![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
36 Cards in this Set
- Front
- Back
|
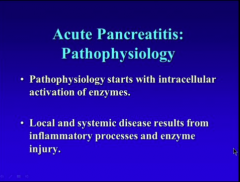
What does pathophysiology of acute pancreatitis start with?
What does local and systemic disease result from? |
|
|
|
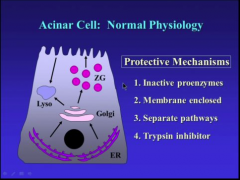
What are the four protective mechanisms of the acinar cell? |
|
|
|
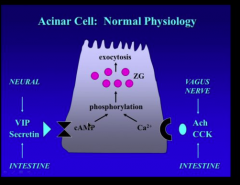
What are the two pathways of activation? What are the components of each that lead to activation? |
|
|
|
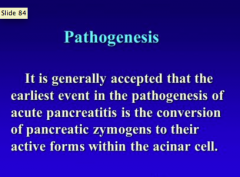
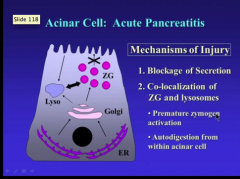
What is the earliest event in the pathogenesis of acute pancreatitis? |
|
|
|
What are the two mechanisms of injury in acute pacreatitis? What do they lead to? |
|
|
|
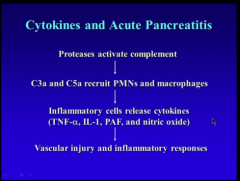
What activates complement? Draw the pathway to vascular injury and inflammatory response |
|
|
|
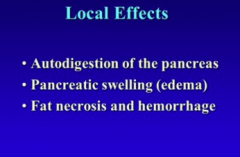
What do the local effects appear as? (digestion, swelling, necrosis, blood)
What are the major clinical symptoms? Where would the pain be? |
Pain, nausea, vomiting Epigastric, midabdomen, radiating to the back because pancreas is retroperitoneal! |
|
|
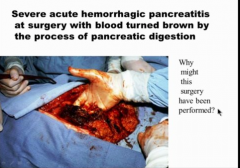
Hemorrhage => splenic vein and artery are right on top of the pancreas! Blood will pour out if the enzymes leak out => if it erodes the splenic artery there is rare chance of survival, vein has better odds.
Usually surgery is from necrosis and infection. |
|
|
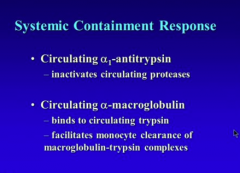
What inactivates proteases?
What binds to circulating trypsin and facilitates monocyte clearance of macro globulin trypsin complexes? |
|
|
Complete |
|
|
|
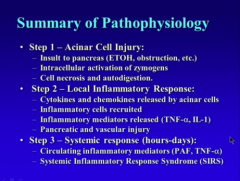
What are the three steps of acute pancreatitis? |
|
|
|
What are the two main causes of acute pancreatitis? What are the three main symptoms? What two enzymes are elevated? How do you manage the condition? |
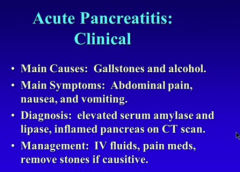
|
|
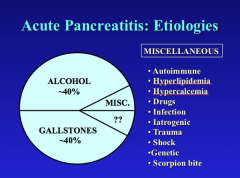
|
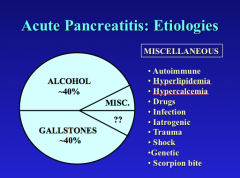
|
|
|
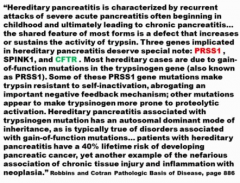
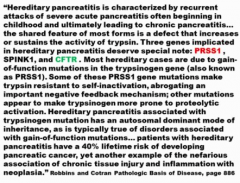
What is the location of the trypsinogen mutation? What does it result in? What type? |
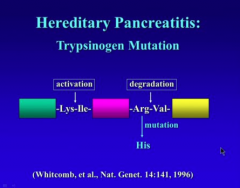
Autosomal dominant, young age => recurrent acute pancreatitis
Degradation in C-terminus (mutation is here and degradation is inhibited => recurrent pancreatitis) |
|
|
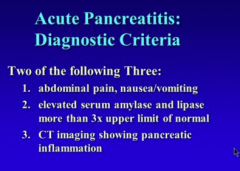
What are the three diagnostic criteria for acute pancreatitis? |
|
|
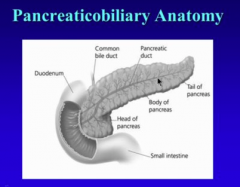
What empties into ampulla of cater? |
Common bile duct and pancreatic duct => obstruction by stone will block both |
|
|
|
|
|
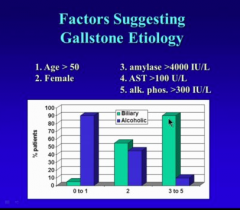
Gallstones: Sex? Age? Amylase level? AST level? Alk phos level? |
|
|
|
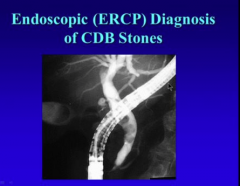
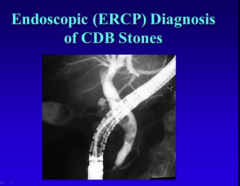
What is the ultimate diagnosis made by? |

Opening of ampulla of Vater to remove stones |
|
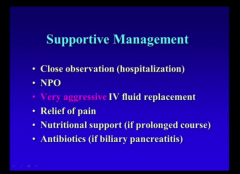
What is the biggest mistakes physicians make? |
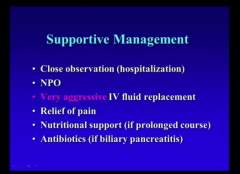
Not being aggressive enough with fluid replacement! |
|
|
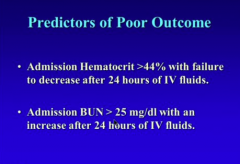
What are two predictors of poor outcome? Hematocrit and BUN levels... |
|
|
|
What percent interstitial pancreatitis? What percent necrotizing? Which has worse prognostic outcome? |
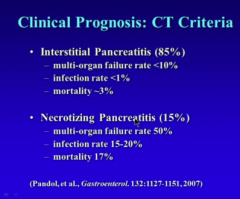
|
|
|
What are some of the complications of acute pancreatitis? Fluid, cysts, fistulas, vein.. |
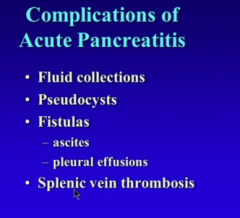
|
|
|
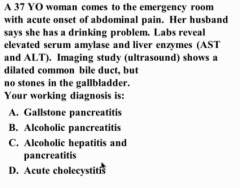
Gallstone pancreatitis! 10% of people who are drinkers get pancreatitis 10% of drinkers get alcoholic hepatitis Common bile duct is dilated and liver enzymes are elevated
DILATED COMMON BILEDUCT WITH PANCREATITIS = GALLSTONE PANCREATITIS |
|
|
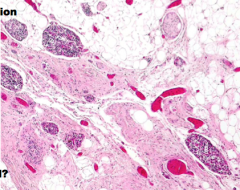
What is the pathophysiology of chronic pancreatitis? What is the cause? Three symptoms? Diagnosis? How do you manage? |
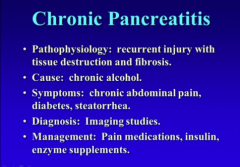
|
|
|
|
|
|
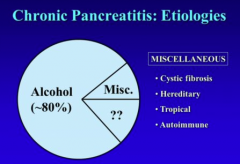
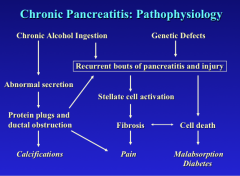
What are the two causes of pathophysiology that lead to recurrent bouts of pancreatitis and injury? What does alcohol effect? What type of obstructions does it lead to? What things do the recurrent bouts of pancreatitis and injury lead to? |
|
|
Are the islets preserved in chronic pancreatitis? Why? |
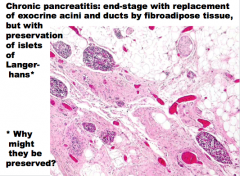
Islets are more resistant than the acini. They do not self digest in the same way that the acini do. |
|
|
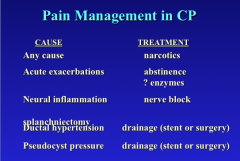
What is the number one symptom of chronic P? What are two other symptoms? |
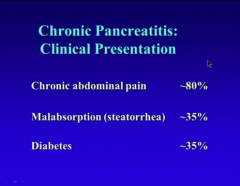
|
|
|
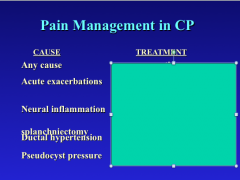
What is the pain related to? |
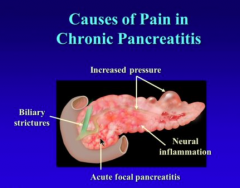
Fibrotic pancreas, pressure within organ Pseudocysts that form and swell, biliary stricture. |
|
Complete |
|
|
|
What is steatorrhea? Does fat malabsorption occur before protein or carb? Why? What are the three treatments? |
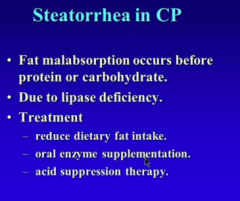
|
|
|
When is diabetes seen in CP? What is lost? Is ketoacidosis rare? Why low dose insulin? |
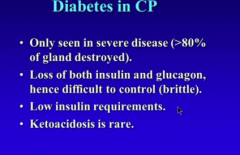
|
|
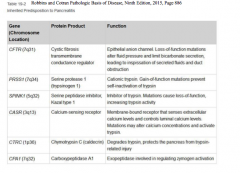
Just focus on the first three. |
|
|
|
|
|
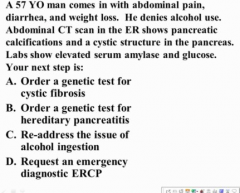
|
C = re-address the issue of alcohol ingestion Don't present with hereditary or CF at 57!
CHRONIC PANCREATITIS = ALCOHOL! |

