![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
62 Cards in this Set
- Front
- Back
|
The abdominal esophagus is the distal portion of the esophagus below the _______________
What is it innervated by? |
esophageal hiatus of the diaphram
anterior & posterior vagal trunks from the esophageal plexus of nerves |
|
|
What are the primary functions of the upper & lower esophageal sphincter?
|
upper- prevents entrance of air during respiration
(^located at pharyngoesophageal junction) lower- guards against gastroesophageal reflux (^located at esophageal hiatus of diaphram) |
|
|
Obj.
Describe the 3 esophageal constrictions |
1. cervical constriction
-upper esophageal sphincter 2. thoracic constriction -arch of aorta & left main bronchus 3. diaphragmatic constriction -lower esophageal spincter |
|
|
Clincially, esophageal constrictions are important for:
|
-passing an instrument through esophaus & into stomach
-interpreting radigraphs of patients w/ dysphagia -swallowed foreign objects -caustic fluids cause strictures |
|
|
Obj.
What does achalasia cause & why might it occur? |
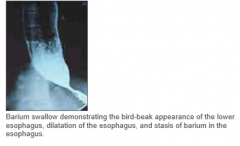
causes: failure of lower esophageal sphincter to relax, leading to dysphagia, regurgitation, chest pain & bird-beak appearance on radiograph
due to: absence of ganglion cells w/i wall of esophagus |
|
|
Obj
A hiatal hernia is a predisposing factor for longitudinal tears in the distal esophagus & gastroesophageal junction. What may this tearing lead to? |
Upper GI bleeding (10% of cases), presenting as hematemesis
|
|
|
What else may result in longitudinal tearing of the esophagus, known as Mallory-Weiss tears?
|
severe retching or vomiting due to acute alcohol intoxication
|
|
|
T/F
The stomach may vary in its position depending on patients posture and body type |
TRUE
|
|
|
What are the 4 main parts of the stomach?
|
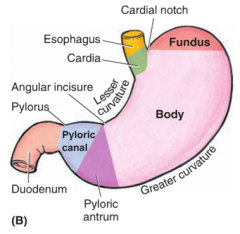
1. cardia
2. fundus 3. body 4. pyloric (subdivided into antrum & canal, whose junction is indicated by the angular incisure) *also note, lesser (facing liver) and greater (inferior/left) curvature |
|
|
The pyloric region has a thickened ring of circular smooth muscle , the ________________, which controls passage of chyme into the duodenum under ___________ nerve control
|
pyloric sphincter
vagus nerve (parasympathetic) control |
|
|
Obj
Congenital hypertrophic pyloric stenosis is marked by what symptom? |
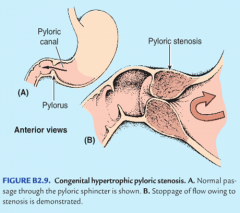
hypertrophy of the pyloric sphincter, inhibiting gastric emptying w/ non-bile stained, severe "projectile" vomiting, presenting as 4-8 wks in infants
(secondary dilatation of stomach) |
|
|
The _______ attaches the stomach from the lesser curvature to the liver.
The _______ attaches the greater curvature to the posterior body wall, spleen, & diaphragm & also migrates to wall off inflamation |
less omentum
greater omentum |
|
|
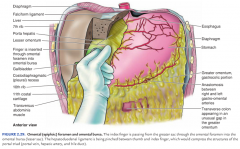
Of the 2 main types of hiatal hernias ________________ does NOT result in regurgitation of gastric contents (& is less common) & ____________ DOES and may lead to Barrett's esophagues
|
parasophageal hiatal hernia (does NOT)
sliding hiatal herna (DOES) |
|
|
Obj.
If medical treatment of gastric ulcers is unsuccessful _____________may be performed. In some instances this procedure must be accompanied by _________________ to allow gastric emptying (since sphincter cant relax) |
vagotomy= surgical section of the vagus nerve
drainage procedure (ie pyloroplasty) |
|
|
obj
Duodenal ulcers may cause fatal ________ from the ______________ artery. |
hemorrahage
gastroduodenal branch of the celiac artery *may result in peritonitis (superiorly) or pancreatitis (inferiorly) |
|
|
obj
Describe the development of gallstone ileus |
-an inflamed gallbladder may adhere to superior duodenum & pass gallstone into it through a cholecystenteric fistula
-a gallstone entering this way may obstruct the ileocecal valve, producing gallstone ileus |
|
|
Obj
What may hepatopancreatic ampulla obstruction be caused by? what may it lead to? |
-obstruction may be caused by gallstones becoming lodged or tumors forming w/i the narrow hepatopancreatic ampulla
-may lead to bile flow backing up into pancreatic duct causing bile pancreatitis/gallstone pancreatitis |
|
|
Obj
What is superior mesenteric artery syndrome? |
-The inferior 3rd of the duodenum passes btwn the superior mesenteric artery & aorta where it becomes compressed & completely obstructed
*surgical emergency |
|
|
Obj
Differentiate btwn characteristics of upper GI and lower GI bleeding |
Upper- typically produces vomiting of blood (hematemesis) and/or black tarry stool (melena)
Lower- bright red rectal bleeding (hematochezia) *ligament of Treitz is the junction point btwn upper & lower GI |
|
|
The ______________, where the small intestine transitions from retriperitoneal to intraperitoneal is a frequent site for peritoneal folds & _________
|
duodenojejunal junction
paraduodenal fossae (recesses) |
|
|
Obj
A loop of small intestine may become entrapped w/i a paraduodenal fossae as a _________________ & have to be surgically freed During surgery what artery & vein are at risk of damage? |
paraduodenal /internal hernia
inferior mesenteric artery & vein |
|
|
How are the jejunum & ileum distinguished by blood supply?
|

jejunum- has FEW arterial arcades & LONG vasa recta in mesentary w/ LITTLE fat
ileum- has MANY arterial arcades & SHORT vasa recta in mesentary laden (LOT) w/ fat |
|
|
How does the mucosa of the ileum & jejunum differ?
|
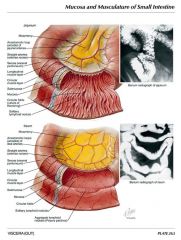
ilueum is smooth & jejunum has plicae circulares "feathery" appearance
|
|
|
obj
What is an ileal (Meckel's) diverticulum? |
it is a remnant of the embryonic vitelline duct (yolk stalk), contains all layers of intestinal wall= true diverticulum (may contain ectopic gastric or pancreatic tissue)
*most common congenital anomaly of small intestine |
|
|
An ileal diverticulum usually follows the rule of 2's, what is the rule of 2s?
|
rule of 2s:
-it occurs in 2% pop -is symptomatic in 2% of ppl w/ it -is symptomatic in first 2 yrs of life -is 2 in long -is located w/i 2 ft of ileocecal junction |
|
|
What may be caused be an ileal diverticulum?
|
-painless hemorrhage
-intestinal obstruction -inflammation (diverticulitis) -perforation -pain mimicking appendicitis -lower GI bleeding (hematochezia) ^ most common cause in children |
|
|
obj
What are appendicitis signs and symptoms? |
-vague central periumbilical pain that later becomes sharp, localized, right lower quadrant pain at McBurnery's point
-vomiting typically follows pain -positive obturator or psoas signs |
|
|
Differentiate btwn obturator & psoas sign
|
Obturator sign:
-pain on passive medial rotation of flexed R thigh = inflamed pelvic appendix -appendix in contact w/ fascia over obturator internus muscle Psoas (iliopsoas) sign: - pain against resisted flexion of R thigh (passive extension) =inflamed retrocecal appendix -appendix in contact w/ fascia over ilipsoas muscle |
|
|
Where is McBurney's point located?
|
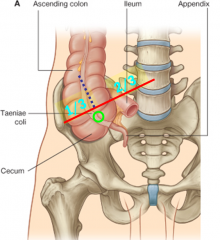
at a point 1/3 the distance on a line connecting the right ASIS & umbulicus
|
|
|
obj.
What is cecal volvulus? |
Twisting of the cecum on itself, causes obstruction & compromises blood supply (strangulation)
^predisposable due to mobile ascending colon |
|
|
obj.
Differentiate btwn the 2 major inflammatory bowel diseases; ulcerative colitis and Crohn’s disease |
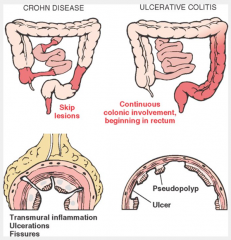
ulcerative colitis:
-begins in distal rectum & spreads into colon -does NOT involve small intestine -characterized by continuous inflammatory lesions involving mucosa & submucosa only Crohn's disease -involves terminal ileum & colon -characterized by inflammatory lesions of ALL layers of bowel wall (transmural lesions) -discontinuous "skip" lesions -causes malnutrition -intestinal obstruction & fistulas may occur *both cause abdominal pain, bloody diarrhea, fever & predispose to cancer |
|
|
Obj.
Sigmoid volvulus is made more likely by a (short/long) sigmoid mesocolon. What does sigmoid volvulus result in? |
long
-results in obstruction & infarction *90% of colon volvulus cases involve sigmoid colon |
|
|
obj.
Differentiate btwn diverticulosis and diverticulitis |
diverticulosis:
-sigmoid colon prone to develop outpocketings of it's own wall -often asymptomatic, can cause cramping, continuous low abdominal discomfort, bloating, constipation, diarrhea -present in 50% ppl over 60yr Diverticulitis: -infected/inflamed diverticula -may cause bleeding (intermittent or massive hemorrhage (rare), obstruction, or perforate -fistula may form btwn colon & adjacent organs |
|
|
If an infected diverticula perforates, what may result?
|
an absecess may form of infection may spread to produce generalized peritonitis
|
|
|
Obj.
What is Hirschsprung disease (congenital megacolon) and how does it present? |
-portion of colon is dilated (megacolon) due to failure of peristalsis resulting from absence of autonomic ganglic w/i intestinal wall, distal to dilated segment
-absent ganglia due to arrest in migration of embryonic neural crest cells -presents as denlargement & constipation in neonate *most common cause of neonatal obstruction of colon *10% of cases are in down syndrome children |
|
|
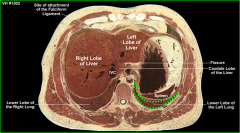
The liver occupies most of the right __________, upper __________ & extends into the left __________+
|
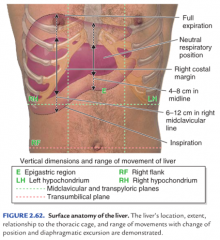
right hypochondrium
upper epigastrium left hypochondrium |
|
|
Important ligaments of the liver:
______ contains to ligamentum teres hepatis & paraumbilical veins ____________ outlines bare area of liver & is continuous & triangular ligaments __________ composed of hepatogastric & hepatoduodenal ligaments |
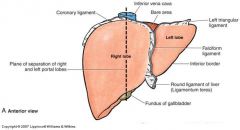
falciform ligament
coronary ligament lesser omentum *also note R & L triangular ligaments |
|
|
Important functions of the liver (5):
|
1. carb metabolism
2. protein metabolism (produces blood clotting factors) 3. lipid metabolism 4. bile production 5. detoxification |
|
|
obj
The livers attempts to detoxify may be overwhelmed in chronic alcoholism resulting in _____________ This condition may also result from what? |
cirrhosis (fibrosis of the liver)
-viral inflammation (hep B & C), obstruction of bile drainage, etc |
|
|
Unlike the rest of the body, in which venous drainage passes directly toward the sup or inf vena cava, venous drainage from the abdominal gastrointestinal system & spleen goes where?
|
enters the hepatic portal vein for transport to the liver
|
|
|
obj
What impairments to portal venous blood flow may result in portal hypertension? |
Impairments:
-prehepatic (portal vein thrombosis) -intrahepatic (cirrhosis) -posthepatic (R-sided heart failure or Budd Chiari syndrome |
|
|
What is Budd-Chiari syndrome?
|
hepatic vein thrombosis, prevents drainage of blood from liver into the inferior vena cava via hepatic veins
|
|
|
Obj
Portal hypertension complications and treatment |
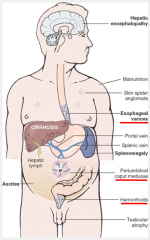
complications:
-esophageal varices (at gastroesophageal junction)--> fatal hemorrhage -caput medusae (subcutaneous veins radiate out from umbilicus, secondary to paraumbilical veins) -hemorrhoids (at anorectal junction) treatment: -portosystemic (portocaval) shunt btwn portal vein & inferior vena cava -splenorenal shunt btwn splenic vein & left renal vein |
|
|
Venous drainage of GI to liver also provides a pathway for what?
|
metastasis of cancer from GI into liver
|
|
|
The gallbladder recieves blood from cystic artery, which arises from the R hepatic artery within the cystohepatic triangle, what is this triangle formed by?
|
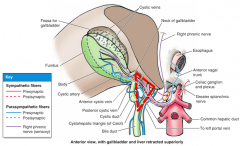
-common hepatic duct
-cystic duct -visceral surface of liver |
|
|
If the cystic artery or right hepatic artery is cut during cholecystectomy, how may a surgeon control bleeding?
|
Pringle maneuver-
surgeon may pass index finger through omental foramen & pinch hepoduodenal ligament btwn thumb & index finger |
|
|
Obj
Gallstones (cholelithiasis) may possibly cause what complications? |
if it obstructs bile flow, bile will be absorbed into blood, causing:
-yellowing of skin, sclera, & mucous membranes (jaundice icterus) |
|
|
If the gallbladder becomes inflamed (cholecystitis), pain may be referred from the diaphram to ____________ via the __________nerve
|
right shoulder
phrenic nerve |
|
|
________________, may develop at the junction of the neck of gallbladder & cystic duct when gallstones become impacted at the _____________
|
Hartman's pouch (an abnormal sacculation)
hepatopancreatic ampulla |
|
|
What is an endoscopic retrograde cholangiopancreatography (ERCP)?
|
-insertion of a cannula through the major duodenal papilla & hepatopancreatic ampulla for injection of radiographic contrast medium
|
|
|
Obj
Differentiate btwn acute and chronic pancreatitis |
acute pancreatitis:
-ranges from mild & self-limiting to life threatening -damage is REVERSIBLE -presents w/ abdominal, epigatsric pain radiating to back, nausea, vomiting, fever -commonly caused by alcoholism or gallstone bile flow obstruction chronic pancreatitis: -PERMANENT & progressive damage -diminished exocrine & encodrine function -may lead to chronic pain, weight-loss, diabetes mellitus, pancreatic cancer, pseudocyts -may result from recurrent acute pancreatitis, autoimmune disorders, toxins, obstructions of pancreatic ducts, idiopathic -genetic causes in children *25 yr mortality is 50% |
|
|
Pancreatitis frequently results in development of a ________________
|
pancreatic pseudocyst- an encapsulated (fibrous-walled) collection of pancreatic enzyme-rich fluid w/i pancreas
-most common location in in omental bursa (lesser sac) |
|
|
What are some of the possible complications of pancreatic pseudocysts?
|
-compression or perforation of adjacent structures
-hemorrhage -infection -peritonitis -pleural effusion |
|
|
Obj,
Pancreatic cancer (of pancreatic head) commonly leads to what? What is the first sign of this? |
obstruction of bile duct
painless jaundice is first sign, however overall pain is the most common symptom, usually severe pain radiating to mid or lower back* |
|
|
T/F
Spleen is part of the digestive system |
FALSE
-however does share blood supply w/ GI |
|
|
Where is the spleen located?
What are its functions? |
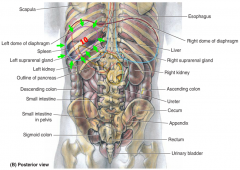
location:
-intraperitoneal -deep to L lower ribs 9-11 -long axis parallel to rib 10 function: -antibody formation -disposal of deteriorating RBCs & platelets -stores blood |
|
|
The spleen is supplied by the _________________
it is drained by __________________, which joins to superior mesenteric vein to form the ______________ |
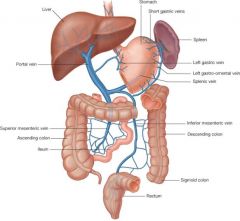
splenic artery (branch of celiac trunk)
splenic vein portal vein *the inferior mesenteric vein usually drains into the splenic veins |
|
|
Obj
Common splenic pathologies- |
-splenic artery may aneurysm during 3rd trimester
^rupture may cause fatal hemorrhage -splenomegaly from hypertension of hemolytic anemia |
|
|
The ________ is the most commonly ruptured abdominal organ w/ life threatening hemmorrhage
What are some common causes of rupture? |
spleen
causes: -blunt trauma to abdomen -lacerated in L lower rib fracture |
|
|
Splenectomy may be required to remove a ruptured spleen. What structure, that enters the splenorenal ligament may be injured during this procedure?
|
tail of the pancreas
*one or more accessory spleens may also be present |
|
|
During splenic needle biopsy, the relationship of the spleen to the costodiaphragmatic recess (which descends to 10th rib at midaxillary line) is important to remember, to avoid what?
|
entering the pleural cavity which would cause pleuritis
|
|
|
Splenic pain would be referred to the _________ via the ___________nerve
|
left shoulder
phrenic nerve |

