![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
61 Cards in this Set
- Front
- Back
|
What are the (4) basic tissue categories?
|
*Epithelial tissue
*Connective tissue -Supporting -Specialized *Muscle tissue *Nervous tissue |
|
|
What determines the properties of connective tissue?
|
The ECM
|
|
|
What are the two main components of connective tissue?
|
Cells
and ECM |
|
|
What are some roles of connective/supportive tissue?
|
They provide structure and strength.
They play a role in defense. They serve as a major storage depot. The ECM regulates cell function. |
|
|
In connective tissue, is there generally more ECM or cells?
|
ECM, lots more ECM
|
|
|
What are some of the major functions of connective tissue?
|
It provide architectural structure and tensile strength. Tissue-specific variation in ECM composition and organization allows the connective tissue to be structurally rigid (collagen-rich), resilient or elastic (elastin-rich).
It participates in defense. It acts as a structural barrier to infection or penetration, and contains host cells active in phagocytosis and immune response. It participates in organ maintenance. ECM components regulate cell proliferation and differentiation. Connective tissue serves as a major storage depot for a range of body resources, such as fat, minerals, water, electrolytes, protein and metabolites. |
|
|
Describe loose connective tissue:
|
This tissue (also called areolar connective tissue) serves as a cushioning layer throughout the body.
It is characterized by a loose, irregular networks of fibers and cells and abundant ground substance. It is not well preserved in routine histological preparation, resulting in an empty appearance in section. It is flexible and well vascularized, but has very little tensile strength. Examples include the papillary layer of dermis, the hypodermis and serosal linings of various epithelia and the investing tissues around blood vessels. |
|
|
Describe dense connective tissue:
|
This tissue has relatively abundant collagen fibers and less ground substance. It contains few cells, mostly fibroblasts. Compared to loose tissue, it is less flexible, with higher strength. It can be classified into regular and irregular.
Two types: Regular and Irregular |
|
|
Describe Regular dense connective tissue
|
Regular dense connective tissue has parallel unidirectional stress resistance or structure. It is found in specialized structures such as tendons.
|
|
|
Irregular dense connective tissue
|
Irregular dense connective tissue has a random network of large collagen fiber bundles, giving stress resistance in many directions. It is more widespread than regular dense connective tissue; typical example of irregular dense connective tissue are dermis and organ capsules.
|
|
|
Describe adipose tissue:
|
Adipose tissue
Some areas of loose connective tissue have a high content of unilocular adipocytes (white fat). Multilocular adipocytes are typically found in a well vascularized lobular tissue (brown fat). |
|
|
Describe elastic tissue:
|
Elastic tissue is rich in parallel bundles of elastic fibers called elastin. It is found in specialized sites such as the yellow ligaments of vertebral column, vocal chords, and artery walls.
|
|
|
Describe reticular connective tissue:
|
Reticular tissue provides a delicate structural framework for several organs (e.g. bone marrow, lymph nodes, spleen). Macrophages are often anchored to this framework. It consists of a branching network of type III collagen fibers.
|
|
|
What are the resident cells of connective tissue?
|
Fibroblasts
Adipocytes Macrophages Mast Cells Wandering Cells |
|
|
What are fibroblasts?
|
Fibroblasts are the most abundant connective tissue cell type; they are stellate or elongated in shape with an elongated nucleus. Fibroblasts are the most active in synthesis, secretion and turnover of ECM components, particularly collagens.
|
|
|
What are adipocytes?
|
Adipocytes (fat cells) are large spherical cells, distended by non-membrane bound lipid. The eccentric nucleus is flattened, giving a "signet ring" appearance in sections. Adipocytes are long-lived, but do not proliferate.
|
|
|
What are unilocular adipocytes?
|
Unilocular adipocytes have single, central lipid droplet, chiefly triglycerides.
|
|
|
What are multilocular adipocytes?
|
Multilocular adipocytes ('brown fat') store fat as lipid droplets of various sizes. They have a central nucleus and numerous mitochondria. These cells function in heat generation by inefficient consumption of ATP. In humans they are primarily seen in infants.
|
|
|
What are macrophages derived from?
|
Blood monocytes
|
|
|
Describe macrophages:
|
They reside for months in connective tissue.
Macrophages are large (10-30 mm in diameter), irregularly shaped and with many lysosomes. Macrophages have an important role in defense: *They ingest and degrade foreign matter, microorganisms and damaged cells *They kill microorganisms and tumor cells by reactive oxygen and reactive nitrogen metabolites *They stimulate immune response, display digested foreign protein fragments on their surface (immune presentation), which can trigger specific lymphocytes to produce antibodies. *They efficiently ingest antibody-coated (opsonized) material. *They secrete lytic enzymes, cytokines, prostaglandins, cytokines, complement proteins, growth factors, etc. |
|
|
Describe Mast Cells:
|
Mast cells are similar to blood basophils and participate in immune responses.
These cells are round, 20-30 mm in diameter and include abundant, large, metachromatic granules that contain histamine, heparin, serotonin and other mediators of inflammation (e.g., chemotactic factors, proteases and cytokines). When surface receptors for IgE antibodies on mast cells bind antigen, granule release is triggered initiating the immediate hypersensitivity reaction. Mast cells are typically located near blood vessels, which respond rapidly to the released substances (vasodilatation). Histamine also causes bronchoconstriction (due to smooth muscle contraction in the airways). Mast cells originate in the bone marrow and circulate to connective tissue, where they reside for weeks to months |
|
|
What are wandering cells?
|
These include all blood leukocytes, some of which reside in connective tissue for their entire functional life span. Cells enter tissue from the blood by squeezing between endothelial cells of capillaries or venules by a process called "diapedesis".
|
|
|
How do wandering cells get out of the blood stream?
|
Diapedesis
|
|
|
What are the (3) fundamental types of ECM?
|
Basement membrane/basal lamina
Interstitial ECM Provisional ECM |
|
|
Describe basement membrane/basal lamina:
|
Flexible thin sheets of specialized ECM proteins that underlie all epithelial cell sheets and also surround muscle cells, fat cells and Schwann cells.
|
|
|
Describe interstitial ECM:
|
ECM fibers in a hydrated polysaccharide gel with cells distributed in it. In connective tissues such as bone, cartilage, and dermis, this ECM is relatively plentiful and cells are sparse. In other tissues (e.g., liver, kidney) interstitial ECM is present but is less abundant.
|
|
|
Describe provisional ECM:
|
Formed from fibrin and other plasma proteins during blood clotting.
|
|
|
What are the main structural proteins of ECM?
|
The major components of ECM are long polymers of structural proteins such as collagen and elastin, and proteoglycans (proteins containing long charged polysaccharide chains). ECM also includes a large number of proteins that regulate cell adhesion, migration, proliferation and differentiation.
|
|
|
What are the most abundant proteins in mammals?
|
Collagens
|
|
|
What is the most abundant collagen and where is it located?
|
Collagen type I is the most abundant.
Located: dermis, tendon, ligaments and cornea (most connective tissue) |
|
|
Describe Type I Collagen:
|
fibers are relatively thick and arranged in large bundles to form flexible, inelastic fibers of high tensile strength.
|
|
|
Describe Type II Collagen:
|
hyaline cartilage the fibers are much finer
|
|
|
Describe Type III Collagen:
|
Reticular fibers are composed mostly of collagen type III (originally called reticulin).
They are thinner than type I collagen fibers, form delicate networks rather than bundles, Have a particular affinity for silver stains. |
|
|
Describe Type IV Collagen:
|
Non-fibrillar
Found in basement membrane |
|
|
Describe Type VII Collagen:
|
Found in basement membrane
|
|
|
What type of collagen is hyaline cartilage composed of?
|
Type II
|
|
|
What is the biological pathway of creating collagen?
|
Collagen monomers are synthesized with an extension peptide, and these are called called a pro-alpha chain. When the extension peptides are removed, multimeric collagen fibrils and fibers can form.
Collagen has two unusual amino acids, hydroxyproline and hydroxylysine, formed post-translationally, which are important for collagen stability. Hydroxyproline is generated from proline by two different hydroxylating enzymes that require Fe++, oxygen, alpha-ketoglutarate and ascorbic acid (vitamin C). Hydroxylation reactions precede trimer formation. Collagen pro-alpha chains self-assemble into a procollagen triple helix, and are then secreted from the cell. The extension peptides are cleaved, marking the transition from procollagen to tropocollagen. To form a collagen fibril, tropocollagen molecules bind to another, with a displacement that allows a small gap before the next tropocollagen molecule is added. This gives rise to a characteristic banded pattern seen in the microscope. To obtain a fibril with high tensile strength, the collagen trimers are tightly linked by covalent bonds between lysines, between hydroxylysines or between both. |
|
|
Describe elastin:
|
Elastic fibers are composed primarily of the protein elastin, and form an irregular thin fiber network. Assembly of elastin into fibers from its soluble precursor tropoelastin requires the microfibrills of fibrillin, which are incorporated in and around the fibers. Elastin fibers are abundant in tissues such as elastic cartilage, lung or skin and give these tissues elasticity and a characteristic yellow color. In the unstretched state, elastin is coiled up. When the protein stretches, cross bridging between chains hold the individual polypeptide chains in the structure together.
|
|
|
Is hyaluronic acid sulfanated?
|
No
|
|
|
What are GAGs?
|
Glycosaminoglycans
|
|
|
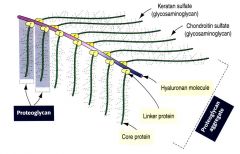
Glycosaminoglycans:
|
GAGs
polysaccharides: they are long, highly negatively charged, unbranched carbohydrate chains made up of a repeating disaccharide. One of the pair of the disaccharide is an acidic sugar (a uronic acid) and the other is an aminosugar (N-acetyl glucosamine or galactosamine). The key feature of GAGs is that their highly charged structure forces them to be remarkably extended, very hydrated molecules that fill extracellular space. One type of GAG, hyaluronic acid, exists as a free polysaccharide with no attached protein. |
|
|
What is the key feature of GAGs?
|
The key feature of GAGs is that their highly charged structure forces them to be remarkably extended, very hydrated molecules that fill extracellular space.
|
|
|
What are proteoglycans?
|
Proteoglycans are a type of glycoprotein in which long GAG chains are attached post-translationally to a polypeptide backbone (core protein).
The GAG side chains are added to serine or threonine residues in the core protein. There are four major types of GAG chains in proteoglycans: chondroitin sulfate, heparan sulfate/heparan, keratan sulfate and dermatan sulfate. Hyaluronic acid is not sulfated. |
|
|
What are the (4) major types of GAG chains in proteoglycans?
|
chondroitin sulfate
heparan sulfate/heparan keratan sulfate dermatan sulfate Hyaluronic acid is not sulfated. |
|
|
What are (2) examples of major cell adhesion proteins?
|
fibronectin and laminin
Cell adhesion proteins are secreted ECM proteins that attach cells to the rest of the matrix. Since these linkages are dynamic, they serve major regulatory roles in tissue physiology, development and healing. |
|
|
Describe fibronectins:
|
Fibronectins are a family of closely related glycoproteins that form fibrillar arrays on the cell surface and in ECM, but one form is found soluble in plasma and is important for wound healing. Many integrins (cell surface proteins) recognize specific amino acid sequences in fibronectin. Fibronectin has roles in cell migration, wound healing, and cell differentiation.
|
|
|
Describe laminin:
|
Laminin is a cross-shaped heterotrimer in the basement membrane. Major functions of laminin include promotion of cell adhesion, migration, proliferation, and differentiation. Whereas fibronectin binds to a range of collagen types, laminin binds specifically to collagen IV. Cell surface receptors for laminin include certain members of the integrin family, as well as other non-integrin receptors.
|
|
|
Describe integrins:
|
Integrins are receptor molecules on the cell surface that bind and respond to ECM components. Some integrins combinations recognize multiple matrix components, while others recognize only fibronectin or only laminin. Integrins also connect the ECM to cytoskeleton. Intracellularly, the cytoplasmic tail of integrin binds to talin, vinculin, and alpha-actinin, which in turn bind to actin filaments. Attachment of cells to the ECM occurs at specialized membrane structures called focal adhesions and hemidesmosomes.
The regulation of integrin activity allows cells to attach or detach from the ECM. For example, in epidermis, the adhesion of the keratinocyte basal cells to their underlying basement membrane must be inactivated so that these cells can detach from the epidemis. Blood cells have some integrins that have to be activated before they can mediate adhesion. This regulation allows these cells to circulate in the blood stream unimpeded until they encounter a specific stimulus such as a site of infection or a damaged blood vessel. |
|
|
What is osteogenesis imperfecta?
|
Genetic defect in collagen type I
|
|
|
What are Chondrodystrophies?
|
Defects in cartilage due to changes in collagen type II
|
|
|
Describe Ehlers-Danlos syndroms:
|
affect a variety of collagens, like collagen type III which is made by muscle cells. The make up of the wall of the aorta can be come weakened, causing a dissecting aneurism
|
|
|
What embryonic tissue is the basis for and all connective tissue is derived from it?
|
mesenchymal tissue
|
|
|
What type of cells could a mesenchymal cell differentiate into?
|
Osteoblast
Chondroblast Fibroblast |
|
|
Where is reticular tissue found?
|
In delicate areas.
bone marrow lymph nodes spleen |
|
|
What is often found within reticular tissue?
|
Macrophages
|
|
|
Is adipose tissue vascular and why?
|
Yes it is vascular to allow for the depositing and removing of fatty acids and delivering those around the body.
|
|
|
Where do monocyte cells originate?
|
In bone marrow to later become macrophages or osteoclasts
|
|
|
How do mitochondria move about the body?
|
Via pseudopodia
|
|
|
What protein is the chief component in elastic fibers?
|
elastin
|
|
|
What is elastin composed of?
|
Assembly of elastin into fibers from its soluble precursor tropoelastin requires the microfibrills of fibrillin, which are incorporated in and around the fibers.
|
|
Name
|
Orthodontists get 98s, Surgeons get 99s
|

