![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
106 Cards in this Set
- Front
- Back
|
What is Dr. David Cullen's recommendations for avoiding hypotension in beach chair position?
|
1. Titration of anesthetics to avoid excessive depth of anesthesia
2. Minimizing sudden changes in position 3. Administration of IV fluids to offset the effects of NPO status and the sitting position on venous return 4. Use of vasopressors to maintain blood pressure, as needed 5. Correction of blood pressure for the difference in height between the site of measurement and the brain |
|
|
What is the change in BP of the brain in relationship to the height of site of measurement?
|
BP change = 2mmHg for every 1 vertical inch (2.5cm)
|
|
|
What is the conversion factor for mmHg to cm H2O?
|
1 mmHg = 1.36 cmH2O
1 cmH2O = 0.735559121015 mmHg |
|
|
What are 2 ways to avoid V/Q mismatch when positioning patients?
|
1) adequate positive-pressure ventilation
2) skeletal muscle relaxation |
|
|
What changes in breathing does the anesthetized spontaneously breathing patient experience?
|
decreased tidal volume
FRC and increased closing volume |
|
|
What body parts are mostly responsible for breathing when laying supine?
|
Abdominal wall
Diaphragmatic movement |
|
|
What are the 2 most common nerve injuries?
|
Ulnar
Brachial |
|
|
What are some ways to avoid an Ulnar injury to a patient?
|
*Keep hand and forearm supinated or neutral position
*Avoid excessive pressure on the postcondylar groove of the humerus |
|
|
How can you avoid a brachial plexus injury?
|
*Avoid shoulder brace use in Trendelenburg positioning
|
|
|
Describe correct use of chest roll in lateral and prone positions
|
Avoid the placement of a high “axillary/chest” roll. Does not belong in the axilla.
Place axillary/chest roll well away from the axilla to prevent compression of the axillary artery and brachial plexus Breasts inside the chest rolls. “Push-up bra” effect Abdomen hanging free Genitals free |
|
|
What position is likely to injure the peroneal/saphenous and sciatic nerves?
|
Lithotomy position
|
|
|
What are some keys to avoid injury while in lithotomy position?
|
minimalize time in lithotomy position
*use 2 assistants to adjust the patients legs simultaneously to avoid stretch injury *Avoid excessive flexion of the hips, extension of the knees or torsion of the lumbar spine |
|
|
What positions are likely to injure the obturator and femoral nerves?
|
Lithotomy Position and Sitting position extreme hip flexion
|
|
|
What precautions should be taken to prevent injury in prone positions?
|
Assess ROM in neck and shoulder prior to induction
Avoid pressure on the eyes Chest Rolls/Wilson Frame Hypotension d/t venous pooling Breasts-should be in a push up bra effect and inside of chest roll Abd/Stomas/Genitals-hanging free Prevent nerve injury ulnar/brachial plexus/facial and occular Evaluate often Document Induct on bed or stretcher Have enough people to safely turn pt |
|
|
What are risk factors associated with nerve injury in lithotomy position?
|
Prolonged surgery >3hrs
Very thin body habitus Recent Smoking |
|
|
What are measures for treating VAE?
|
Notify surgeon
Flood Surgical field immediately Identify source-close open venous sinus Place Patient supine L.lat. decubitus Trendelenberg Aspirate air from centeral venous catheter Support BP/CO ACLS protocols |
|
|
Describe how to perform the leak test to determine airway edema
|
with pt. head up and awake, deflate the ETT cuff and occlude tube
Can pt . breath around it? If so-the tracheal diameter is greater than the ETT = extubation likely safe |
|
|
What is indicated when no breath sound is heard around ETT during leak test?
|
Extubation may be followed by airway loss d/t edema
Leave intubated-and keep head up |
|
|
What is the makeup of air?
|
Nitrogen ~ 78%
Oxygen ~ 21% Argon ~ 1% CO2 ~ .04% |
|
|
What is 1 atmosphere equivalent to at sea level?
|
101.3 kPa
1030 cm H2O 14.7 psi 29.9 Hg 760 torr |
|
|
How does PaO2 relate to FiO2?
|
PaO2 is roughly 5x the FiO2
|
|
|
What influences the rebreathing of gases by the anesthetized patient?
|
1. Fresh gas flow rates
2. Mechanical dead space 3. Design of breathing system |
|
|
What is insufflation?
|
Stream of gas or vapor combined with O2 or air during spontaneous ventilation. (Air under draps, Jet ventilation)
|
|
|
What are advantages to open system ventilation?
|
- Minimal dead space
- Minimal resistance - Room air or O2 - No rebreathing |
|
|
What are disadvantages to open system ventilation?
|
- Inspired gas concentrations unpredictable
- Inability to assist respiration - Heat/moisture loss - Waste of gas/Pollution |
|
|
What is the % of O2 delivered via NC?
|
25% - 45% (1-6 LPM)
|
|
|
What percent of O2 does simple mask deliver?
|
35-55%
|
|
|
What percent of O2 does partial rebreather mask deliver?
|
~60%
|
|
|
What are the 3 types of non-rebreathing valves?
|
spontaneous, controlled or both.
Ambu = Controlled Laerdal - spontaneous or controlled Lewis-leigh = spontaneous or controlled Stephen-slater = spontaneous |
|
|
What is the inside diameter of all devices?
|
15mm
|
|
|
What is the most efficient system for spontaneous ventilation?
|
Mapleson A - FGF of 70% of alveolar ventilation to prevent rebreathing (controlled vent. requires 3x Vm)
|
|
|
What is the optimal size for anethesia breathing bags?
|
1, 2 or 3 liters. Should hold volume that exceeds inspiratory capacity
|
|
|
What position should the APL valve be in during spontaneous ventilation?
|
Fully open - permits gas to leave circuit to scavenging system, matching excess fresh gas to the inflow.
|
|
|
What is the APL valve
|
Adjustable Pressure Limiting valve allows assisted or controlled ventilation by compressing reservoir bag
|
|
|
what is the most commonly used non-circle breathing system?
|
Bain circuit (modified mapleson D)
Mapleson F ( Jackson - Rees) |
|
|
What system is the most efficient at controlled ventilation?
|
Mapleson D, F
(FGF > 2 - 3 times Vm to prevent rebreathing) |
|
|
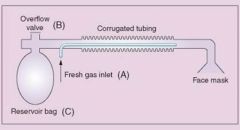
Mapleson System
|

|
|
|
What system is useful in pediatrics?
|
Mapleson D - exhaled gas warms inhaled. Useful for low Vm
|
|
|
What are advantages of Bain circuit?
|
- Warms inhaled gases
- Conserves moisture - Ease of scavenging Ax gases - Lightweight, reusable |
|
|
What are the disadvantages of Bain circuit?
|
- Unrecognized disconnect or kink
(Hypercarbia) |
|
|
What is the Pethick test?
|
Occlude the patient's end of the circuit (at the elbow).
Close the APL valve. Fill the circuit, using the oxygen flush valve. Release the occlusion at the elbow and flush. A Venturi effect flattens the reservoir bag if the inner tube is patent. |
|
|
What is the Venturi Effect?
|
A fluid flowing through a constricted section of a tube undergoes a decrease in pressure
|
|
|
What is the Bernoulli's principle?
|
an increase in the speed of the fluid occurs simultaneously with a decrease in pressure or a decrease in the fluid's potential energy
|
|
|
What are the advantages to a non-circle breathing system?
|
- Simple and sturdy
- Only one moveable part (pop-off valve) |
|
|
What are the disadvantages to a non-circle breathing system?
|
High flow rates required / rebreathing CO2 if too low
CO2 monitoring is not specific or accurate Moisture and heat loss with high flow rates Many different types/incorrect assembly problems |
|
|
What determines the amount of CO2 being rebreathed?
|
Fresh gas inflow rate
Minute ventilation Mode of ventilation (spont. Vs. controlled) Vt RR I:E ratio Duration of expiratory pause Peak inspiratory flow rate Volume of resevoir tubing Volume of breathing bag Ventilation by mask vs, ETT CO2 sampling line |
|
|
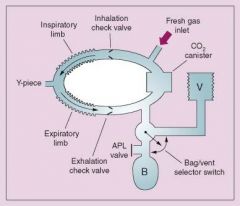
Circle Breathing System
|
|
|
|
What are the components of a Circle system?
|
- Fresh gas inlet
- Gas monitor sensor - Airway pressure sensor monitors / disconnect alarm - Unidirectional valves - Tubing and Y piece - Respirometer - APL valve - Reservoir bag - Bag/vent switch - CO2 absorber - Pressure manometer |
|
|
Where is dead space in a circle system?
|
distal to the Y- piece
|
|
|
What decreases mechanical dead space?
|
Trachs
|
|
|
What is anatomical dead space?
|
Alveolar dead space + Physiologic dead space (150 ml in adults)
|
|
|
What is tidal Volume?
|
Vt= Va + Vd
( alveolar ventilation and gas that is dead space ventilation) |
|
|
What is Minute Volume?
|
Vt x F = Vm
|
|
|
What is Fick's law?
|
Rate of diffusion of oxygen across the alveolar-capillary membrane is directly proportional to :
1) Tissue area 2) Difference in gas partial pressure between the two sides |
|
|
In the alveolar-capillary membrane , what is inversely proportional to tissue thickness?
|
effective diffusion
|
|
|
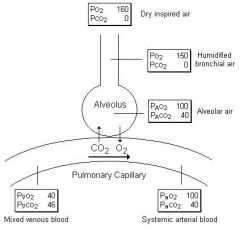
Gas Exchange in the lungs
|
|
|
|
What is the alveolar gas equation?
|
PiO2 = (PB – PH2O) FiO2
PAO2 = PiO2 – (PaCO2/RQ) PAO2 = alveolar oxygen concentration PB = barometric pressure PH2O = water vapor pressure is ~ 47 mmHg FiO2 = inspired oxygen concentration PaCO2 = arterial carbon dioxide concentration RQ = respiratory quotient, norm 0.8 |
|
|
What does the alveolar gas equation determine?
|
The alveolar O2 partial pressure
|
|
|
What is normal RQ ?
|
0.8 ( ratio of carbon dioxide production to oxygen consumption)
|
|
|
What alters RQ?
|
Altered by dietary extremes
Carbohydrates 1.0 Normal 0.8 Fats 0.7 |
|
|
What is the A-a gradient?
|
a measure of how effectively oxygen that is in your alveoli moves into your pulmonary vasculature.
A-a gradient = PAO2 – PaO2 Norm 5-10mmHg, but increases with age |
|
|
In zone 1 which is greater? the alveolar pressure or the venous pressure?
|
Zone 1- PA>Pa>Pv
|
|
|
In zone 2 which is greater , the Venous pressure or the arterial pressure?
|
Zone 2- Pa>PA>Pv
|
|
|
In zone 3 which is greater the Arterial pressure or the alveolar pressure?
|
Zone 3- Pa>Pv>PA
|
|
|
What attributes to the intrapulmonary shunt?
|
Anesthesia – 14% Shunt
Pnuemonia Acute respiratory distress syndrome Patent foramen ovale Atelectasis |
|
|
What is the physiological shunt?
|
Anatomic Shunt + Intrapulmonary Shunt
|
|
|
What is the anatomical shunt comprised of?
|
Bronchial arteries
Thebesian veins |
|
|
What is the treatment for shunting?
|
Underlying cause
Increased FiO2 PEEP Avoid barotrauma |
|
|
What are 4 dead space etiologies?
|
Pulmonary Embolism
Decreased cardiac output COPD ARDS – pulmonary vasoconstriction |
|
|
Where does the majority of tidal volume go during spontaneous ventilation?
|
The dependent alveoli because they are more compliant
|
|
|
What happens to PVR when cardiac output is increased?
|
Decreases passively due to recruitment and distention
|
|
|
What is recruitment?
|
- Increase in surface area for flow decreases PVR.
- Recruitment is the principal change as vascular pressures increase from low to moderate (Increased pulmonary blood flow increases mean PAP Increased mean PAP opens new parallel pathways for blood flow) |
|
|
What is distention?
|
An increase in mean PAP increases the radius of pulmonary vessels and thus decreases pulmonary vascular resistance
However, Higher PVR occurs at high and low lung volumes |
|
|
What is an example of distention?
|
Ex. One lung ventilation : Increased PVR at low lung volumes diverts blood flow from collapsed alveoli
|
|
|
What is the reason for recruitment and distention?
|
- Decrease PVR
- Prevent major increase in PAP |
|
|
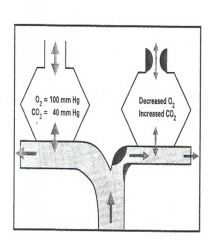
Hypoxic Pulmonary Vasoconstriction
|
|
|
|
What does acidosis do to pulmonary vascular tone?
|
Increases
|
|
|
What does global hypoxia do to pulmonary vascular tone?
|
increases
|
|
|
What neural system controls the decrease of PVR?
|
Parasympathetic stimulation
|
|
|
What hormones control the decrease of PVR?
|
B-adrenergic agonists
Nitric Oxide Prostaglandin E1 |
|
|
What hormones control the increase in PVR?
|
Histamine
Norepinephrine Epinephrine |
|
|
How much oxygen is transported via hemoglobin?
|
20 cc in 15 grams
|
|
|
How much O2 is consumed per minute?
|
250-300cc
|
|
|
How much O2 is extracted in tissues? heart?
|
25-30% . 60-70%
|
|
|
What is the definition of hypoxemia?
|
A decrease in the partial pressure of oxygen in the systemic arterial blood
|
|
|
What is impaired oxygen delivery most often the result of ?
|
Most often due to reduced cardiac output, anemia, or severe hypoxemia
|
|
|
What are some causes of V/Q mismatch?
|
COPD
Pulmonary embolism Pneumonia Pulmonary edema |
|
|
What are some causes of diffusion abnormalities?
|
Emphysema
Pulmonary fibrosis CO poisoning Oxy-Hgb Dissociation curve |
|
|
OxyHemoglobin Dissociation Curve
|
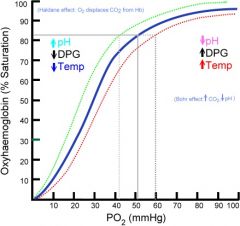
.
|
|
|
What is the partial pressure at P50 on a normal Oxyhemoglobin dissociation curve?
|
27mmHg
|
|
|
What causes a left shift in the Oxyhemoglobin curve?
|
Alkalosis
Decreased PCO2 Decreased temperature Abnormal and fetal hemoglobin Carboxyhemoglobin (↑binding of O2 to Hgb) Methemoglobinemia (benzocaine, prilocaine) Decreased 2,3 DPG |
|
|
What causes a right shift in the oxyhemoglobin curve?
|
Acidosis
Increased PCO2 Increased temperature Increased 2.3 DPG (chronic hypoxia) Inhalation anesthetics |
|
|
What is A-V o2 difference?
|
Represents extraction of oxygen at tissue level
Determines O2 carried versus O2 returned Normal (a-v)O2 is 5 ml |
|
|
How much CO2 is produced each minute during normal matabolism?
|
200-250 cc
|
|
|
Which is more soluble oxygen or co2?
|
Oxygen x20
|
|
|
How is most of CO2 transported?
|
via HCO3 (80-90%)
Carbonic acid (5%) Hb-CO2 (5-10%) |
|
|
What is the best indicator of alveolar ventilation ?
|
PaCO2
PaCO2 is directly proportional to the metabolic production of CO2 and inversely proportional to alveolar ventilation |
|
|
What causes hypercarbia?
|
Fever
Seizures/Shivering Sepsis Hyperalimentation Malignant hyperthermia Tissue reperfusion Sympathetic response to stress (pain) |
|
|
Body response to Hypercapnia
|
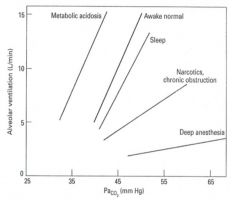
|
|
|
What happens to the CO2 response curve in COPD?
|
Chronically shifted to right
|
|
|
What is the Bohr effect?
|
describes how carbon dioxide and H+ affect the affinity of hemoglobin for oxygen. High CO2 and H+ concentrations cause decreases in affinity for oxygen, while low concentrations cause high affinity for oxygen.
|
|
|
Which way does the oxyhem. curve shift as the CO2 enters blood from the tissues?
|
To the right
|
|
|
What happens as CO2 enters blood from the tissues?
|
tissues shifts the oxyhemoglobin dissociation curve Rightward
Displaces O2 from the hemoglobin Promotes unloading of O2 at tissue level |
|
|
What happes as CO2 enters blood from the alveoli?
|
shifts the oxyhemoglobin dissociation curve Left
Facilitates loading of O2 onto Hgb |
|
|
calculate A-a gradient
|
(age + 10) / 4
|
|
|
calculate oxygen content of arterial blood
|
CaO2 = (1.34)(Hg)(%Sat) + (0.003)(PaO2)
|

