![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
94 Cards in this Set
- Front
- Back
|
What is the Potassium range? |
3.5 - 5.0 mEq/l |
|
|
What are the 3 causes of Hyperkalemia? |
1. Excess potassium intake 2. Shift of potassium out of cell EX) Acidosis, Crush injury, Fever, Burn 3. Failure to eliminate potassium EX) ACE inhibitors, NSAIDs, Potassium sparing diuretics |
|
|
What are the 3 causes of Hypokalemia? |
1. Potassium loss EX) Dialysis, GI loss, Diapharisis 2. Shift of potassium into cells EX) Increase epi & insulin, Tissue repair, Alkalosis, 3. Lack of potassium intake |
|
|
What are the s/s (Clinical manifestation) of Hyperkalemia? |
M - Muscle cramping U - Urine abnormalities R - Respiratory distress D - Decrease cardiac contractility E - EKG changes R - Reflexes decrease |
|
|
What are the s/s (Clinical manifestation) of Hypokalemia? |
"A SIC WALT" A - Alkalosis S - Shallow respiration's I - Irritability C - Confusion W - Weakness and fatigue A - Arrhythmia's L - Lethargy T - Thready pulse |
|
|
What are diagnostic findings of Hyperkalemia? |
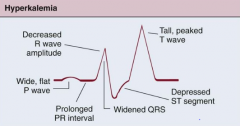
Tall, peaked T wave Prolonged PR interval ST segment depression Loss of P wave Widening QRS Ventricular fibrillation Ventricular standstill |
|
|
What are diagnostic findings of Hypokalemia? |
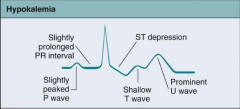
ST segment depression Flattened T wave Presence of U wave Prolonged QRS Ventricular dysrhythmias Bradycardia |
|
|
What is Active Transport? |
Movement of molecules against the concentration gradient with the use of ATP |
|
|
What are the 3 levels of fluid spacing? |
1st spacing - Normal distribution of ICF & ECF 2nd spacing - Abnormal accumulation of interstitial fluid EX) Edema 3rd Spacing - trapped somewhere in the body and can't be exchanged & unavailable for functional use |
|
|
What is a hypertonic solution? |
Hyper = Colton burns energy
The cells will shrink because more solutes in ICF than our ECF |
|
|
What is hydrostatic pressure? |
Hydrostatic pressure is the Pushing force Capillary hydrostatic pressure - pushes fluid from the vascular system into interstitial space |
|
|
What is a hypotonic solution? |
Hypo = Hippo
The cells will swell because because there are less solutes in ICF than our plasma (ECF) |
|
|
What is an isotinic solution? |
Same solute as plasma |
|
|
What is Osmotic Pressure? |
The pull pressure
|
|
|
What is Osmosis? |
The movement of water down a concentration gradient from area of low solute concentration to high solute concentration across a semi- permeable membrane Passive process |
|
|
Facilitated diffusion |
Needs the uses of a protein channel to cross the cell membrane Moves from high to low concentration Passive (No energy needed) |
|
|
What is Osmolality? |
Measures concentration of molecules per WT of H2O EX)Used to evaluate the concentration of plasma or serum in urine |
|
|
What is Osmolarity? |
Measure the total Mmol per solution OR concentration of molecules in the solution |
|
|
What is the range of plasma Osmolality? |
275-295 mil osmol per KG |
|
|
What lab value would be deamed water deficient? |
Plasma osmolality greater than 295 More solutes than water |
|
|
What lab value would be deamed water excess? |
Plasma osmolality less than 275 More water than solutes |
|
|
What is the key to osmolality? With EX! |
Focus on salutes EX) More solute than water = high osmolality EX) More water than solutes = low Osmolality |
|
|
What three reasons fluid would shift from plasma (ECF) to interstitial (ICF) |
1. increase in hydrostatic pressure 2. decrease in osmotic pressure (PULL) EX) low proteins 3. increase in interstitial osmotic pressure EX) burn that damages cell wall, and leaks plasma protein |
|
|
What three reasons would cause fluid to shift from interstitial (ICF) to Plasma (ECF)? |
1. Increase Osmotic pressure EX) give hypertonic solution 2. |
|
|
What two glands regulate fluid balance? |
Hypothalamus and pituitary |
|
|
What are the 3 causes of Hypernatremia? |
1. Excessive Sodium Intake EX) Near drowning in salt water 2. Inadequate Water intake EX) Altered LOC 3. Excessive Water loss EX) Hyperventilation, Diarrhea |
|
|
What are the 3 causes of Hyponatremia? |
1. Excessive Sodium loss EX) GI loss, Renal loss, Skin loss 2. Inadequate sodium intake EX) Fasting diets 3. Excessive water gain EX) Excessive hypotonic fluids |
|
|
What is the range for Sodium? |
135 mEq/L - 145 mEq/L |
|
|
What disease states cause Hypernatremia? |
Diabetes Insipidus Primary Hyperaldosteronsism Cushing syndrome Uncontrolled Diabetes Mellitus |
|
|
What disease states cause Hyponatremia? |
SIADH Heart Failure Primary Hypoaldosteronism |
|
|
What are the clinical manifestation for Hypernatremia with decrease ECF volume? |
Increase pulse weakness lethargy increase thirst agitation increase pulse weight loss |
|
|
What are the clinical manifestation for Hypernatremia with normal or increased ECF volume? |
increase thirst
weight gain pulmonary edema increase BP Agitation |
|
|
What are the clinical manifestation for Hypothermia with decrease ECF volume? |
Personality change
increase pulse, thready cold clammy tremors decrease JVD |
|
|
What are the clinical manifestation for Hyponatremia with normal or increase ECF volume? |
Headache weight gain increase BP Abdominal cramps confusion |
|
|
Fluid volume defict can result from? |
H2O deficiency = hypernatremia Na+ deficiency = Hyopnatremia Isotonic ECF deficit = Normal Na+ |
|
|
Fluid volume excess can result from? |
H2O excess = Hyponatremia Na+ excess = Hypernatremia Isotonic ECF excess = Normal Na+ |
|
|
What is the normal range for calcium? |
8.6 - 10.2 mg/dl |
|
|
What are some causes of Hypercalcemia? |
Increase total calcium EX) Thiazide diuretics, prolonged immobility, Vit D overdose Increase ionized calcium EX) Acidosis |
|
|
What are some causes of Hypocalcemia? |
Decrease total calcium EX) decrease serum albumin, diarrhea, alcoholism, lasix, loop diuretics Decrease ionized calcium EX) Alkalosis, Excess administration of citrated blood` |
|
|
What are the clinical manifestation of Hypercalcemia? |
Decrease memory polyuria bone pain dehydration stupor depressed reflexes |
|
|
What are the clinical manifestation of Hypocalcemia? |
Easy fatigability chvostek's signs laryngeal spasm Trousseau signs Hyperreflexia Numbness & tingling of extremities |
|
|
What are the diagnostic findings of hypercalcemia? |
>10.2 mg/dl calcium Short ST segment Short QT interval Ventricular dysrhythmias |
|
|
What are the diagnostic findings of hypocalcemia? |
< 8.6 mg/dl Elongation of ST segment Prolongation of QT intervals Ventricular tachycardia |
|
|
What is the normal range of Magnesium?
|
1.5 - 2.5 mEq/L
|
|
|
What are some causes of Hypermagnesemia? |
Renal failure Diabetic ketoacidosis Tumor lysis syndrome Excessive intake of Mg+ |
|
|
What are some causes of Hypomagnesemia?
|
Chronic alcoholism NG suction increase urine output Mal absorption syndrome Prolonged malnutrition |
|
|
What are the clinical manifestation of Hypermagnesemia? |
Flushed warm dysphagia muscle weakness decrease pulse & BP Diminished tendon reflex |
|
|
What are the clinical manifestation of Hypomagnesemia?
|
Confusion Tremors Seizures Muscle cramp Increase pulse & BP Insomnia Hyper active deep tendon reflexes |
|
|
What can you do to treat hyponatremia? |
Restrict fluids IV NS (Administer slowly) |
|
|
What can you do to treat hypernatremia?
|
Restrict sodium in the diet Increase water intake Be on the look out for hidden sodium in food |
|
|
What can you do to treat hypokalemia? |
Administer K+ NEVER GIVE IV BOLUS Encourage food rich in potassium ********Assess renal function prior to any K+ adminitration*** |
|
|
What can you do to treat hyperkalemia? |
Administer 50% glucose with R insulin IV loop diuretics Renal dialysis Administer calcium gluconate to protect heart |
|
|
What can you do to treat hypocalcemia? |
Admin Ca+ 30 min prior to meals Increase Ca+ intake Admin Ca+ IV slowly (Infiltration can cause necrosis) |
|
|
What are the ranges for PH, PaCO2, & HCO3? |
ACIDOSIS --------- ALKALOSIS PH = 7.35 - 7.45 PaCO2 = 45 - 35 HCO3 = 22 - 26 |
|
|
What lab values will be interpreted as Respiratory Acidosis? |
PH = < 7.35 PaCO2 = >45 HCO3 = Normal |
|
|
What lab values will be interpreted as Respiratory Alkalosis? |
PH = >7.45 PaCO2 = < 35 HCO3 = Normal |
|
|
What lab values will be interpreted as Metabolic Acidosis?
|
PH = < 7.35 PaCO2 = NORMAL HCO3 = <22 |
|
|
What lab values will be interpreted as Metabolic Alkalosis? |
PH = > 7.45 PaCO2 = NORMAL HCO3 = < 22 |
|
|
What are causes of Respiratory Acidosis? WHY |
Anything that cause you to have hypoventalation, because you will retain to much CO2 EX) Narcotic overdose |
|
|
What are the S/S of Respiratory acidosis? |
Rapid shallow breathing Headache dysrhythmias Muscle weakness Disorientation Decrease BP |
|
|
What is the treatment for a PT with Respiratory Acidosis? |
Treat the cause - Find a way to excrete CO2 Fast & deep breathes - This will increase the quantities and excrete more CO2. |
|
|
What are causes of Respiratory Alkalosis? WHY
|
Anything that will cause you to Hyperventilate (Increase of rate and depth) - Because you will be excrete to much CO2 EX) Anxiety, Fear |
|
|
What are the S/S of Respiratory alkalosis?
|
Decrease in BP Hypokalemia Numbness & tingling of extremities Increase Anxiety & irritability Seizures Hyper reflexes & Muscle crampling |
|
|
What is the treatment for a PT with Respiratory Alkalosis? |
Shallow and Slow - Will decrease tidal volume and cause less gas exchange OR Brown bag special - Will cause the re breathing of exhaled CO2 |
|
|
What are the cause of Metabolic Acidosis? |
Caused by a gain in acid products, other than CO2 EX) DKA, Lactid acidosis due to starvation, Over dose on aspirin OR A loss in basic products EX) Diarrhea because of the loss of basic properties of the stomach |
|
|
What are the S/S of Metabolic Acidosis? |
Warm flushed skin
Nausea & Vomiting Kussmaul Respiration Decrease muscle tone Decrease reflexes |
|
|
What is the treatment for a PT with Metabolic Acidosis?
|
ID & Treat the cause EX) IF over dose on aspirin - then get activated charcoal to contain the aspirin |
|
|
How can the lungs help treat Metabolic Acidosis? |
Lungs will hyperventilate because we have to much acid and the lungs can control CO2 and lower the acidity of the body and raise PH |
|
|
What are the cause of Metabolic Alkalosis? |
A loss of acid other than CO2 EX) Vomiting, NG sucting OR Increase of base products EX) Tums, because it is an anti-acid |
|
|
What are the S/S of Metabolic Alkalosis? |
Confusion Hypoventilation Increase anxiety Dizzy Increase irritability Tremors muscle cramps Tingling of fingers & toes |
|
|
What is the treatment for a PT with Metabolic Alkalosis? |
ID & treat cause EX) If vomiting give anti-emetics to stop vomiting |
|
|
How can the lungs help to treat Metabolic alklosis? |
They will hypoventilate to conserve CO2 and lower the bodies PH. |
|
|
Which foods contain sodium? |
Frankfurters Mustard Butter Ketchup Soy sauce White/whole wheat bread Lunch Meat |
|
|
Which food contain Potassium? |
Cantaloupe Mushrooms Potatoes Raisin Tomatoes Spinach Oranges Avocado Pork, Beef , & Veal |
|
|
What food contain calcium? |
Chesse Collard greens Sardines Tofu Rhubarb Yogurt Milk & Soy milk |
|
|
What food contain magnesium? |
Cauliflower Canned tuna Oatmeal Peas Green leafy vegetables Pork, Beef, Chicken |
|
|
Define Cor Pulmonale. |
Enlargement of the right ventricle caused by a primary disorder of the respiratory systems. |
|
|
What is a Pnemothroax? |
Air enters the pleural space |
|
|
What is a Hemothorax? |
When blood enters the pleural space |
|
|
What is a thoracentesis and how does it work? |
The insertion of a needle into the pleural space, this allows the air or fluid to be withdrawn from the space. |
|
|
What is a thoractomy? |
A surgical incision that allows access to the PT heart, lungs, esophagus, thoracic aorta, or anterior spine. |
|
|
What is pulmonary hypertension? |
Elevated pulmonary arterial pressure, result from an increase resistance in blood flow through pulmonary circulation. EX) Mean pulmonary artery pressure >25 mm/hg @ rest OR >30 mm/hg during exercise |
|
|
What is Chest physiotheraphy? why do you do it? |
A procedure that breaks up mucus in the lungs, done by cupping your hands and tapping the back of the PT repeatedly Ex) Cystic fibrosis |
|
|
What is postural drainage? |
The use of body position to drain secretions from one or more segments of the lungs. |
|
|
What are the clinical manifestation of acute bronchitis? |
Viral infection 90% of time Productive cough can be green headache, fever, chest pain, dyspnea, Will hear rhonchi, wheezes, and crackles on expiration or exertion. |
|
|
What is the collaborative & Nursing care for acute bronchitis? |
Treatment is supportive care so you treat the symptoms. |
|
|
What is the CURB 65 scale used for? What does it stand for? |
Used to determine the severity of pneumonia C - Confusion U - BUN > mg/dl R - Resp rate >30 breaths/min B - Systolic BP < 90 Diastolic BP <60 65 - > 65 YOA |
|
|
How do you score the CURB 65 assessment? |
0 = treat at home 1-2 = Consider hospitalization 3 = Hospital admission 4-5 = Admit to ICU |
|
|
What is the etiology of Pneumonia? |
When the bodies natural defense mechanisms fail to protect the Lower respiratory systems |
|
|
What is the patho of pneumonia? |
The alveoli begin to fill with fluid and interrupts gas exchange. This leads to excessive mucus production and produces further obstructions. |
|
|
What are the clinical manifestations of pneumonia? |
hypoxia, tachypnea,tachycardia, dyspnea, productive cough |
|
|
What is the collaborative care associated with pneumonia? |
IV antibiotic therapy Increase fluids to > 3 L per day Limit activity and rest antipyretics analgesics O2 therapy if indicated |
|
|
How does you differentiate between differentiate between community and hospital acquired pneumonia? |
In community the onset of symptoms occur >14 days after being hospitalized or in a long term care facility. |
|
|
What has to happen for a PT to be diagnosed with hospital acquired pneumonia? |
The client has onset of symptoms 48 hr or later after hospitalization without intubation |

