![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
19 Cards in this Set
- Front
- Back

Label
|
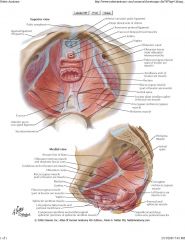
|
|
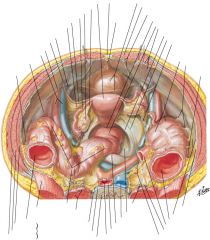
Label these
|
|
|

What is this a picture of?
|
This is looking down into the pelvis where you can see this is a woman as there is a uterus. You see the continuation of the sigmoid colon as the rectum, the straight part of the distal colon descending down into the pelvis. At the end there you see the peritoneal refleciton.
|
|
|
What is the function of the obturator nerve and when do we have to watch for it?
|
The function of the obturator nerve is to adduct muscles of the thigh.
*We have to watch out for the obturator nerve when we are performing: - TURBT of the lateral walls of the bladder. - Node dissection for prostate - Node dissection for cystectomy |
|
|
Of what are the pelvic fasciae made?
|
Collagen, elastic tissue, and smooth muscle adding to the increased strength of these tissues and suggesting a role in support as well as possible function of the pelvis viscera.
|
|
|
What are the three important components of the pelvic fascia?
|
--Anteriorly, the puboprostatic ligaments attach to the lower fifth of the pubis, lateral to the symphysis and to the junction of the prostate and external sphincter. In females, these are called the pubourethral ligaments and insert on the proximal third of the urethra.
--Laterally, the arcus tendineus fascia pelvis extends from the puboprostatic ligament to the ischial spine. In the male, it is between the pelvic side wall and prostate/bladder. In the female, it is the lateral attachment of the anterior bladder wall to the pelvic side wall. --Posteriorly, fascia fans out to either side or rectum and attaches to the pelvic side as wall as the lateral and posterior vesical ligaments (in females, these are the cardinal and uterosacral ligaments). The peritoneum overlying these “ligaments” form discrete folds (rectovesical in male, rectouterine in female) which are easily seen in cystectomies. |
|
|
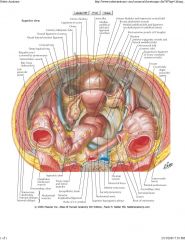
Where does the aorta divide into common iliac and the common iliac divide into internal & external?
|
At L4 and at the SI joint
|
|
|
What is another name for the internal iliac artery? Name the 3 branches of its posterior trunk and what they supply. Name the 7 branches of the anterior trunk and what they supply.
|
The internal iliac artery is also known as the hypogastric artery
POSTERIOR TRUNK: --Superior gluteal (gluteus muscles & overlying skin) --Ascending lumbar (posterior abdominal wall) --Lateral sacral (sacral nerves and sacrum). ANTERIOR TRUNK: --Superior vesical artery (bladder, ureter, seminal vesicles and vas deferens) --Middle rectal (seminal vesicles, prostate, ureter, bladder and rectum) --Inferior vesical artery (lower ureter, bladder base, prostate, seminal vesicals, vagina) --Uterine artery (uterus, bladder, ureter) --Internal pudendal (rectum ,perineum, external genitalia) --Obturator artery (thigh adductors & overlying skin) --Inferior gluteal artery (gluteus muscles and overlying skin) |
|
|
What does “water flows under the bridge” refer to in the pelvis, and why does a Urologic Surgeon care?
|
The fact that the uterine artery passes ABOVE and IN FRONT of the ureter, making the ureter vulnerable during the taking of the uterine pedicles, necessitating your presence in WC24 to fix things.
|
|
|
Where is the best place to ligate the dorsal vein of the penis during radical retropubic prostatectomy and why?
|
Distally because it trifurcates into a central superficial branch and two lateral plexuses when it reaches the pelvis.
|
|
|
Name the 3 main groups of pelvic lymph nodes and what they drain.
|
--Internal iliac nodes (presacral , obturator, and internal pudendal nodes) which drain the majority of the pelvic viscera
--External iliac nodes (which drain the anterior abdominal wall, urachus, bladder and part of internal genitalia) --Superficial and deep inguinal nodes (external genitalia and perineum) |
|
|
Why should the pelvic peritoneum be incised only medial to the ureter?
|
The pelvic ureter blood supply enters laterally.
|
|
|
What is the approximate bladder capacity of an adult when filled?
|
Approximately 500 mL.
|
|
|
What anchors the bladder to the anterior abdominal wall?
|
The urachus anchors the bladder to the abdominal wall. The urachus arises from the median umbilical fold and rarely is patent (which would cause a fistulous connection between the bladder and the umbilicus).
|
|
|
Why is it possible to perform a suprapubic cystostomy without risking entry into the peritoneal cavity?
|
With distension, the bladder rises out of the true pelvis and separates the peritoneum from the anterior abdominal wall.
|
|
|
What is Waldeyer’s sheath?
|
It is a fibromuscular sheath that extends longitudinally over the ureter and follows it to the trigone.
|
|
|
What is a Hutch Diverticulum?
|
Herniating bladder mucosa through the detrusor hiatus above the ureter, caused by outlet obstruction & causing reflux
|
|
|
What are the three layers of the trigone?
|
--Superficial layer (derived from longitudinal muscle of the ureter- extends to urethra to insert at verumontanum)
--Deep layer (continues from Waldeyer’s sheath and inserts at bladder neck) --Detrusor layer (formed by outer longitudinal and middle circular muscle layers of bladder wall) |
|
|
Where is the main blood supply of the bladder located?
|
ateral and posterior pedicles (lateral and posteromedial to the ureters, respectively)
|

