![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
98 Cards in this Set
- Front
- Back
|
mechanisms of defense against germs
|
* include the skin; the moist mucous membrane lining of the respiratory, digestive, reproductive, and urinary tracts; the blood-clotting mechanism, white cells, and other substances in the blood; the thymus gland in the chest; and small lymph nodes or glands spread all over the body.
* Together, they form the body's immune defense system |
|
|
lymphadenitis
|
* swelling and tenderness of lymph nodes or tissues due to the accumulation of lymph
|
|
|
interstitial fluid
|
* aka. tissue fluid
|
|
|
cisterna chyli
|
* the storage area for lymph moving into the venous system
* an enlarged pouchlike structure in the thoracic duct in the abdomen |
|
|
lymphangitis
|
* inflammation of the lymphatic vessels
* characterized by thin, red streaks extending from an infected region * the infectious agent that causes lymphangitis may eventually spread to the bloodstream, causing septicemia (blood poisoning) and possibly death from septic shock. |
|
|
lacteals
|
* lymphatic capillaries in the wall of the small intestine
* they transport fats obtained from food to the bloodstream |
|
|
lymphatic system
|
* is not a closed system of vessels like the circulatory system. Instead, lymph fluid flows through the lymphatic vessels and eventually empties into the circulatory system.
* characterized by structural components, the lymphatic organs, and by a functional group of defensive cells and molecules that protect us from infection and disease. * lymph circulation relies on the valves in the vessel walls, skeletal muscle action, and respiratory movements. lymphatic system has three primary functions 1. Returns excess interstitial fluid to the blood. 2. Absorbs fats and fat-soluble vitamins from the digestive system and transports them to the venous circulation. 3. Serves as a defense mechanism against invading organisms and disease. |
|
|
lymph
|
* fluid similar to blood plasma. NO platelets in lymph
* clear fluid composed of water, electrolytes, waste from metabolizing cells, and some protein from the systemic circulation; all of which are present in blood plasma and tissue fluid * many additional substances that cannot enter or return through the capillary walls, including excess fluid and protein molecules are returned to the blood as lymph * formed in the tissue spaces that is transported by way of lymphatic vessels * formed from the blood plasma and tissue fluid during capillary exchange and eventually returns to the blood as part of the venous flow. * does not rely on the heart to pump it through the system so if flows much slower than blood * moves through the vessels according to pressure gradients, skeletal muscle action, respiratory movements, and the contraction of smooth muscle and valves in vessel walls. |
|
|
lymphatic vessels
|
* formed when lymph capillaries merge to form the vessels that carry fluid away from the tissues.
* help maintain fluid balance * similar to veins but have thinner walls and have more valves lining the inside of them, and have nodes located at certain intervals along their course. * movement of lymph in lymphatic vessels is one way, and does not form a circular route. * often have a beaded appearance caused by the presence of valves that assist in maintaining a one-way flow of lymph * smaller lymphatic vessels continue to merge into larger and larger lymphatic vessels until they merge into the two main ducts and empty into these two ducts: 1. right lymphatic duct 2. thoracic duct * these ducts eventually empty into the right and left subclavian veins in the circulatory system where lymph fluid is added to the blood flowing to the heart |
|
|
Lymph Nodes
|
* small bean-shaped structures approximately 2.5 cm in length, can be as small as a pin head or the size of a lima bean
* located along lymphatic vessels in clusters and groups, except in the nervous system, * Superficial nodes can be felt, or palpated, in the groin, axilla (armpit), and neck * are lymphoid organs because they contain lymphoid tissue * biological filtration * lymph is filtered and detoxified here and then exits through one efferent lymph vessel to continue its journey to the heart * filtered so that bacteria, cancer cells, and damaged tissue cells are removed and prevented from entering the blood and circulating all over the body. * An outer shell of dense tissue known as the fibrous capsule protects each lymph node. Within the node are compact clusters of lymphocytes called lymph nodules, which form the main structure of the node * lymph enters by way of the afferent lymphatic vessels where it "percolates" slowly through sinuses that surround nodules found in the outer (cortex) and inner (medullary) areas of the node. perform two main functions: 1. defense 2. white blood cell formation |
|
|
fibrous capsule
|
* An outer shell of dense tissue that protects each lymph node
|
|
|
lymph nodules
|
* located within the lymph node are compact clusters of lymphocytes called lymph nodules
* form the main structure of the node. |
|
|
afferent lymph vessels
|
* where lymph enters (several afferent lymph vessels) the lymph node through to be filtered and detoxified
* there are 4 afferent vessels |
|
|
efferent lymph vessel
|
* where lymph exits from the lymph node before moving on to the heart
|
|
|
inguinal lymph nodes
|
* located in the groin
* drain lymph from the leg and external genitals |
|
|
lymphatic capillaries
|
* after digestion, lacteals take part in the absorption of fats and other nutrients to produce a milky lymph called "chyle"
* very similar to blood capillaries in that they both are microscopic, both are formed from sheets consisting of a cell layer of simple squamous epithelium called endothelium. * the flattened endothelial cells forming lymphatic capillaries is not as tight as the fit with blood capillaries; as a result they are more porous and allow larger molecules, including proteins and other substances, as well as the fluid itself to enter the vessel and eventually return to the general circulation. * after lymph flows through the lymphatic capillaries it next moves into successively larger and larger vessels called lymphatic venules and veins eventually into two terminal vessels; the right lymphatic duct and the thoracic duct, which empty their lymph into the blood in veins into the neck region. |
|
|
Thymus or thymus gland
|
* a primary organ of the lymphatic system that is located in the mediastinum, behind the sternum and below the thyroid gland, extending upward in the mid-line of the neck
* composed of lymphocytes in a meshlike framework * plays an critical role in the development of the vital immune system before and immediately after birth * It serves as the final site of lymphocyte development before birth, and soon after birth, it begins secreting a group of hormones known as thymosin * T cells are white blood cells that mature in the thymus * the fetal bone marrow forms immature lymphocytes, which then move to the thymus for further maturation * The thymus begins to atrophy, or deteriorate, after puberty until it is largely replaced by fat and connective tissue in the older adult; a process called involution. by age 60 the thymus is half its maximum size and is virtually gone by age 80. * secretes thymosin which turns into T cells * largest in a child at about 2 years of age. * weighs approximately 35g to 40g * active, natural - contract disease and produce memory cells * active, artificial - receive a vaccination and produce memory cells * passive, natural - receive maternal antibodies through placenta or mother's milk * passive, artificial - receive antiserum with antibodies from another host (individual's immune system) |
|
|
thymosin
|
* a group of hormones that is secreted from the thymus
* allows lymphocytes to develop into mature T cells, which attack foreign and abnormal cells and regulate many immune functions |
|
|
mediastinum
|
* a subdivision in the midportion of the thoracic cavity
|
|
|
T cells
|
* developed from lymphocytes, white blood cells that mature (develop) in the thymus gland. main cell in cell-mediated immunity
* after they become T cells they go on to produce cell-mediated immunity, which is a resistance to disease organisms that results from the actions of cells - chiefly sensitized T cells by attacking an invading pathogen (antigen) * Embedded in each T cell's cytoplasmic membrane are protein molecules in a lock-key configuration that respond to only one specific kind of antigen molecule. * When a T cell comes into contact with its specific antigen, the antigen binds to the protein on the T cell's surface, changing it into an activated T cell. * produce effector cells along with memory cells * effector T cells actively engage in immune responses, whereas the memory T cells do not. * some activated T cells kill infected cells and tumor cells directly * moves to the site of the antigen and releases cell poison * release a substance that attracts macrophages * mediates the contact dermatitis allergic response Activated T cells produce clones of: * Killer T cells, which directly destroy the invading antigen * Helper T cells, which secrete substances to stimulate B cells and other T cells * Suppressor T cells, which inhibit T and B cells when the antigen has been destroyed * Memory T cells, which stimulate a rapid, intense response to future repeated exposures * During fetal development, the bone marrow releases immature lymphocytes into the blood. About one half of these cells migrate to the thymus gland, where they mature and become T cells. Eventually, the circulatory system carries T cells away from the thymus gland to various lymphoid tissues and nodes T cell activity: 1. ingestion of antigen macrophage 2. macrophage presents antigen to T cell 3. binding of antigen to proteins on the surface of T cells 4. T cell is activated 5. activated T cells produce clones 6. destruction of antigen |
|
|
Tonsils
|

* located in the mouth and back of the throat
* These masses of lymphoid tissue serve as a line of defense that protects us against outside microbes (bacteria) attempting to invade the body * a first line of defense * called tonsillitis when subject to chronic infection three types of tonsils: 1. palatine tonsils - are located on each side of the throat; usually removed during a tonsillectomy 2. pharyngeal tonsils (adenoids when they are swollen) - are near the posterior opening of the nasal cavity 3. lingual tonsils - are located at the base of the tongue |
|
|
Spleen
|
* located in the upper left hypochondriac region: below the diaphragm, above the left kidney and descending colon, and behind (lateral to) the stomach. protected by the lower ribs
* the largest of the lymphatic organs—shaped like an oversized lymph node—and is surrounded by a fibrous capsule * The spleen has a rich blood supply and may contain more than 500 ml (about 1 pint) of blood * it contains venous sinuses called red pulp, which store large numbers of red blood cells * areas of the spleen also contain white blood cells (lymphocytes), appropriately described as the white pulp * The spleen filters blood and removes microbes, utilizing phagocytosis to destroy the microbes it filters. * The spleen assists with hematopoiesis by allowing nongranular leukocytes to complete maturation * Aging RBCs and platelets are destroyed in the spleen, and the iron in the hemoglobin is stored for future use * the spleen serves as a valuable reservoir for blood to be used when needed * While the spleen is considered an important organ, it is not essential for life and can be removed by a splenectomy after injury or for disease conditions |
|
|
splenomegaly
|
* an abnormal spleen enlargement
* ie. infectious conditions such as scarlet fever, syphilis, and typhoid fever are characterized by splenomegaly. * sometimes accompanies hypertension, hemolytic anemia in which red blood cells appear to be broken apart at an abnormally fast rate * treatment: most often cured by spleen removal |
|
|
Disorders of the Lymphatic System
|
* usually the result of an obstruction to lymph flow, infection, or a tumor
a few lymphatic disorders: * Lymphedema: An accumulation of lymph distal to an obstruction in a lymph vessel causes it to swell. ie. after a mastectomy * Parasitic infections: While rare, these can be a cause of severe forms of lymphedema. An example of this type of infection is known as elephantiasis. * Lymphadenitis: Microbes transported in lymph from other areas of infection can cause acute infection of the lymph nodes. * Lymphomas: Malignant tumors of lymphoid tissue are classified as Hodgkin's or non-Hodgkin's lymphomas. * Tonsillitis: The position of the tonsils is vulnerable and subjects them to infection. * Splenomegaly: Abnormal spleen enlargement is observed in a variety of disorders. |
|
|
lymphoid tissue
|
* help defend the internal environment
* a mass of developing lymphocytes and related cells |
|
|
capillary beds
|
* where the exchange of substances between blood and tissue fluid occurs
|
|
|
lymph - process of formation:
|
1. blood plasma filters out of the capillaries into microscopic spaces between tissue cells because of the pressure generated by the pumping action of the heart.
2. its then called Interstitial fluid (liquid), or tissue fluid. much of this fluid goes back into the blood by the same route it came out (through the capillary membrane) 3. the remainder of the interstitial fluid enters the lymphatic system before it returns to the blood. 4. now the fluid is called lymph and it enters a network of tiny blind-ended tubes distributed in the tissue spaces. 5. these tiny vessels, called lymphatic capillaries, permit excess tissue fluid and some other substances such as dissolved protein molecules to leave the tissue spaces. 6. movement of lymph in lymphatic vessels is one way, and does not form a circular route. 7. the flattened endothelial cells forming lymphatic capillaries is not as tight as the fit with blood capillaries; as a result they are more porous and allow larger molecules, including proteins and other substances, as well as the fluid itself to enter the vessel and eventually return to the general circulation. 8. after lymph flows through the lymphatic capillaries it next moves into successively larger and larger vessels called lymphatic venules and veins eventually into two terminal vessels; the right lymphatic duct and the thoracic duct, which empty their lymph into the blood in veins int the neck region. |
|
|
thoracic duct
|
* lymph from about three fourths 3/4 of the body eventually drains here
* the largest lymphatic vessel in the body |
|
|
right lymphatic duct
|
* lymph from the right upper extremity and from the right side of the head, neck and upper torso flows or drains into here.
|
|
|
lymph ducts
|
* empty into the circulatory system by draining into the subclavian veins.
|
|
|
immune system
|
* the armed forces of the body, which stands ready to attack and defend us against enemy invaders
* the body's specific defense system, makes us able to resist threats to our health and survival. * in the lymphatic system: lymph nodes, tonsils, thymus and spleen * not just a small group of organs working together; it's an interactive network of many organs and billions of freely moving cells and trillions of free-floating molecules in many different areas of the body. It includes the structures and processes that defend us against: * Foreign bodies * Microorganisms * Transplanted tissue cells that are unfamiliar * Our own cells that have turned malignant two major categories of attack: 1. nonspecific immunity 2. specific immunity Primary cells of the immune system: 1. phagocytes a. neutrophils b. monocytes c. macrophages 2. lymphocytes a. T lymphocytes b. B lymphocytes |
|
|
Nonspecific immunity
|
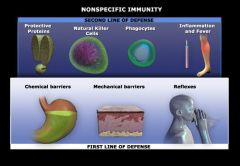
* aka. innate immunity, native immunity, genetic immunity
* Nonspecific defense mechanisms are directed against all pathogens and foreign substances that threaten the internal environment * rapid reaction; immediate up to several hours * provides general protection against irritants or substances that threaten the body and represents the first two lines of the body's defense * Nonspecific defense mechanisms work against all foreign agents and do not require recognition of a specific agent to provide protection functions: 1. Prevents the invader from spreading to nearby tissues. 2. Disposes of cellular debris. 3. Begins damage repair The first line of defense includes: * Mechanical barriers—skin and mucous membrane (prevent entry into the body by bacteria and many other substances such as toxins and harmful chemicals) * Chemical barriers—stomach acids and tears (tears wash harmful substances away) * Certain reflexes—sneezing second line of defense: * protective proteins * natural killer cells * phagocytes * inflammation and fever If pathogens penetrate the first line of defense, the second line of defense is called into action. * When foreign substances are detected, the immune system sends leukocytes to defend the body, which responds by initiating an inflammatory response. * Various types of leukocytes such as neutrophils and macrophages ingest and destroy the invaders by phagocytosis. also dendritic cells * As phagocytes destroy bacteria, they release pyrogens, producing a fever that is thought to stimulate phagocytosis and decrease the ability of the pathogen to multiply. * Protective proteins such as interferon and complement are excreted to boost the immune system and destroy bacteria. * Finally, natural killer cells, a special type of lymphocyte, act nonspecifically to kill targeted cells. |
|
|
Specific immunity
|
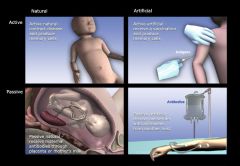
* aka. adaptive immunity, or acquired immunity
* considered the third line of defense * acts against specific substances and organisms * slower response to react; several hours to several days. * Specific immunity is designed to be selective. The characteristic unique to this defense mechanism is a memory, which is very important. * first exposure to an invading organism disease symptoms may occur. The components of the specific defense mechanism remembers the organism (antigen) and defends against the invader with a quicker response if it enters the body a second time. this information is stored in memory cells to be used for future exposures. This quick response prevents the person from experiencing symptoms the second time and provides a degree of immunity. * immunity to one type of disease-causing bacteria or virus does not protect the body against others. * classified as either "natural" or "artificial" depending on how the body is exposed to the harmful agent controlled by two classes of lymphocytes: 1. T cells 2. B cells includes: 1. Humoral—Also known as antibody-mediated immunity, this specific immunity involves B cell mechanisms. 2. Cell-mediated—This immunity involves T cell mechanisms. |
|
|
complement
|
* protective proteins normally present in an inactive state in the blood, which when activated kill foreign cells by dissolving them using phagocytosis and inflammation - process called complement cascade.
* classified as "natural" or "artificial" depending on how the body is exposed to pathogens and "active" or "passive" depending on the source of the immunity * excreted to boost the immune system and destroy bacteria in Nonspecific immunity * they are critical to immune system functions along with antibodies |
|
|
natural immunity
|
* acquired immunity, specific immunity
* exposure to the causative agent is not deliberate and occurs in the course of everyday living * may be "active" or "passive" |
|
|
antigen
|
* a substance that causes the formation of antibodies
* compounds whose molecules have small regions on their surfaces that are uniquely shaped to fit into the combining sites of a specific antibody molecule as precisely as a key fits into a specific lock. "lock-and-key" |
|
|
humoral (response)
|
* immunity is produced when antibodies render antigens (or change them so they are) unable to harm the body, by creating an antigen-antibody to make the antigen or cell harmless.
* An immediate allergic response or "immediate hypersensitivity reaction" is usually a humoral response that involves the release of antibodies by plasma cells in response to the invasion of allergens: * antibody-mediated immunity - this specific immunity involves B cell mechanisms. * most effective against bacteria, viruses that are outside body cells, and toxins * also involved in allergic reactions. |
|
|
antibodies
|
* protein compounds normally present in the body that contain combining sites on the molecular surface and destroy antigens.
* they are critical to immune system functions along with complements. * They produce humoral or antibody-mediated immunity by changing the invading antigen so that it can no longer harm the body. * Specific antibodies bind to specific antigens and form antigen-antibody complexes that produce a variety of changes to inactivate or kill the invading cells. * characteristics: uniquely shaped concave regions called combining sites on its surface, the ability of an antibody molecule to combine with a specific compound called an antigen. * function is promotion and enhancement of phagocytosis Antibodies act on antigens by: * Causing them to agglutinate - clumping which facilitates phagocytosis * Neutralizing their harmful toxins - inactivated * Making them susceptible to destruction by phagocytosis * releasing inflammatory chemicals |
|
|
inflammatory response
|
* Redness, swelling, heat, or pain may result at the site of inflammation due to increased blood flow and vascular permeability of the capillaries that surround the area (resulting in tissue swelling and the pain that it causes).
* a set of nonspecific reactions that occurs in the body as a result of invading pathogens. * second line of defense |
|
|
interferon
|
* a protective protein excreted to boost the immune system and destroy bacteria in Nonspecific immunity in response to a viral infection
|
|
|
natural killer cells
|
* The natural killer cells assist with nonspecific immunity to destroy microbes.
* These cells do not attack pathogens directly, but rather attack and destroy cells in the body that contain pathogens. * They are particularly effective in killing viruses. * Natural killer cells puncture the cell membrane of an infected cell, which allows water to flood the infected cell and rupture (lyse). |
|
|
Neutrophils
|
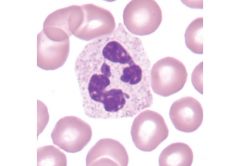
* circulate through the blood to assist the immune system
* phagocytic cells in the immune system * small leukocytes with fine granules—are often the first cells to leave the blood and travel to the site of infection. * They increase in number significantly during acute infections, but their value is short-lived because they die after ingesting only a few bacteria. * the pus found at some infection sites is mostly dead neutrophils |
|
|
macrophages
|
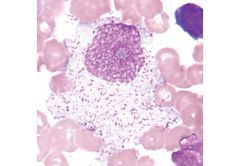
* are located in the tissues of the body and walls of blood vessels.
* phagocytic cells in the immune system * Macrophages usually take over defending the body after the neutrophils have died or during the latter stages of the infection. * They are also present in lymph nodes, where they cleanse the lymph of debris as it filters through the node. |
|
|
memory cells
|
* cells that "remember" the initial encounter with an antigen for future response
* When a subsequent exposure to a familiar antigen occurs, memory cells are transformed into plasma cells with the appropriate antibodies to destroy the pathogen quickly—often with few or no symptoms. * lay dormant in lymphatic tissue until the same antigen again enters the system; then very quickly they develop into plasma cells and secrete large amounts of antibody. * can secrete antibodies but do not immediately do so, only when activated |
|
|
Cell-mediated immunity
|
* This immunity involves T cell mechanisms, part of specific immunity.
* A delayed allergic response usually involves cell-mediated immunity. Onset is delayed approximately 48 hours, and T cells trigger events that lead to local skin inflammation. |
|
|
artificial immunity
|
* deliberate exposure to the potentially harmful agent or causative agent
* specific immunity, called immunization * may be "active" or "passive" |
|
|
types of immunity examples
|
natural passive - infant protection via mother's milk
natural immunity - exposure to the causative agent is not deliberate artificial passive - immunity obtained by injection of antibodies developed by another individual's immune system artificial active - immunity obtained by vaccination natural active - an individual develops a disease and acquires immunity to subsequent exposure to the same disease. artificial immunity - exposure to the causative agent is deliberate |
|
|
inflammatory chemicals
|
* release of these chemicals such as histamine causes inflammation, which causes blood vessels to dilate and increased numbers of phagocytes to flow to the injured site.
|
|
|
complement cascade
|
* One of the most important ways in which antibodies defend
* After being activated by antibodies, complement proteins begin a cascade reaction, which forms a highly specialized antigen-antibody complex and targets cells for destruction * Invading cells are destroyed when the antigen-antibody complex attaches to the plasma membrane and creates holes or doughnut-shaped protein rings * These holes allow sodium to enter the cell, and then water follows by osmosis * The cells rapidly begin to lyse as the internal osmotic pressure increases |
|
|
passive immunity
|
* lasts shorter time than active immunity
* specific immunity * results when immunity to a disease that has developed in another individual or animal is transferred to an individual who was not previously immune. * provides immediate protection but generally lasts shorter than active immunity |
|
|
active immunity
|
* lasts longer than passive immunity
* specific immunity * occurs when an individual's own immune system responds to a harmful agent, regardless of whether that agent was naturally or artificially encountered * generally lasts longer than passive immunity |
|
|
Immune system cells
|
* All immune system cells develop from primitive cells in the bone marrow called stem cells by going through specific stages of development
Primary cells: 1. phagocytes - contribute to immunity by ingesting and digesting foreign cells or particles. a. Neutrophils b. monocytes c. macrophages 2. lymphocytes - contribute to immunity by producing antibodies a. B cells b. T cells |
|
|
monocytes
|
* When monocytes leave the blood, they increase in size and are then referred to as macrophages
* develop into macrophages once in the tissues * phagocytic cells in the immune system |
|
|
plasma cells
|
* immune system structures that secrete copious (huge) amounts of antibodies into the blood.
* to 2000 antibody molecules per second by each plasma cell for every second of the few days that it lives. * "antibody factories" of the body |
|
|
lymphocytes
|
* most numerous immune cells
* are responsible for antibody production two main types: 1. B lymphocytes, referred to as B cells 2. T lymphocytes, referred to as T cells * Although both B cells and T cells originate from stem cells in the bone marrow, they differ significantly in their development, function, and type of immunity that they provide the body |
|
|
phagocytes
|
* immune system structures that ingest and digest bacteria
two most important types: 1. Neutrophils 2. Monocytes |
|
|
B cells
|
* immune system structures that function indirectly to produce humoral immunity. Meaning they do not directly assault the antigen
* first stage of B-cell development, transformation of stem cells into immature B cells, occurs in the liver and bone marrow before birth but only in the bone marrow in adults * first discovered in a bird organ called the bursa * produces antibodies * each B cell carries a different type of antibody; they enter the blood and are transported to their new home mostly by lymph nodes. * second stage of B-cell development changes an inactive B cell into an activated B cell. * activated B cells divide rapidly and repeatedly to form clones of memory cells and plasma cells. turn into: 1. plasma cells (or effector cells) 2. memory cells * When activated, B cells develop into plasma cells, which in turn secrete antigen-combating antibodies into the blood. * The circulating antibodies produce humoral immunity and then destroy specific pathogens (antigens). * B cells also form memory cells, which are stored in lymph nodes for future use B cell actions: 1. stem cell 2. inactive B cells 3. binding of antigen to antibody on surfaces of inactive B cells 4. activated B cells 5. formation of plasma cells and memory cells 6. antibodies |
|
|
stem cell
|
* cells taken from embryonic tissue, adult donors, or from the umbilical cord blood of newborn infants to conduct research in areas such as muscle, nerve, and organ replacement and regeneration.
* arise from primitive cells in the bone marrow |
|
|
Hypersensitivity
|
* an inappropriate or excessive response of the immune system.
* may be mild—such as itching or redness of the skin—or it may be quite severe. * When individuals experience severe hypersensitivity, it can manifest itself with multiple serious symptoms such as a critical drop in blood pressure, bronchoconstriction, and an irregular heart rate * There are three types: 1. Allergy 2. Autoimmunity 3. Isoimmunity |
|
|
allergen
|
* harmless environmental antigen that stimulates an allergic reaction in a susceptible, sensitized person.
* antigen that triggers an allergic response |
|
|
anaphylaxis or anaphylactic shock
|
* Severe hypersensitivity to an allergen
* results in circulatory failure (shock) * Healthcare workers have only minutes to reverse the process before death can occur. * usually treated with antihistamines |
|
|
antihistamines
|
* used to relieve symptoms of allergies
|
|
|
autoimmunity
|
* inappropriate response or excessive response to our own or self-antigen
* When the immune system is functioning properly, it correctly distinguishes its own body cells and chemicals from those that are foreign invaders. This ability prevents the immune system from initiating a self-destructive immune response * disorders that result from auto immune responses are called autoimmune diseases |
|
|
isoimmunity
|
* an excessive reaction of the immune system to antigens from a different individual of the same species
* It occurs most frequently during pregnancies and tissue or organ transplants * Erythroblastosis fetalis is the result of antibodies formed by the mother during pregnancy entering the fetal bloodstream and causing an inappropriate immune reaction * Tissue or organ transplants from donors often cause a rejection syndrome, whereby the immune system attacks foreign antigens present in the tissue or organ of the donor. Two successful ways known to prevent this reaction are tissue typing and immunosuppressive drugs. |
|
|
allergy
|
* hypersensitivity to harmless environmental antigens which become allergens when they stimulate an allergic response
* When a sensitized person reacts to an allergen, plasma cells secrete a type of antibody called IgE in response to the specific antigen. * IgE antibodies come in contact with mast cells, which have receptors for them. * IgE antibodies bind to the mast cell, causing it to release substances such as histamine that stimulate local or systemic inflammation and irritation. * antigen-antibody reactions occur as a result of a susceptible person being exposed to an allergen repeatedly - triggering the production of antibodies; than a person becomes sensitized. * symptoms: runny nose, conjunctivitis and urticaria or hives. may cause constriction of the airways, relaxation of blood vessels, and irregular heart rhythms. ie. ragweed, venom from insects, some medications, and certain foods allergic response order: 1. allergen activates B cell 2. Activated B cell forms a clone with anti-body secreting plasma cell 3. plasma cell secretes IgE antibodies against the allergen 4. IgE antibodies bind to mast cells in the body tissues 5. the mast cells release chemicals that cause inflammation and t. |
|
|
mast cells
|
* cells that release substances in response to injury and infection. these cells have receptors for IgE and store substances such as histamine that cause inflammation and irritation.
|
|
|
autoimmune diseases
|
* In certain individuals, immune cells sometimes lose their ability to differentiate between foreign antigens and self-antigens. As a result, immunity mechanisms are activated against self cells and phagocytes may begin to attack healthy cells.
* Diseases that develop in response to self-attack are called autoimmune diseases. * acquired after birth and is not related to genetic defects. ie. Rheumatoid arthritis, myasthenia gravis, systemic lupus erythematosus (SLE) and some forms of diabetes mellitus are just a few of the diseases that we classify as autoimmune diseases |
|
|
Immune System Deficiency or immunodeficiency
|
* the failure of the immune system mechanisms to successfully defend against pathogens
two major categories: 1. Congenital immune deficiency, which results from improper lymphocyte development before birth 2. Acquired immune deficiency, which develops after birth and is not related to genetic defects. One of the best examples of acquired immune deficiency is acquired immunodeficiency syndrome (AIDS). |
|
|
grafts
|
* or tissue transplants
* often done to repair damage caused by burns |
|
|
immunosuppressive drugs
|
* suppress the immune system's ability to attack the foreign antigen and are used when the patient demonstrates a rejection syndrome.
* suppressing an immune system for someone who already has an acquired immune deficiency syndrome would be inappropriate |
|
|
retrovirus
|
* viral DNA often becomes part of the cell's DNA
ie. HIV is a retrovirus |
|
|
host-versus-graft rejection
|
* results when the recipient's immune system recognizes foreign antigens and attacks them destroying the donated tissue.
|
|
|
graft-versus-host rejection
|
* results when the donated tissue attacks the recipient's antigens, destroying tissue throughout the body.
* most severe, may lead to death |
|
|
HIV
|
* after being infected symptoms may not appear for months
* attacks several types of cells, although it has its most obvious effects in a certain type of T cell called a CD4 T cell. * mutates so development of a vaccine is difficult * Norvir is an AIDS inhibitor medication - blocks HIV's ability to reproduce within infected cells * pneumocystosis is a common infection among AIDS patients - a secondary condition to HIV |
|
|
severe combined immune deficiency (SCID)
|
* a congenital immune deficiency in which both humoral and cellular immunity are defective
* involves disruption of stem cell development before birth |
|
|
PSA or prostate-specific antigen
|
* a test that screens for prostate cancer
|
|
|
human lymphocyte antigens or HLAs
|
* most commonly involved in transplant rejection
* the immune system sometimes reacts against antigens (HLAs) presented in grafted tissue causing a rejection syndrome |
|
|
lymphedema
|
* an abnormal condition in which tissues exhibit swelling (edema) because of the accumulation of lymph
* lymph may accumulate in tissue when the lymphatic vessels are partially blocked * may result from a congenital abnormality or a specific injury or blockage of lymphatic drainage * may also result from lymphangitis * rarely it may be caused by small parasitic worms that infest the lymphatic vessels; when this type of infestation blocks the flow of lymph, edema of the tissues drained by the affected vessels occurs. * cancer of the breast is one of the most common forms of this disease in women. |
|
|
elephantiasis
|
* literally "condition of being like an elephant"
* caused by severe cases of lymphedema |
|
|
biological filtration
|
* a process in which cells (phagocytic cells in the case of lymph nodes) alter the contents of the filtered fluid
* biological filtering of bacteria by phagocytosis prevents local infections from spreading |
|
|
lymphangiogram
|
* an x-ray image where a special dye is injected into the soft tissues that drain the part of the lymphatic network
|
|
|
Lymphoma
|
* refers to lymphatic tumors; most often malignant but in rare cases can be benign
* characterized by painless enlargements of the lymph nodes in the neck and other regions, followed by anemia, weight loss, weakness, fever, and spread to other lymphatic tissues * later stages it spreads to many other areas of the body * early detection can be successfully treated with intensive radiation and chemotherapy * occurs more often in men than in women. two major categories: 1. Hodgkin's lymphoma 2. Non-Hodgkin's lymphoma |
|
|
monoclonal antibodies
|
* specific antibodies produced or derived from a population or culture of identical, or monoclonal cells
* with monoclonal antibody techniques, lymphocytes that are produced by the body after the injection of a specific antigen are "harvested" and then "fused" with other cells that have been transformed to grow and divide indefinitely in a tissue culture medium called hybridomas. * hybridomas continue to produce the same antibody produced by the original lymphocyte. * used in over-the-counter pregnancy test kits to trigger the action producing a color change |
|
|
hybridomas
|
* fused hybrid cells formed by lymphocytes that are produced by the body after the injection of a specific antigen are "harvested" and then "fused" with other cells that have been transformed to grow and divide indefinitely in a tissue culture medium.
|
|
|
complement-binding site
|
* when antigens that are molecules on an antigenic or foreign cell's surface combine with antibody molecules, they change the shape of the antibody molecule slightly, just enough to expose two previously hidden regions called complement-binding sites.
* this exposure initiates a series of events that eventually kill the cell |
|
|
dendritic cell (DC)
|
* a type of phagocytic cell
* highly branched (dendrite "branch") cells are produced in bone marrow and are released into the bloodstream. * some remain in the blood but many migrate to tissues in contact with the external environment - the skin, respiratory lining, digestive lining |
|
|
antigen-presenting cells (APCs)
|
* made from macrophages and dendritic cells (DCs)
* they ingest a cell or particle, remove its antigens, and display some of them on their cell surfaces. * the displayed antigens can then be presented to other immune cells to trigger additional, specific immune responses. |
|
|
clone
|
* a family of many identical cells, all descended from one cell
|
|
|
cytotoxic T cells
|
* when bound to antigens these cells release a substance that acts as a specific and lethal poison against the abnormal cell.
* kill infected cells and tumor cells directly |
|
|
regulatory T cells
|
* activated regulatory T cells help shut down an immune reaction after the antigens have been destroyed
* also help prevent inappropriate immune reactions. |
|
|
contact dermatitis
|
* a delayed allergic response involved with cell-mediated immunity
* ie. T cells trigger events that lead to local skin inflammation a few hours or days after initial exposure to an antigen such as poison ivy, soaps, and cosmetics. * hypersensitive individuals may use hypoallergenic products (products without common allergens) to avoid such allergic reactions. |
|
|
self-antigens
|
* o that are native to a person's body and that are used by the immune system to identify components of "self"
* can also be segments of a person's genetic material (DNA or RNA) or certain proteins or other chemicals made in the body * in autoimmunity, the immune system inappropriately attacks self-antigens |
|
|
lupus or systemic lupus erythematosus (SLE)
|
* chronic inflammatory disease that affects many tissues in the body: joints, blood vessels, kidneys, nervous system, and skin
* an autoimmune disease * the name refers to a red rash that often develops on the face * results from the production of antibodies against many different self-antigens |
|
|
rejection syndrome
|
* can occur after a transplant
* when the immune system sometimes reacts against foreign antigens present in the grafted tissue occurs in two ways: 1. host-verses-graft rejection 2. graft-verses-host rejection - most severe two ways to prevent rejection syndrome: 1. tissue typing - identify HLAs and other antigens of donor and recipient 2. immunosuppressive drugs - such as cyclosporine and prednisone suppress the immune system's ability to attack the foreign antigens in the donated tissue. |
|
|
vaccine
|
* literally means "cow substance" - cowpox virus
* active, artificial |
|
|
perinatal infection
|
* an infection passing from mother to infant during birth.
|
|
|
gamma globulin
|
* a class of plasma protein composed almost entirely of immunoglobulin proteins that function as antibodies.
|
|
|
complement fixation
|
* kills target cells by drilling holes in their plasma membrane, which disrupts the sodium and water balance
* inflammation is a consequence of complement fixation |

