![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
190 Cards in this Set
- Front
- Back
|
What is pain?
|
The conscious experience of an unpleasant sensory or emotional experience associated with actual or potential tissue damage.
|
|
|
What is nociception?
|
the process of neurotransmission, originating from sensory receptors (nociceptors) which transmits and processes information related to tissue damage.
|
|
|
What is hyperalgesia?
|
an exaggerated response to a noxious stimulus.
|
|
|
What is allodynia?
|
a pain response to a non-noxious stimulus (such as a gentle touch.)
|
|
|
What is peripheral sensitisation?
|
sensitization of C & A nociceptors, predominantly induced by inflammatory mediators released by tissue damage such that their response threshold is lowered and/or they produce a greater response to the same stimulus.
|
|
|
What is central sensitisation?
|
The enhanced excitability of spinal nociceptive neurons to result in a hypersensitive and hyperactive nociceptive transmission system. Can be short lived, associated with transient changes in neurotransmitter activity, or long-lived, associated with phenotypic changes in these central neurons.
|
|
|
What is analgesia?
|
The absence of pain sensation.
|
|
|
What is distress?
|
Physical and emotional / mental strain or stress.
|
|
|
What is somatic pain?
|
Somatic pain is easily localized and so often described as acute, aching, stabbing or throbbing. Somatic pain includes cutaneous pain after an operation. Somatic pain can be further classified as superficial (skin) or deep (joints, muscle, or periosteum) in origin.
|
|
|
What is peripheral pain?
|
Either visceral (thoracic/abdominal) or somatic (joints, muscles, or periosteum.) Visceral pain is poorly localized and frequently described as cramping or gnawing. May be also reffered pain to cutaneous sites far from site of injury.
|
|
|
What is neuropathic pain?
|
The result of trauma, inflammation, or sensitization of peripheral nerves or spinal cord. Neuropathic pain is described as burning, lacerating, and intermittent, and is often poorly responsive to treatment.
|
|
|
What is idiopathic pain?
|
Persistent pain in the absence of an identifiable organic substrate. Idiopathic pain is often excessive and associated with emotional stress or behavioral abnormalities.
|
|
|
What are the physiological signs of pain?
|
Inc blood pressure, inc heart rate, inc peripheral vasoconstriction - identifiable by pale mucus membranes, inc respiratory rate, possible muscle splinting, inc catabolic processing, dec food / water intake, dec voiding
|
|
|
What is multimodal analgesia?
|
The simultaneous administration of a combination of analgesic agents (opiods, NSAIDs, and alpha2-agonists) with different modes of action and different side effects which may act synergistically and achieve optimal analgesia with less risk/side effects than large doses of a single drug.
|
|
|
What is pre-emptive analgesia?
|
Administration of an analgesic agent prior to noxious stimulation.
|
|
|
How do anaesthetics affect fluid deficits?
|
"Decompensate" - ie, incapacitate compensatory mechanisms, depress cardiac output, derange blood-gases, exacerbate pH changes, impair renal function, increase respiratory water losses (low FiH2O); also, surgery imposed H2O deprivation, 3rd space losses, gross haemorrhage, evaporation from wound, blood sequestration in tissues then removed (ex spay), urinary losses.
|
|
|
Define the term: hypotonic.
|
Water lost in excess of electrolytes (pure water).
|
|
|
What are the clinical signs of hypotonic /free water loss? How can they be corrected?
|
Skin tenting, tachycardia, hypotension
|
|
|
Succinylcholine
1. Type of agent 2. Mechanism of action 3. Indications 4. Speed of onset and clearance 5. Side effects 6. Contraindications |
1. a depolarizing paralytic anesthetic.
2. Binds to muscarinic (organs) and nicotinic (muscles) receptors, causing depolarization of muscles (fasciculations) and blocks ACh. 3.RSI, Converting from a laryngeal mask to ETT, short procedure, Risk of aspiration, laryngospasm. 4. Onset = 30 sec. Duration 5-10min. 5.Malignant hyperthermia. Plasma Cholinesterase deficiency = paralysis upon waking. Hyperkalemia. Muscarinic = Bradycardia, dysrythmia, sinus arrest. Increased ICP, IOP and Gastric pressure. Fasciculations and post-op myalgia 6. History of MH, PCD. Hyperkalemia, Allergy. myotonia. Caution in eye injury, myasthenia gravis. |
|
|
What type of paralytic is succinylcholine? How does it work?
|
A depolarizing paralytic. It binds to the nicotinic receptor, causes prolonged muscle depolarization and fasciculations then paralyzes the muscle. Then it remains in the receptor and is slowly degraded. Not degraded by acetylcholinesterase.
|
|
|
Propofol
1. type of drug 2. Mechanism of action (2) 2. uses (3) 3. Side effects (6) |
1. A sedative hypnotic and amnesic with muscle relaxant properties. It is not an analgesic and thus fentanyl is also used. It's the white drug.
2. Potentiates GABA and blocks sodium channels. 3. Used for Rapid Sequence Induction RSI, procedural sedation and as a general anaesthetic. SIDE EFFECTS 1. Increased ICP, 2. increased IOP, 3. decreased RR, 4. decreased BP, 5. decreased HR 6. Apnea |
|
|
Midazolam
1. Mechanism of action 2. Uses 3. Side effects 4. Reversal |
1. Benzo that potentiates GABA, decreasing CNS neuron activity. Sedative, hypnotic, anxiolytic and amnesic properties.
2. Ultra-short acting benzo - used for procedural sedation, prior to induction 3. Confusion, somnolence, bradycardia, hypotension 4. Overdose reversed by flumazenil. |
|
|
How is benzodiazepine overdose treated?
|
Flumazenil
|
|
|
Morphine
1. Mechanism of action 2. Uses 3. Side effects intraoperatively 4. Reversal of overdose |
1. binding to and activating the μ-opioid receptors in the central nervous system. Endogenous opioids include endorphins, enkephalins, dynorphins also bind to the μ-opioid receptor.
2. Analgesic with long acting properties compared with fentanyl which is quite short. 3. Hypotension & bradycardia. Also causes nausea and constipation. 4. Intraoperatively use phenylephrine (norepinephrine) to increase BP. In overdose use Narcan (Naloxone) but watch for rebound pain. |
|
|
Rocuronium
1. Mechanism of action 2. Uses 3. Length of activity 3. Side effects 4. Reversal |
1. Non-depolarizing muscle relaxant. Competitively antagonizes acetylcholine nicotinic receptors and prevents muscular contraction. Does not cause fasciculations like succinylcholine.
2. Used as a paralytic and muscle relaxant for intubation and mechanical ventilation and to prevent laryngospasm. 3. Takes effect in 1-2 minutes (2-3 x longer than succ), but can use higher dose for RSI. Lasts longer - 20-30 minutes. 4. No risk of Malignant hyperthermia. Prolonged Apnea and paralysis without reversal. 5. Reversed with a Neostigmine and Glycopyrrolate cocktail. |
|
|
Sevoflurane
1. Mechanism of action 2. Use 3. Side effects 4. Reversal |
1. An ether which is a sedative, hypnotic and amnesic with mild muscle relaxant properties.
2. Used as an inhaled volatile anesthetic for the induction and maintenance of general anesthesia. 3. Rare cause of malignant hyperthermia. Apnea. 4. Reversed with high flow O2 to wash out lungs. |
|
|
Phenylephrine
1. Mechanism of action 2. Use 3. Side effects |
1. A vasopressor which is a pure alpha agonist. A weak form of norepinephrine. Causes constriction of blood vessels to increase preload without affecting HR or contractility.
2. Used to increase BP. Increase preload and afterload. 3. Compensatory decrease in heart rate. Due to the increased preload and BP, heart slows down. |
|
|
Ephedrine
1. Mechanism of action 2. Use 3. Side effects |
1. Ephedrine is a sympathomimetic amine & weak form of epinephrine. Vasopressor and inotrope. Acts on alpha and beta receptors. Causes blood vessel constriction (alpha = preload and afterload) and increased cardiac heart rate and contractility (beta).
2. Used to counteract blood loss and morphine induced hypotension and bradycardia. 3. Hypertension, arrythmias, confusion and agitation, sweating. |
|
|
Neostigmine and Physostigmine
1. Mechanism of action 2. Uses |
1. a parasympathomimetic, specifically, a reversible cholinesterase inhibitor. By interfering with the breakdown of acetylcholine, neostigmine indirectly stimulates both nicotinic and muscarinic receptors. Unlike physostigmine, neostigmine has a quarternary nitrogen; hence, it is more polar and does not enter the CNS. its effect on skeletal muscle is greater than that of physostigmine, and it can stimulate contractility before it paralyzes.
2. improve muscle tone in people with myasthenia gravis and routinely, in anesthesia at the end of an operation, to reverse the effects of non-depolarizing muscle relaxants such as rocuronium and vecuronium when preparing to extubate. Used in combo with glycopyrrolate. |
|
|
Glycopyrrolate
1. Mechanism of action 2. Uses |
1. Muscarinic anticholinergic with no central effects
2. used as a preoperative medication to reduce salivary, tracheobronchial, and pharyngeal secretions, as well as decreasing the acidity of gastric secretion. It is also used in conjunction with neostigmine, a neuromuscular blocking reversal agent, to prevent neostigmine's muscarinic effects such as bradycardia. |
|
|
Odansatron / Granisetron
1. Mechanism of action 2. Uses 3. Dose |
Granisetron is a serotonin 5-HT3 receptor antagonist that acts at the nausea and vomiting centre via antagonizing vagus nerve receptors in the medulla oblongata..
2. Antiemetic a. Chemotherapy b. Anaesthetic induced Post-op nausea and vomiting prophylaxis. c. Bowel surgery and radiation releases 5HT3 and it is effective. 3. 1mg IV q8h. Best given intraoperatively 1mg po bid. |
|
|
Metochlopramide (Maxaran)
1. Mechanism of action 2. Uses |
1. Dopamine antagonist. Powerful antiemetic and gastric motility agent.
2. Used for post op nausea, chemo induced nausea and after bowel surgery to promote gut motility. Also used in combo with Ketorolac (Toradol) for migraine headaches. |
|
|
Ketorolac (Toradol)
1. Mechanism of action 2. Uses 3. Contraindications |
1. Potent NSAID - can only use for a max of 5 days. Anti-inflammatory, anti-pyretic, analgesic. competitive blocking of the enzyme cyclooxygenase (COX). Like most NSAIDs, ketorolac is a non-selective COX inhibitor.
2. Migraine headaches. Post operative pain. 3. NSAID and ASA allergy. Renal disease (constricts afferent arteriole). |
|
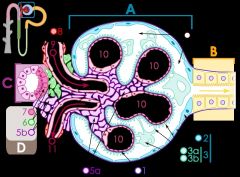
Name the structures.
|
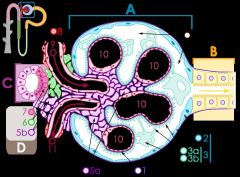
Diagram of renal corpuscle structure:
A – Renal corpuscle B – Proximal tubule C – Distal convoluted tubule D – Juxtaglomerular apparatus 1. Basement membrane (Basal lamina) 2. Bowman's capsule – parietal layer 3. Bowman's capsule – visceral layer 3a. Pedicels (podocytes) 3b. Podocyte 4. Bowman's space (urinary space) 5a. Mesangium – Intraglomerular cell 5b. Mesangium – Extraglomerular cell 6. Granular cells (Juxtaglomerular cells) 7. Macula densa 8. Myocytes (smooth muscle) 9. Afferent arteriole 10. Glomerulus Capillaries 11. Efferent arteriole |
|
|
Prochlorperazine (Stemetil)
|
Prochlorperazine (marketed under the names Compazine, Stemzine, Buccastem, Stemetil and Phenotil) is a drug that belongs to the phenothiazine class of antipsychotic agents that are used for the treatment of nausea and vertigo. It is also a highly-potent typical antipsychotic, 10 to 20 times more potent than chlorpromazine.
|
|
|
Droperidol
1. Action and use 2. Side effects |
1. antidopaminergic drug used as an antiemetic and antipsychotic.
2. QT prolongation and torsades de pointes. The evidence for this is disputed, with 9 reported cases of torsades in 30 years and all of those having received doses in excess of 5 mg.[3] QT prolongation is a dose-related effect,[4] and it appears that droperidol is not a significant risk in low doses. |
|
|
Diphenhydramine (Benadryl)
1. Mechanism of action 2. Systemic effects - 2 3. Uses - 3 |
1. A - Blocks histamine at H1 receptor sites.
2 A - increase of vascular smooth muscle contraction, thus reducing the redness, hyperthermia and edema that occurs during an inflammatory reaction. B - Blocking the H1 receptor on peripheral nociceptors also decreases sensitization and reduces itching. 3. A - Antiemetic, nausea and vomiting. B - Antihistamine for allergic reactions. C - extrapyramidal side effects of typical antipsychotics, such as the tremors that haloperidol can cause. |
|
|
Hydromorphone (Dilaudid)
1. Mechanism of action 2. Uses 3. Side effects 4. Reversal |
1. u-opioid receptor agonist. 5-10 times stronger than morphine. Where morphine is given in doses of 5-10mg post-op, hydromorphone is given in doses of 0.5-2mg.
2. Faster acting than morphine, good for PCA over several days. Also produces fewer active metabolites, thus less side effects. 3. Fewer side effects than morphine. Resp depression, hypotension, Nausea, vomiting, constipation, sedation, dependece, itching, redness. 4. Reversed with naloxone (narcan) |
|
|
Fentanyl
1. Mechanism of action 2. Uses 3. Side effects 4. Dose |
1. synthetic primary μ-opioid agonist. 100 times more potent than morphine.
2. administered in combination with a benzodiazepine, such as midazolam, for procedural sedation, anesthesia and analgesia. 3. Resp depression, hypotension, nausea, vomiting, itching, redness. 4. Dose - 3-10 ug/kg |
|
|
Define anesthesia.
|
Lack of awareness or sensation. Can be a spectrum from local anaesthesia, conscious sedation with analgesia to general anesthesia.
|
|
|
Atropine
1. Mechanism of action 2. Uses 3. Side effects |
1. Anticholinergic - Competitive antagonist for the muscarinic acetylcholine receptor.
Lowers parasympathetic activity 2 - a. Cycloplegic / Mydriatic b. Bradycardia, asystole and pulseless electrical activity (PEA) - usual dosage = 0.5 to 1 mg IV push every three to five minutes 3. Ventricular fibrillation, supraventricular or ventricular tachycardia, dizziness, nausea, blurred vision, loss of balance, dilated pupils, photophobia, and, possibly, notably in the elderly confusion and delerium. |
|
|
1. Signs of atropine overdose.
2. Antidote |
1. Ventricular fibrillation, supraventricular or ventricular tachycardia, dizziness, nausea, blurred vision, loss of balance, dilated pupils, photophobia, and, possibly, notably in the elderly, extreme confusion, extreme dissociative hallucinations, and excitation
2. The antidote to atropine is physostigmine or pilocarpine. |
|
|
Preload
1. Define 2. Ways that you can increase preload in anaesthesia 3. Ways you can decrease preload |
1. the pressure stretching the left ventricle after atrial contraction and passive filling. May also be called end-diastolic volume.
2. INcreased with epinephrine- ephedrine (a + B agonist) and norepi - phenylephrine (a agonist). Increased blood volume. 3. Decreased with PEEP (increased intrathoracic pressure) + anaesthetics (relax vessels). |
|
|
Afterload
1. Define 2. Ways that you can increase afterload in anaesthesia 3. Ways you can decrease afterload. |
1. the tension produced by the left ventricle in order to contract. against systemic resistance.
2. Epinephrine and ephedrine increase preload and afterload (+ rate + contractility). Phenylephrine increase preload and afterload. Trendelenberg position (drop head) increases afterload. 3. Decrease with Nitroglycerine, Nitrates, CCB, Beta-blockers. |
|
|
What drugs can be used to alter heart contractility?
|
1. Increase - ephedrine and epinephrine. Dopamine, dobutamine, calcium, digoxin
2. Decrease - CCB |
|
|
What drugs can be used to alter heart rhythm?
|
1. CCB
2. Digoxin |
|
|
How do calcium channel blockers work?
|
Calcium channel blockers work by blocking voltage-gated calcium channels (VGCCs) in cardiac muscle and blood vessels. This decreases intracellular calcium leading to a reduction in muscle contraction. In the heart, a decrease in calcium available for each beat results in a decrease in cardiac contractility. In blood vessels, a decrease in calcium results in less contraction of the vascular smooth muscle and therefore an increase in arterial diameter (CCB's do not work on venous smooth muscle), a phenomenon called vasodilation. Vasodilation decreases total peripheral resistance, while a decrease in cardiac contractility decreases cardiac output. Since blood pressure is determined by cardiac output and peripheral resistance, blood pressure drops.
|
|
|
Digoxin:
Describe the two ways it acts on the heart. |
1. A decrease of conduction of electrical impulses through the AV node, making it a commonly used antiarrhythmic agent in controlling the heart rate during atrial fibrillation or atrial flutter.
2. An increase of force of contraction via inhibition of the Na+/K+ ATPase pump. This results in increased Ca+ in the sarcoplasmic reticulum. Thus less frequent and more powerful contractions. |
|
|
What factors do you want to consider on an anaesthetic history?
|
1. Difficult intubation + why
2. Neck or Oralaryngeal trauma 3. Medications and drugs 4. Smoking 5. Post-op nausea and vomiting and history of motion sickness 6. Allergies to meds and anaesthetics 7. Personal/Family history of Malignant hyperthermia and Plasma Cholinesteras Deficiency 8. Poor response to codeine - they also won't respond well to Ketorolac (Tramadol) |
|
|
What other drug will not work well for a patient with a history of poor response to codeine?
|
Ketorolac (Tramadol)
|
|
|
What are the 2 most common reasons for delayed discharge after surgery?
|
1. Post-op nausea and vomiting
2. Pain |
|
|
How common is post-op nausea and vomiting?
|
About 25% of pts.
|
|
|
Which factors predispose to post-op nausea and vomiting?
|
Prototype - young female non-smoker with history of motion sickness who gets opioids intraopertively.
1. Female 2. Non-smoker 3. History of PONV or motion sickness 4. Opioids 5. Prolonged surgery |
|
|
When should you consider prophylaxis for nausea & vomiting (PONV)?
How? |
When there are 2 or more risk factors.
1. Female 2. Non-smoker 3. History of PONV, motion sickness 4. Opioids during surgery? Prophylaxis = Odansitron / Granisetron (5HT3 antagonist), dimenhydramine, droperidol |
|
|
What intraopertive drugs can increase the risk of Post-op Nausea Vomiting?
|
Nitrous oxide, inhaled anaesthetics (sevoflurane etc.), opioids, neostigmine
|
|
|
What is a 5HT3 antagonist?
Use? Examples? |
1. Antagonize a the 5HT3 subtype of serotonin receptor found in terminals of the vagus nerve which stimulates the nausea and vomiting center in medulla oblongata.
2. Used to control chemo induced N+V and PONV. 3. Odansetron and Granisetron |
|
|
List 5 side effects that may occur with the intravenous administration of 1 mg/kg of succinylcholine. (Do not include malignant hyperthermia trigger)
|
Hyperkalemia
Sustained contraction in myotonia Cholingergic: Sinus bradycardia, increased secretions Fasciculations, myalgia Increased IOP, ICP, intragastric pressure |
|
|
What 2 structures obstruct the airway in an unconscious patient who is supine.
|
Tongue, epiglottis
|
|
|
With just your hands, how should you open the airway in an unconscious patient who
i) has a suspected C-spine injury ii) has no suspected C-spine injury. |
1. Jaw thrust
2. Sniffing position - Head tilt & Chin lift |
|
|
List 2 devices that can be placed blindly that can assist you in opening the airway.
|
Nasopharyngeal airway, oropharangeal airway
|
|
|
What concentration of oxygen should be given to all patients who present with apnea?
|
100%
|
|
|
What piece of oxygen therapy equipment will you use to deliver this concentration of oxygen to all patients who present with apnea?
|
Ambu bag and mask with 100% O2
|
|
|
Where can this piece of equipment be found on most nursing wards?
|
crash cart, on the wall
|
|
|
List 5 usual steps taken in examining a patient’s airway to determine the ease of intubating conditions for oral intubation, and note for each what constitutes a normal or abnormal finding:
|
1. TMJ mobility: condyle should be able to move 1 cm anteriorly
2. mouth opening: > 2 fingers 3. thrymental distance: > 6.5 cm 4. cervical spine mobility: flexion and extension without discomfort 5. Mallampati = visability of hypopharyngeal structures: full view of uvula, tonsillar pillars, tonsils, posterior pharyngeal wall, soft palare and tongue |
|
|
A 65-year old man presents to your family practice office for a preoperative assessment before a proposed ventral hernia repair. He is a known hypertensive and has been treated with Metoprolol 50 mg bid and Hydrochlorothiazide 50 mg a day. His blood pressure today is 180/110 mm Hg.
A. What are 4 specific questions you would ask him on history related to his hypertension? (4) |
Duration
Usual BP Hx of MI, Stroke, kidney damage |
|
|
A 65-year old man presents to your family practice office for a preoperative assessment before a proposed ventral hernia repair. He is a known hypertensive and has been treated with Metoprolol 50 mg bid and Hydrochlorothiazide 50 mg a day. His blood pressure today is 180/110 mm Hg.
B. What 3 physical findings are crucial to determine with regards to his cardiovascular "fitness" for elective surgery? |
S4, retinal changes, renal bruit
|
|
|
A 65-year old man presents to your family practice office for a preoperative assessment before a proposed ventral hernia repair. He is a known hypertensive and has been treated with Metoprolol 50 mg bid and Hydrochlorothiazide 50 mg a day. His blood pressure today is 180/110 mm Hg.
What 3 investigations are strongly indicated in this patient related to the information given? (3) |
Echo, ekg, creatinine
|
|
|
You are seeing a 32 year old woman in the holding area outside the operating room immediately prior to her scheduled laparoscopic cholecystectomy. She tells you that she has had a ‘cold’ for 2 days.
What 5 items elucidated on either history, physical examination or laboratory data would cause you to postpone this elective procedure? |
Increased WBC
Adventitious lung sounds Absent breath sounds/dullness Fever New productive cough |
|
|
A 44 year old morbidly obese (200 kg) man presents for an emergency appendectomy.
List 5 important problems associated with morbid obesity that puts these patients at an increased risk for anaesthesia and surgery. (10) |
Aspiration
Possible difficult intubation Decreased FRC – reduced lung space to preoxygenate means less time to intubate before patient desturates Difficult bag mask ventilation Increased positive pressures required for ventilation |
|
|
A 75-year-old man presents for a total hip replacement. He is given a general anaesthetic. The drugs used for induction are sodium thiopental 250 mg, fentanyl 250 micrograms and succinylcholine 100 mg. Anaesthesia is maintained with isoflurane 0.2-0.8%, nitrous oxide 60%, rocuronium increments and morphine increments.
His usual blood pressure is 150/85 mm Hg. One and one-half hours after induction, his blood pressure drops to 90/60. List 5 reasons for intraoperative hypotension in this man: briefly discuss how each of these items actually causes the blood pressure to fall. (10) |
1. isoflurane = myocardial depression = hypotension
2. nitrous oxide = myocardial depression = hypotension 3. morphine = release histamine = vasodilation hypotension 4. blood loss = hypovolemia hypotension 5. positive pressure ventilation = IVC compression = decreased venous return = decreased preload = hypotension |
|
|
List 5 potential complications from the use of non-steroidal anti-imflammatory drugs i.e NSAIDS. (10)
|
AIN, fluid retention, allergy, gastritis/GI bleed, hypertension, bone marrow suppression (platelet dysfunction), worse CHF
|
|
|
What is the aortocaval syndrome?
|
Compression of IVC and/or aorta by gravid uterus.
|
|
|
List three ways to decrease the effects associated with aortocaval syndrome.
|
1. Lie patient on left side, 2. Right hip wedge, 3. Avoid supine position
|
|
|
List 4 potential complications of single unit blood transfusion and 6 potential complications related to multiple unit blood transfusion. (10)
|
Single: Immune, nonhemolytic: 1. immediate hemolytic reaction, 2. delayed hemolytic reaction 3. infection, 4. allergic reaction
Multiple: 1. hyperkalemia, 2. dilutional coagulopathy, 3. dilutional thrombocytopenia, 4. circulatory overload, 5. citrate toxicity (hypocalcemia), 6. iron overload |
|
|
List 5 ways in which you could distinguish between a neuromuscular block associated with a 1-mg/kg dose of succinylcholine and one associated with a non-depolarizing muscle relaxant (Rocuronium).
|
Succinylcholine = time to block < 1 min, no fade with tetanus, not reversible, TOF ratio > 0.4
Non-depolarizing (Rocuronium) = > 2 mins, fades with tetanus, positive post tetanic facilitation, reversible, TOF ratio < 0.7 |
|
|
List 5 ABSOLUTE contraindications to the administration of either succinylcholine or a non-depolarizing relaxant. (Do not give the contraindications to succinylcholine, rather GENERAL absolute contraindications to muscle relaxation with either type of drug. Assume the patient has a functioning intravenous in situ) (5)
|
1. allergy to medication
2. unable to secure airway 3. lack of resuscitative equipment 4. lack of anaethesia medications 5. unable to bag mask ventilate |
|
|
Name 2 situations, 1 in the operating room and 1 outside the operating room setting where a laryngeal mask might be used. (2)
|
Surgery where intubation not required:
1. No risk of aspiration 2. Short procedure 3. Non-obese, not pregnant, no ascites OUTSIDE OR Emergent - can't intubate, can't ventilate. Inadequate seal (e.g. beard) with face mask |
|
|
List 6 contraindications to the elective use of a laryngeal mask in the operating room. (6)
|
need PPV, risk of aspiration, pharyngeal pathology, limited mouth opening, cervical vertebra/laryngeal cartilage #, spontaneous breathing, trendelenberg positioning
|
|
|
What size laryngeal mask would be used for an average female (1) and an average male (1)? (2)
|
females 3, males 4
|
|
|
35-year old man is having an inguinal hernia repair under general endotracheal anesthesia. He is a previously healthy man with no cardiorespiratory problem. He is intubated with a 8.0mm endotracheal tube and his lungs are being ventilated with a tidal volume of 500 cc at a respiratory rate of 10 breaths/minute. His intraoperative course has been uneventful since the induction of anesthesia, 1 hour ago. Over the course of 15 minutes, his oxygen saturation, which had been stable at 98% has fallen to 90%. BP is 120/80 and heart rate is 110 bpm. List 5 possible causes of this problem and for each problem, list one therapeutic intervention to improve the situation. (10)
|
Endobronchial intubation: pull back tube
Tube disconnected: check tubing Patient biting down on tube: relaxation, insert oropharyngeal airway Secretions blocking tube: suction PE/Atelectasis = increase PEEP to reduce atelectasis |
|
|
Name 5 SPECIFIC preoperative investigations that an anaesthetist would consider important information in the assessment of a patient suffering from severe chronic obstructive lung disease who is scheduled for an elective ventral hernia repair. (5)
|
Hgb, PaO2, PaCO2, HCO3, PFTs, CXR, EKG
|
|
|
Name 5 SPECIFIC preoperative investigations that an anaesthetist would consider important information in the assessment of a patient suffering from severe chronic obstructive lung disease who is scheduled for an elective ventral hernia repair and give a BRIEF reason as to the importance for each individual investigation.
|
1. ABG: hypoxemia, acidosis and appropriate compensation
2. CXR: hyperflation and evidence of any cardiac failure or pulmonary infection 3. CBC: any additional pulmonary infection 4. PFT: extent of obstruction 5. ECG: cardiac failure |
|
|
List 5 classes of drugs that a patient may be asked to discontinue prior to elective surgery. (10)
|
1. oral hypoglycemics
2. anticoagulants 3. antiplatelets 4. insulin 5. antidepressants |
|
|
A 75-year-old man undergoing a laparotomy for a bowel obstruction has received a general anaesthetic. He is intubated and ventilated and has been paralyzed with rocuronium. Anesthesia is maintained with 70% nitrous oxide, 30% oxygen and 1% isoflurane. He has a history of hypertension for which he takes Vasotec. One hour after the surgery began, his blood pressure, which had been stable, drops to 80/40 mm Hg.
A. List 5 actions you would take at this point. |
1. verify monitors connected properly
2. crystalloid infusion - Ringer's Lactate 3. decrease nitrous oxide = will increase BP 4. decrease isoflurane = will increase peripheral resistance 5. consider phenylephrine - will increase peripheral resistance without increasing heart rate and contractility. |
|
|
List 5 common causes of intraoperative hypotension. (5)
|
1. inhalational anesthesia
2. opiods 3. hemorrhage 4. loss of fluids 5. positive airway ventilation causing IVC compression |
|
|
A previously healthy 32-year-old man has undergone an open reduction and internal fixation of a tibial fracture following an injury incurred in a football game. He weighs 90 kg and has no history of abnormal bleeding or bruising. He is currently taking ranitidine 150 mg once daily for a duodenal ulcer and is asymptomatic. He has no known allergies. In the Post Anaesthetic Care Unit (PACU), he is complaining of severe pain.
A. In the PACU, what medication and dose would you use to start treating his pain? (3) |
Morphine 1-3 mg IV
|
|
|
What THREE specific methods of anaesthesia can be used for a Caesarean section. (3)
|
Epidural, spinal, GA
|
|
|
List 4 common side effects of opioid medications.
|
1. histamine release leading to hypotension
2. constipation 3. respiratory depression 4. nausea/vomitting |
|
|
A previously healthy 32-year-old man has undergone an open reduction and internal fixation of a tibial fracture following an injury incurred in a football game. He weighs 90 kg and has no history of abnormal bleeding or bruising. He is currently taking ranitidine 150 mg once daily for a duodenal ulcer and is asymptomatic. He has no known allergies. In the Post Anaesthetic Care Unit (PACU), he is complaining of severe pain.
After 1 hour and a large dose of morphine he is still in pain. What alternate therapy could you offer him? |
(3) PCA Using hydromorphone
|
|
|
What THREE specific methods of anaesthesia can be used for a Caesarean section. List two significant disadvantages of each technique. (6)
|
1. epidural: block sympathetic nerves and worsen hypotension, slower onset
2. spinal: block sympathetic nerves and worsen hypotension, one dose only, motor block, dural puncture headache 3. general: technique difficult due to upper airway edema, maternal drugs transfer to neonate causing neonatal depression and requiring resuscitation |
|
|
What type of anaesthesia would most likely be given to a patient requiring EMERGENCY Caesarean section for an acute haemorrhage secondary to an abruptio placenta? (1)
|
insufficient time to establish regional anaesthesia. Thus rapid sequence general anesthesia.
|
|
|
List 2 common uses for propofol. (2)
|
1. induction, 2. maintenance anesthesia
|
|
|
List 5 important physiological effects of an intravenous induction dose of propofol. (5)
|
1. decreased ICP, 2. increased IOP, 3. decreased RR, 4. decreased BP, 5. decreased CO
|
|
|
Pain on injection may occur with propofol. List 3 ways you might avoid or decrease the incidence of this side effect? (3)
|
1. mix in small dose of lidocaine, 2. administer through a fast flowing iv catheter,
3. adminster through a more proximal iv catheter |
|
|
What are the five minimum pieces of equipment required to intubate? (5)
|
1. suction, 2. O2, 3. laryngoscopy, 4. ETT, 5. stylet
|
|
|
A 24 year old previously healthy male is brought by ambulance to the emergency department. He has taken an unknown quantity of an unknown drug. He is unconscious and breathing at a rate of 5 per minute. His saturation on room air is 88%. He has no gag reflex and the casualty officer would like you to intubate him. He has not sustained a cervical spine injury. Assuming that all the equipment you need is ready, describe the five steps you would follow to perform the intubation. (5)
|
1. position patient
2. open mouth 3. laryngoscopy 4. insert ETT though vocal cords, remove laryngoscope 5. confirm ETT placement |
|
|
Name 3 ways to confirm placement of an ETT.
|
1. Chest wall rising with ventillation
2. Air entry heard by stethoscope at bilaterally at the mid-axillary line 3. End tidal CO2 30-40mmHg |
|
|
List 5 GENERAL causes of hypoxaemia. (10) (Do not give specific examples i.e. pulmonary embolus).
|
1. decreased FIO2
2. decreased alveolar ventilation 3. increased shunting 4. increased dead space ventilation 5. decreased diffusion 6. poor placement of ETT |
|
|
A 60 year old woman with insulin-dependent diabetes presents to the preoperative consultation clinic having been scheduled for a total knee arthroplasty in 2 week’s time.
A. What 6 specific questions related to her diabetes would be important to ask to assess her fitness for anaesthesia and surgery? (6) B. What 4 specific tests would you order preoperatively? (4) |
1. how long?
2. end organ damage? 3. monitor blood glucose regularly? 4. adequate control? 5. admissions to hospital for hypo or hyperglycemia? 6. other CAD risk factors? 1. blood glucose, 2. ECG, 3. lytes and creatinine, 4. urinalysis |
|
|
A 50 year old man takes beta blockers and Ca2+ channel blockers for stable angina. He is coming for elective surgery in one week. What should you tell him about his medications and eating and drinking before his operation? (3)
B) What are 2 reasons that we have patients fast before elective surgery? (2) C) What immediate outcome may occur under general anaesthesia in a patient who has a full stomach? D - What is a potential consequence of this outcome? E - What 3 reasons contribute to these outcomes? (3) |
A- 1. take B-blockers and CCB at usual time with sips of water
2. no solids at least 8 hrs prior 3. no fluids at least 4 hrs prior B - 1. decrease gastric volume, 2. decrease gastric acidity C - (1) aspiration D - (1) pneumonitis, atelectasis, ARDS, abscess E - volume, acidity, particulate matter |
|
|
Many unnecessary blood tests are ordered prior to surgery. List 5 pieces of information learned from the patient’s history that would cause you to order preoperative coagulation studies. (10)
|
1. on anticoagulants, 2. liver disease, 3. known factor deficiency, 4. family history of factor deficiency
5. surgery involving lots of blood loss |
|
|
A. You are called to the postanaesthetic care unit to see a patient who has a saturation of 80%. She has been in the PACU for 20 minutes after having had a total abdominal hysterectomy. She is otherwise healthy. Her blood pressure is 120/80 mm Hg and her heart rate is 120 bpm. Describe in point form EXACTLY what your management of this situation would be. (5)
B. What are five GENERAL potential causes of her tachycardia? (5) |
A - 1. assess airway, secure airway
2. assess need for ventilation 3. increase O2 4. look for acute blood loss, stop 5. fluid resuscitation 6. Control pain 7. Empty bladder B - Hypovolemia, pain, arrhythmia, full bladder, anxiety, anemia, drugs (e.g. atropine, pancuronium) |
|
|
You are called to the floor to see a patient who the nurse believes has had a narcotic overdose. He has been on the ward for 2 hours having just had an open reduction and internal fixation of a femoral fracture. He is on PCA which his wife has been using regularly on his behalf.
A. What would be your management of the situation at this point? (2) B. If the patient is rousable and maintains his airway, what would you do in this case? (5) C. If the patient is difficult to rouse, snores and has a respiratory rate of 8 per minute, and a saturation of 80% on room air with a stable BP and Heart rate, what would you do? (3) |
A - Assess responsiveness, resp rate, heart rate, pupils, educate patient and wife
B - reduce PCA infusion rate, hold bolus doses for now, reassess frequently C - 1. assess and secure airway 2. give O2 3. give small incremental doses of 40 mcg naloxone |
|
|
List 5 options for pain relief during labour. (5)
Lamaze, epidural, NO, pudendal block, opioids B. For each of the options for pain relief during labour listed above; give 1 advantage and 1 disadvantage for each. (5) |
Lamaze: gives woman control, not great analgesia
Epidural: good analgesia, hypotension NO: easy, does not relieve pain completely Spinal: good analgesia, motor blockade Opioids: easy, maternal/neonatal depression |
|
|
You are called to the recovery room (PACU) to see a patient who has just arrived after having had a laparoscopic cholecystectomy. The patient was awake, alert, extubated and breathing spontaneously. The nurse has just given a gram of Ancef intravenously at the surgeon’s request. The nurse tells you that the patient is having an “allergic reaction”.
A) What 5 signs and/or symptoms might the patient be experiencing to support this diagnosis? (5) B) What 5 steps MUST be taken to treat this patient? (Be specific) (5) |
A - rash, stridor, tachycardia, hypotension, bronchospasm, urticaria
B - 1. Stop Ancef, 2. 100% O2, 3. 50 mcg epinephrine iv, 4. N/S, 5. benadryl 50 mg iv 6. Ranitidine |
|
|
A. What two genetic disorders related to anaesthesia might be elicited by asking a patient about their family history of anaesthetics? What investigations can be done to determine if the disorder has been transmitted to the patient? (4)
B. What would be the symptoms that might occur, related to each disorder, if a patient received a general anaesthetic without any precautions against the above problems? (6) (Separate the symptoms according to the disorder.) |
A - Cholinesterase deficiency: genotyping
MH: muscle biopsy B - Cholinesterase deficiency: prolonged paralysis MH: - hypermetabolic state (increased temp, increased O2 consumption, resp acidosis, tachypnea, tachycardia) - muscle rigidity - rhabdomyolysis - renal failure |
|
|
With respect to the following drugs:
A. What is the usual initial dose of epinephrine used in a cardiac arrest situation? (1) B. What is the optimal route of administration of epinephrine in the above situation? (1) C. What is the dose of lidocaine used for ventricular dysrhythmias? D. What is the weight of a patient to whom the administration of 20 ml of 2% lidocaine with epinephrine would be a maximum? E. What dose of epinephrine is contained in 1 cc of a 1:200,000 solution? (1) F. List 3 advantages of mixing epinephrine in local anaesthetic solutions (3) G. What dosage of atropine should be given to a patient with a bradyarrhythmia who is hypotensive? (1) H. 20ml of 1.5% lidocaine is equivalent to how many milligrams? |
A - 1mg IV push q3-5 min
B - IV push q3-5 min C - 1-1.5 mg/kg push D - 400mg/7=57 E - 5 mcg F - Decrease systemic absorption, higher threshold for anesthetic, longer duration of epidural G - 0.5-1.0mg H - 300mg - IV lidocaine 1% = 10mg/ml. 1.5% lidocaine = 15mg/ml |
|
|
List 5 maneuvers that can be used to open the airway and permit ventilation in an unconscious patient that you are unable to ventilate with a bag and mask alone. (10)
|
1. chin lift, 2. jaw thrust, 3. insert nasal airway, 4. insert oral airway, 5. remove any foreign object
|
|
|
. List 4 methods to absolutely confirm that an endotracheal tube is situated in the trachea. (10)
|
See it go through cords, bronchoscope, capnograph, CXR
|
|
|
You are seeing a 30 year old woman in your family practice office as part of a work-up for infertility. She has had asthma for the past ten years and uses a Ventolin inhaler on a prn basis. Over the past three weeks, she has been using the Ventolin more than usual and has been waking up at night coughing. On physical examination she has bilateral wheezes that do not clear with cough. She is scheduled to have a diagnostic laparoscopy in one week’s time.
A. What are four therapeutic modalities that may be used to improve her condition? (8) B. When you see her again on the day prior to surgery, her condition is unchanged. What would you do at this point? (2) |
A - 1. addition of inhaled steroid, 2. addition of inhaled LABA, 3. addition of oral steroid, 4. smoking cessation
B - Cancel and optimize? |
|
|
A 65 year old man with untreated hypertension presents to the emergency department, complaining of severe abdominal pain. He has been seen by general surgery and has an incarcerated inguinal hernia that required EMERGENCY surgery. His blood pressure is now 200/120 mm Hg. List five IMPORTANT and specific anaesthetic considerations of this patient undergoing this procedure.
A. Give 5 indications for performing a rapid sequence induction. (5) B. Besides performing a rapid sequence induction, how can we minimize the risk of aspiration? (5) |
A - GERD/hiatus hernia, not NPO, pregnant, overdose/LOC, delayed emptying
B - 1. NPO (8 hrs for food, 4 hrs for clear fluids) 2. H2-antagonists to decrease acidity (eg. Na citrate) 3. increase gastric emptying (eg. metoclorpropamide) 4. NG tube to empty stomach 5. extubate awake on side |
|
|
A - Describe the ACLS protocol for symptomatic Bradycardia.
B - What should be done if the above measures fail? |
Pacing Always Ends Danger
Pacing **TCP Immediately prepare for transcutaneous pacing (TCP) with serious circulatory compromise due to bradycardia (especially high-degree blocks) or if atopine failed to increase rate. Consider medications while pacing is readied. Always - Atropine = 1st-line drug, 0.5 mg IV/IO q3-5 min. (max. 3mg) Ends - Epinephrine 2-10 µg/min 2nd-line drugs to consider if atropine and/or TCP are ineffective. Use with extreme caution. Danger - Dopamine - 2-10 µg/kg/min B - Search for other causes - |
|
|
What are the ACLS DDx for a problem search when interventions fail to correct cardiac abnormalities.
|
6H's and 5T's
Hypoxia Hypoglycemia Hypo/Hyperkalemia Hypocalcemia Hypovolemia Hypothermia Hyperacidemia Thrombus - MI/PE Tension Pneumo Tamponade |
|
|
How should you treat symptomatic hyperkalemia?
|
Sodium bicarbonate, calcium chloride, albuterol nebulizer, insulin/glucose, dialysis, diuresis, Kayexalate
|
|
|
What features would you see with a patient who is crashing and has cardiac tamponade?
What is the treatment? |
No pulse w/ CPR, JVD, narrow pulse pressure prior to arrest.
Tx - Pericardiocentesis. |
|
|
Why do you give Fentanyl intraoperatively despite the patient being unconscious?
What about when harvesting organs from a brain dead patient? |
Despite unconsciousness, incision and intubation will result in a pronounced sympathetic drive at level of spinal cord.
You must control pain and hemodynamics even on a brain dead patient. |
|
|
What are contraindications to inhaled anaesthetics?
What are your options? |
Hx of Malignant Hyperthermia
Cardiopulmonary procedures that bypass heart and lungs Neck Surgery preventing access Options are to use local, regional or TIVA GA (propofol, thiopental or Ketamine ) |
|
|
How are exhaled anaesthetics such as sevoflurane and isoflurane cleared from the body?
|
By inhalation - thus you need to increase the O2 when preparing for extubation.
|
|
|
An 82 year old male is scheduled for elective repair of a AAA. What factors will affect his perioperative plan and outcome?
|
Elderly - Requires lower MAC, less opioids, increased risk of delirium, more pronounced hemodynamic changes, less pulmonary reserve for intubation.
Vascular surgery = >5% mortality. |
|
|
Describe the primary and secondary ABCDs.
|
Primary = BLS protocol, Airway with head tilt, Breathing with bag, Chest compressions, Defibrillation.
Secondary = ETT, Breathing monitors, Circulatory IV and Meds, Differential Dx = PATCH4 MDS |
|
|
How should you manage an unstable VT or VF tachycardia without pulses?
ACLS Pulseless arrest algorythm |
1. 5 cycles of CPR followed by Synchronized cardioversion for all unstable VT and VF tachycardias. Followed by 5 cycles of CPR. Give Epinephrine. 5 cycles CPR. Check rhythm.
2. Do secondary survey - PATCH4 MDS if no response to measures. |
|
|
How should you manage an unstable PEA and Asystole tachycardia without pulses?
ACLS Pulseless Arrest Algorythm |
5 cycles of CPR. IV epinephrine 1 mg every 3-5 min. 5 cycles of CPR. Atropine 1mg IV. 5 cycles of CPR. Check rhythm.
Do secondary survey - PATCH4 MDS if no response to measures. |
|
|
How should tachycardia with pulses be managed.
ACLS Tachycardia Algorythm |
1. Unstable? Immediate synchronized cardioversion.
2. Stable? Narrow QRS = Vagal manoevre, Adenosine, Converts = SVT Tx recurrence with Beta blocker (metoprolol) or diltiazem Does not convert = A Fib or Flutter - Diltiazem oe Beta-blocker (metoprolol). Wide QRS = Amiodarone and Cardioversion |
|
|
How should Bradycardia be approached within the ACLS algorythm?
|
1. HR <60 and adequate perfusion = monitor with ECG, IV access, O2, oximetry, ABG, Lytes.
2. HR <60 and poor perfusion = Prepare transcutaneous pacing, consider atropine 1mg IV, epinephrine 1mg IV if no response, continue pacing. Search for causes - PATCH4 MDS |
|
|
A 50 year old man takes beta blockers and Ca2+ channel blockers for stable angina. He is coming for elective surgery in one week. What should you tell him about his medications and eating and drinking before his operation? (3)
|
1. take B-blockers and CCB at usual time with sips of water
2. no solids at least 8 hrs prior 3. no fluids at least 4 hrs prior |
|
|
B) What are 2 reasons that we have patients fast before elective surgery? (2)
|
1. decrease gastric volume, 2. decrease gastric acidity
|
|
|
What immediate outcome may occur under general anaesthesia in a patient who has a full stomach?
What is a potential consequence of this outcome? What 3 reasons contribute to these outcomes? (3) |
(1) aspiration
(1) pneumonitis, atelectasis, ARDS, abscess volume, acidity, particulate matter |
|
|
Many unnecessary blood tests are ordered prior to surgery. List 5 pieces of information learned from the patient’s history that would cause you to order preoperative coagulation studies. (10)
|
1. on anticoagulants, 2. liver disease, 3. known factor deficiency, 4. family history of factor deficiency
5. surgery involving lots of blood loss |
|
|
A 60 year old woman with insulin-dependent diabetes presents to the preoperative consultation clinic having been scheduled for a total knee arthroplasty in 2 week’s time.
A. What 6 specific questions related to her diabetes would be important to ask to assess her fitness for anaesthesia and surgery? (6) B. What 4 specific tests would you order preoperatively? (4) |
1. how long?
2. end organ damage? 3. monitor blood glucose regularly? 4. adequate control? 5. admissions to hospital for hypo or hyperglycemia? 6. other CAD risk factors? 1. blood glucose, 2. ECG, 3. lytes and creatinine, 4. urinalysis |
|
|
List 5 GENERAL causes of hypoxaemia. (10) (Do not give specific examples i.e. pulmonary embolus)
|
1. decreased FIO2
2. decreased alveolar ventilation 3. increased shunting 4. increased dead space ventilation 5. decreased diffusion |
|
|
A. You are called to the postanaesthetic care unit to see a patient who has a saturation of 80%. She has been in the PACU for 20 minutes after having had a total abdominal hysterectomy. She is otherwise healthy. Her blood pressure is 120/80 mm Hg and her heart rate is 120 bpm. Describe in point form EXACTLY what your management of this situation would be. (5)
B. What are five GENERAL potential causes of her tachycardia? (5) |
A. 1. assess airway, secure airway
2. assess need for ventilation 3. increase O2 4. look for acute blood loss, stop 5. fluid resuscitation B. Hypovolemia, pain, arrhythmia, full bladder, anxiety, anemia, drugs (e.g. atropine, pancuronium) |
|
|
You are called to the floor to see a patient who the nurse believes has had a narcotic overdose. He has been on the ward for 2 hours having just had an open reduction and internal fixation of a femoral fracture. He is on PCA which his wife has been using regularly on his behalf.
A. What would be your management of the situation at this point? (2) B. If the patient is rousable and maintains his airway, what would you do in this case? (5) C. If the patient is difficult to rouse, snores and has a respiratory rate of 8 per minute, and a saturation of 80% on room air with a stable BP and Heart rate, what would you do? (3) |
A. Assess responsiveness, resp rate, heart rate, pupils, educate patient and wife
B. reduce PCA infusion rate, hold bolus doses for now, reassess frequently C. 1. assess and secure airway 2. give O2 3. give small incremental doses of 40 mcg naloxone |
|
|
List 5 options for pain relief during labour and give 1 advantage and 1 disadvantage for each. (5)
|
Lamaze: gives woman control, not great analgesia
Epidural: good analgesia, hypotension NO: easy, does not relieve pain completely Spinal: good analgesia, motor blockade Opioids: easy, maternal/neonatal depression |
|
|
You are called to the recovery room (PACU) to see a patient who has just arrived after having had a laparoscopic cholecystectomy. The patient was awake, alert, extubated and breathing spontaneously. The nurse has just given a gram of Ancef intravenously at the surgeon’s request. The nurse tells you that the patient is having an “allergic reaction”.
A) What 5 signs and/or symptoms might the patient be experiencing to support this diagnosis? (5) B) What 5 steps MUST be taken to treat this patient? (Be specific) (5) |
A. rash, stridor, tachycardia, hypotension, bronchospasm, urticaria
B. 1. Stop Ancef, 2. 100% O2, 3. 50 mcg epinephrine iv, 4. N/S, 5. benadryl 50 mg iv |
|
|
What two genetic disorders related to anaesthesia might be elicited by asking a patient about their family history of anaesthetics? What investigations can be done to determine if the disorder has bee transmitted to the patient? (4)
B. What would be the symptoms that might occur, related to each disorder, if a patient received a general anaesthetic without any precautions against the above problems? (6) (Separate the symptoms according to the disorder.) |
A. Cholinesterase deficiency: genotyping
MH: muscle biopsy B. Cholinesterase deficiency: prolonged paralysis MH: - hypermetabolic state (increased temp, increased O2 consumption, resp acidosis, tachypnea, tachycardia) - muscle rigidity - rhabdomyolysis |
|
|
A. What is the usual initial dose of epinephrine used in a cardiac arrest situation? (1)
1mg B. What is the optimal route of administration of epinephrine in the above situation? (1) IV push C. What is the dose of lidocaine used for ventricular dysrhythmias? (1) 1-1.5 mg/kg push D. What is the weight of a patient to whom the administration of 20 ml of 2% lidocaine with epinephrine would be a maximum? (1) 400mg/7=57 E. What dose of epinephrine is contained in 1 cc of a 1:200,000 solution? (1) 5 mcg F. List 3 advantages of mixing epinephrine in local anaesthetic solutions (3) Decrease systemic absorption, higher threshold for anesthetic, longer duration of epidural G. What dosage of atropine should be given to a patient with a bradyarrhythmia who is hypotensive? (1) 0.5-1.0mg H. 20ml of 1.5% lidocaine is equivalent to how many milligrams? (1) 300mg |
A. 1mg
B. IV push C. 1-1.5 mg/kg push D. 400mg/7=57 E. 5 mcg F. Decrease systemic absorption, higher threshold for anesthetic, longer duration of epidural G. 0.5-1.0mg H. 300mg |
|
|
List 5 maneuvers that can be used to open the airway and permit ventilation in an unconscious patient that you are unable to ventilate with a bag and mask alone. (10)
|
1. chin lift, 2. jaw thrust, 3. insert nasal airway, 4. insert oral airway, 5. remove any foreign object
|
|
|
List 4 methods to absolutely confirm that an endotracheal tube is situated in the trachea. (10)
|
See it go through cords, bronchoscope, capnograph, CXR
|
|
|
You are seeing a 30 year old woman in your family practice office as part of a work-up for infertility. She has had asthma for the past ten years and uses a Ventolin inhaler on a prn basis. Over the past three weeks, she has been using the Ventolin more than usual and has been waking up at night coughing. On physical examination she has bilateral wheezes that do not clear with cough. She is scheduled to have a diagnostic laparoscopy in one week’s time.
A. What are four therapeutic modalities that may be used to improve her condition? (8) B. When you see her again on the day prior to surgery, her condition is unchanged. What would you do at this point? (2) |
A. 1. addition of inhaled steroid, 2. addition of inhaled LABA, 3. addition of oral steroid, 4. smoking cessation
B. Cancel and optimize |
|
|
Give 5 indications for performing a rapid sequence induction. (5)
B. Besides performing a rapid sequence induction, how can we minimize the risk of aspiration? (5) |
A. GERD/hiatus hernia, not NPO, pregnant, overdose/LOC, delayed emptying,
B. 1. NPO (8 hrs for food, 4 hrs for clear fluids) 2. H2-antagonists to decrease acidity (eg. Na citrate) 3. increase gastric emptying (eg. metoclorpropamide) 4. NG tube to empty stomach 5. extubate awake on side |
|
|
You are attending a breech delivery (in a peripheral hospital) with the staff obstetrician. It is a very difficult delivery complicated by trapping of the after-coming head. When the baby is finally delivered, it is limp and blue. The obstetrician is attending to the mother who is having a brisk postpartum haemorrhage.
A. The baby’s heart rate is 50 bpm. What resuscitative efforts should be done now? List 8 steps/actions in the management of this situation (8) B. At 6 minutes of life, the heart rate is 120 bpm, respirations are slow and irregular. The baby is limp, does not respond to stimulation but is centrally pink with blue hands and feet. What Apgar score corresponds with these findings? (2) |
A.
1. open airway (infant supine or on side) 2. suction mouth then nose 3. 100% O2 4. keep neonate warm and dry 5. physical stimulation (slapping soles of feet, rubbing back) 6. PPV if apnea, HR <100, or central cyanosis despite 100% O2 7. chest compressions (if HR < 80 despiate PPV) 8. iv fluids (pallor despite 100% O2, weak pulse, BP < 55.30) 9. epinephrine (0.01 mg/kg) if HR still < 80 despiate 100% O2 and chest compressions B. HR: 2, Respiration: 1, Irritability: 0, Tone: 0, Colour: 1, TOTAL: 4 |
|
|
What are the five minimum pieces of equipment required to intubate? (5)
|
1. suction, 2. O2, 3. laryngoscopy, 4. ETT, 5. stylet
|
|
|
A 24 year old previously healthy male is brought by ambulance to the emergency department. He has taken an unknown quantity of an unknown drug. He is unconscious and breathing at a rate of 5 per minute. His saturation on room air is 88%. He has no gag reflex and the casualty officer would like you to intubate him. He has not sustained a cervical spine injury. Assuming that all the equipment you need is ready, describe the five steps you would follow to perform the intubation. (5)
|
1. position patient in sniffing position
2. open mouth and check for obstructions, dentition 3. laryngoscopy, exposing the vocal cords 4. insert ETT though vocal cords, remove laryngoscope 5. confirm ETT placement with stethoscope, end-tidal CO2, condensation or bronchoscope confirmation. |
|
|
Name 5 ways that you can confirm placement of an ETT tube.
|
1. Visualize placement with naked eye or glidescope.
2. Bronchoscopy down tube 3. Auscultate lungs for breath sounds 4. End Tidal CO2 5. Condensation on ETT 6. Compliance of manual bag with ventillation and chest expansion 7. CXR |
|
|
Describe the sniffing position for placement of an ETT. Why important?
|
Flexion of C6-C7 and Extension of C1-C2.
Aligns Oral, pharyngeal and laryngeal axis. |
|
|
List 5 problems associated with the use of intramuscular narcotics ordered on a prn basis for postoperative pain. (10)
|
Inadequate analgesia, increased side-effects, delays to relief, large variability in different patients in maximum levels, wide fluctuations, painful injections
|
|
|
A 20 year old male is scheduled for removal of impacted wisdom teeth under general anaesthesia. During a pre-op assessment, he states that his first cousin had an unusual reaction under anaesthesia and subsequently had a positive biopsy for malignant hyperthermia. Neither of his parents has had a general anaesthetic.
A. What 2 anaesthetic agents should be avoided in this patient? (4) B. List five signs of a malignant hyperthermia reaction. (5) C. What is the drug of choice and dose for treating malignant hyperthermia? (1) |
A. succinylcholine, inhalational agents
B. Hyperthermia, muscle rigidity, hypertension, tachycardia, tachypnea, cyanosis C. dantrolene (2 mg/kg) |
|
|
List four GENERAL indications for endotracheal intubation (NOT restricted to the operating room setting). (10)
|
Five P's
1. Protect airway - aspiration 2. Pharm - administer medications NAVEL (naloxone, atropine, ventolin, epinephrine, lidocaine) 3. Pulmonary toilet - to remove tracheobronchial secretions and prevent ARDS and Atelectasis 4. Positive pressure ventilation - hypoventilation, apnea, hypoxia, status asthmaticus 5. Patency - decreased LOC, facial fractures, edema |
|
|
A 65-year old man is referred to your internal medicine office with the following story: He has had stable class I angina for four years, for which he is taking Vasotec and sublingual nitroglycerine prn. Recently, he has experienced some angina at rest and at night and an episode a week ago lasted half an hour and did not respond to nitroglycerine. He has benign prostatic hypertrophy and is scheduled for surgery (transurethral resection of the prostate) in two weeks time.
A. What are three specific concerns regarding this man’s story? (6) B. List 4 items in your plan of action at this time. (4) |
A. 1. night symptoms, 2. angina at rest, 3. not responsive to NTG
B. Go to ER, ECG, troponins, stress test, Echo, cath |
|
|
At the end of a 2-hour laparoscopic cholecystectomy, all inhalation anaesthetics are turned off and the patient is ventilated through the endotracheal tube with 100% oxygen. After 10 minutes, the patient, who is still intubated, has not begun to breathe spontaneously. Blood pressure is 120/80 mm Hg, heart rate 98 bpm. Anaesthesia was induced with propofol and fentanyl. Intubation was facilitated by 100 mg of intravenous succinylcholine. Maintenance of anaesthesia involved the use of incremental doses of rocuronium, morphine, nitrous oxide and isoflurane. List 5 common and important potential causes of this patient’s postoperative apnea. (10)
|
1. rocuronium, 2. morphine, 3. nitrous oxide, 4. isoflurane, 5. succinylcholine
|
|
|
A 83 year old man with a history of hypertension is undergoing emergency surgery for an incarcerated inguinal hernia. Shortly after induction of the general anesthesia with fentanyl 50 micrograms, propofol 160 mg and rocuronium 50 mg, Nitrous oxide 70% and oxygen 30% and Isoflurane 1%, his blood pressure which had been 150/90 mm Hg on admission to the OR is now 80/60 with a heart rate of 120 bpm.
A. What might be the cause of this fall in blood pressure? (5) B. What would you do? (5) |
A. 1. fentanyl, 2. propofol, 3. nitrous oxide, 4. isoflurane, 5. decreased sympathetics after removal of painful stimulus
B. 1. crystalloids, 2. phenylephrine (increases BP without increasing HR), 3. decrease nitrous oxide 4. decrease isoflurane, 5. monitor |
|
|
Name 5 conditions that are associated with difficult VENTILATION.
|
BONES.
Beard, Obeses, No teeth, Elderly, Snoring (Sleep apnea). |
|
|
Name 6 conditions associated with a difficult INTUBATION and 1 reason why for each.
|
1. Obesity - extra tissue collapses airway
2. Pregnancy - edematous tissues 3. Scleroderma - connective tissue leads to low compliance in pharynx. 4. Arthritis - Osteo and Rheum - c-spine instability, TMJ stiffness, atlanto-axial instability 5. Acromegaly - big tongue, thick throat 6. Congenital anomolies. |
|
|
List 4 MAJOR side effects related to the use of NSAIDS. (8)
B. What is the mechanism of action that leads to the adverse effects? (2) |
A. 1. bleeding, 2. renal failure, 3. worsens CHF, 4. PUD
B. 1. platelet inhibition, 2. prostaglandin synthesis inhibition |
|
|
List 5 advantages of the use of patient-controlled analgesia over intramuscular injections of narcotics. (10)
|
Quicker onset
No painful injections Able to adjust to patient variability Able to adjust as pain needs change overtime Reduce side-effects More effective analgesia |
|
|
You have just positioned a patient supine after administering a spinal anesthetic with hyperbaric bupivacaine for an elective repeat cesarean section. The patient’s blood pressure was 110/65 preoperatively and is now 88/45.
A. List 2 reasons why her blood pressure has dropped. (2) B. What is your immediate management? (3) C. List three signs or symptoms that she might experience while her blood pressure is 88/45. (2.5) D. List three other signs or symptoms that she might experience while her blood pressure is 88/45. (2.5) E. List the 5 components of the Apgar score. (2.5) |

A. Aortocaval, sympathetic nerve block from spinal anesthesia
B. 1. position patient on left side, 2. O2, 3. IV crystalloids C. lightheadedness, palpitations, visual changes, D. 1. tachycardia, 2. tachypnea, 3. presyncope E. Activity, Pulse, Grimmace, Appearance, Respirations 1-3. |
|
|
A previously healthy 18 year old male was stabbed in the back at an after hours club. He comes to the ER with a single wound 2 cm in length, 5 cm below the left scapula and 15 cm left of the midline. He is awake and alert, BP 110/50 mm Hg, SpO2 97%.
A. What immediate steps should be taken in the management of this patient? (3) 10 minutes later he is pale, diaphoretic: BP 70/40 mm Hg, HR 130 bpm. SpO2 88% B. What are 3 LIKELY possibilities for the above changes. (3) C. What treatment measures would you institute at this point? (2) He stabilises for 1 hour, then again gets hypotensive. His repeat Hb is 45. You now decide to give him a blood transfusion immediately. Unfortunately the blood bank says it will be 30 min. before fully cross matched blood is available. D. What are your transfusion options at this time? (2) |
A. ABCs, IV, O2 monitor, Cardiac monitor
B. Tension pneumo, tamponade, hemothorax C. Ventilate with 100% O2, fluids wide open D. O positive, type specific |
|
|
Succinylcholine is often given to patients undergoing anaesthesia and surgery. In otherwise healthy patients with no history of neuromuscular diseases, allergy, personal or family history of pseudocholinesterase deficiency, list 5 side effects that may occur with the intravenous administration of 1 mg/kg of succinylcholine. (Do not include malignant hyperthermia trigger) (10)
|
Myalgias, hyperkalemia, bradycardia, increased secretions, increased ICP/IOP
|
|
|
A 50 year old female has undergone a total abdominal hysterectomy. She has been fasting since midnight. Her surgery began at 08:00 and took 2 hours. The total estimated blood loss was 500 cc. Considering all sources of perioperative fluid loss, answer the following question.
How much fluid (i.e. Normal saline) should she be given by the end of the case? Show how you derived the total amount, including formulas. She weighs 50 kg. (10) |
maintenance requirement per hour: 4 ml x 10 kg + 2 ml x 10 kg + 1 ml x 30 ml = 90 ml/h
fluid deficit: 90 ml/h x 10 h = 900 ml third space losses: 6 ml/kg/h x 50 kg x 2 hr = 600 ml blood loss replacement: 500 ml x 3 = 1500 ml TOTAL: 3090 ml |
|
|
What is more important, Ventilation or Intubation?
|
Ventilation - if you can't ventilate they die. If you can't intubate you can still ventilate until you wake or get a surgical airway.
|
|
|
A. List four devices for delivering supplemental oxygen to spontaneously-breathing (not intubated) patients. For each, give the approximate FiO2 or range of FiO2 that can be delivered by each: (8)
B. What device and corresponding FIO2 would you select for a 60 year old obese patient with severe COPD, a known CO2 retainer, who has presented to the Emergency Department with acute bronchitis, and whose PaO2 is 48 (normally 55) and PaCO2 is 65 (previously 50)? His lips and nail beds are blue-tinged. (2 marks): |
A. Nasal Prongs =24-44%, face mask=40-60%, mask with reservoir=60-80%, Venturi 24, 28, 31, 35, 40%
B. Venturi 24% |
|
|
What is the standard medication to use in wide QRS (>0.12sec) tachycardia with pulses?
|
Amiodarone 150mg IV over 10 minutes. If Torsades de Pointes give 1-2 mg magnesium over 30 min.
|
|
|
A 50 kg male has been NPO for 12 hours prior to a 3 hour laparatomy. He lost 300cc of blood. Calculate fluid requirements.
|
12h NPO = 4:2:1 = 90cc/h x 12 = 1080
3h Surgery Maint. = 90cc/h x 3 = 270 Losses @ 3:1 = 900cc Third space loss (Medium surgery) = 6cc/kg/h = 6 x 50 x 3 = 900cc Total = 3150 of Ringers (or NS). Note: Third space loss calculation Small surg (nose, foot, hand) = 4cc/kg/h Med. Surg (laparotomy, bowel resec, c-sec) = 6cc/kg/h BIG = 8cc/kg/h (AAA, cardiac, thoracic, transplant). |
|
|
How do you calculate third space losses for surgical procedures?
|
Note: Third space loss calculation
Small surg (nose, foot, hand) = 4cc/kg/h Med. Surg (laparotomy, bowel resec, c-sec) = 6cc/kg/h BIG = 8cc/kg/h (AAA, cardiac, thoracic, transplant). |
|
|
Laryngospasm
1. Etiology 2. When does it most commonly occur? 3. Complications 4. . Tx |
1. induced by secretions, inadequate anestheisa, anaphylaxis and airway manipulation.
2. Most commonly occurs in a patient who is going into or out of paralysis during intubation or extubation. 3. Results in inability to ventilate a patient = EMERGENCY. 4. Succinylcholine to stop spasm, then ETT. |
|
|
Laryngeal Mask (LMA)
1. When to use 2. Sizing 3. Contraindications |
1. a. Great for can't intubate/ventillate.
b. When not using a paralytic. c. Short procedure. d. Breathing spontaneously. 2. Women = Size 3, Men = Size 4. 3. Succinylcholine, Sevoflurane. Full stomach, preganant, ascites, reflux. |
|
|
DDx of Hypertension Intraoperatively. Give 10.
|
Pain, hypoxia, drugs (epi, phenyl, atropine, dopamine), fluid overload, electrolytes (Ca+) Pheochromo, Thyroid storm, Malignant Hyper, Machine not working (art line too low, wrong size BP cuff).
|
|
|
DDx of High Airway pressure with ventilation. Give 10.
|
Kink/Fluid in tubes, Kink in ETT, secretion/tissue in ETT, ETT placed down Left bronchus, PTX, trendelenberg, obesity, ascites, surgeon leaning on patient, bronchospasm.
|
|
|
Bronchospasm
1. Etiology 2. Clinical signs 3. Complications 4. Management |
Bronchospasm or a bronchial spasm is a sudden constriction of the muscles in the walls of the bronchioles. Often occurs at the induction stage before patient is fully anesthetized. It is caused by the release (degranulation) of substances from mast cells or basophils under the influence of anaphylatoxins. Asthma, chronic bronchitis, anaphylaxis, pilocarpine (which is used to treat illness resulting from the ingestion of deadly nightshade as well as other things) and beta blockers
2. Prolonged expiratory phase, wheeze, hypoxia, increased airway pressures, silent chest, upslopping CO2 tracing with ventilation. 3. Hypoxia, unable to venilate, hypercarbia, resp acidosis, CV collapse. 4. Atropine, increase inhalation anesthetic (bronchodilator), Induction (propofol) for Status athmaticus, salbutamol & Ipratoprium bromide by MDI, Prednisone, |
|
|
1. An elderly male with pain in his left hip is scheduled for a hip arthroplasty. He requests to have a spinal anesthetic. All are potential complications of a spinal anesthetic EXCEPT:
Hypotension Infection at site Hematoma at site Local anesthetic toxicity Nausea & Vomiting |
Nausea & Vomiting
|
|
|
2. All of the following are contraindications to spinal anesthesia EXCEPT:
Raised intracranial pressure Hypovolemia Coagulopathy Infection at site of needle insertion Kyphosis |
Kyphosis
|
|
|
3. A 24 week pregnant woman is in need of an emergency appendectomy. All are physiologic changes in pregnancy EXCEPT:
Decreased gastroesophageal sphincter tone Decreased haemoglobin Decreased coagulation factors Decreased functional residual capacity Decreased systemic vascular resistance |
Decreased coagulation factors
|
|
|
What is the name of the curved laryngoscope blade? Straight?
|
Macintosh is curved, Miller is straight
|
|
|
Name important measurements and classification systems in the assessment of an airway?
|
Mallampati Score, weight, head and neck movements, mouth opening, thyromental distance, jaw subluxation
|
|
|
How long prior to surgery is a patient able to consume clear fluids?
|
2 hours
|
|
|
A patient who is a smoker, is obese or has controlled Type 2 diabetes is considered which ASA class?
|
2
|
|
|
What length of time must a patient wait post MI before undergoing elective surgery?
|
4-6 weeks
|
|
|
When is an ECG indicated prior to surgery?
|
Heart disease, hypertension, diabetes, other risk factors for cardiac disease (may include age), subarachnoid hemorrhage, CVA, head trauma
|
|
|
Define MAC
|
The minimum alveolar concentration of an inhalational anesthetic agent is the concentration that prevents movement in response to standard surgical stimulus (incision) in 50% of patients
|
|
|
What is the proper positioning of patients during intubation?
|
The sniffing position: head bowed forward, nose in the air
|
|
|
What is the proper depth of endotracheal tube placement?
|
The tip 2 cm above the carina, the cuff 2 cm below the vocal cords
|
|
|
What medications can be given through the ET tube?
|
Naloxone, atropine, ventolin, epinephrine, lidocaine
|
|
|
What are some signs of an esophageal intubation?
|
ETCO2 zero or near zero, poor breath sounds on auscultation, impaired chest excursion, hypoxia
|
|
|
At what SaO2 can cyanosis be detected?
|
SaO2 = 80%
|
|
|
How do you calculate the fluid maintenance requirements in an adult?
|
4 mL/kg/hour for the first 10 kg, 2 ml/kg/hour for the second 10 kg, 1 ml/kg/hour for the remaining weight
|
|
|
What replacement ratio must be used when using crystalloid to replace blood loss? Colloid?
|
3 mL crystalloid / 1 ml blood loss, 1 ml colloid / 1 mL blood loss
|
|
|
Which anesthetic drugs can trigger Malignant Hyperthermia crisis?
|
Enflurane, halothane, isoflurane, desflurane, sevoflurane (end in –ane), succinylcholine, decamethonium
|
|
|
All of the following are contraindications to
spinal anesthesia EXCEPT: a) Raised intracranial pressure b) Hypovolemia c) Coagulopathy d) Infection at site of needle insertion e) Kyphosis |
e) Kyphosis
|
|
|
An elderly male with pain in his left hip is scheduled for a hip arthroplasty. He requests to have a spinal anesthetic. All are potential complications of a spinal anesthetic EXCEPT:
a) Hypotension b) Infection at site c) Hematoma at site d) Local anesthetic toxicity e) Nausea & Vomiting |
e) Nausea & Vomiting
|
|
|
A 24 week pregnant woman is in need of an emergency appendectomy. All are physiologic changes in pregnancy EXCEPT:
a) Decreased gastroesophageal sphincter tone b) Decreased haemoglobin c) Decreased coagulation factors d) Decreased Functional Residual Capacity e) Decreased Systemic Vascular Resistance |
c) Decreased coagulation factors
|

