have?
Parietal cell |
Make stomach acid (hydrochloric acid or HCl)
|
|
|
In the gastric pit (gland), what function does the following cell have?
Chief cell |
Make enzymes, such as pepsinogen
|
|
|
In the gastric pit (gland), what function does the following cell have?
Endocrine cell |
Make several hormones
|
|
|
What is the main function of the small intestine?
|
Nutrient absorption
|
|
|
How long is the small intestine?
What is width of the small intestine? |
20-22 ft.
1 in. |
|
|
What are the 3 parts of the small intestine and how long are they?
|
Duodenum, 10 in.-1 ft.
Jejunum, 8 ft. Ileum, 12 ft. Tip: Remember order by this phrase: "Don't Jump In". |
|
|
plicae circulares
|
permanent folds in the small intestine covered with villi, which are in turn covered with microvilli
|
|
|
Where do nutrients absorbed in the small intestine go?
|
Capillary network and lacteal, located inside villi
|
|
|
Which type of cell are the villi on the plicae circulares lined with?
|
Simple columnar epithelial cell
|
|
|
Where does the large intestine begin?
|
At the cecum in the lower left quadrant, near appendix
|
|
|
cecum
|
a dead end pouch in the digestive system where material can go one way or the other
|
|
|
What is the more common name for the large intestine?
|
Colon
|
|
|
What are the 4 parts of the large intestine?
|
Ascending colon
Transverse colon Descending colon Sigmoid colon |
|
|
taenia coli
|
bands of longitudinal smooth muscle found on the large intestine
|
|
|
Describe the lining of the large intestine.
|
Simple columnar epithelia with goblet cells.
|
|
|
What is it that you eat?
|
Food
|
|
|
What do you swallow?
|
Bolus
|
|
|
What goes into the small intestine?
|
Chyme
|
|
|
What comes out of your large intestine?
|
Feces
|
|
|
What human body structure changes food into a bolus?
|
Oral cavity
|
|
|
What organ changes a bolus into a chyme?
|
Stomach
|
|
|
What organ changes chyme into feces?
|
Large intestine (colon)
|
|
|
How does the large intestine change chyme into feces?
|
It takes the water out of it
|
|
|
cirrhosis
|
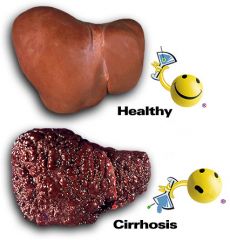
buildup of scar tissue and nodules in the liver that interfere with its function; commonly caused by chronic alcoholism
|
|
|
emesis
|
vomiting
|
|
|
hepatitis
|
inflammation of the liver usually caused by a virus; 5 types A-E
|
|
|
diverticulosis
|
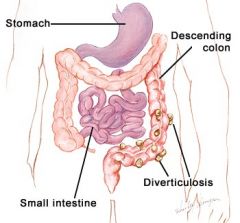
condition that occurs when small pouches (diverticula) push outward through weak spots in the colon
|
|
|
diarrhea
|
frequent, watery bowel movements
|
|
|
gastric ulcer
|
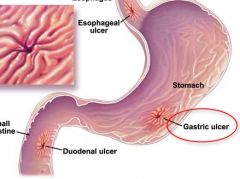
sore that erodes the lining of the stomach
|
|
|
What extra layer of muscle does the stomach have compared to similar digestive organs?
|
Oblique layer
|
|
|
How do parietal cells make stomach acid (HCl)?
|

|
|
|
What are the 3 phases of gastric secretion?
|
Cephalic
Gastric Intestinal |
|
|
What prompts the cephalic phase of gastric secretion?
|
CNS via sight/smell/thoughts of food
|
|
|
What is the purpose of the cephalic phase?
|
Prepares the stomach for a bolus
|
|
|
How does the cephalic phase prepare the stomach for a bolus? (3)
|
Makes more mucus
Releases pepsinogen and HCl Stimulates gastrin |
|
|
gastrin
|
hormone that stimulates production of acids and enzymes; increases motility
|
|
|
What initiates the gastric phase of gastric secretion?
|
Arrival of the bolus in the stomach
|
|
|
When does the cephalic phase subside?
|
When you realize you are not getting any food
|
|
|
What is the function of the gastric phase? (3)
|
Enhance secretions from cephalic phase
Homogenize and acidify chyme Initiate digestion of proteins by pepsin |
|
|
How does the gastric phase perform its function? (3)
|
Increase HCl and pepsinogen production
Increase motility Initiate mixing waves |
|
|
When a bolus arrives in the stomach during the gastric phase, what is the effect?
|
Distention
|
|
|
distention
|
bloating or swelling of the abdomen
|
|
|
homogenize
|
to blend or puree
|
|
|
What initiates the intestinal phase?
|
Chyme entering small intestine
|
|
|
What is the function of the intestinal phase? (2)
|
Control rate of chyme entrance into duodenum
Alerts liver and pancreas to start secreting hormones CCK, GIP, and secretin |
|
|
What occurs during the intestinal phase? (2)
|
Slowed HCl and pepsinogen production
Reduction in gastric motility |
|
|
How long is each phase of gastric secretion?
|
Cephalic = Minutes
Gastric = 3-4 hours Intestinal = Hours |
|
|
What stimulates cholecystokinin (CCK)?
|
Arrival of chyme containing lipids and partially digested proteins in duodenum
|
|
|
What are the 2 net effects of cholecystokinin (CCK)?
|
Increase the secretion of pancreatic enzymes
Push pancreatic secretions and bile into the duodenum |
|
|
What stimulates secretin?
|
Chyme arriving in the duodenum
|
|
|
What are the 3 primary effects of secretin?
|
Stimulate production of alkaline buffers
Increase rate of bile secretion Slow down gastric secretion and motility |
|
|
What initiates gastric inhibitory peptide (GIP)?
|
Arrival of chyme containing fats and carbohydrates in the duodenum
|
|
|
What are the 2 primary effects of gastric inhibitory peptide (GIP)?
|
Stimulate release of insulin from pancreas
Slow down gastric secretion and motility |
|
|
Identify the 2 functions of the liver pertaining to the digestive system.
|
Produce bile salts
Detoxify blood via hepatic portal system |
|
|
What connects the liver to the small intestine?
|
Gall bladder (a bile duct)
|
|
|
Describe the histology of the liver.
|
Each liver lobule has sinusoids that empty into its own central vein
|
|
|
Why does blood in the arteries and veins of a hepatic triad go in the same direction?
|
They are NOT corresponding arteries and veins
|
|
|
What are the 3 parts of a hepatic triad?
|
Branch of hepatic portal vein
Branch of hepatic artery proper Bile duct |
|
|
hepatic portal vein
|
large vein through which oxygen-depleted blood from the stomach, the intestines, the spleen, the gallbladder, and the pancreas flows to the liver
|
|
|
How does blood leave the hepatic portal system?
|
By way of hepatic veins that go to the inferior vena cava
|
|
|
Kupffer cells
|
free macrophages of the liver
|
|
|
What are the 2 digestive functions of the pancreas?
|
Produce pancreatic juice
Neutralize acidic chyme via HCO3- |
|
|
How acidic is the chyme coming out of the stomach?
|
pH 1.5 - 2
|
|
|
What produces the conscious urge to defecate?
|
Arrival of feces in the rectum
|
|
|
What is the 4-step process of the defecation reflex?
|
Distention
Stimulation of stretch receptors Increased peristalsis Relaxation of internal anal sphincter |
|
|
What is normal feces composed of?
|
75% H2O
5% Bacteria 20% Undigested material |

