![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
100 Cards in this Set
- Front
- Back
|
What cells produce Growth hormone and where are they located?
|
Somatotrophs in the anterior pituitary
|
|
|
Does growth hormone act on target cells directly?
|
Yes
|
|
|
What organ does Growth Hormone to stimulate?
What does that organ produce. |
The Pancreas which produces Insulin-like Growth Factors 1 and 2
|
|
|
What causes the release of Growth Hormone?
|
The anterior pituitary receives the signal from the hypothalamus in the form of Growth Hormone Releasing hormone (GHRH)
|
|
|
What hormone inhibits GH?
|
Somatostatsin
|
|
|
Where is somatostasin produces and what does it counterbalance?
|
In the periventricular region of the hypothalamus.
It counter balances GHRH |
|
|
What type of pattern is GH release?
|
Pulsatile
|
|
|
When is the frequency at its highest for GH release?
|
During slow wave (Non REM) cycle of sleep
|
|
|
What are 2 other names for the Non REM cycle?
What happens during this portion of sleep? |
Restorative Sleep and Delta sleep
THe body repairs and stores tissues. "If this party of sleep is missed it gives the greatest feeling of not being well rested." |
|
|
What two aspects of Growth Hormone release are increased during Non REM sleep?
|
Both frequency and amplitude of GH concentration increases.
|
|
|
What is the predominant direct effect of GH?
|
To RAISE blood glucose by decreasing the uptake of glucose by tissue types in the body like muscles, fat and the liver.
|
|
|
How does GH act on the liver to increase blood glucose? (2 ways)
|
It stimulates glucose production by promoting the breakdown of glycogen.
It also produces new glucose by gluconeogenesis. |
|
|
How does Growth Hormone act INDIRECTLY in the body?
|
Through the regulation of the release of 2 more hormones. IGF 1 and 2
|
|
|
What are the cells called that produce IGFs 1 and 2?
|
Somatomedins in the LIver
|
|
|
Why were the hormones IGFs 1 and 2 named "insulin-like growth factors?"
|
Because they act like insulin to reduce glucose levels in the blood.
|
|
|
What are the general effects of IGFs on the body?
|
-They increase production of visceral tissue.
-They increase production of lean body mass (skeletal tissue) -They increase the linear growth of long bones. |
|
|
How does GH's direct and indirect effects contradict?
|
Direct actions are to increase blood glucose levels.
Indirect actions cause a decrease in blood glucose level through IGFs. |
|
|
What effect does GH, IGF-1 and IGF-2 have on the anterior pituitary?
|
All three provide negative feedback regulation on the Anterior Pituitary.
|
|
|
Where is the Thyroid gland located and what is its shape?
|
Sits at the base of the neck and shaped like a bow tie.
Composed of 2 lobes with a connecting piece. |
|
|
What comprises the functional unit of the Thyroid Gland?
|
Follicular cells and follicles
|
|
|
What cells synthesize Thyroid Hormone?
|
Follicular cells
|
|
|
Describe the functional unit of the thyroid hormone.
|
Follicles.
Lobes of endocrine cells that are surrounding an acellular material. The center of the lobe holds the colloid material. |
|
|
What surrounds the follicular cells of the thyroid gland?
|
Capillaries!
The follicles are highly vascularized. |
|
|
What is the function of the colloid?
|
Stores thyroid hormones in the midst of a proteinous matrix.
|
|
|
What is thyroid hormone composed of?
|
Tyrosine an Iodine
|
|
|
What component of thyroid hormone cannot be produced in the body?
|
Iodine.
We only get it through our food: SALT!! |
|
|
How does iodine enter the follicular cell? The colloid?
|
Iodine is actively pumped into the follicle.
Once inside it moves directly/passively into the colloid. |
|
|
What is tyrosine attached to in the first stages of TH production?
|
THYROGLOBULIN
|
|
|
How does tyrosine get into the colloid?
|
exocytosis
|
|
|
How is tyrosine attached to iodine and where does this happen?
|
Iodine attaches to THYROGLOBULIN, which houses the tyrosine.
It takes place in the colloid. |
|
|
Why does iodine stay attached to they thyroglobulin inside the colloid?
|
So that it will not diffuse out prematurely.
|
|
|
What signals for T3 and T4 to be released?
|
The thyroid will receive a signal from TSH, which binds to a TSH receptor on the thyroid follicular cell.
|
|
|
When TSH attaches to receptors on follicular cells, what is the first response?
|
The follicular cell will start to endocytose a chunk of the colloid matrix which houses the big TGB proteins.
|
|
|
How does the follicular cell free up the endocytosed TGB in the vesicles?
|
It fuses the vesicles with lysosomes which break the peptide bonds and liberates the contents including T3 and T4
|
|
|
How does T3 and T4 released from the vesicle get out of the follicular cell?
|
T3 and T4 are lipid soluble and they simply float across the membrane.
|
|
|
Explain to overall production of TH.
|

|
|
|
Give 2 examples of conditions that stimulate the release of or inhibit T3 and T4
|
-When infants feel cold they increase their amounts of T4 and T3
-Chronic stress will inhibit the production of T3 and T4 |
|
|
What enzyme must a target tissue have to use T4 or T3?
|
monoiodinase
|
|
|
Where is the T3 receptor in the cell?
|
It is a nuclear receptor that sits on the promoter region of gene.
|
|
|
Name some examples of proteins created from T3 acting on the gene.
|
-Na/K ATPase pumps
-Gluconeogenic enzymes: -Respiratory enzymes (those in aerobic metabolism) -B adrenergic enzymes -Enhances hepatic glucose production -The breakdown of stored fat and muscle tissue -Metabolic related enzymes and structural proteins -It is PRIMARY determinant of basal metabolic rate |
|
|
What hormone is the primary determinant of basal metabolic rate?
|
Thyroid Hormone (T4 and T3)
|
|
|
Where is Thyroid Hormone absolutely critical?
|
Fetal development
|
|
|
What condition occurs as a result of thyroid hormone deficiency?
|
Cretinism: mental retardation, growth delays, short stature, protuberant abdomen, coarse hair, many structural abnormalities and developmental delays
Iodine deficiency in pregnancy. |
|
|
Where are the adrenal glands located?
|
On top of the kidneys
|
|
|
What is the outer layer of the adrenal gland called?
What type of hormones does it produce? |
Adrenal Cortex
Steroid Hormone |
|
|
What is the outermost layer of the adrenal cortex called?
|
Zona Glomerulosa
|
|
|
Where is the Zona Fasciculate?
|
The middle layer of the Adrenal Cortex
|
|
|
What is the innermost layer of the Adrenal cortex called?
|
Zona Reticularis
|
|
|
What are the sex hormones and how much of them are produced in the cortex?
|
Testosterone, estrogen, progesteron and different intermediates in the production of these sex hormones
-Only a very small amount is made in the cortex |
|
|
Where are glucocorticoids made?
|
In the cortex
|
|
|
What is the primary glucocorticoid?
|
Cortisol, and similar in structure is Cortisone
|
|
|
What pattern does cortisol follow for activation?
|
It follows a diurnal pattern
|
|
|
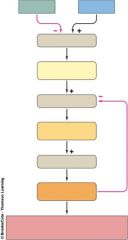
How is cortisol released?
|
Increases in production of CRH to act on the AP to release ACTH to act on the cortex to release cortisol.
|
|
|
Where does high levels of cortisol place negative feedback?
|
On the hypothalamus and the anterior pituitary
|
|
|
What is a second condition that causes the release of cortisol?
|
Stress
|
|
|
What affect does cortisol have that can be useful in a stress response?
|
Increase blood glucose
|
|
|
How does cortisol raise blood sugar?
|
-Reduces uptake of glucose by the cells
-Decrease uptake of glucose by insulin sensitive tissues -Antagonizes insulin receptors -Acts on the liver to stimulate the production of glucose (gluconeogenesis) -Can break down muscle INHIBITS UPTAKE AND STIMULATES THE LIVER |
|
|
What regions of the body does cortisol not break down subcutaneous fat?
|
Face and abdomen
|
|
|
What is Cushion Syndrome?
|
High levels of cortisol
-See moon face a lot of fat on the waist, less on the arms and legs |
|
|
What effects does cortisol have on bone?
|
-Interferes with the laying down of new bone
-Interferes with absorption of Ca in GI tract -Excess levels can demineralize and weaken bones and cause osteoporosis like conditions. |
|
|
What effect does cortisol have on NE?
|
It helps to set baseline vascular tone so NE can regulate after that.
|
|
|
How does cortisol effect the immune system?
|
It acts as an immuno suppressant and a potent anti-imflammatory
|
|
|
What is Cushing?
|
giving high doses of cortisol
|
|
|
How does cortisol effect the CNS?
|
In appropriate levels it enhances mental acuity. If the levels get to high it can turn acuity to agitation and limited mental acuity.
|
|
|
what is the primary mineralcorticoid?
|
Aldosterone
|
|
|
Why did mineralcorticoids get their name?
|
Named after their effects on sodium and potassium levels
|
|
|
Where is aldosterone produced?
|
Only one place, Zona Glomerulosa!
|
|
|
What is the effect of aldosterone?
|
Tends to increase sodium levels and decrease potassium levels.
|
|
|
Where is aldosterone's site of action?
|
In the kidneys for renal excretion.
|
|
|
What does the adrenal medulla secrete>?
|
Catecholamines
|
|
|
What is the exocrine function of the pancreas?
|
Produces digestive enzymes and releases them on the surface of the duodenum (SI)
|
|
|
What is the endocrine function of the pancreas?
|
to produce 2 hormones, insulin and glucagon.
|
|
|
Where does the endocrine portion of the pancreas take place?
|
Islets of Langerhans
|
|
|
Which cells secrete glucagon and what is its function?
|
Alpha Cells
-Antagonistic to insulin -Maintain the blood glucose level during a fasting state |
|
|
Where is insulin produced and what is its function?
|
Beta Cells
-Antagonistic to glucagon -Released at an onset of a meal and when blood glucose starts to rise. -Known as the absorptive state |
|
|
What happens to insulin during fasting?
|
We stop producing insulin and we are not taking in glucose
|
|
|
What do the delta cells secrete?
|
Somatostatin
|
|
|
What is the safe range of Ca++ in the ECF?
|
6.6-10.6
|
|
|
List some possible outputs for CA++
|
-Feces, kidney excretion
-taken out of circulation and used to make new bone |
|
|
How does Ca++ get inputed into the system?
|
-Absorbed through the gut
-Retained in the kidneys -Resorb or breakdown bone to get a little bit of Ca++ back in the blood |
|
|
What other ionic compound does Ca++ have an affinity for?
|
Phosphate
|
|
|
How does Phosphate interact with Ca++?
|
It will bind with Ca++ in plasma and reduce the free Ca++
|
|
|
What will a rise in phosphate concentration do in the body?
|
It will cause a rise in PTH because it will predict that there will be a DROP in Ca plasma conentration.
|
|
|
What two hormones are responsible for regulating Ca++ in the body?
|
-Parathyroid hormone PTH
-Calcitonin |
|
|
Does PTH or Calcitonin have a more profound effect on blood Ca++ levels?
|
PTH
|
|
|
What is PTH's relationship with Calcitonin?
|
antagonistic
|
|
|
The sum of PTHs effect on the body will result in what?
|
ELEVATE blood Ca++ levels
|
|
|
What two mechanisms does bone use to effect Ca++ levels in the body?
|
-Osteoblast: break down bone to release Ca++ into the blood
-Osteoclast: build up bone to remove excess calcium in the blood |
|
|
What substance surrounds bone and contributes to plasma Ca++ levels?
|
Acellular Matrix surrounds the bone and has Ca Occitate within Ca in the plasma.
|
|
|
What lies next to the bone cells that acts as a source of Ca for bone or a deposit for Ca once bone has broken down?
|
Blood vessels
|
|
|
List two ways that our body increases its Vitamin D concentration.
|
-Through direct sunlight (UV) exposure
-Or consumed dietarily |
|
|
When we consume or produce Vitamin D is it active or inactive?
|
Inactive
|
|
|
How does the body activate Vitamin D?
|
First done in the liver and then sent to the kidney.
The PTH regulates the release of Vitamin D in the plasma |
|
|
Does phosphate act directly on the kidneys?
|
No, it acts through PTH, which can then act on the kidney.
|
|
|
What produces and releases Calcitonin?
|
Thyroid gland, specifically the Thyroid C cells (parafollicular)
|
|
|
What is the effect of Calcitonin on the blood?
|
It will REDUCE blood Ca++
|
|
|
How many mechanisms does Calcitonin use to reduce blood Ca++ levels?
|
ONE ONLY
|
|
|
A source of inhibition for calcitonin directly relates to what for the PTH?
|
A source of Stimulation for PTH.
|
|
|
What effect does a rise in phosphate have on PTH and activated Vit D?
|
It will activate PTH and cause a rise in activated Vit D in the Kidneys.
|
|
|
When Ca++ drops, what results can be seen in the body?
|
-May see a rise in Phosphate
-A rise in PTH -A drop in Calcitonin _ |

