![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
193 Cards in this Set
- Front
- Back
|
Properly do a Mallapati classification
|
Patient sitting head neutral position
open mouth maximally (nml 50-60mm) stick out tongue as far as possible Do not say "Ahh" - makes it better DO not arch tongue - makes it worse |
|
|
airway eval
Atlanto occipital joint extension |
Nml 35 degrees
If cannot do this and anesh tries to extend neck, get bulge pushing larynx anterior, cant see glottis. Extension of only 11 degrees ~ Grade III or IV View |
|
|
airway eval
Anterior mandibular space eval |
Ask pt extend head to max
measure thyroid cartilege notch to tip of mentum/chin. If under 6cm, harder to line up to intubate. (small mandible, short muscley neck. If over 6cm Good sign. The distance from the inner surface of the mandible to the hyoid bone during neck extension should be at least two large fingerbreadths in adults. If the thyromental space is examined, the comparable distance is 50 mm, which is about three large fingerbreadths. There appears to be no difference in the results of using the hyomental or thyromental distances, except that the thyroid cartilage may be easier to locate. These areas are important because the laryngoscope displaces the tongue into this space, and exposure of the glottis may be inadequate if the space is narrowed or noncompliant. A receding or hypoplastic mandible results in a situation often referred to as an anterior larynx or high larynx by clinicians. An inability to bring the lower incisors edge to edge with the upper incisors (i.e., impaired mandibular protrusion) is an important warning that laryngoscopy may be difficult.[10] Conversely, if the lower incisors can be brought forward to bite the upper lip beyond the vermilion, mandibular displacement can be expected to aid intubation. The latter case would seem to diminish the impact of the Mallampati score. |
|
|
Med conditions altering airway mgt
table from Miller |
Table 42-3 -- Selected pathologic states that influence airway management
Pathologic State Difficulty Infectious epiglottitis Laryngoscopy may worsen obstruction. Abscess (submandibular, retropharyngeal, Ludwig's angina) Distortion of airway renders mask ventilation or intubation extremely difficult. Croup, bronchitis, pneumonia (current or recent) Airway irritability with tendency for cough, laryngospasm, bronchospasm Papillomatosis Airway obstruction Tetanus Trismus renders oral intubation impossible. Traumatic foreign body Airway obstruction Cervical spine injury Neck manipulation may traumatize spinal cord. Basilar skull fracture Nasal intubation attempts may result in intracranial tube placement. Maxillary or mandibular injury Airway obstruction, difficult mask ventilation, and intubation; cricothyroidotomy may be necessary with combined injuries Laryngeal fracture Airway obstruction may worsen during instrumentation. Endotracheal tube may be misplaced outside larynx and may worsen the injury. Laryngeal edema (postintubation) Irritable airway, narrowed laryngeal inlet Soft tissue, neck injury (edema, bleeding, emphysema) Anatomic distortion of airway Airway obstruction Neoplastic upper airway tumors (pharynx, larynx) Inspiratory obstruction with spontaneous ventilation Lower airway tumors (trachea, bronchi, mediastinum) Airway obstruction may not be relieved by tracheal intubation. Lower airway is distorted. Radiation therapy Fibrosis may distort airway or make manipulations difficult. Inflammatory rheumatoid arthritis Mandibular hypoplasia, temporomandibular joint arthritis, immobile cervical spine, laryngeal rotation, and cricoarytenoid arthritis make intubation difficult and hazardous. Ankylosing spondylitis Fusion of cervical spine may render direct laryngoscopy impossible. Temporomandibular joint syndrome Severe impairment of mouth opening True ankylosis False ankylosis (burn, trauma, irradiation, temporal craniotomy) Scleroderma Tight skin and temporomandibular joint involvement make mouth opening difficult. Sarcoidosis Airway obstruction (lymphoid tissue) Angioedema Obstructive swelling renders ventilation and intubation difficult. Endocrine or metabolic acromegaly Large tongue, bony overgrowths Diabetes mellitus May have reduced mobility of atlanto-occipital joint Hypothyroidism Large tongue and abnormal soft tissue (myxedema) make ventilation and intubation difficult. Thyromegaly Goiter may produce extrinsic airway compression or deviation. Obesity Upper airway obstruction with loss of consciousness Tissue mass makes successful mask ventilation unlikely. |
|
|
Airway Mgt
Nml mouth opening |
Adults should be able to open their mouths so that there is a 30- to 40-mm distance (about two large fingerbreadths) between upper and lower incisors.
|
|
|
Airway Mgt
Indications for Orotracheal intubation |
Prevent aspiration (recent meal, obstruction)
Need freq suctioning Need Pos Pressure Vent lungs (thoracotomy, NM blockade planned) Any position other than supine planned Site on head, neck, upper airway Mask is hard (no teeth, linebacker) Upper airway dz (cancer) |
|
|
Airway Mgt
How |
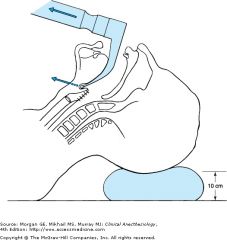
1. Raise table so pts face at level of your xiphoid cartilege so you don't have to bend over.
(CRicoid pressure at induction. Thumb and index finger posteriorly against vertebra.) 2. Patient's crown on pillow. Extend OA about 80 degrees to line up open throat with neck/pharynx tube. 3. Use right thumb to push down pts mandible, use index finger to roll away lower lip so not crushed by blade. 4. L-scope in left hand at junction of blade and handle. Insert at right side of mouth to sweep pts tongue off to the left.Dont crank on teeth esp. max incisors. NEVER LEVER HANDLE TOWARDS YOURSELF. CURVED BLADE/MAC 1. life towards pts feet. |
|
|
ACLS
after shock? if pulse ? |
do CPR after shock
if pulse check BP |
|
|
ACLS
asytole |
ECG gain up and check leads
epi, no shock atropine 1 mg/kg alternate with epi |
|
|
ACLS
v fib and v tach |
shock
5 cycles of CPR for 2 minutes (during this get airway and fluids) At end of CPR check rhythm shock epi amiodarone 300 mg then 150 mg OR lidocaine 1 mg/kg then 1/2 @ 5-10 min intervals |
|
|
ACLS
PEA (ECG can be anything except v fib or vtach) |
5 cycles of CPR
epi no shock Repeat epi 1mg every 3-5 min as long as cardiac arrest. atropine 1 mg if brady (rate <60) 1 mg every 3-5 min up to 3 mg lax dose H's and T's hypovolemia hypoxia Hydrogen ions acidosis (Rx Na bicarb) hypoglycemia Hyperkalemia (Rx Na bicarb) Toxins - drug OD TCA OD (Rx Na Bicarb) tamponade cardiac tension pneumo thrombosis : cardiac or pulm trauma |
|
|
ACLS
slow pulse under 60 bpm |
symptomatic
0.5 mg atropine and transcut pacing |
|
|
ACLS
fast pulse over 150 symptomatic and stable |
vagal manuver (valsava, no carotid massage)
narrow QRS and reg rhythm : adenosine symtomatic and unstable : synch cardiovert |
|
|
ACLS recus
laryngospasm vs bronchspasm |
Both give epi 50 mcg IV
succ will only help laryngospasm For laryngospasm: * pos pressure vent until opens * if unconsc succ Bronchspasm usually asthma or peanut allergy give epi 50 mcg Iv and be ready to repaeat dose in about 3-5 minutes. May need nebs albuterol or racemic epi. |
|
|
ACLS recus
what can cause checst wall tightness and can't ventilate and what is treatment ? |
opiods esp synthetic
fentanyl at induction can't ventilate even with bag, person unresponsive, can't move arms sometimes. IF unconscious : succ If consc : reverse opiod with naloxone |
|
|
ACLS
anaphalaxis |
O2 so sat >95%
moniter cardiac rhythm Epi subQ 0.3 ml of 1:1000 (or IV 50 mcg) and hypotension/severe resp distress If bronchospasm or wheezing : albuterol nebs IV saline Benadyl IV/IM If BP sys below 80 and severe distress repeat epi If in 5 min still hypotension repeat epi if still low BP, dopamine |
|
|
ACLS seizures
|
check glu -> Rx IV glucose D50 or IM glucagon
narcan versed 2-5 mg/min IV/IM |
|
|
pKa of local anesth
|
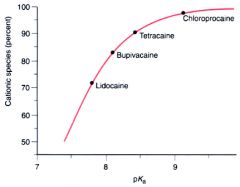
Figure 14-2 The fraction of local anesthetic in the protonated, cationic form in aqueous solution at physiologic pH (7.4) as a function of the pKa of the drug. The drug with the lowest pKa, lidocaine, has the smallest fraction of its molecules protonated and the largest in the neutral form, and vice versa for the local anesthetic with the highest pKa, chloroprocaine. Individual drug molecules become protonated and deprotonated in thousandths of a second in solution.
|
|
|
Inhal An
Rise in alveolar conc of anesth is faster w/ soluble or non-soluble ? Name soluble and non-soluble anesthetics ? |
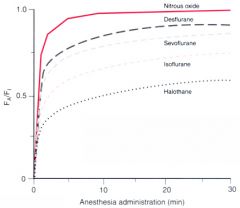
Figure 5-2 The rise in alveolar (Fa) anesthetic concentration toward the inspired (Fi) concentration is most rapid with the
least soluble anesthetics, nitrous oxide and desflurane, and slowest with the most soluble anesthetic, halothane. All data are from human studies. |
|
|
what is 2nd gas effect ?
|
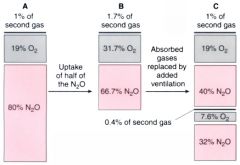
Figure 5-3 A, The rectangle represents a lung filled with 80% nitrous oxide plus 1% of a second gas. B, Uptake of one half of the nitrous oxide does not halve the concentration of nitrous oxide, and the reduction in volume thereby increases the concentration of the second gas. C, Restoration of the lung volume by addition of gas at the same concentration as that contained in A increases the nitrous oxide concentration and adds to the amount of the second gas present in the lung.
|
|
|
what is 2nd gas effect ?
|

Figure 5-4 In patients, administration of 65% nitrous oxide produces a more rapid rise in the alveolar concentration of anesthetic/concentration of inspired anesthetic (Fa/Fi ratio) for nitrous oxide than administration of 5% (i.e., concentration effect, two solid lines). The Fa/Fi ratio for 4% desflurane rises more rapidly when given with 65% nitrous oxide than when given with 5% (i.e., second gas effect, two dotted lines).
|
|
|
Inhal
If you increase ventilation what is effect on conc inhal anesth ? For what gases does this matter more ? |

Figure 5-5 The alveolar concentration of anesthetic/concentration of inspired anesthetic (Fa/Fi ratio) rises more rapidly if ventilation is increased. Solubility modifies this impact of ventilation; the effect on the anesthetizing partial pressure is greatest with the most soluble anesthetic (ether) and least with the least soluble anesthetic (nitrous oxide).
|
|
|
inhal
what about changing CO? |

Figure 5-7 If unopposed by a concomitant increase in ventilation, an increase in cardiac output will decrease alveolar anesthetic concentration by augmenting uptake. The resulting alveolar anesthetic change is greatest with the most soluble anesthetic. Fa/Fi is the alveolar concentration of anesthetic/concentration of inspired anesthetic.
|
|
|
inhal
what effects recovery from an ? |

Figure 5-18 Both solubility and duration of anesthesia affect the fall of the alveolar concentration (Fa) from its value immediately preceding the cessation of anesthetic administration (Fa0). A longer anesthetic slows the fall, as does a greater solubility, and the effects are shown for the increasingly soluble desflurane, sevoflurane, and isoflurane (A to C). The horizontal lines designated (a), (b), and (c) indicate 80%, 90%, and 95% decreases, respectively, in the alveolar concentration from the concentration at the end of anesthesia.
|
|
|
inhal
what is diff hypoxia ? |
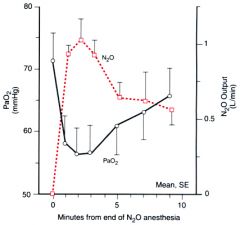
At end of anesh, when turn off nitrous, as it leaves blood, get hypoxia. Prevent by giving 100% O2 at end of anesth.
Figure 5-23 At time zero, the inspired gas was changed from 21% oxygen/79% nitrous oxide to 21% oxygen/79% nitrogen. Arterial oxygen subsequently fell in association with the outpouring of nitrous oxide. |
|
|
inhal
effect of inhal an on vent ? |

Figure 6-13 Comparison of mean changes in resting Paco2, tidal volume, respiratory rate, and minute ventilation in patients anesthetized with halothane (H), isoflurane (I), enflurane (E), sevoflurane (S), desflurane (D), or nitrous oxide (N). Anesthetic-induced tachypnea compensates in part for the ventilatory depression caused by all volatile anesthetics (i.e., decreased minute ventilation and tidal volume and concomitant increased Paco2). Desflurane results in the greatest increase in Paco2, with corresponding reductions in tidal volume and minute ventilation. Isoflurane, like all other inhaled agents, increases respiratory rate, but isoflurane does not result in dose-dependent tachypnea.
|
|
|
NMB
dur of effect ? |
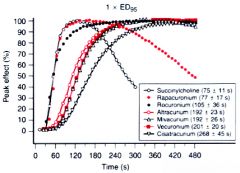
Figure 13-19 Percentage of peak effect after a1 × ED95 dose of succinylcholine, rapacuronium, rocuronium, atracurium, mivacurium, vecuronium, and cisatracurium at the adductor pollicis muscle. Times (mean ± SD) in seconds to 95% of peak effect are shown in parentheses.
|
|
|
nmb
Binding site of non depol vs depol nbm ? |
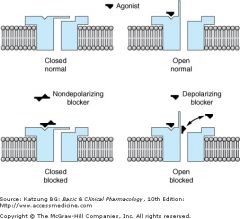
Depol are agonists.
NonDepol are compet antagonists. Top: The action of the normal agonist, acetylcholine, in opening the channel. Bottom, left: A nondepolarizing blocker, eg, rocuronium, is shown as preventing the opening of the channel when it binds to the receptor. Right: A depolarizing blocker, eg, succinylcholine, both occupying the receptor and blocking the channel. Normal closure of the channel gate is prevented and the blocker may move rapidly in and out of the pore. Depolarizing blockers may desensitize the end plate by occupying the receptor and causing persistent depolarization. |
|
|
nmb
ToF and tetanus response to depol and non-depol nbm ? |
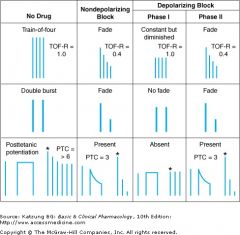
Fade: indicates NON-depol block, may show pre-junct action of NMB reducing amt of Ach. when fade is gone -> sign of clin recovery.
Post-tetanic facilitation : when do tetany (long 5 sec stim) and then twitch and see greater twitch response = 'POST TETANIC FACILITATION. See in partial non-depol block. Shows partial inc in Ach from tetanic stim. A phase I block (succ, depol) in contrast, no fade, no ToF, no post-tet facilitation.But if keep giving succ, changes to phase II block which ressembles a non-depol block. In the train of four (TOF) pattern, four stimuli are applied at 2 Hz. The TOF ratio (TOF-R) is calculated from the strength of the fourth contraction divided by that of the first. In the double burst pattern, three stimuli are applied at 50 Hz, followed by a 700 ms rest period and then repeated. In the posttetanic potentiation pattern, several seconds of 50 Hz stimulation are applied, followed by several seconds of rest and then by single stimuli at a slow rate (eg, 0.5 Hz). The number of detectable posttetanic twitches is the posttetanic count (PTC). (*, first posttetanic contraction.) |
|
|
iv
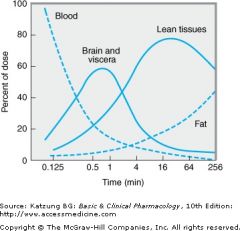
thiopental : time to redist to VRG ? fat ? |
|
|
|
local
ester vs amide ? |
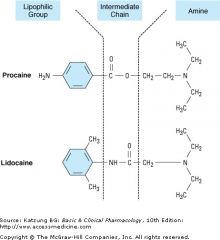
Structures of two prototypical local anesthetics, the aminoester procaine and the aminoamide lidocaine. In both drugs, a lipophilic aromatic group is joined to a more hydrophilic tertiary amine base, by an intermediate amide or ester bond.
|
|
|
local
channel binding state ? |
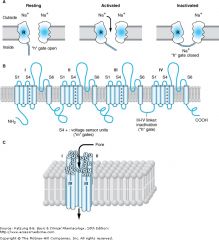
Functional and structural features of the Na+ channel that determine local anesthetic (LA) interactions. A: Cartoon of the sodium channel in an axonal membrane in the resting (h gate open), activated (h gate open), and inactivated states (h gate closed). Recovery from the inactivated, refractory state requires opening of the h gate. Local anesthetics bind to a receptor (R) within the channel and access it via the membrane phase or from the cytoplasm.
|
|
|
local
types of injections near spine ? |
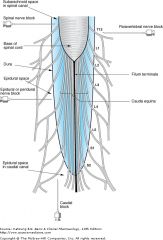
|
|
|
iv
type of opiod receptors ? opiods MOA ? |
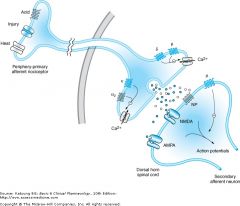
Act inside and outside CNS
potency : ~ afficnity for R , levo-iso more effective MOA: dec neurotransmission as PRE-SYN inhib of NT (Ach, subt P). Also opiod R activation inc K+ conduction so cell hyperpolarized. Mu-1 : supra-spinal anal, spinal, euphoria, miosis, urine retain Mu-2 : spinal, vent depression, bradycardia, constipation, phy dependance Kappa : supraspinal , spinal, dysphoria, sedation, miosis Delta : supraspinal, spinal, vent depression, urine retain, phy dependance |
|
|
airway
how insert LMA ? |
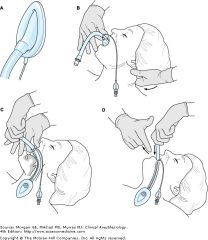
A: The laryngeal mask ready for insertion. The cuff should be deflated tightly with the rim facing away from the mask aperture. There should be no folds near the tip. B: Initial insertion of the laryngeal mask. Under direct vision, the mask tip is pressed upward against the hard palate. The middle finger may be used to push the lower jaw downward. The mask is pressed forward as it is advanced into the pharynx to ensure that the tip remains flattened and avoids the tongue. The jaw should not be held open once the mask is inside the mouth. The nonintubating hand can be used to stabilize the occiput. C: By withdrawing the other fingers and with a slight pronation of the forearm, it is usually possible to push the mask fully into position in one fluid movement. Note that the neck is kept flexed and the head extended. D: The laryngeal mask is grasped with the other hand and the index finger withdrawn. The hand holding the tube presses gently downward until resistance is encountered
|
|
|
airway
proper placement Mac blade ? |
|
|
|
airway
view w. curved blade / Mac |
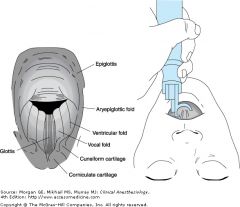
|
|
|
airway
diff airway algo |

|
|
|
inhal
what effects uptake of gas ? |
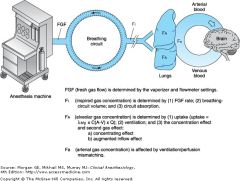
Inc rate of induction:
inc anesth conc inc fresh gas flow inc alv ventilation ** dec COoutput (alveolar blood flow, predispose to anesthetic ODose) 2nd gas effect non rebreathing ** low blood:gas SOLUBILITY (diff in part pressure of alv gas and venous blood) GREATER the uptake of anesth agent, greater diff between inspired and alveoli conc, and slower the rate of induction. NB :Slows induction :shunt whereas wasted ventil to nonperfused alv no change |
|
|
PreOp
General testing : when do ECG ? Hgb ? glu and creat/BUN ? When CXR ? PFT ? |
when do ECG ? General An men over 40 and women over 50
Hgb ? gen all women ; men over 50 glu and creat/BUN ? Over 65 CXR ? over 74 PFT ? COPD and upper abd sx NB 2-7% labs abn |
|
|
PreOp labs
MAC or regional |
Over 50 : Hgb in last 6 mnths
Over 65: Hgb (6 mnths) ECG: last year Over 74 : In last 6 mnths hgb, creat/BUN, glu, AND ECG |
|
|
PreOp
ASA for : poorly cont HTN DM vascular comps angina prior MI pulm dz that limits activity |
ASA 3
severe systemic dz limits funtional activity |
|
|
PreOp
ASA for controlled and mild (no severe comps) HTN DM chrn bronchitis morvod obesity exteme age |
ASA 2
mild well controled dz no functional limitations |
|
|
PreOp
unstable angina CHF adv pulm, renal, liver dysfunction |
ASA 4 : severe systemic dx constant threat to life.
Note: ASA does not count dz being operated on that will be fized by opeartion. IE Gb dz for GB sx |
|
|
PreOp
ASA ruptured Aneur PE head injury w/ high ICP |
ASA 5
moribund, will die without operation |
|
|
PreOp
ASA brain dead organ donor |
ASA 6
|
|
|
PreOp
Plan What is regional anesth ? |
Epidural / spinal / caudal
Pt conscious + : GI and skel m relaxed Use for lower leg and GI sx -: may not have enough sens anal, See drop in BP esp if hypovolemic |
|
|
PreOp plan
peripheral N block |
when :
sx on arm or leg +: keep airway reflex so good pts lung , kidney, heart dz Sx: AV shunt -: occ not enough sens and motor anal Poor choice drunk/agit as key to it is technique and skill at block. |
|
|
Intub
drugs |
preox
LOC : propofol / etomidate +/- opiod blunt pressor resp to intubate +/- lido paralyze: succ/rXXX intubate |
|
|
PreOp
how to check intub in trachea |
capnograph > 20 mmHg CO2 with exhale
pulse ox over 95% |
|
|
Pre Med
why clonidine ? |
sedate
blunt ANS (HTN, tachy, catach from anx and surg stim) |
|
|
PreMed
why anti-hist |
promethazine w/ mepiridine to augment sedation w/o inc Resp depression.
diphenhydramine with cimetidine to dec chance of allergy (contrast dye in atopic pt) |
|
|
PreMed
Who gets anto-acid meds |
pregnant
GERD Sx reflux obese diff airway |
|
|
PreMed
metoclopromide |
IV acts in 1-2 min use for emergency sx in pts who ate
PO : 30-60 min pre DM preg recent ate and nonGI sx, diff airway SE : can go to brain EPS |
|
|
PreMed
for anti-sial effects only |
glycopyrrolate
strong anti-sial (vs atropine) and 2 duration |
|
|
PreMEd
anti sial and sedation |
scopolamine
SE CNS toxicity delerium esp elderly as crosses BBB. Also mydriasis/cyclo. |
|
|
PreMed
When use atropine |
Kids to prevent vagal bradycardia with propofol and other anesth
Has antisial, sedative, CNS toxicity. Can cause tachycardia. |
|
|
PreOp
Fasting food breast milk formula |
fast light meal 6 hrs
non human milk " formula " BREAST milk 4 hrs clears 2 hrs (ice chip, gum, candy) 2 hrs |
|
|
PreOp
anti nausea meds More nausea : female, h/o, Sx: gyne, eye, cosmetic, ortho shoulder, general >regional |
phenergan : histamine
ondasertron 5HT3 blocker droperidol low dose, dopamine blocker, SEDATES, give after benzo or dysphoria. Droperidol can SEDATE but pt still anxious. scopolamine anti-chol Decadron/corticosteroid |
|
|
IV
effect on BP ? |
Drop BP:
* thiopental * propofol Minimal to no drop: * etomidate midozolam INCREASE BP * ketamine |
|
|
IV effect on HR ?
|
Dec HR
none increase HR thiopental (as drop BP) ketamine |
|
|
IV effect on ICP ?
|
increase ICP :
ketamine dec : ** thiopental : barbs used as Rx for high ICP propofol etomidate midozolam neutral to dec |
|
|
IV effect ventilation ?
|
all depress ventilation except ketamine which has dose dep depress of ventilation.
At low doses, does not but since you give with Versed, do see depression of vent. |
|
|
IV Na and Vomiting ?
|
Dec in N/V:
propofol Increase: etomidate ketamine |
|
|
IV adrenocort supress ?
|
etomidate and some midozolam
|
|
|
IV
barbs effect of adding sulfer methyl |
sulfer : (thiopental, thiaamytal)
more lipid soluble, hypnotic, rapid onset and sht duration Oxy: methohexitol shortens duration NB: MOA depress retic activating system and transmission thru sym ganglion as dec rate of dissociation of GABA from R. ALSO hyperpol mmb post-syn so inhibit post-syn neurons |
|
|
IV barbs
PK |
awake as redist
elim due to metab Distribution : lipid solubility and tissue blood flow |
|
|
change EEG ?
|
barbs : isoelectric EEG w/ hypnosis also dec ICP and CBF and CMRO2
benzo: isoelectic etomidate: activate epiletic foci with myoclonus ketamine: myoclonus but NO seiz on EEG |
|
|
IV
Methohexital |
histamine
CV: mild dec BP with mild tachycardia, dec CO and contractility RR: trans stim then apnea, less responsive to CO2, dec RRATE and TVol, can see bronchospam/laryngospams at light depths, Brain: dec ICP and CBF and CMRO2 methohexital VS thiopental more un-ionized 2.5x as potent Neg: no skel m relaxation, occ excitatory, hangover, CI poryphries |
|
|
IV
propofol a phenol MOA |
GABA -R
dec dissociation prolonged opening Cl ch hyperpol mmb no impulse conduction |
|
|
IV
propofol PK |
Onset: rapid LOC in 30 sec
Rapid awake Redist, clear, metab fast: clearence faster than hep blood flow. Can give cont IV infusion, no cum effect. |
|
|
Iv
propofol CNS RR CV AE |
Propofol
CNS : dec ICP CBF CMRO2; keeps tuoreg to CO2 level RR: dose dep dec resp and transient apnea, bronchodilation CV: dec SVR, dec MAP, neg inotrope, No change in HR, depressant CV more than thiopental esp older pts, hypovol, those on ACE-I |
|
|
IV
propofol Allergies |
has egg
soybean oil sulfite glycerol |
|
|
Iv
etomidate a carboxylate imidazole PK? |
MOA:
enahnce GABA PK: Onset : LOC in 30 sec rapid awake as re-dist, no hangover rapid clearence metab by hydrolysis little cm effect |
|
|
Iv
etomidate CNS RR AE |
Etomidate
CNS: dec CMRO2, CBF, ICP, can + seizure foci on EEG but an anti-convulsant, MYOCLONUS RR: transient dose-dep dec Tidal vol and inc RRate CV: modest BP dec due to dec SVR, minimal myocardial depression AE: myoclonus, pain on inject, bugs, adrenocort supress 11Bhy-ase lasts 4-6 hrs post induction dose. HIgh % N/V |
|
|
IV
ketamine MOA |
NMDA R
opiod R monamine R muscarinic R Ca ion ch NOT gaba R stimulates central nerv system stim Sym Nerv system inhibits reuotake of norepi |
|
|
IV ketamine
PK |
rapid onset: high lipid soluble, easily ionized in body, rapid brain uptake
redist from brain and VRG, dist t1/2 10 min metab : microsomal, active metab; induces liver enz (tolerance) Shrt elim halflife of 2 hr as extensive liver uptake 0.9 |
|
|
IV ketamine
CNS RR CV |
CNS: VASODILATOR inc CBF and ICP, manage effect w. proper ventilation, MYOCLONUS w/o seizure on EEG, anti-convulsant
RR: min depression of resp, if give IV w/ opiods can see apnea, BRONCODILATION, SALIVATION, HYPERTONICITY upperairway keeps reflex CV: like SNS stim inc BP, PAP, HR and CO |
|
|
IV ketamine
and emergence delerium |
See with doses > 2 mg/kg Iv
females over 16 personalit d/o and freq dreams Prevent by predose w/ benzos |
|
|
IV benzos
useful as adj b/c MOA |
anx reduce
sedate amnesia minimal dep CV and resp anti-convulsant RELAX SKEL M rare allergy MOA: enhance GABA Cl channel, hyperpol ch, usually post-syn nerves in CERBRAL CORTEX midozolam has 2x affiity vs diaz for R |
|
|
IV
benzo PK |
lipid sol so rapid to CNS
resdist metab: Diaz-> liver to active metabolites t1/2 2-3 days Midozolam -> liver p450 3A4 inactive metabolite t1/2 1-4 hrs lorazepam -> not active metabolite, t1/2 10-20 hrs |
|
|
Iv benzos
CNS RR CV |
CNS : dec CMRO2 and CBF, isoelectric EEG, no effect ICP, anti-convul, no neuroproective effect
RR: min depr alone but apnea with opiods CV: stable but esp w/ induction midozolam can get dec SVR which can drop BP |
|
|
IV benzos
injection rxns ? |
diazepam no water soluble, has propylene glycol -> thrombophlebtitis
ativan also thrombo but no prop glycol. Both hurt with injection. Not water soluble. |
|
|
Iv benzo reversal
do reverse what? do not reverse what ? |
reverse CNS effect
but not amnesia DO not see anx, HTN, tachy or stress like with narcan. Need much less with kids. adults 0.2 mg titrateup to 10 mg kid 0.01 mg/kg up to 1 mg |
|
|
Iv opiods
effects ? Why good as premed ? |
analgesia
no loss of touch, propio or LOC Good pre-med: anal lines, no direct myo depres, delays time to need post-op pain med. |
|
|
IV opiods
morphine |
IV
peak onset : 20 min Effects: smooths out HR to surg stim (less inc) AE: depress resp at medulla, Nausea by stim central, ortho hypo as periph vasodil, |
|
|
IV opiods
fentanyl |
fentanyl
Peak onset 1 min Effects : evens out HR (less rise w. surg stim) |
|
|
IV opiods
which R do vent depression ? |
Mu-1 : supra-spinal anal, spinal, euphoria, miosis, urine retain
*** Mu-2 : spinal, vent depression, bradycardia, constipation, phy dependance Kappa : supraspinal , spinal, dysphoria, sedation, miosis *** Delta : supraspinal, spinal, vent depression, urine retain, phy dependance |
|
|
IV opiods
which R do spinal and supraspinal anal ? |
*** Mu-1 : supra-spinal anal, spinal, euphoria, miosis, urine retain
ONLY SPINAL Mu-2 : spinal, vent depression, bradycardia, constipation, phy dependance *** Kappa : supraspinal , spinal, dysphoria, sedation, miosis *** Delta : supraspinal, spinal, vent depression, urine retain, phy dependance |
|
|
IV opiods
which R do sedation ? |
Mu-1 : supra-spinal anal, spinal, euphoria, miosis, urine retain
Mu-2 : spinal, vent depression, bradycardia, constipation, phy dependance *** Kappa : supraspinal , spinal, dysphoria, sedation, miosis Delta : supraspinal, spinal, vent depression, urine retain, phy dependance |
|
|
IV opiods
which R do bradycardia ? |
Mu-1 : supra-spinal anal, spinal, euphoria, miosis, urine retain
*** Mu-2 : spinal, vent depression, bradycardia, constipation, phy dependance Kappa : supraspinal , spinal, dysphoria, sedation, miosis Delta : supraspinal, spinal, vent depression, urine retain, phy dependance |
|
|
IV opiods
compare potency of morphine meperidine alfent fent remifent sufent |
morphine 1.0
meperidine 0.1 (so 1/10 as strong) alfent 10-25 fent 75-125 remifent 250 sufent 500-1000 |
|
|
IV opiods effects
CNS |
Opiods
CNS: depend on R, dec CBF/ICP as long as not hypovent, SKEL M RIGID esp synthetics N/V via central Mepiridine metabolite can cz seizures dec MAC of vol anesth |
|
|
IV
opiods effect RR CV GI |
RR: depress vent via Mu-2 on brainstem, less resp to CO2 and inc PaCO2, dec RRate and inc Tvol,
Some HISTAMINE so inc AIRWAY RESIST, DEC COUGH REFLEX CV: min depress alone, no heart sens to catach, MORPHINE : histamine dec BP, others opiods hypotension as blunt response for vasodilation BRADY: except meperidine (tachy) as stimulate vagus GI: bil colic, dec gastric empty, constipate, GU: urine retain, effect immune system, tolera and phy dependance. |
|
|
IV opiods
Uses in anesht |
anal pre and post sx
induction and main : must give w/ oter drugs for amnesia inhib reflex sym responses suppl inhaled anesth (dec MAC needed) ProS: CV stability, no myocard sens to catech, easy arosal post-op, no end organ toxic, post-op analgesia, Disad: recall, chest wall rigid, postural hypotens, if under dose during procedure HTN and tachy, N/V, bil colic, urine retention |
|
|
IV opiods
naloxone |
reversibly binds opiod R
non specific effect so careful as might reverse analgesia : see HTN, tachy, pulm edema, N/V Duration 30-45 min |
|
|
IV opiods
remifentanyl is special why ? |
Not metab in liver like other opiods.
ULTRA SHORT ACTING ester hydrolsis in plasma, non-specific enz so pts w. aty enz nml wake up. pts with liver dz nml wake up no effect w. long infusion, still wake up in 3 min |
|
|
IV opiods and renal failure
|
pts renal failure and
morphine mepiridine can take days to wake up nor-meprindine can cause seizures and myoclonus not reversible w. naloxone. |
|
|
IN opiods
2nd peak |
fentanyl has 2nd peak
2-4 hrs later |
|
|
IV
barbs and benzo neuroprotection |
barbs neuroprotect NOT benzos
barbs vasoconst brain protect cerebral clot local ischemia prob not global like cardiac arrest |
|
|
Iv
effect on brain opiods vs b's |
Vs benzo and barbs
opiods less of dec in O2 use, CBF, and ICP. And opiods may not blunt inc ICP seen with intubation if pt not asleep enough. high doses fent : occ seiz activ might be muscle ridigity mepiridine : seiz activity |
|
|
IV
what to dec shivering ? |
mepiridine 25 mg
|
|
|
IV
ketamine Who good for ? Who bad for ? |
Good for asthma , early hypovol shock
Bad for: Due to inc HR/MAP/CO: CAD, uncontrolled HTN, CHF, art aneur, severe end state shock w. depleted NE stores |
|
|
PreOp Meds
CI to sedative meds pre-op |
severe lung dz
hypovol impending airway obst high ICP/intracranial pathology depr mental status under 1 yr or elderly no informed consent to Sx Also some pts may do ok with some anx, may be better then IM or long hangover for sht ambul sx |
|
|
PreOp meds
who does well with pre-op sedation |
kids for separation
drug abusers to avoid w/drawal med cond where stress bad: CAD, HTN Pre Heart sx Cancer sx / pre-op pain Regional anesthesia And pre-op opiods help induction. |
|
|
nmb
metabolism of depol vs nondepol |
Ach: metab by AchEase in cleft
depol : diffuse away, metab psesudoAchE in plasma, nonspecific esterases, or butrylcholesterase NonDepol : redist, grad metab, excretion by body OR giving reversal agents (except mivacurium) |
|
|
NMB
Why don't kids get succ? |
Hyperkal
rhabdo cardiac arrest in unrecog myopathy |
|
|
nbm
potassium and succ |
K will rise 0.5 mEq/L
CA rise life threat in: burn trauma, hemm shock w/ met acidosis neuro d/o (GBS, stroke, myopthies like duchennes, encephalitis, severe parkinsons, tetanus, polyneurpathy, severe intra ab infection spinal cord injury prolonged immobiliaztion ruptured cerbral aneurysm/closed head injury Reason is immature extrajunct AchR release excess K. |
|
|
nmb
rule w. potency and speed of onset ? |
more potent -> longer onset
|
|
|
nmb
excreted by kidney and prolonged effect in renal failure ? |
doxacurium
pancuronium pipecuronium (vec) |
|
|
nmb
effect of CHF or cirrhosis ? |
larger Vd and smaller plasma conc for given dose.
So may need larger starting dose and then smaller main dose |
|
|
NBM
cisatra and atra metab ? |
nonspecific Hoffman elim
to laudanosine no NMB but CNS excitement |
|
|
nmb
mivacuronium ? special ? |
like succ metab by plasma psuedochlEase
tiny bit by Achase Prolonged in pts aty enx or low levels |
|
|
nmb
pancuronium special ? |
vagolytic
catech release from adren N -> HTN and tachy |
|
|
nmb
long term use vec in ICU ? |
days long NM blockade on wake up
active metab accum OR devel of polyneuropathy |
|
|
NMB
which drug is like succ ? |
Rocuronium 0.9-1.2 mg/kg
onset like succ in 60-90 sec for RSI but has longer duration |
|
|
NMB
succ prolonged by |
onset 30-60 sec, low lipid soluble
duration 10 min , as serum levels falls drug diffuses away Prolonged only modestly in : preg, hypothermia, liver dz DRUGS: echothiophate, neostig, pyridostim phenelzine (MAOI) cancer drug (cyclophosphamide) metoclopromide esmolol pancuronium OCP abx -mycin, glycosides, cycin, linc inhal anesth, LA, lithium Mg citrate anti-arrthy |
|
|
NMB
gene varients and succ |
Abn genes
hetero 1/50 pts 20-30 block, dibucaine inhibited 40-60% homo 1/3000 pts 4-8 hrs, dibucaine inhib 20% (nml enz inhib by dibucaine 80%) |
|
|
NMB
nondepol drug effects |
DECRASED response:
*** echothiophate, neostig, pyridostim UNLIKE SUCC anti-seiz meds prolonged abx -mycin, glycosides, cycin, linc dantrolene inhal anesth, LA, ketamine Mg citrate anti-arrthy' |
|
|
NMB
effect of cholinesterase inhibitors ? non depol succ ON EFFECT OF OTHER 3? |
Ex neostimgine and pyridostigmine
Prolong depol succ Phase I block : - inhibit AchE so more Ach in terminal so more depol - reduce hydrolysis of succ by inhibit pseudocholAse Organophos pesticides prolong succ to 30 min NonDepol blockers: - sm doses occupy some Ach R so partly block succ phase I depol effect - Exception is pancur which augments succ by blocking pseudocholAses Succ will reduce doses needed of nondepol blockers for up to 30 min, if if give enough succ to create phase 2 block, a nonpol will creat paraylsis |
|
|
NMB
succ and fasciculations |
Seen in adults not kids and elderly
Prevent with pre-treat small dose non-depol This antag the block with succ so need more succ. |
|
|
NMB
random odd AE succ? |
inc IOP so no use open globe
myalgias : pretz rocur/NSAIDS and occ myoglobinuria Intragastric pressure inc masseter M ridgid malig hyperthermia myotonic pts get myoclonus slight inc ICP but not as much as intubation slight histamine |
|
|
NMB
release histamine |
atracur
mivacur |
|
|
nmb vagal block
|
pancur
|
|
|
nmb liver
|
pan and vec metab by liver : have active metab
Biliary excr : vec and rocur Liver failure prolongs : pancur and rocu , less effect on vec |
|
|
NMB
nondepol onset |
slow onset: doxo 4 min
mod rapid : others 2-3 min rapid rapid: rocur 1.5 min |
|
|
NMB
nondepol duration |
duration
short : mivacurium (plas enz) 15-20 min INTERMED: atra onset 2.5-3' Dur 30-45' cisatra Onset 2-3' Dur 40-75' vec Onset 2-3' Dur 2-3' 45-90 ' roc Onset 1.5 min DUR 35-75 min LONG: All renal elim doxa onset 4min Dur 90-150' pancur onset 2-3' Dur 60-120' pipe onset 2-3' Dur 80-120' |
|
|
delayed awakening GA old man
Differential ? |
*hypotension to brain (worse if chr HTN)
*stroke *renal/liver dz less drug clear *DM hyperosm coma or hypogly *severe hypothyroid * Malig hyper: dont see delay awake but can see somnolence, PRIOR OK ANES DOSE NOT R/O malig hyper !! *home drugs that dec MAC : ldopa *ethanol intox, old and benzos *less hepatic flow (cimetidine) *additive anti-chol effects w/scopol and sedatives like opiods (esp low CO and IM) *hypothermia *hyponatermia * intraop hyperventil so high trigger of PaCO@ to spont breath * art hypoxia or hypercapnia Do ABG and serum Na PE pupils - should not be fix and dilated unless gave atro/scopol VEntilate, narcan, flumenazil, physostimg (jaw thrust test for paralysis vs coma) If prior GA and no probs can rule out aty enz Unlikely low levels of enz (not see apnea) |
|
|
NMB
nicotinic R muscarinic R |
Nicotinic R
stimulate autonomic ganglia skel m R Agonists: Ach, nicotine Antag : NonDepol relaxants Muscarinic R activate end organ effectors bronchial sm m : bronchoconstrict salivary glands/gastric glands : secrete Heart SA node, AV node : dec HR Smooth m bronchi, GI, bladder, blood vessels Agonist drugs : Ach, methacholine, bethanechol Antag: antimuscarinics - atropine, scopolamine, glycopyrrolate Carbachol for glaucoma: both R |
|
|
NMB
neostigmine |
AchAse inhibiter
Main use reversal of NMBlockade MOA: indirectly inc amt of Ach in cleft to compete w/ non-depol agent by irrever bind to AchE enzyme Neostim has direct weak effect of agonst on nicotonic R pre-syn so might inc release of Ach. In excess doses, paradoxically potentiate nondep block. Also potentiate depol block of succ - inc Ach - inhibit pseudocholAse Also have muscarinic SE: CV: brady and brady arrhy Pulm: bronchospasm, sec Cerebral excitation w/ physistigmine only GI spasm and saliva GU bladder tone inc Pupil constritct |
|
|
inhal
what inc rate of recovery from anesth |
inc fresh gas flow
inc alv ventil non re breathing low blood gas solubility low tissue blood solubity dec duration of anesthetic Recovery differs from induction as: no conc effect metab can dec part pr alveoli |
|
|
inhal
speed recovery |
elim rebreathing
high fresh gas flow low anesth circit vol / low absorb by circuit low solubility high cerebral blood flow inc ventilation |
|
|
elements of total anesth for GA
|
reversible LOC
anal entire body amnesia some muscle relax |
|
|
inhal
potency relates to what ? |
lipid solubility
(meyer-Overton rule) suggests common MOA unitary hypothesis |
|
|
inhal
halothane hepatitis |
obese women with 2 doses
1/ 35,000 family or personal h/o of it |
|
|
inhal and coronary arteries
|
Isoflo dilates cor Art but not as much as nitrogly or adenosine.
theory possible cor A steal in times of tachycardia or drop in perf pressure |
|
|
inhal
des solubility ? what is give rapid inc ? |
Des low soluble fast induction and fast recovery
Rapid inc in dose -> inc HR, BP, catech release in pts, esp bad if CAD. (worse then with iso) |
|
|
inhal
non stinky |
sevo
non pungent rapid induction wheras for adults generaly other gases not as prefered for induction. |
|
|
inhal
no change in MAC |
duration Or mech of an
gender thyroid dz hyper or hypo kalemia PaCO2 15-90 PaO2 over 38 spine cord injury |
|
|
inhal
increase MAC |
HYPERthermia
Drugs that inc catechol - MAOI, TCA, coke, acute speed INFANTS 1yr over HYPER NATREMIA possible alcoholism |
|
|
inhal
dec MAC |
- HYPO thermia
- MEDS: preop med, IV anesth, acute ethanol ingestion , opiods in spine, alpha2agonists : clonidine - Elderly, - under 1 yr old/neonates - PREGNANT and post-partum by 3 days - PaO2 under 38 / HYPOXIA - hypotension BP under 40 - lithium - HYPONATREMIA - Cardiopulm bypass |
|
|
inhal effects Resp
|
- dec resp to PaCO2 at carotid body
- rapid breathing / rise in RRate - shallow / dec in tidal vol Rise in PaCO2 unless mech vent dose dep Not seen with nitrous |
|
|
inhal
airway resist |
inhal bronchodilators as relax sm m
SEVO the most, and halo Except iso and esp DES can cause coughing, breathing holding, layrnspasm, secns |
|
|
inhal effects CV
|
- direct myocard depression in vitro esp bad if CHF
- iso/des/sevo periph vasodilate -> dec MAP, no change in CO, inc HR, they dec SVR - halo : dec contractility and dec CO -> dec MAP, no change in HR, no change in SVR Effect on CVP: all inc except sevo due to inc in pulm vasc resist. nitrous also inc pulm vasc resist esp in pts with pulm HTN already Nit : no change in MAP so if mix with vol anes see less of a drop in BP |
|
|
inhal
effects CNS |
All vasodil inc CBF
dec cerebral metabolic rate inc ICP |
|
|
inhal
nitrous sym mimetic effects |
inc plasma catech
mydriasis inc body temp sweaty inc CVP / R at pressure vasoconst systemic and pulm system |
|
|
inhal
renal effects: liver: |
inhal
renal effects: dec blood flow and GRF liver: dec art and portal flow, |
|
|
inhal
nitrous +/- |
Pro
fast uptake/elim min resp and CV depression nonpungent, no malig hyper Con combust, closed air space expands, B12 inactivation, lacks potency |
|
|
inhal
halothane |
Pros
potent STABLE HR Con needs preserv slow uptake and elim biotrans -> toxic idio syn hep necrosis sens heart to catech trigger malig hyper |
|
|
inhal
iso |
pro
** dec CMRO2 stable CO (slight inc HR maybe ) Con tachy at greater conc pungent trigger MHyper |
|
|
inhal
des |
Pro
rapid uptake and elim Dis pungent tachy w. rapid inc dose need special vaporizer $ trigger M hyper |
|
|
inhal
sevo |
Pros
rapid uptake and elim non pungent less myocardial depression stable HR Dis: reacts w. CO2 absorber release Floride $ trigeer M Hyper |
|
|
inhal
enflo |
Pro
stable HR ** muscle relax Dis: EEG seizure myocardial depression trigger M hyper |
|
|
inhal
myocardial depression ? stable HR ? |
myocardial depression ?
Bad : enflu Less: sevo , nitrous stable HR : halo unless catech enflu, sevo Tachycardia w. greater conc: iso, des |
|
|
nitrous
|
cant use alone : MAC 105
good analgesia expands air pockets does not sens myo to catach no change in BP MOA: inhibits NMDA glut ch for Ca |
|
|
which sens heart to catech
|
halo
maybe enf and iso |
|
|
which worse resp depressants
|
des and enfl
some brochodilate : halo and sevo irritate : des cough and enfl |
|
|
a blood gas part co:eff of 0.5 means what ?
|
it is LOW
INsoluble so fast onset and fast recovery. LIKE nitrous des sevo |
|
|
what does a MAC of 1% mean ?
|
??
|
|
|
local
list esters |
ESTERS have 2 I's
esters are older and cocaine is older. procaine tetracaine occ spinals |
|
|
tetracaine
|
ester
very potent 16 high lipid soluble long duration USED topical spray for bronchoscope |
|
|
Cocaine
|
esters
not as potent medium duration VASOCONST unlike others (which dilate) USe for nasal hemm and for nasal scoping. |
|
|
benzocaine
|
topical ester
SE contact derm PABA methHgb and dec O2 carry capacity |
|
|
procaine / novocaine
|
ester
local sht dur low potency low lipid solubilty small Use IV regional 4/1000 CNS stim -> convulse |
|
|
Lidocaine
|
Amine 2 I's
clear by liver Low Pka and small -> fast onset med dur Rx lido seizures : prophy in toxicity w. benzos fix acidosis w hyper vent makes ch rested thiopent / versed |
|
|
mepivocaine
|
Amide
slower onset, long duration low lipid solubility low potency (low pka in general low pka is fast on BUT mepivocaine is ) |
|
|
ropivocaine
|
Amide 2 I's
mod/ high potency lipid soluble long duration aka naropin |
|
|
bupivocaine
Pharm ? tox and Rx ? |
aka marcaine
lipid soluble and binds lipids potent amide long duration Given IV : hypotension, AV block, vfib v tack Rx. lipid emulsion and used to do CB bypass |
|
|
DO locals vasodil/const ?
|
Locals intrinsic VASODILATE
lido > mepiv causes more systemic absorb and shorter duration of lido except coke Can add epi to make vasoconst. |
|
|
Adding epi to local does what ?
|
vasoconst
prolong local action limit systemic absorb sec systemic toxic same rate of onset dont add bicarb |
|
|
local lungs clear ?
liver ? renal ? |
lungs :
lido bupiv prilo LIVER clears amides , P450 None by renal as not water soluble. |
|
|
what are lipid soluble ?
|
lipid soluble ones are long duration :
etidocaine tetracaine ropiv VS lido procaine prilocaine mepivocaine |
|
|
local in acid tissue ?
|
more is ionized, kess drug can cross lipid mmb.
|
|
|
local ptn bind ?
|
etido
bupiv tetracaine |
|
|
local binds what order of nerves ?
|
outside on mantle : proximal
small diameter MYELIN faster firing fibers But in life : C fibers: sympathetic postgang pain B sensory motor last (propio pressure touch) |
|
|
where is there more systemic toxicity with blocks ?
|
top is
INTERCOSTAL * CAUDAL * epidural brachial ones : inc scalenes *most blood flow to region |
|
|
prilocaine ?
|
over 600 mg metab o toludine
which makes meth hgb Rx methylene blue |
|
|
local
what is seen on EKG with local poisoning ? |
long PR
wide QRS myocardial depression (brady arrhy AV block ) but w/ bupiv vfib to vtach profound hypotension later as CNS excite to CNS depression |
|
|
what is EMLA ?
|
2.5% lido
prilocaine "eutectic" means melts on skin and can cross dermis but takes 45 min |
|
|
PreMed Iv
CV effects thiopental |
BP drops
HR increase SVR drops |
|
|
PreMed Iv
CV effects propofol |
dec BP
dec SVR dec HR |
|
|
PreMed Iv
CV effects etomidate |
minimal dec all (HR SVR BP)
|
|
|
PreMed Iv
CV effects ketamine |
inc all
HR SVR BP |
|
|
PreMed Iv
CV effects versed |
minimal dec SVR and BP esp w/ med combos
|
|
|
PreMed Iv
CV effects which cause N/V |
thio none
prop dec N/V etomidate increase ketamine increase versed no change |
|
|
PreMed Iv
resp effects |
thio pent : dec
prop dec etom dec ket dose dep when use w. other meds VERSED : NO |
|
|
PreMed Iv
ICP / CBF effects |
thio DEC
prop DEC etomidate DEC ketamine INCREASE versed no change/MINIMAL |
|
|
BARBS which first anal or hypnosos ?
muscle changes ? |
analgesia then hynosis then EEG changes.
No skel m relaxation. |
|
|
propofol MOA
|
hyperpol mmb
acts with GABA R so its dissoc so ch open rapid clearence exceeds hep liver blood flow |
|
|
IV
etomidate RR changes ? GI ? |
Yes,
FAST SHALLOW (unlike barbs) dec TV and inc rate GI: lots of N/V |
|
|
IV
how is potency of opiods determined ? |
affinity for R
|
|
|
special fast cleared opiod
|
remifentanyl cleared by plasma esterases non-specific to inactive metab in blood and tissue cells
|
|
|
lipid soluble of opiods
|
low lipid soluble : morphine, slow onset long duration
high: fentanyl and sufent : rapid onset, sht duration (lipid sol can be taken up by lungs and then given back to sytem circ) |

