![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
150 Cards in this Set
- Front
- Back
|
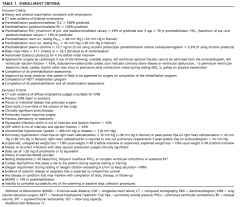
1. The insulation on the power cord of a piece of class 1 equipment is faulty such that the active wire is in contact with the equipment casing. What will happen when the power cord is plugged in and the piece of equipment is turned on |
E.
Class 1 – single insulation, has an earth connector that will divert energy if insulation fails and a fuse or RCD should disconnect power supply. Fuse exists within equipment supply line. However, rate that fuse breaks is still slower than RCD |
|
|
2. EZ99 According to the current ANZCA approved standards for labeling, the appropriate colour label for an intraosseous infusion is (some remember it saying INTERosseous, not intraosseous... possibly typo, possibly trick question) |
IA – Red |
|
|
PP102 An 8 year old 30kg girl presents for resection of a Wilms tumour. Her starting haematocrit is 35% and you decide that your trigger for transfusion will be 25%. The amount of blood that she will need to lose prior to transfusion is |
Answer: 600 ml (C) |
|
|
4. A 30 year-old pregnant patient develops contractions at 30/40 weeks gestation which of the following cannot be used for tocolysis
A. Clonidine B. Indomethacin C. Magnesium D. Salbutamol E. Nifedipine |
A Clonidine |
|
|
5. A patient known to have porphyria is inadvertently administered thiopentone on induction of anaesthesia. In recovery the patient complains of abdominal pain, prior to having a seizure and losing consciousness. Which drug should NOT be given? |
A
Pethidine due to nor pethidine lowering seizure threshold. |
|
|
6. A patient with HOCM presents with dyspnoea and angina on exertion. Which of the following is the best agent to treat these symptoms
A. Glycerol trinitrate B. Metoprolol C. Morphine D. Hydrochlorthiazide E. Salbutamol |
B
Beta blockade to reduce dynamic LV outlet obstruction and SAM |
|
|
7. A patient undergoes a femoral-popliteal bypass and has a mildly elevated troponin on day 1 post-operatively. They are otherwise asymptomatic with no other signs/symptoms of myocardial infarction and have an uneventful recovery. What do you do? |
A
From VISION study that demonstrated association between increased 30 day mortality with elevated post-op troponin |
|
|
8. A 40 year-old lady with a history of a bleeding diathesis presents for a tonsillectomy. What is the most likely cause? |
C.
Haemophilia B. All others are pro-coagulant disorders. Note X-linked disease. |
|
|
9. What is the most cephalad intervertebral space at which a spinal can be sited in a neonate where the risk of damage to the spinal cord is minimal
A. L1/2 B. L2/3 C. L3/4 D. L4/5 E. L5/S1 |
D
|
|
|
10. St John's Wort (Hypericum perforatum) potentiates the effects of
A. Dabigatran B. Heparin C. Warfarin D. Aspirin E. Clopidogrel |
E
Reduces the effect or warfarin/heparin/dabigatran. Little effect on aspirin. |
|
|
11. You are performing an awake fibreoptic intubation, through the nose, on an adult patient. In order, the fibrescope will encounter structures with sensory innervation from the following nerves |
D |
|
|
2. A patient is having an electrophysiological study and ablation for atrial fibrillation. Suddenly the blood pressure drops to 76/38 mmHg, with the heart rate at 110 in sinus rhythm. What is the best investigation to confirm the cause of hypotension? |
C.
EP Study risk of perforation atria/vessels. Troponin/ECG/Angio may miss hypovolaemia and surgical cause. Hence TOE best. |
|
|
13. Which is the most powerful predictor of atrial fibrillation post cardiac surgery. |
A |
|
|
14. A man with a history of Parkinsons disease has undergone uncomplicated general anaesthetic for a knee replacement but develops post-operative nausea and vomiting (PONV). He received 4mg dexamethsone intraoperatively as prophylaxis. What would you use to treat his PONV in recovery? |
E
Ondansetron best used in combination with Dexamethasone. Also most effective at rescue PONV. Droperidol should only be used if other therapies have failed. Do not readminister medications that have been used for prophylaxis |
|
|
15. Which of the following is of the least benefit in the treatment of severe anaphylaxis? |
E
Subcutaneous adrenaline not "stated" in guidelines. Nebulised salbutamol only useful if bronchospasm is part of presentation. |
|
|
16. A 70 year old patient is being treated for congestive cardiac failure. They are able to shower themselves and complete other ADLs but get dyspneoa on mowing the lawn. They are New York Heart Association classification |
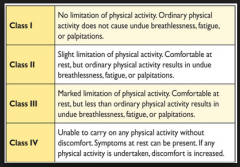
B
|
|
|
17. The percentage of post dural puncture headaches that would resolve spontaneously by 1 week is closest to |
B
70% by 1 week, 95% by 6 weeks. |
|
|
18. Which piece of airway equipment is designed for use with a fibreoptic bronchoscope |
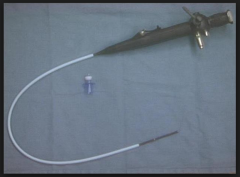
A |
|
|
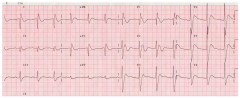
19. A 50 year old lady is seen at the pre-operative assessment clinic, she is on 150mg/day methadone, what is the most likely ECG change to be found in her pre-op ECG? |
B
Prolonged QTc |
|
|
20. Current guidelines regarding cardiopulmonary resuscitation include all of the following EXCEPT
A. Allow equal time for chest compression and relaxation B. Give 2 rescue breath before commencement of CPR C. Chest compression at 100bpm D. Chest compression should be at least 5cm depth E. Chest compression to breath ratio at 30:2 |
B
Refer to BLS, Resus guidelines |
|
|
21. When a 3 lead ECG is applied correctly in the CS5 position, you will monitor lead II when you suspect which of the following conditions |
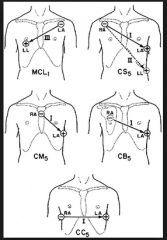
B
CS5 position: Lead I - anterior ischaemia Lead II - Inferior ischaemia + arrhythmia
Miller's |
|
|
22. You are anaesthetizing a 50 year old man who is undergoing liver resection for removal of metastatic carcinoid tumour. He has persistent intraoperative hypotension despite fluid resuscitation and intravenous octreotide 50 ug. The treatment most likely to be effective in correcting the hypotension is: |
E
|
|
|
23. Using the American Heart Association specification, the colours of the electrodes in a 3-lead electrocardiographic (yes the typo is what they used) is |
D
White is Right; Smoke over Fire |
|
|
24. When performing laryngoscopy using a Macintosh blade, your best view is of the patient's epiglottis touching the posterior pharyngeal wall. Using the Cormack and Lehane scale this is grade |
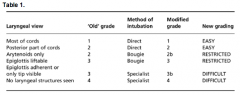
D
Cormack and Lehane further modified by Yentis & Lee to subdivide Grade II into IIa and IIb
Cook further subdivided Grade III into a & b as per chart in 1999 |
|
|
25. You are doing a supraclavicular brachial plexus block on an awake 35 year-old lady who is healthy with no significant past medical hsitory. Soon after injecting 20mLs of 0.375% ropivicaine she becomes agitated, has a seizure and loses consciousness. Your 1st step in management is |
D
ABCs first then treat seizure cause |
|
|
26. A G1P0 patient with a dilated cardiomyopathy and an ejection fraction (EF) of 35% presents for a caesarean section. The benefits of regional vs general anaesthesia are |
C
Increased ejection fraction |
|
|
27. A patient has a terminal malignancy. His family doesn’t want you to tell the patient about his diagnosis and prognosis. Your decision to inform him is an example of: |
A |
|
|
28. A septic patient has a CVP of 12mmHg, a blood pressure of 80/40mmHg and a pulse rate of 90/minute. Which is the best agent to treat their hypotension |
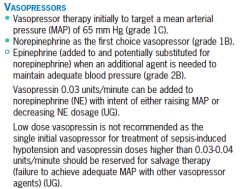
C
Refer to Surviving Sepsis Guidelines 2014
|
|
|
29. Which organ is least tolerant of ischaemia following removal for transplantation |
B
Removal of the organs is performed under cold protection by applying ice to the surgical field. Organs are removed according to their susceptibility to ischemia, with the heart first and the kidney last in a multiorgan donor.
Cold Ischaemia Time: Heart<Lung<Liver<Pancreas<Kidney<Cornea |
|
|
30. You are performing a TAP block. If the needle is correctly positioned where will you deposit the local anaesthetic |
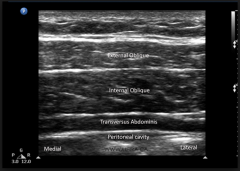
C
Deposit LA between Internal Oblique and Transversus Abdominus |
|
|
31. You are inserting a left sided double lumen tube into a 140kg 160cm woman. At what depth measured at the incisors is it most likely to be in the correct position |
D
2009 BJA Article 170cm = 29cm M = F, every +/- 10cm correlates to +/- 1cm |
|
|
32. A patient is cooled to 33 degrees Celcius in an attempt to improve neurological outcome after out-of-hospital ventricular fibrillation cardiac arrest. The evidence for this treatment comes from |
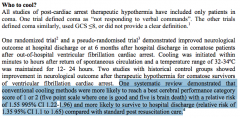
D
According to resus guidelines, one systematic review (which includes 2 RCTs) |
|
|
33. Which of the following decrease during pregnancy |
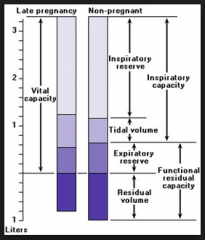
A
RV/FRC decreased IRV decreased TV increased RR increased VC same |
|
|
34. You are anaesthetizing a patient with chronic renal failure for removal of a Tenkoff catheter and have intubated using rocuronium at a dose of 1.2mg/kg. You are immediately unable to intubate or ventilate and you decide to reverse the patient with sugammadex. What dosage would you use
A. 2mg/kg B. 4mg/kg C. 8mg/kg D. 12mg/kg E. 16mg/kg |
E
Normal reversal = 2mg/kg Deep 4mg/kg Immediate reversal post RSI 16mg/kg |
|
|
35. During an elective thyroidectomy a patient develops symptoms consistent with the diagnosis of “thyroid storm” which of the following treatment options in NOT appropriate
A. Carbimazole B. Beta-blocker C. Propythiouracil D. Plasmaphoresis E. Hydrocortisone |
D |
|
|
36. A young female patient with anorexia nervosa, had just started eating again. After three days she develops dyspnea and is found to have cardiac failure. Which of the following is the most important to correct |
C Phosphate
|
|
|
37. A pregnant lady is undergoing neuroradiological coiling of a cerebral aneurysm. At what gestational age should you monitor foetal heart rate to ensure adequate uteroplacental blood flow
A. 20 weeks B. 24 weeks C. 28 weeks D. 30 weeks E. 32 weeks |
B
Fetal Viability from 24 weeks |
|
|
38. What is the mechanism of central sensitisation?
A. Increased intracellular magnesium B. Antagonism of the NMDA receptor C. Glycine is the major neurotransmitter involved D. Recurrent a-delta fibre activation E. Alteration in gene expression |
E
BJA recent article “When does acute pain become chronic?”
Intracellular Mg decreased (normally acts to block NMDA receptor) Increased NMDA-R activity in central sensitisation Glutamate is the major neurotransmitter Recurrent C-Fibre implicated in wind-up |
|
|
39. Which of the following is the best predictor of a difficult intubation in a morbidly obese patient |
A |
|
|
40. A female patient with a history of COPD presents for lung volume reduction surgery, which of the following is a contraindication for surgery (? indicates a poor prognosis) |
D or B (if stated giant bullous disease)
Poorer prognosis post-op if: FEV1 < 20% predicted DLCO < 20% predicted Homogenous Emphysema on CT Prednisolone > 20mg/d Contraindicated if: Giant Bullae Alpha 1 Antitrypsin Bronchiectasis/Clinically sig sputum load Pleural/Interstitial Disease Prev Lobectomy/LVRS Signif Pulm HT/Systemic uncontrolled HT
See NETT Trial |
|
|
41. A patient with known metastatic lung cancer is found to have hypercalcaemia, all of the following would help excretion of calcium except
A. Bisphosphates B. Calcitonin C. Frusemide D. Sodium Chloride E. IV crystalloids |
A
Bisphosphonates do not increase excretion per se. |
|
|
42.What potentiates/interacts with adenosine |
E
Dipyrimadole potentiates action of adenosine. Hence reduce does if treating SVT |
|
|
43. A 2 year-old child has just undergone strabismus surgery. They had an URTI 1/52 prior to surgery. They had an uneventful general anaesthetic with a 4.5mm cuffed ETT, was extubated and sent to recovery. 20 minutes later they develop respiratory distress. Their saturations are 96% on room air, and there is noticeable tracheal tug. What is the most appropriate initial management that will help with their respiratory distress |

B
Example of delayed respiratory distress, however maintaining oxygenation. Likely post-extubation stridor. Initial management to avoid agitation, as may exascerbate, definitive management would be nebulised adrenaline (0.5ml/kg 1:1000 up to 5ml)
Ref: Clinical Pediatric Anesthesia: Case-based Handbook |
|
|
44. Which antihypertensive is not safe to use in pregnancy |
B
ACEi contraindicated in pregnancy due to associations with foetal defects (including cardiac/renal failure/ growth restriction) |
|
|
45. Which has the weakest evidence for prevention of postoperative infection |
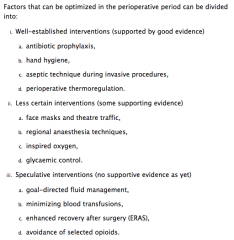
B
E option ambiguous (?Cessation smoking), otherwise smoking is a/w post-op wound infection
CEACCP 2011: Preventing Post Operative Infection: The Anaesthetist's Role |
|
|
46. During a cerebral aneurysm clipping, the anaesthetist can assist with the placement of the clip by giving the patient which drug immediately prior to clipping |
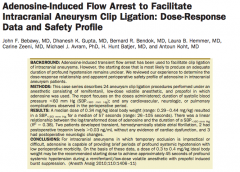
D
Adenosine 0.3-0.4mg/kg used for temporary circulatory standstill ,just prior to clipping aneurysm, lasting approx 45s
|
|
|
47. The POISE trial showed that the perioperative administration of metoprolol XR resulted in decreased |
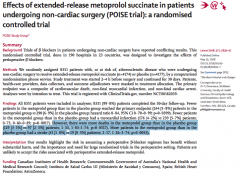
D |
|
|
48. In paediatric trauma, the Broselow tape is used to estimate |

B
Colour coding which correlates to height – approx weight and drug doses for each colour. |
|
|
49. Which of the following should be used by a lay person to indicate that they should commence CPR |
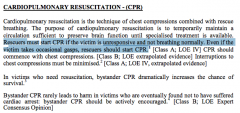
C
Difficult interpretation. Resus guidelines state unconscious and abnormal breathing (rather than absent). Little morbidity associated with CPR in unconscious patient, even if not required. |
|
|
50. A patient presents for dilation of a pharyngeal stenosis post laryngopharyngectomy 12 months earlier. After inducing anaesthesia you site a size 7 reinforced ETT in the stoma. Over the next 30 minutes the patient gradually desaturations. Despite hand bag ventilation and an increased FiO2 of 1 the saturations remain at 88%. This is due to |
A |
|
|
51. PiCCO determines cardiac output utilizing |
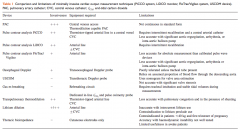
C
Both PiCCO and LiDCO use pulse contour analysis with thermodilution calibration
CEACCP 2011: Minimially Invasive Cardiac Output Monitors |
|
|
52. During scoliosis surgery with monitoring of somatosensory evoked potentials, which tract are they mainly monitoring |
C
SEPs Measure the integrity of the sensory pathways in the dorsal column of the spinal cord by stimulating a peripheral sensory nerve and measuring the electrical response in the brain. |
|
|
53. A patient has suffered flash burns of the upper half of the left upper limb, all of the left lower limb and the anterior surface of the abdomen. The approximate percentage of the body surface which has been burned is
A. 18% B. 23% C. 32% D. 41% E. 48% |
C
lower limb = 18%, anterior abdomen 9%, half upper arm 4.5% Rule of nines (for adults) |
|
|
54. Complications of mediastinoscopy include all of the following except |
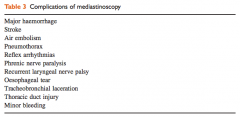
B
CEACCP article “Anaesthesia for mediastinoscopy” |
|
|
55. A 70 year old man with severe mitral stenosis and normally in sinus rhythm, is going for an ORIF of fractured radius and ulna. Soon after induction of GA, he develops a tachyarrhythmia with BP 70/40mmHg and HR 130bpm. The most appropriate immediate action is |
E
Mitral Stenosis & AF --> loss of atrial kick, impaired LV filling, associated with tachycardia and decreased diastolic filling time. Most appropriate management is DC Cardioversion given previous normal sinus rhythm. |
|
|
56. The time constant of the alveoli is |
A
Time Constant = Resistance x Compliance |
|
|
57. The MAC awake:MAC ratio of sevoflurane is closest to |
B |
|
|
58.Abnormal Q waves occur in all the following EXCEPT |
A
Digoxin toxicity --> arrhythmias (both SVT, brady, ventricular), VEBs. Digitalis effect --> Short QT, "sagging" ST segment, T wave changes (peak/invert/biphasic), U waves, J point depression, prolonged PR |
|
|
59. Patient complains of numbness in the anterior 2/3 of tongue after GA with LMA. Most likely nerve injured is |

C
Lingual branch of Mandibular (CN V3) nerve supplies cutaneous sensation to anterior 2/3 tongue.
Taste (special sense) supplied by chordae tympani branch of Facial (CN VII) Nerve, which joins Lingual branch of CN V3 and runs as Lingual nerve.
Posterior 1/3 sensation supplied by Glossopharyngeal (CN IX) Nerve |
|
|
60. A 70 year old man with non-valvular atrial fibrillation is taken off his warfarin for 7 days prior to surgery and has no bridging therapy. His daily risk of stroke is |
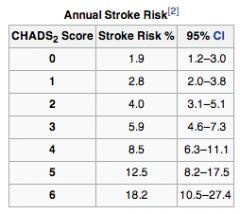
B
Assuming patient is otherwise well: CHADS2 = 0
Daily risk = Annual Risk/365 = 1.9%/365 = 0.005% |
|
|
61. In patient with ankylosing spondylitis which of the following is INCORRECT |
C
Anaemia of chronic disease occurs in ~ 15%, not 85%.
Ref. Oxford Handbook of Med
Other manifestations: Age 2nd-3rd decade M:F=3:1 HLA B27 (90%) p/w Sacroiliitis, Bamboo spine, Back pain, morning stiffness, improved by exercise, Schoeber test, Acute Anterior Uveitis 30%(unilateral), Cataracts, Aortic Regurg, BBBs, 3rd Degree HB, IBD, Restrictive lung disease both extrinsic and ILD. Amyloidosis |
|
|
62. Which of the following are NOT useful in the management of Torsades de Pointes |
B
Avoid Class I antiarrhythmics (further prolong QTc)
Magnesium definitive Rx DCCV may be useful Overdrive Pacing may be useful Isoprenaline in bradycardia associated TdP
Ref: CEACCP and eMedicine
|
|
|
63. Compared with a plenum vaporizer what is NOT a disadvantage of draw-over vaporizer (repeat but still not quite remembered correctly) |
C
Sevoflurane can be used with drawover (eg 2x OMV in series) |
|
|
64. The desflurane vaporizer is heated because of its |
A
The main problem with desflurane is that it has a high saturated vapor pressure at room temperature (700mmHg at 20°C). Boiling point at 22.8°C compare with sevoflurane at 58.5°C or isoflurane at 48.5°C.
|
|
|
65. The thermoneutral zone in a neonate in degrees celcius is
A. 26-28 B. 28-30 C. 30-32 D. 32-34 E. 34-36 |
D
32 - 34 in Term infants. 34 - 36 for low birth weight. Power And Kam. P418 |
|
|
66. Which of the following is most effective way to reduce renal failure in AAA surgery
A. Fluid bolus prior to aortic clamping B. Fluid bolus after aortic clamp release C. Frusemide D. Minimize cross-clamp time E. Mannitol |
D
The incidence of renal failure after AAA surgery is 5.4%, 0.6% require haemodialysis. Infra-renal cross clamping reduces renal blood flow by up to 40% through the alteration of the renin-angiotensin system.
Loop diuretics (e.g. furosemide), dopamine, mannitol, fenoldapam and N-acetylcysteine are proposed renal protective agents. There is no Level 1 evidence to support their use.
The mainstay of renal preservation is by adequate fluid resuscitation and the avoidance of nephrotoxins (NSAID’s, ACEI, aminoglycosides).
Ref: Anaesthesia for Abdo vasc surgery, AICM 2007 |
|
|
67. Which type of aortic dissection can be managed conservatively/non-operatively
A. Debakey 1 B. Debakey 2 C. Stanford A D. Stanford B E. Stanford C |
D
Stanford Type A involves the ascending aorta - may extend into the arch and descending aorta (DeBakey type I and II).
Type B involves the descending aorta only (DeBakey type III)
|
|
|
68. The most likely cause of death after pharyngeal, esophageal or tracheal perforation is
A. Air embolus B. Hemorrhage C. Failure to intubate D. Failure to ventilate E. Sepsis |
E
Retained gastric contents, saliva, bile, and other substances may enter the mediastinum, resulting in mediastinitis. Sepsis rapidly ensues. |
|
|
69. An essential criteria for diagnosis of left bundle branch block (LBBB) on ECG is
A. RSR in V1 B. Minimum duration QRS of 0.2 secs C. Deep slurred S wave in V6 D. Loss of septal Q waves in V5 and V6. E. T waves opposite direction to main direction of QRS, |
D.
Loss of septal Q waves in V5 and V6. |
|
|
70. If a patient experiences parasthesia in the little finger during supraclavicular brachial plexus block, the needle is in proximity to the
A. Posterior cord B. Middle trunk C. Ulnar nerve D. Lower trunk E. Medial cord |
D
The block is performed at the level of the distal trunks and origin of the divisions, where the brachial plexus is confined to its smallest surface area.
Cords are named in relation to level of axillary artery (i.e. distal to clavicle) |
|
|
71. Which of the following are feature of Conn's syndrome? |
C.
Primary hyperaldosteronism |
|
|
72 Commonest valvular heart disease seen in pregnancy is |
C |
|
|
73. Incidence and severity of vasospasm following sub-arachnoid haemorrhage is seen maximally at |
D |
|
|
74. The predominant pathology seen in restrictive heart disease is |
A |
|
|
75. What is the first sign/symptom seen with an inadvertent total spinal whilst performing caudal anaesthesia in a neonate |
C
Immature sympathetic nervous system in children/neonates. Hence little obvious sympatholysis. Desaturation secondary to thoracic nerve blockade will occur prior to LOC. |
|
|
76. Which of the following is an absolute contraindication to electroconvulsive therapy |
E
Ding, A&A, 2002. Advised to wait 3-6 months post MI. No data to support this. |
|
|
77. Prolonged Trendelenburg (head-down) positioning causes which of the following |
D
Increased venous return, increased MAP increased PAP |
|
|
78. Performed a brachial plexus block. Normal sensation still remains in medial forearm. Which part of brachial plexus is most likely to have been missed |
E.
Nerve not blocked is medial cutaneous nerve of forearm. |
|
|
79. A 29 year old female undergoes craniotomy for posterior fossa tumour. Which of the following is an absolute contraindication to the sitting position |
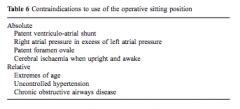
A |
|
|
80. A 4 year old child booked for minor surgery is seen in pre-admission clinic where a murmur is detected. Which feature will warrant further investigation |
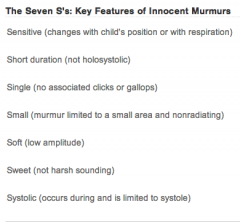
A
Seven S's of Innocent Murmurs
Ref: AAFP |
|
|
81. The autonomic supply of the ciliary ganglion is such that it |
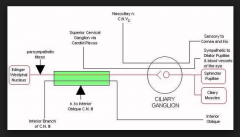
E |
|
|
82. Regarding Thallium Stress Testing in predicting perioperative cardiac events |
B Non-invasive Cardiac imaging relative high negative predictive value. Stress echo and Thallium scan roughly equivalent |
|
|
83. An elderly gentleman on warfarin has suffered a subdural haematoma. His INR on admission was 4.5. The resident in Ed has already given him 2.5mg of Vit K. To reverse his coagulopathy prior to urgent surgery you should give him |
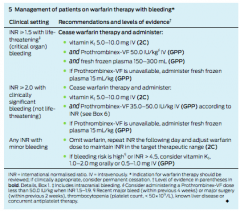
E
As per MJA 2013 Statement on Warfarin Reversal. Intracranial bleeding constitutes critical organ bleeding. |
|
|
84. During caesarean section a meconium stained floppy apnoeic baby is delivered. When the midwife gives you the baby, it is apnoeic, cyanotic with heart rate of 90 bpm. What do you do next |
E
resus.org.au |
|
|
85. A 70 year old lady suffered a subdural haematoma. She is currently confused and the neurosurgeon wants to take her to theatre for urgent decompression. She is a vague historian, but from notes you find out she had ablation and pacemaker put in 7 months ago - DDD mode. Cardiac technician in 1 hour away and the surgeon wants to proceed. What do you do |
E
In general, aim for PPM to have been checked in last 12 months, AICD in last 6 months. Important to assess underlying rhythm.
Application of a magnet to a modern pacemaker produces an asynchronous mode of pacing to protect a patient from the effects of EMI.
The asynchronous rate obtained depends on the programming of the device, the remaining battery life, and defaults that vary by manufacturer.
BJA, 2011, Periop Mx of pt’s with implantable cardiac devices |
|
|
86. New blood pressure measuring device is developed. Best was to compare it to the current gold standard |
B
Bland Altman Plot is best test for determining agreement.
Kendall Coefficient of Concordance, No assesses agreement around raters for non parametric data (eg movie ratings from different critics). It’s the normalization of the Friedman test.
Pearsons coefficient measures linear correlation between two variables
Friedmans test determines differences between treatments over multiple test attempts. Non-parametric. |
|
|
87. What happens when you place a magnet over a biventricular internal cardiac defibrillator
A. Switch to asynchronous pacing, B. Damage the internal programming, C. Nothing, D. Switch off antitachycardia function, E. Switch of rate responsiveness, |
D
Disable antitachycardia functions, does not affect pacing mode. Response will vary across different manufacturer's and pre-defined programmes.
|
|
|
88. A 54 year-old patient is on warfarin for AF. They have a history of alcohol abuse and liver failure with a bilirubin of 28 and an albumin of 30. He also has a history of DVT following a flight. What is his CHADS2 score
A. 0 B. 1 C. 2 D. 3 E. 4 |
A
CHADS: |
|
|
89. A full size C oxygen cyclinder (size A in New Zealand) has pressure
regulated from
A. 16000kpa to 400kpa B. 16000kpa to 240kpa C. 11000kpa to 400kpa D. 11000kpa to 240kpa E. ? |
A
|
|
|
90. What is approximately the systolic blood pressure in an awake neonate
(mmHg) |
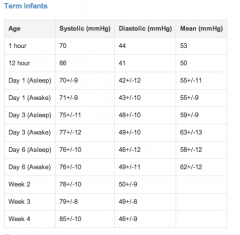
B
Neonatal Handbook, Dept Health Victoria |
|
|
91. A 25 year male with a history of asthma who is usually on fluticonasone and salbutamol nebs presents with an acute exacerbation. On examination you see he is distressed, RR 26 bpm. On auscultation: poor air entry and polyphonic wheeze bilaterally. ABG: pH 7.45, pCO2 27, pO2 75, HCO3 24. He has been treated with salbutamol and ipratropium nebules and intravenous hydrocortisone. What is the next step in his treatment? |
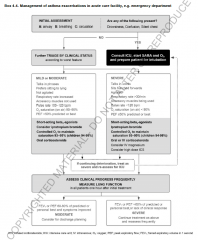
C
See Global Initiative for Asthma 2014 document |
|
|
92. You are doing an awake fibreoptic intubation and having difficulty identifying the anatomy of where you are. Then you observe a trifurcation. The lobe of the lung to which this airway is connected is |

C |
|
|
93. A 35kg 5 year old girl is having elective surgery for suturing of a superficial leg laceration. After induction with N2O/Sevoflurane/O2 and in absence of any visible veins you have placed an appropriately sized LMA. Following this her SpO2 immediately drop to 90%. What is your initial management? |
A |
|
|
94. Ulcerative colitis is associated with all of the following EXCEPT:
A. Cirrhosis B. Iritis C. Psoriasis D. Arthritis E. Sclerosing cholangitis |
C
Ann Rheum Dis doi:10.1136/annrheumdis-2012-202143
Psoriasis, psoriatic arthritis and increased risk of incident Crohn's disease in US women, but NOT Ulcerative Colitis |
|
|
95. Regarding rotameters |
D
These are cone shaped tubes that contain a bobbin and are specific for each gas. The
At low flows, the bobbin is near the bottom of the tube and the gap between the
As flow rate increases, the bobbin rises up the flowmeter and the gap increases until it |
|
|
96. You see a man in his 60s in clinic 1 week prior to laparoscopic cholecystectomy. He has dilated cardiomyopathy with an ejection fraction of 30%, but does not get dyspnoeic with normal activities of daily living. What is the most appropriate management of his heart failure? |
C |
|
|
97. The best clinical indicator of severe aortic stenosis is |
A |
|
|
98. Atrial Septal Defect murmur is heard due to blood flow through |
B |
|
|
99. At what valve area do you begin to get symptoms at rest, with mitral stenosis? |
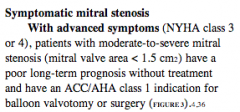
D
Mod-severe mitral stenosis can cause NYHA class 3 or 4 symptoms, at or below a valve area of 1.5cm2. See article below from Cleveland Clinic. |
|
|
100. Nitrous oxide anaesthesia may cause all of the following EXCEPT |
E N2O causes irreversible inhibition of methionine synthetase. |
|
|
101. The diagnosis of neuroleptic malignant syndrome requires the presence of |
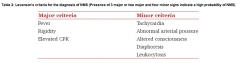
D
Both B&D are correct, so I suspect the question read Creatinine and not Creatine making Muscle Rigidity the correct answer. |
|
|
102. Regarding tryptase level testing for suspected anaphylaxis, all are true EXCEPT: |
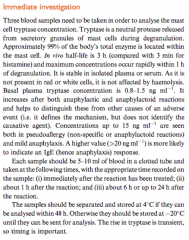
E
See CEACCP 2004: Anaphylaxis. Tests should be at 1hour, 6 hours and 24 hours post-reaction. |
|
|
103. An 18 month old boy presents for surgery for an incarcerated inguinal hernia. On examination you note that he has had an URTI for approximately one week. Your advice regarding surgery should be |
E as surgery is urgent.
From OHA page 770. ‘Anaesthesia in the presence of an URTI is associated with increased complications in younger children….excess secretions, airway obstruction, largyngospasm and bronchoconstriction. The risk is increased 5-fold using an LMA and 10-fold with intubation. Children with moderate to severe infections should be postponed. Those with productive cough, purulent chest or nasal secretions, pyrexia and signs of viraemia or constitutional illness including diarrhoea and vomiting. |
|
|
104. The incidence of fat embolism syndrome following a unilateral closed femoral fracture is |
A
See CEACCP 2007 “Fat Embolism”. |
|
|
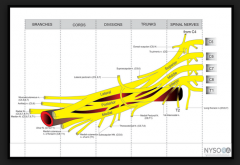
105. The thoracodorsal nerve arises from |
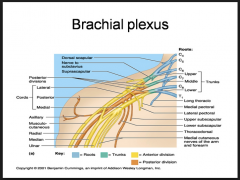
C |
|
|
106. Neurosurgery operation in the sitting position. MAP 80mmHg, CVP 5mmHg, the transducers are located 13cm below the external auditory meatus. What is the CPP? *Note - I specifically remember that 70mmHg was an option* |
B
1mmHg= 1.36cmH2O and CPP= MAP- ICP or ICP whichever is higher |
|
|
107. A man attending his daughter's wedding is involved in fight with his son-in-law. He does not know where he is, opens eyes to voice, but removes tie when instructed. What is his GCS? |
D
|
|
|
108. Which of the following drugs is least likely to cause hypoxia in ARDS |
A
|
|
|
109. What is the best predictor of poor prognosis with aortic stenosis?
A. Chest pain B. Paroxysmal nocturnal dyspnoea C. Syncope D. Palpitations E. Fatigue |
B
50% survival: Angina at 5 years Syncope at 3 years Dyspnoea at 2 years |
|
|
110. Pierre-Robin sequence is characterized by cleft palate, micrognathia and |
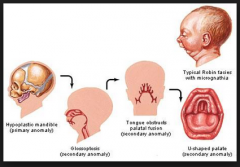
C |
|
|
111. After 3 litres of normal saline, the dilutional anaemia is initially offset by
A. Increased cardiac output B. Increased oxygen extraction C. Capillary vasodilation D. ? E. ? |
A
From Miller, Ch 57. The hypervolumetric haemodilution will lower PaO2 but compensatory mechanisms occur to ensure surplus Oxygen delivery to the tissues continues. A sudden reduction of [RBC] – reduction in viscosity – reduced peripheral resistance- and so increased VR with increased CO results. |
|
|
112. Anaesthetic Machine is left on all weekend with flow rate of oxygen at 6 litres/min. A Desflurane vaporiser is placed on it on Monday morning without changing the CO2 absorber. What is the most likely toxic product produced? |
C
From Stoelting. DIE (Des, Enf, Iso) produce Carbon Monoxide from their CHF2 moeity. |
|
|
113. 2ml of 0.75% ropivacaine is injected for an interscalene block. Soon after the patient loses consciousness. The most likely place of inadvertent injection is |
E |
|
|
114. An 18 month old infant is undergoing a routine spontaneously breathing GA with an LMA. They have a sudden onset of SVT with a heart rate of 220 and a BP of 84/60 with an ETCO2 of 32 and SpO2 of 98. The best management strategy is |
A
Predicted weight = 2(age+4) = 11Kg. Adenosine is first line according to www.resus.org.au Guideline 12.5 at a dose of 01-0.3 mg/kg. Amiodarone is second line at 5mg/Kg. When SVT is pulseless or accompanied by severe hypotension, DCR is indicated at 0.5-1.0J/Kg up to 2 j/Kg if needed. |
|
|
115. When stimulating the ulnar nerve with a nerve stimulator, which muscle do you see twitch |
C |
|
|
116. A middle-aged male with severe mitral stenosis having general anaesthesia for repair of fractured ulna/radius. Ten minutes into the case you notice a tachyarrythmia with his HR 130 and BP 70/-. He is normally in sinus rhythm. What do you do |
C
Decompensated Mitral Stenosis with loss of atrial kick and decreased diastolic filling time with AF with RVR. Cardioversion indicated. |
|
|
117. Circuit disconnection during spontaneous breathing anaesthesia |
D
A not true, as disconnection from inspiratory arm will still allow detection of CO2 in spontaneously breathing patient. |
|
|
118. An 85 year old patient with a bleeding disorder (? haemophilia) suffers a fractured neck of femur (#NOF). You discuss the possibility of a needing a blood transfusion but despite your explanation they refuse because they are scared of CJD infection post transfusion. Subsequently you decide not to proceed with the case because of the high risk of bleeding. The ethical principle that this is an example of is |
patient refusing transfusion is example of Autonomy. Not proceeding due to risk of bleeding is |
|
|
119. A type I diabetic is fasting pre-operatively and you decide to place them on an IV insulin infusion to optimize their perioperative glycaemic control. Their BSL is 7 mmol/L. By what mechanism does the insulin infusion decrease their BSL
A. Stimulates glucose uptake into the liver B. Stimulates glucose uptake into skeletal muscle C. Inhibits glucose production in the liver D. Decreases glucose absorption from the gastrointestinal tract E. Inhibit glucagon release |
B
|
|
|
120. Patient has undergone a bilateral lung transplant. All of following are impaired EXCEPT |
C |
|
|
121. Patient with history of long QT syndrome treated with long term propranolol. How do you know the treatment is effective |
B
CEACCP 2008: Long QT syndrome |
|
|
122. A neonate is born with meconium stained liquor but is vigorous and crying. The reason for not suctioning the pharynx is |
C
See Resus guidelines |
|
|
123. What organism most commonly causes meningitis post spinal anaesthesia |
D |
|
|
124. A male patient has a haemoglobin of 8g/dL and reticulocyte count 10%. The most likely diagnosis is
A. Untreated pernicious anaemia B. Aplastic anaemia C. Acute leukaemia D. Anaemia of chronic disease Hereditary spherocytosis |
E
|
|
|
125. An advantage of supraclavicular block over an interscalene nerve block for shoulder surgery |
A |
|
|
126. A patient with a head injury is found to have a unilateral dilated pupil with no direct or consensual response to light. What is the most likely diagnosis |
D
May cause compression of 3rd cranial nerve ipsilateral to injury leading to fixed and dilated ipsilateral pupil |
|
|
127. In an arterial line system |
D
Optimal damping coefficient 0.64.
If natural resonant frequency high, able to be accurate despite suboptimal damping. Usual resonant frequency of our systems are 10-15 Hz- need frequencis of 10-20,000 Hz to negate the importance of the coefficient value. Impractical in anaesthetics as would have to be very stiff & short, or VERY expensive. |
|
|
128. The commonest postoperative complication in a patient with a neck of femur fracture (#NOF) is
A. UTI B. Pneumonia C. Myocardial Infarction D. Delirium ? |
D |
|
|
129. Which of the following is an advantage of a bronchial blocker cf to a double lumen tube |
A
Bronchial Blockers allow selective lobar isolation, which DLT cannot. Otherwise no benefit over DLT |
|
|
130. Laser endotracheal tubes |
D
Larger diameter compared to standard tubes due to reflective lining.
Laser/Tubes with Double cuffs are still combustible, but are saline filled and dye filled, to aid detection of rupture. |
|
|
131. Pulsus paradoxus in cardiac tamponade, the blood pressure decreases |
E |
|
|
132. You are anesthetizing a patient for a laparotomy who has a history of pulmonary hypertension. Regarding the patients anaesthetic management |
A
Ketamine may increase pulm HT |
|
|
133. In a patient with severe rheumatoid arthritis, which radiological finding is most consistent with severe atlantoaxial instability (? C1/C2 instability) |
A
Anterior subluxation with gap >4mm on flexion lateral C-spine xray is diagnostic |
|
|
134. You are called to the labour ward to assist in the manual removal of a retained placenta in a healthy woman. The obstetrician asks you to administer intravenous glycerol trinitrate. An initial safe dose, that you would expect to be effective, would be |
B
|
|
|
135. What is the most accurate method of determining foetal heart rate in a neonate |
B
As per Neonatal resus guidelines |
|
|
136. Definitive evaluation of malignant hyperthermia (MH) susceptibility does NOT include observing |
unsure still- possibly A |
|
|
137. A 60 year-old man with anterior mediastinal mass, is having a mediaastinoscopy. During induction they lose cardiac output, desaturate and drop their ETCO2. What is the best management strategy |
D
Loss of muscle tone may lead to tracheal compression. Reposition lateral or prone to reduce subglottic compression of airway. |
|
|
138. Which is true of Eaton-Lambert syndrome that differentiates it from myasthenia gravis? |
C
Lambert's Sign is improvement in muscle weakness with exercise ELS associated with small cell ca Disorder of presynaptic release Remains sensitive to NDMR
|
|
|
139. A 55 year-old man presents to the emergency department with an obviously infected heel ulcer - BP 100/60, PR 110/minute, temperature 35.8, Na 125, K 2.7, BSL 55, Creatinine 180. Which do you give first/most urgently? |
B
Management of HONK |
|
|
140. A new test has been developed to diagnose a disease. To determine the SPECIFICITY of this new test it should be administered to |
B
Hence required to know the true negative rate. |
|
|
141. During one lung ventilation, hypoxaemia can occur. The cause for this is: |
B
Shunt has the greatest effect. Other factors are also contributory. |
|
|
142. A child with intra-operative blood loss. A cardiac arrest is most likely because of |
D
Anaesth & Analg, Vol. 105, No. 2, August 2007. - review of anaesthesia-related cardiac arrest. Showed underestimation of blood loss leading to hypovolaemic shock most common cause of arrest related to anaesthetic (23%). Types of surgery most related; craniotomy & spinal surgery. |
|
|
143. The lumbar plexus supplies all of the following EXCEPT: |
A
Subcostal Nerve comes from T12 |
|
|
144. The symptom indicating poorest prognosis in an adult patient with aortic stenosis
A. Chest pain B. Malaise C. Palpitations D. Paroxysmal nocturnal dyspnoea E Syncope |
D |
|
|
145. A 50 year old male in recovery after an anterior cervical fusion, developing increasing respiratory distress, bulge under original incision, combative, repeatedly removing oxygen mask, SpO2 96%. What is the most appropriate management |
C
Safest if he wasn’t combative would be awake fibreoptic (B). However may have to choose C- gas induction then direct laryngoscopy. |
|
|
146. Regarding post dural puncture headache, all of the following are true, EXCEPT: |
A- true. of these 40% will need repeat patch |
|
|
147. A 70 year-old male presents for right lower lobectomy. Preoperative spirometry shows FEV1 2.4L (4.2L predicted), FVC 4L (5L predicted). The predicted post-operative FEV1 is: |
C
Total number of Bronchopulmonary segments = 18
Post op predicted FEV1 = preop x (remaining segments/18)
ppoFEV1 = 2.4 x (13/18) = 1.733L |
|
|
148. What is the most important immediate treatment for a cardiac arrest due to ventricular fibrillation in a patient with hypertrophic obstructive cardiomyopathy? |
C |
|
|
149. Hypercalcaemia due to hyperparathyroidism is associated with
A. A shortened PR interval B. A prolonged QTc interval C. Muscle rigidity D. Polyuria and polydipsia E. Increased glomerular filtration rate |
A/D
ECG changes: Short PR, short QT. J waves. Ectopic beats, Ventricular irritability.
Ref: LITFL
nb Polyuria & Polydipsia also observed in hypercalcaemia. |
|
|
150. The cause of early mortality (early - within 30 minutes) in a pregnant women with amniotic fluid embolism is
A. Bronchospasm B. Hypovolaemia C. Malignant arrhythmia D. Pulmonary hypertension Pulmonary oedema |
D
Phase 1- Amniotic fluid & foetal cells enter maternal circulation. Pulm art vasospasm due to highly immunogenic nature of fluid, causes pulmonary hypertensions, RH failure and collapse, hypoxaemia & hypotension. |

