![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
72 Cards in this Set
- Front
- Back
|
What is the general pathogenesis of aortic aneurysms?
|
--Increased matrix metalloproteinases
--+/- decreased tissue inhibitors of them Spillover inflammation from atherosclerosis |
|
|
What are some less common causes of aortic aneurysms?
|
1. Genetic defects in fibrillin or collagen (Marfan syndrome)
2. Infection (called "mycotic" even when not fungal, which is most of the time) 3. Vasculitis (giant cell arteritis) |
|
|
What are the complications of aortic aneurysms?
|
1. RUPTURE!
2. Mural thrombus formation 3. Embolism of atheroma or thrombus 4. Obstruction of aortic branches 5. Aortoenteric fistula |
|
|
What is the major determinant of rupture?
|
DIAMETER
The greater the diameter, the greater the risk of rupture. |
|

What is shown here? Is it common? In what groups?
What is it associated with? What is a systemic manifestation? What does it involve (anatomy)? |
Giant cel (temporal) arteritis
Yes! Elderly white females of N. European descent Associated with polymyalgia rheumatica Fever Temporal, opthalmic arteries and thoracic aorta |
|

What is the pathology?
|
Multinucleated giant cell attack on internal elastic lamina with lamina destruction --> arterial wall injury--> fibrosis--> intimal thickening and CD4 lymphocytes
|
|

Diagnosis?
Treatment? |
High ESR and positive biopsy
Steroids |
|

Draw this!
|

You did it!
|
|
|
Giant cell arteritis is a _____________ attack on _________________ in arteries and calcified atrophic _____________ of thoracic aorta. The prerequisite for arterial calcification explains why giant cell arteritis occurs almost exclusively in the elderly.
|
Multinucleated giant cell attack
Calcified internal elastic lamina Tunica media |
|
|
True or false.
Both the INNATE and ADAPTIVE arms of the immune system lead to vessel injury. |
TRUE
|
|
|
What initiates the immune response?
What are the immune cells in arteries mostly? Do they have a high or low threshold of activation? What do they not express? What state do they maintain for T cells? |
Dendritic cells
Immature dendritic cells High threshold of activation CD80 and CD86 Anergic tolgerogenic state for T cells |
|
|
In the pathogenesis of giant cell arteritis, _______________ activate immature dendritic cells.
|
Antigens from pathogenesis or formed in situ from calcification
|
|
|
What do the activated cells produce large amounts of?
What do they upregulate the release of from T cells? What homing chemokines do the dendritic cells release? What do they bind to? What does this result in? |
IL-12 and IL-18
INF-gamma CCL19 and CCL21 CCR7 --> local arrest of activated dendritic cells which are trapped in the arterial wall. |
|
|
The activation of vascular dendritic cells is mediated via the ligation of their ___________.
|
TLRs
|
|
|
Describe the TLR mechanism
TLR-4 specifically |
Ligation of PAMP or DAMP to the extracellular portion of the TLR --> activation of intracellular TRAM motif, intracellular cellular second message, and NfKB --> enters nucleus --> translation of pro-inflammatory molecules.
|
|
|
The aortic arch and its branches are derived from the __________, while the descending aorta derives from the ____________.
_____________ is abundantly expressed on activated adventitial dendritic cells. |
Ectoderm
Mesoderm TLR-4 |
|
|
Upon recognition of a PAMP or DAMP, IFN-gamma is produced in large amount and leads to ___________________.
Activated dendritic cells secrete pro-inflammatory cytokines, mainly which three? |
mononuclear infiltration
IL-2, IL-6, IFN-gamma |
|
|
What do IL-2, IL-6, and IFN-gamma mediate?
What is the overall result? |
Recruitment of inflammatory cells
Inhibition of cell migration Enhancement of T cell proliferation Stimulation of T and B cells Amplification of immune response through positive feedback loops. |
|
|
What does the progress of the immune response depend on?
What two distinct immune axes do these response to respectively? |
Th1 and Th17 CD4 T cells
IL-12-IFN-gamma and IL-1-IL-23 |
|
|
What is the dominant cell population in the intramural lesions and the periphery of patients with untreated giant cell arteritis? What signature cytokine do these cells produce? Can steroid therapy help? Why or why not?
|
Th1
IFN-gamma No, they get continuous signaling from dendritic cells that continue to produce IL-12. |
|
|
What does increased IFN-gamma correlate with?
What are these involved with? What may VEGF in turn promote that would lead to a viscous cycle of inflammation and stenosing fibrosis? |
VEGF and PDGF production
Intimal response that leads to lumen stenosis. IFN-gamma |
|
|
In untreated patients, the number of ________ cells is elevated 10-fold in the peripheral blood and they accumulate in the vascular infiltrates.
|
Th17
|
|
|
_____________ leads to an almost complete reduction of both circulating and lesional _________ cells.
|
Prednisone
Th17 |
|
|
Systemic manifestions of giant cell arteritis are the most responsive to what? Why? Which axis is suppressed?
|
Prednisone therapy
Normalization of Th17 cell levels Suppression of IL-1--IL-6--IL-17 axis |
|
|
What induces macrophages to form multinucleated giant cells and granulomas?
|
IFN-gamma
|
|
|
The pro-inflammatory environment, shaped by what 5 factors, promotes the infiltration of the arterial wall by activated monocytes?
|
IL-1, IL-6, IL-17, IL-23, IFN-gamma
|
|
|
Matrix metalloproteases that are released by macrophages and smooth muscle cells are associated with what three things?
|
Matrix degeneration
Intimal hyperplasia Luminal narrowing |
|
|
Which MMPs play a role in internal elastic lamina degradation characteristic of giant cell arteritis?
What do they destroy? |
MMP-2 and MMP-9
Elastin |
|
|
What is peripheral arterial disease?
Is it common? |
Chronic atherosclerotic occlusive disease of large and medium arteries, primarily of the legs.
Yes! Elderly and men |
|
|
What are symptoms of peripheral artery disease?
|
Intermittent claudication (limb pain brought on by exercise and relieved by rest) --> could be in calf muscles when disease in femoral or popliteal arteries, the usual
Pain at rest, ulcers = SEVERE DISEASE |
|
|
What are the signs of peripheral artery disease?
|
1. Diminished or lost distal pulses
2. Bruits (swishing sounds auscultated over lesions with turbulent flow) 3. Pallor (or cyanosis) 4. Skin atrophy 5. Muscle atrophy 6. Ulceration 7. Necrosis (gangrene) |
|
|
How is the diagnosis made for PAD?
What is the treatment? |
History and physical examination
First line treatment: Exercise --> walking! Helps develop collaterals. |
|
|
Is acute arterial occlusion common?
What is it usually due to? |
No
Thromboemboli --80% from heart (65% mural from MI;10% left atrial -->atrial fibrillation, mitral stenosis; 5% dilated cardiomyopathy 15% unidentifiable 5% miscellaneous |
|
|
What are signs and symptoms of acute arterial occlusion?
Who do you call? |
FIVE Ps!
1. Pain 2. Pallor 3. Paresthesia 4. Paralysis 5. Pulselessness (legs = 70%, arms = 8%). THE SURGEON! SURGICAL EMERGENCY! |
|
|
Where are the other 10% (locations for pulselessness)?
|
Brain
Other sites = intestines, kidneys, and spleen |
|
|
How is the diagnosis made for acute arterial occlusion?
What is the treatment? |
History and physical examination
Anticoagulation (heparin), intra-arterial thrombolytic therapy, catheter-based thrombectomy, surgery (thombectomy, bypass) |
|
|
True or false:
Acute arterial occlusion is often a "surgical emergency" --> requires emergency surgery. |
TRUE!
|
|

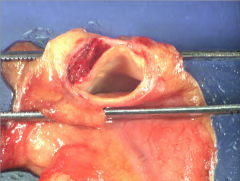
What happened to this right common carotid artery?
|
Dissection from the aorta extended into it.
|
|
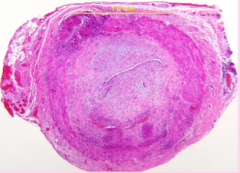
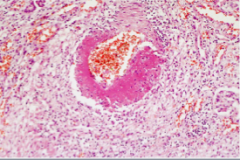
Can you describe the microscopic pathology in this artery?
|
Near-total occlusion of lumen from young fibrous tissue in tunica intima (bluish myxoid ground substance =young)
Two zones of lymphocytes (dark blue dots) and dark pink stuff in and around the tunica media, especially around the region of the internal elastic lamina in the larger zone in the lower part of the image. �� |
|
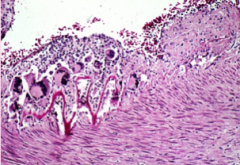
Can you describe the microscopic pathology in this artery?
|
Internal elastic lamina being eaten by giant cells, one lunching on it in mid image, others ready to munch right above the bit that is left.
Numerous lymphocytes around giant cells = secreting interferon gamma. Internal elastic lamina in the right half almost nearly gone. |
|

Can you describe the gross pathology in this foot?
Can you diagnose the disease? Can you guess the pathogenesis? |
Mottling from ischemia in a wedge-shaped distribution, in this case probably due to thromboembolus from iliac or popliteal artery aneurysms the patient had.
� |
|
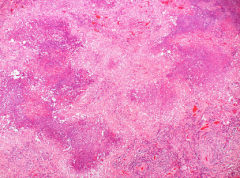
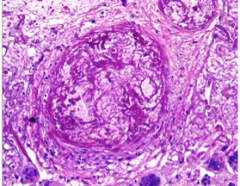
What is this a map of?
|
Geographic necrosis
Abundant basophilic debris (nuclear dust) and the combination called “pathergic necrosis”, which is characteristic of a particular disease. |
|
Can you describe the microscopic pathology in this small artery and vein in a lung?
|
The vein (upper left) and artery(lower center-right) and surrounding tissue are infiltrated by lymphocytes (with edema of the artery) markedly narrowing the lumens and there are giant cells in adventitia of both blood vessels.
Granulomatosis with polyangiitis (Wegener's) |
|

What is happening in these toes?
|
Embolic peripheral arterial disease
|
|

A 4-month-old east Asian female infant was hospitalized after 2 days of fever and the development of full body erythema. Her white blood cell count was 9,200/cu mm (normal 6,000 to 17,000 for 3-5 months old) and C-reactive protein 1.6 mg/dl (normal 0 to 0.5 mg/dl). She was empirically treated for the possibility of a bacterial infection and urticaria, but this failed to reduce her fever after 5 days. In addition, she developed inflamed conjunctivae, a diffuse rash and edema of the peripheral extremities. Her tongue had an appearance like this:
What is the diagnosis? What are the complications? |
Kawasaki disease
--Large coronary aneurysms with rupture or thombosis --myocardial infarction --sudden death |
|

Can you figure out what blood vessel this is and what the arrow is pointing at?
|
Thoracic aorta, identifiable by the aortic valve below
with an intimal tear indicated by the arrow. |
|

How often do you examine the roof of the mouth
in physical examination? What is happening here? What is the diagnosis and what other manifestations will the patient likely have? |
Upper respiratory tract infection
Granulomatosis with polyangiitis (Wegener's) --g. vasculitis of arteries and veins in the lungs causing pathergic necrosis --> radiographically visible nodules --> cavitation Glomerulonephritis DISEASE INVOLVED VEINS AND ARTERIES (IMPORTANT DISTINCTION FROM THE REST) |
|
This 69-year-old white male farmer had hypertension and had quit smoking 30 years ago. He had been in good health until he experienced the sudden onset of sharp epigastric and left upper quadrant abdominal pain and back pain at the same level, along with left leg pain and dyspnea. His left leg was pale, pulseless and paralyzed. His aorta showed:
What does this patient have? |
Type B aortic dissection
|
|
|
Giant cell arteritis:
Describe immunopathology What are the symptoms? How is the diagnosis made? What is the mainstay of treatment? |
Look this up!
|
|
A 45-year-old white male trucker has been having fever, malaise, myalgias, weight loss, abdominal pain, bloody stools and variably sized, tender skin nodules for months, but he has delayed seeking medical evaluation because he lacks health
insurance. The patient is likely to have which antibodies? |
None!
Polyarteritis nodosa not associated with antibodies. |
|
|
What antibodies are associated with microscopic polyangiitis?
What antibodies associated with granulomatosis with polyangiitis (Wegener's)? |
Anti-myeloperoxidase (P-ANCA)
Anti-proteinase-3 (C-ANCA) |
|
|
What antibodies associated with SLE?
|
Anti-dsDNA (specific)
Anti-Smith (specific) Anti-RNP U1 Anti-SS-A (Ro) Anti-SS-B (La) Antiphospholipid (thombotic episodes) |
|
|
What antibodies associated with mixed connective tissue disease?
|
Anti-RNP U1
|
|
|
What antibodies associated with Sjogren syndrome?
|
Anti-SS-A (Ro)
Anti-SS-B (La) |
|
|
What antibodies associated with systemic sclerosis?
Limited schleroderma? |
Anti-Scl-70
Anticentromere (with both) |
|
|
What antibodies associated with antiphospholipid syndrome? Roll in disease?
|
Antiphospholipid = thrombotic episodes
|
|
|
Polyarteritis nodosa is common in which group of people?
|
Middle-aged males
|
|
|
What are the symptoms of polyarteritis nodosa?
|
Fever, malaise, myalgias, weight loss, abdominal pain, bloody stool, skin nodules, peripheral motor neuropathy
|
|
|
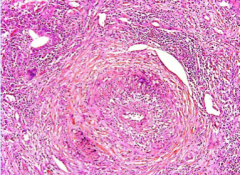
What is polyarteritis nodosa?
|
Segmental transmural necrotizing vasculitis of small and medium sized arteries with fibrinoid necrosis and lesions at different stages.
|
|
|
What happens if you miss a polyarteritis nodosa diagnosis?
|
Fatal!
90% non-fatal if treated |
|
|
You have just have diagnosed a 4.5 cm abdominal aortic aneurysm (AAA) in a 60-year-old man with a history of smoking, but not hypertension. His blood pressure is 120/80 mm Hg. The most important thing to do now is:
Anticoagulate him Lower his blood pressure Screen his 38-year-old son for AAA Screen his 68-year-old brother for AAA Stent the patient’s AAA Surgically resect the patient’s AAA |
Screen his 68 y/o brother.
|
|
|
Do you do anticoagulation for AAA? Do you lower BP?
|
No, no!
|
|
|
What are the AAA size guidelines?
Which ones are manages surgically? What are the two options? What are the differences in mortality rates for elective procedures vs. emergency surgery? |
4cm or less = never burst
4-5cm = burst at rate of 1% per year 5-6 cm = 11% Greater than 6cm = 25% Greater than 5 cm = open placement of tubular prosthetic grafts or endoluminal insertion of stented grafts 5% vs. 50% |
|
|
What are the symptoms of Kawasaki disease?
|
Conjuctival or oral erythema
Blistering Edema of the hands and feet Erythema of the palms and soles Desquamative rash Cervical lymph nodes enlargement (mucocutaneaous lymph node syndrome) |
|
|
How do you treat kawasaki disease?
|
Intravenous immunoglobulin therapy and aspirin = disease rate reduced to 4%
|
|
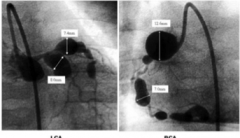
What is shown here?
|
Coronary aneurysms in Kawasaki disease
|
|
|
What is the difference between aneurysm and ectasia?
|
Aneurysm is a discreet localized dilation (outpouching)
Ectasia is not discrete and localized |
|
|
What is the difference between aneurysm and dissection?
|
Dissection is a tear of the tunica intima
letting luminal blood under high pressure into the tunica media, where it tunnels (“dissects”) a second lumen. |
|

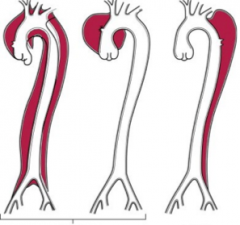
Identify each
|
a = normal vessel
b = true aneurysm (saccular) c = true aneurysm (fusiform) d = false aneurysm e = dissection |
|
Which type of vasculitis is this?
Giant cell Kawasaki disease Polyarteritis nodosa Wegener’s None of the above |
Fungal vasculitis = zygomycosis
Never forget the possibility that what seems to be an autoimmune vasculitis could an infectious vasculitis! |
|
What difference does it make to differentiate between Type A from Type B dissections for treatment?
|
Type A = rapid diagnosis/institution of intensive antihypertensive therapy/surgical plication of the aortic intimal tear = save 65-85% of patients
Type B = 75% survival rate if surgery or antihypertensive medication only. |
|
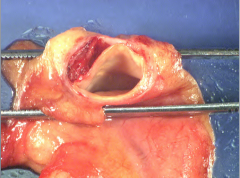
How do know you if a dissection is type B? From earlier case.
|
Dissection is below the ascending aorta
Picture shows an aortic dissection with clotted blood in false lumen. As it moved down aorta, the blood at aortic pressure compressed the ostia of the celiac trunk, superior mesenteric artery, renal arteries, inferior mesenteric artery and finally left femoral artery with resulting occlusion and ischemia. |

