![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
30 Cards in this Set
- Front
- Back
|
How common are incidentally found adrenal lesions discovered to be adrenocortical carcinoma?
|
4-5% in all comers
|
|
|
In the workup of an incidentally discovered adrenal lesion we do studies to determine if that lesion is functional, are all adrenocortical carcinomas functional?
|
No, but 60-80% are functional and so any incidentally discovered lesion must be evaluated with functional studies.
|
|
|
What is the most common secretory product of adrenocortical carcinomas?
|
Cortisol and they cause cushing's syndrome.
|
|
|
What else is commonly elevated in adrenocortical carcinoma and should prompt an evaluation if symptoms are found in adult patients?
|
There tends to be a higher degree of virilization in these patients secondary to associated hypersecretion of 17 ketosteroids and di-hydroepiandosterone. Serum dihydroepiandosterone should be measured in all patients with signs of excessive hormone secretion. Serum testosterone levels should be assessed in women with excessive virilization and serum 17 beta estradiol levels should be determined in men with evidence of feminization (ie gynecomastia or testicular atrophy)
|
|
|
What are differences between adrenal adenomas and adrenocortical carcinomas on cross sectional imaging with computerized tomography or magnetic resonance imaging?
|
Benign adrenal adenomas identified on cross sectional imaging
are often smaller than 3 centimeters and homogeneous in appearance. When identified on traditional computerized tomography of the abdomen, these lesions typically have a density of less than 10 hounsfield units and demonstrate greater than 50 percent washout of contrast at 10 minutes. On magnetic resonance imaging benign adrenal adenomas similarly display rapid washout of gadolinium and frequently demonstrate high lipid content. The majority of these lesions are iso intense with regard to the liver on T 2 weighted imaging. On the other hand, adrenocortical carcinomas are typically larger than 4 centimeters and appear heterogeneous on computerized tomography. houndsfield unit measurements are frequently greater than 25 and less than 50 percent washout of contrast is identified at 10 minutes. Calcifications and necrosis are frequently present in these lesions. |
|
|
What do pheochromocytomas look like on magnetic resonance imaging?
|
They have high signal intensity on T 2 weighted imaging. The ‘‘light bulb’’ signal on T 2 weighted magnetic resonance imaging has classically been used to identify pheochromocytoma, although more recent studies demonstrate that this signal may be less sensitive and specific than previously thought.
|
|
|
If you are concerned for a pheochromocytoma and there is a possibility that it could be coming from an extra adrenal location, what kind of study would you obtain?
|
Metaiodobenzylguanidine scanning may be considered to assess
for extra-adrenal location |
|
|
Is there a role for adrenal biopsy in adrenal incidentalomas and if not is there a role for adrenal biopsy at all?
|
The role of adrenal biopsy is generally reserved for differentiating
between benign adrenal tissue and metastatic disease. Biopsy is most commonly used in cases of known extra-adrenal malignancies which are subsequently found to have an adrenal lesion. While computerized tomography guided adrenal biopsy is associated with few complications, little data exist to support its routine use in patients presenting with adrenal incidentalomas. Adrenal biopsy should be used selectively and it is imperative that a biochemical assessment be performed before this procedure to avoid a potential hypertensive crisis |
|
|
How does adrenal size affect your treatment decision as far as its risk for being a malignancy?
|
More than 60% of adrenal incidentalomas smaller than 4 centimeters are benign adenomas and fewer than 2 percent of these masses will be primary adrenocortical carcinomas.
Adrenocortical carcinoma will account for only 6 percent of adrenal incidentalomas between 4.1 and 6 centimeters. For lesions larger than 6 centimeters, the incidence of primary adrenal malignancy dramatically increases to 25 percent. For this reason, all lesions larger than 6 centimeters must be considered malignant until proven otherwise and, therefore, should be surgically resected. More difficult decisions are involved when non functional 4 to 6 centimeter lesions are identified. In these cases imaging characteristics such as necrosis, hemorrhage, calcifications and delayed washout may aid in decision making regarding the need for surgery. For patients whose mass is between 4 and 6 centimeters, patient age and need for continued surveillance along with comorbidities will be factors in the decision making process. |
|
|
Is there a size estimation error with computerized tomography for adrenal lesions?
|
It is important to note that computerized tomography may underestimate the size of adrenal incidentalomas in upwards of 20 to 47 percent
of cases. Therefore, some suggest that exploration and resection be performed for all lesions 5 centimeters or larger based on cross sectional imaging. |
|
|
What do pheochromocytomas look like on MRI?
|
high signal intensity on T2-weighted imaging. The ‘‘light bulb’’
signal on T2-weighted MRI has classically been used to identify pheochromocytoma, although more recent studies demonstrate that this signal may be less sensitive and specific than previously thought |
|
|
For patients that have a cortisol secreting adrenal adenoma that are not candidates for resection, what treatment options do they have?
|
For non-operative candidates, medical treatment
to control secretion of functional steroids should be initiated. Agents such as aminoglutethimide, metyrapone and ketoconazole (all of which interfere with various steps of steroid synthesis) have been used with some success. It is important that these patients be monitored for adrenal insufficiency. |
|
|
Can you manage patients with pheochromocytomas non operatively and why or why not? What special issues arise around the time of operation?
|
Pheochromocytoma may be associated with life threatening complications
such as congestive heart failure, cerebrovascular accident or myocardial infarction. Catecholamine induced cardiomyopathy with resultant myocardial necrosis and reduced ejection fraction is an additional complication that can often be reversed with appropriate treatment. Therefore, surgical resection is essential in all patients with suspected pheochromocytoma. All patients require preoperative management with alpha and beta adrenergic blockade to help prevent an intraoperative hypertensive crisis. Phenoxybenzamine, a long-acting alpha-blocker, is generally initiated before beta-blockade to prevent elevated peripheral vascular resistance in the face of unopposed excessive alpha-adrenergic stimulation. After appropriate alpha-blockade has been initiated, a beta-blocker such as propanolol should be added for protection against dysrhythmias. |
|
|
What are the physical exam findings as well as symptoms of Cushing's syndrome?
|
Signs of cushing's syndrome are hypertension, glucose intolerance, central obesity, hyperlipidemia, buffalo hump, abdominal striae,
Symptoms may include complaints of easy bruising and thin easy to tear skin. They may complain of the symptoms associated with diabets as above or hypertension. They may also complain of muscle weakness as well as reproductive issues. |
|
|
What are physical exam findings and symptoms of pheochromocytoma?
|
There may actually not be that many physical exam findings besides hypertension, possibly tachycardia, and tremors.
Symptoms of the disease will exist of paroxysmal headaches, tremors, diaphoresis, the pounding feeling in the chest as if you can hear your heart as well as anxiety. |
|
|
What are the physical exam findings and symptoms associated with primary hyperaldosteronism?
|
Well the patient will probably just have hypertension, but you see on their lab values that they have low potassium levels.
The symptoms would include muscle cramps, they also may have polyuria and increased thirst due to the low potassium. |
|
|
So if a patient has a small non functional adrenal incidentaloma how would you follow them?
|
They should be reimaged and repeat tested for functionality every year for 4 years according to the AUA update.
If the lesion increases in size by 1 centimeter or more surgery should be considered. With long-term follow-up only 5 to 25 percent of adrenal incidentalomas will increase in size by greater than 1 centimeter. Approximately 2 to 8% of previously non functioning lesions can be expected to develop functionality over time, with hypersecretion of cortisol being the most common disorder. The National Institutes of Health state-of-the-science statement on AIs in 2003 recommended repeat cross-sectional imaging at 6 and 12 months following the initial study on which the lesion was found. For lesions that do not increase in size, no evidence to support repeated imaging was identified. Additional recommendations included reassessment for functionality at yearly intervals (or sooner if clinically indicated) for up to 4 years. For AIs remaining stable in size on 2 imaging studies at least 6 months apart which do not demonstrate hormonal hypersecretion, further follow-up may not be warranted. |
|
|
After you perform a resection for adreno cortical carcinoma do you still have to follow those patients. I mean is there a risk for recurrence? How do you follow them?
|
For patients undergoing resection of adrenocortical carcinoma,
close radiological follow-up after resection is imperative given the high rate of local recurrence and metastatic spread. Cross-sectional imaging of the chest, abdomen and pelvis at 3-month intervals is mandatory for the first 2 years after resection. This interval may be increased after 2 years but should continue for at least 5 years or more postoperatively. The role of fluorodeoxyglucose photon emission tomography for follow-up has not been well-defined and remains under study |
|
|
What is the surgical treatment of choice for benign functional or non functional adrenal lesions?
|
Laparoscopic adrenalectomy has
emerged as the treatment of choice for the majority of benign, functional or non functional adenomas. |
|
|
Should we consider laparoscopic adrenalectomy the procedure of choice for adrenocortical carcinoma as well?
|
However, due to the high rates of local and distant recurrences
associated with larger primary adrenal carcinomas and the need for careful handling of the tumor capsule, open adrenalectomy with wide margins and en bloc excision of involved structures remains the procedure of choice for large suspected or proven primary adrenal cancers. There are case reports of laparoscopic and robotic as well. |
|
|
Can you manage hyperaldosteronism non-surgically?
|
Hyperaldosteronism is often associated with severe hypertension, electrolyte disturbances and end organ damage. Therefore, surgical
resection is recommended in patients with aldosterone producing adenomas and proven unilateral hypersecretion of aldosterone. |
|
|
Can you treat the patient with a unilateral aldosterone producing adenoma without surgery?
|
Significant improvements in
blood pressure control will be demonstrated in 40 to 50 percent of patients, although they may require continued treatment with antihypertensive medications. For patients who are poor operative candidates medical management with mineralocorticoid receptor antagonists such as aldactone is indicated. |
|
|
Damage on a first stage turbine blade is an indication of what ?
|
FOD
|
|
|
What are survival rates for patients with adrenocortical carcinomas?
|
Survival rates for patients with adrenocortical carcinoma
are inversely related to disease stage at presentation. Reported 5 year overall survival rates are low (15% to 38%) and median survival rates for those with metastasis are invariably less than 12 months. |
|
|
What are the two most common tests used to diagnose Cushing's syndrome?
|
The most commonly used tests are 24-hour urinary free cortisol measurement and overnight
cortisol suppression test. The overnight cortisol suppression test is the oral administration of 1 mg dexamethasone at 23:00 hours followed by measurement of serum cortisol at 08:00 hours the next morning. A morning serum cortisol greater than 5 grams per deciliter is considered diagnostic of Cushing syndrome. The specificity of this study is reported to be 97%. |
|
|
What is the best test for the diagnosis of pheochromocytoma?
|
More recently, measurement of plasma or urinary fractionated metanephrines (metabolites of catecholamines) has been used, as
available data demonstrate its improved diagnostic sensitivity in detecting silent pheochromocytoma. Metanephrine measurement is believed to be a more sensitive assay because pheochromocytoma catecholamine release is episodic while its metabolism is continuous and, therefore, metanephrines should remain persistently high in the serum and urine. |
|
|
What can cause a false positive test for pheochromocytoma?
|
However, one must carefully
review patient medications before interpreting these studies, as many of them, including levodopa, monoamine oxidase inhibitors, benzodiazepines and tetracycline, are known to falsely increase catecholamine and metanephrine levels. Additionally, rapid withdrawal from clonidine can result in elevated levels of catecholamines. If possible, patients should discontinue these medications before screening. |
|
|
What is the screening test of choice for hyperaldosteronism? What percentage of patients with primary hyperaldosteronism will have normal serum potassium levels?
|
Many patients with primary hyperaldosteronism will have evidence
of hypokalemia secondary to potassium wasting. However, upwards of 40% of patients with this condition will be normokalemic. Therefore, while measurement of serum potassium is important for all patients with adrenal adenomas, it is not a reliable screening test for hyperaldosteronism. The aldosterone to renin ratio is now a widely accepted screening test for this condition. In general, the majority of patients with primary hyperaldosteronism will have a suppressed plasma renin activity, although up to 30% with essential hypertension can be expected to have a low plasma renin activity as well. The aldosterone to renin ratio is defined by the ratio of plasma aldosterone to plasma renin activity. To accurately determine the aldosteron to renin ration, patients must discontinue beta-blockers, clonidine and diuretics. Beta-blockers and clonidine suppress plasma renin activity, therefore generating false positive results, while diuretics stimulate renin secretion and may yield false-negative results. Early studies demonstrated successful identification of patients with primary hyperaldosteronism when the aldosteron to renin ratio was 40 or greater. |
|
|
In patients with adrenal incidentalomas what is the best way to manage a patient that has a high aldosterone to renin ratio concerning for hyperaldosteronism?
|
Therefore, in any patient with an adrenal incidentaloma and an increased aldosterone to renin ratio, confirmatory testing with sodium loading is indicated.
Elevated aldosterone levels after sodium loading confirms the presence of hyperaldosteronism. While increased serum aldosterone and aldosterone to renin ratio values in patients with adrenal incidentalomas raise suspicion for an aldosterone producing adenoma, they do not confirm a unilateral source of aldosterone production. Therefore, lateralizing studies such as adrenal venous sampling are often performed before contemplating surgical intervention for hypertension management. |
|
|
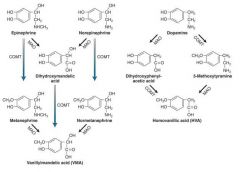
What is the degradation pathway for catecholamines and one of the major final breakdown products?
|
|

