![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
93 Cards in this Set
- Front
- Back
|
Pt c/ tumor @ cerebello-pontine angle c/o "unsteadiness" |
Acoustic neuroma;
-Sx: tinnitus, unsteadiness, hearing loss -Cerebello-pontine angle |
|
|
Acoustic neuroma:
-Affects CN_ @ location _ |
Acoustic neuroma:
-Affects CN8 @ cerebello-pontine angle (cps) -Sx: hearing loss, unsteadiness, vertigo, vomiting -Tx = surgery |
|
|
Pt has a parotid tumor that has had a long, indolent course, now invades facial nerve root
(hint: it is not mucoepidermoid carcinoma) |
Adenoid cystic carcinoma
-#2 malignant tumor of salivary glands -#1 malignant tumor of small/submandibular/mino salivary glands -Long, indolent course -Propensity to invade nerve roots -Tx: parotidectomy -Prophylactic MRND + post-op XRT if high grade |
|
|
__ = #2 malignant tumor of salivary glands
-#1 malignant tumor of small/submandibular/mino salivary glands |
Adenoid cystic carcinoma
-#2 malignant tumor of salivary glands -#1 malignant tumor of small/submandibular/mino salivary glands -Long, indolent course -Propensity to invade nerve roots -Tx: parotidectomy -Prophylactic MRND + post-op XRT if high grade |
|
|
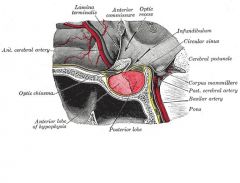
__ is released by supraoptic nucleus of hypothalamus into posterior pituitary in response to high serum osmol.
|
ADH:
-high plasma osmolarity -> supraoptic nucleus of hypothalamus releases ADH into post. pituitary -> increased H20 absorption in collecting ducts -DI (low ADH): EtOH, head injury -> low urine spec grav, high serum Na. Tx: DDAVP, free H20 -SIADH: head injury -> low UOP, high urine spec grav, low serum Na. Tx: fluid restriction, then diuresis. give 3% if intitial tx fails |
|
|
What is this patient's problem?
-Loss of bilateral motor, pain, and temp -Preserved position sense, light touch |
Anterior spinal artery syndrome:
-Lost bilateral motor, pain, and temp -Keep position sense, light touch |
|
|
What spinal cord syndrome? Bilat loss of motor, pain, temp sensation below lesion.
-most commonly occurs 2/2 _ |
Anterior spinal artery syndrome: most commonly c/ acutely ruptured cervical disk. Bilat loss of motor, pain, temp sensation below lesion. Preserved position-vibratory sensation and light touch. ~10% recover to ambulation
-Brown-Sequard: incomplete transection (hemisection of cord). usually 2/2 penetrating injury. Loss of ipsilateral motor, contralateral pain, and temp below lesion. 90% recover to ambulation. -Central cord syndrome: usually 2/2 hyperflexion of cervical spine. Bilat loss of motor, pain, temp sensation in upper extremities. lower extremities spared. -Cauda equina: pain + weakness in lower extremities 2/2 compression of lumbar nerve roots |
|
|
damage to the __ causes conduction aphasia (auditory comprehension and speech articulation are preserved, but difficult to repeat heard speech)
|
Arcuate fasiculus:
-neural pathway connecting the posterior part of the temporoparietal junction with the frontal cortex in the brain and is now considered as part of the superior longitudinal fasciculus -previously thought to connect Wernicke's area and Broca's area, new research demonstrates that the arcuate fasciculus instead connects to posterior receptive areas with premotor/motor areas, and not to Broca's area -Damage can cause conduction aphasia= auditory comprehension and speech articulation are preserved, but people find it difficult to repeat heard speech. |
|
|
25 M presents c/ sudden headache, LOC. CT shows brain bleed. Likely 2/2 __. Tx is _
|
arteriovenous malformations:
-50% present c/ hemorrhage. -Usually pts <30 y/o. congenital. sudden HA, loss of consciousness -Tx: resection if poss for both symptomatic and asymptomatic -Can coil embolize prior to resection |
|
|
10 y/o boy presents c/ cyst that has recurrent infections
-Cyst tract near angle of mandible -Cyst most likely connects to the _ |
Type 1 branchial cleft cyst:
-Extends from angle of mandible -> external auditory canal -Often ass'd c/ facial nerve -Tx: resection (avoid facial nerve) |
|
|
10 y/o boy presents c/ cyst in lateral neck medial to the anterior border of sternocleidomastoid.
Cyst most likely connects to _ |
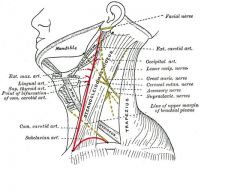
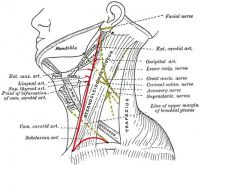
Type II branchial cyst = most common branchial cleft cyst:
-Extends from antrerior border of sternocleidomastoid -> through carotid bifurcation -> to tonsillar pilar -Tx: resection |
|
|
#1 type of branchial cleft cyst is _
|
Type II branchial cyst = most common branchial cleft cyst:
-Extends from antrerior border of sternocleidomastoid -> through carotid bifurcation -> to tonsillar pilar -Tx: resection |
|
|
_% of intracranial neoplasms are mets
-_% of those pts are surgical candidates -_ primary = #1 source of lung mets |
Brain tumor:
-Gioma = #1 primary brain tumor, multiforme = #1 subtype -50% of intracranial neoplasms = mets. 20-25% of cancer pts get IC mets, become symptomatic 2/2 mass effect on white matter -25% of solitary brain met pts are surgical candidates -Lung = #1 source of brain mets -#1 brain tumor in kids = medulloblastoma -#1 metastatic brain tumor in kids = neuroblastoma |
|
|
Broca's area located in __. Responsible for _
|
Broca's area: in posterior part of frontal lobe. Speech motor
|
|
|
What is this trauma patient's problem:
-loss of ipsilateral motor; contralateral pain + temp |
Brown Sequard syndrome:
-spinal cord 1/2 transected -loss of ipsilateral motor; contralateral pain + temp |
|
|
What syndrome? loss of ipsilateral motor, contralateral pain and temp below lesion.
-Usually 2/2 __ -_% recover to ambulation |
Brown-Sequard: incomplete transection (hemisection of cord). usually 2/2 penetrating injury. Loss of ipsilateral motor, contralateral pain, and temp below lesion. 90% recover to ambulation.
-Anterior spinal artery syndrome: most commonly c/ acutely ruptured cervical disk. Bilat loss of motor, pain, temp sensation below lesion. Preserved position-vibratory sensation and light touch. ~10% recover to ambulation -Central cord syndrome: usually 2/2 hyperflexion of cervical spine. Bilat loss of motor, pain, temp sensation in upper extremities. lower extremities spared. -Cauda equina: pain + weakness in lower extremities 2/2 compression of lumbar nerve roots |
|
|
What syndrome? pain + weakness in lower extremities 2/2 compression of lumbar nerve roots
|
Cauda equina: pain + weakness in lower extremities 2/2 compression of lumbar nerve roots
-Anterior spinal artery syndrome: most commonly c/ acutely ruptured cervical disk. Bilat loss of motor, pain, temp sensation below lesion. Preserved position-vibratory sensation and light touch. ~10% recover to ambulation -Brown-Sequard: incomplete transection (hemisection of cord). usually 2/2 penetrating injury. Loss of ipsilateral motor, contralateral pain, and temp below lesion. 90% recover to ambulation. -Central cord syndrome: usually 2/2 hyperflexion of cervical spine. Bilat loss of motor, pain, temp sensation in upper extremities. lower extremities spared. |
|
|
what is this patients problem?
-loss of bilateral upper extremity motor, pain, temp -legs relatively spared -this injury is typically 2/2 __ |
Central cord syndrome:
-bilateral loss of upper extremity motor, pain, temp -legs relatively spared -usually 2/2 hyperextended C-spine injury |
|
|
What syndrome? Bilat loss of motor, pain, temp sensation in upper extremities. lower extremities spared.
-Usually 2/2 _ |
Central cord syndrome: usually 2/2 hyperflexion of cervical spine. Bilat loss of motor, pain, temp sensation in upper extremities. lower extremities spared.
-Anterior spinal artery syndrome: most commonly c/ acutely ruptured cervical disk. Bilat loss of motor, pain, temp sensation below lesion. Preserved position-vibratory sensation and light touch. ~10% recover to ambulation -Brown-Sequard: incomplete transection (hemisection of cord). usually 2/2 penetrating injury. Loss of ipsilateral motor, contralateral pain, and temp below lesion. 90% recover to ambulation. -Cauda equina: pain + weakness in lower extremities 2/2 compression of lumbar nerve roots |
|
|
Patient age 20-60 c/ hx HTN presentes c/ head bleed. Suspect...
-Tx for this problem is _ |
Cerebral aneurysms:
-usually patients >40 y/o. bleed @ age 20-59, a/w HTN., Most congenital. -Presentation: bleed, mass effect, seizure, or infarct -Occur @ branch points in artery, most in carotid or anterior circulation -Often place coils before clipping + resecting if elective resection |
|
|
what is the typical goal cerebral perfusion pressure?
-what is Cushing's triad? |
cerebral perfusion pressure usually should be ~70
(MAP-ICP) -If head trauma + low CPP => elevate HOB, sedate + paralyze, mod hyperventilation for pCO2 30-35, mannitol. craniectomy if these fail. -Max brain swelling 48-72 hrs p/ trauma -CUSHINGS TRIAD = signs of high ICP: hypertension, HR lability, slow respirations (intermittent bradycardia = sign of impending herniation) -Dilated pupil p/ trauma => ipsilateral temporal herniation onto CN3 |
|
|
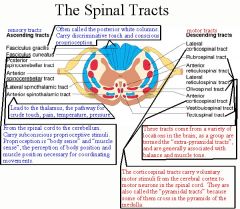
Corticospinal tract: what type of neurons
|
Corticospinal tract: motor neurons
|
|
|
Cricothyroid muscle is ennervated by the _ nerve
|
Cricothyroid muscle is ennervated by the superior laryngeal nerve
|
|
|
what is Cushing's triad?
(think cerebral perfusion pressure) |
cerebral perfusion pressure usually should be ~70
(MAP-ICP) -If head trauma + low CPP => elevate HOB, sedate + paralyze, mod hyperventilation for pCO2 30-35, mannitol. craniectomy if these fail. -Max brain swelling 48-72 hrs p/ trauma -CUSHINGS TRIAD = signs of high ICP: hypertension, HR lability, slow respirations (intermittent bradycardia = sign of impending herniation) -Dilated pupil p/ trauma => ipsilateral temporal herniation onto CN3 |
|
|
dorsal nerve roots:
-afferent or efferent? -what type of fibers? |
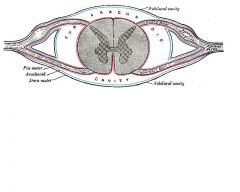
dorsal nerve roots: generally afferent. sensory fibers
|
|
|
CT shows lens shape brain bleed that goes into brain
-what type of bleed is it? -what artery is often to blame? __% mortality |
Epidural hematoma:
-lens shape, goes into brain, pushes brain away -lucid interval -10% mortality -middle meningeal artery |
|
|
Eryhtoplakia vs. Leuokplakia - which has more malignant potential?
|
Erythroplakia:
-Worse (pre-malignant) than leukoplakia -Retinoids can reverse leukoplakia, reduce risk of 2nd head/neck malignancy |
|
|
Frey's syndrome: after parathyroidectomy
-Injury to the _ nerve -> cross-enervates c/ _fibers to the _ -> effect: _ |
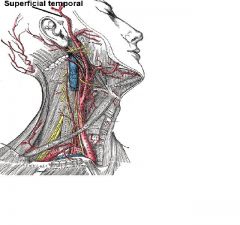
Frey's syndrome: typically after parathyroidectomy
-Injury to the AURICULOTEMPORAL nerve -> cross-ennervatation of sympathetic fibers to the sweat + salivary glands of the skin -> GUSTATORY SWEATING -Usually self-limited, but for refractory cases put a piece of alloderm b/w auriculotemporal + skin nerves auriculotemporal nerve = a branch of mandibular nerve that runs with the superficial temporal artery and vein, and provides sensory innervation to various regions on the side of the head = the nerve that is painful in mumps |
|
|
Pt c/ recent parathyroidectomy or similar surgery experiences gustatory sweating.
-This is called __ syndrome -Tx is _ |
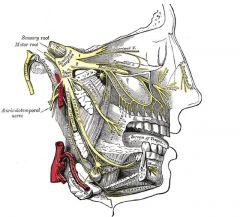
Frey's syndrome: typically after parathyroidectomy
-Injury to the AURICULOTEMPORAL nerve -> cross-ennervatation of sympathetic fibers to the sweat + salivary glands of the skin -> GUSTATORY SWEATING -Usually self-limited, but for refractory cases put a piece of alloderm b/w auriculotemporal + skin nerves auriculotemporal nerve = a branch of mandibular nerve that runs with the superficial temporal artery and vein, and provides sensory innervation to various regions on the side of the head = the nerve that is painful in mumps |
|
|
if a head injury patient has GCS 8 or less, consider 2 therapeutic interventions...
|
if a head injury patient has GCS 8 or less, consider:
-Intubation -ICP monitor |
|
|
If a head injury patient has GCS 5 or less, mortality is __%
|
If a head injury patient has GCS 5 or less, mortality is 50%
|
|
|
#1 brain tumor = _
|
Glioma: #1 brain tumor
-Glioma multiforme = #1 subtype. uniformly fatal |
|
|
Injury to cranial nerve _ (aka the _ nerve) affects swallowing
|
Injury to the GLOSSOPHARYNGEAL (CN 9) affects swallowing
|
|
|
Glottic ca: tx depends on _
|
Glottic ca:
-If cords not fixed =. XRT -Cords fixed => surgery + XRT |
|
|
Pt suffers a nerve injury during parotid surgery.
Most likely to be the _ nerve, which presents c/ _ when injured |
Greater auricular nerve = most commonly injured in parotid surgery
Numbness over lower portion of auricle |
|
|
max brain swelling p/ head trauma = _ - _ hours
|
cerebral perfusion pressure usually should be ~70
(MAP-ICP) -If head trauma + low CPP => elevate HOB, sedate + paralyze, mod hyperventilation for pCO2 30-35, mannitol. craniectomy if these fail. -Max brain swelling 48-72 hrs p/ trauma -CUSHINGS TRIAD = signs of high ICP: hypertension, HR lability, slow respirations (intermittent bradycardia = sign of impending herniation) -Dilated pupil p/ trauma => ipsilateral temporal herniation onto CN3 |
|
|
Head/Neck SCCa staging:
-Stage 1: up to _ cm, no nodes. Tx: __ -Stage 3 or 4 tx = _ |
Head/Neck SCCa staging:
-Stage 1: up to 4 cm, no nodes. Tx: surgery or RT -Stage 3 or 4: combine surgery + XRT |
|
|
Child presents c/ salivary gland tumor.
Most likely to be_ |
Hemangioma:
-#1 salivary gland tumor in children |
|
|
What is a Charcot-Bouchard aneurysm?
|
Hypertensive bleeds:
-generally involve basal ganglia, putamen = most common site. -Arteries to this area can withstand high pressures, but long-standing HTN causes fibrinoid necrosis, and miliary microaneurysms known as Charcot-Bouchard aneurysm. -CT = most common diagnostic tool diagnosing the disease. -does not generally involve subarachnoid space. -Clinical recognition of cerebellar hematoma permits evacuation of the clot before condition ends fatally via brain stem compression and obstructive hydrocephalus |
|
|
intracerebral hematoma:
-_ lobe most often affected -drain if _ |
intracerebral hematoma:
-temporal lobe most often affected -drain if large or causing focal deficit |
|
|
premature baby c/ hx cyanotic heart defect has bulging fontanelle, low BP
-Suspect _ -Tx is _ |
Intraventricular hemorrhage (subependymal hemorrhage)
-seen in preemies 2/2 rupture of fragile vessels in germinal matrix -RFs: ECMO, cyanotic congenital heart dz -Sx: bulging fontanelle, neuro deficit, low BP, low Hct -Tx: ventricular catheter for drainage, prevention of hydrocephalus |
|
|
Teen male presents c/ symptoms of nasopharyngeal obstruction, epistaxis.
-Consider __ -Tx is __ |
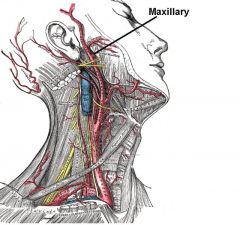
Juvenile nasopharyngeal angiofibroma:
-Benign -Teen males -Present c/ obstruction, epistaxis -Tx: embolize (internal maxillary artery), then extirpate |
|
|
Juvenile nasopharyngeal angiofibroma:
-Tx includes embolization of __ artery |
Juvenile nasopharyngeal angiofibroma:
-Benign -Teen males -Present c/ obstruction, epistaxis -Tx: embolize (internal maxillary artery), then extirpate |
|
|
Lip ca:
-99% are type __ -Most common location -Tx depends on _ -If node (+), must do a __ |
Lip ca:
-99% epidermoid carcinoma -Lower > upper lip 2/2 sun exposure -Resect + primary closure if <50% of lip -Otherwise do a flap Node (+) > radical neck dissection |
|
|
An obese 54yr male presents to your clinic with a firm, painless, right lateral neck mass that measures 2cm and does not move with deglutition. What is the most likely diagnosis?
|
All posterior neck masses are lymphoma until proven otherwise.
All fixed anterior neck masses are metastatic nodal disease (usually squamous head and neck neoplasm) until proven otherwise |
|
|
Pt suffers a nerve injury during submandibular resection
Most likely to be the _ nerve, which supplies the _ |
MARGINAL MANDIBULAR nerve = most commonly injured in submandibular resection
-supplies the lower lip and chin |
|
|
__ artery supplies the lateral 2/3 of cerebral hemispheres, internal capsule, basal ganglia, somatosensory cortex
|
MIDDLE CEREBRAL ARTERY => lateral 2/3 of cerebral hemispheres, internal capsule, basal ganglia, somatosensory cortex
|
|
|
-#1 brain tumor in kids = _
|
-#1 brain tumor in kids = medulloblastoma (15%)
- originates in the cerebellum (2/3 or peds brain tumors are infratentorial) or posterior fossa. - primitive neuroectodermal tumors => spread through the cerebrospinal fluid (CSF) and frequently metastasize to different locations in the brain and spine. #1 metastatic brain tumor in kids = neuroblastoma |
|
|
the _ connects the vestibular system with the cranial nerves controlling eye movements.
|
median longitudinal fasiculus connects the vestibular system with the cranial nerves controlling eye movements.
|
|
|
#1 malignant salivary gland tumor
|
Mucoepidermoid carcinoma: 30% of parotid malignancies
-Wide range of aggressiveness -Tx: resection of salivary gland (parotidectomy) -Prophylactic MRND + post-op XRT if high grade -lymphatic drainage to intraparotid nodes, anterior cervical chain nodes |
|
|
Pt has a parotid tumor that invades both deep and superficial portions of the gland, involves facial nerve => facial droop
What is this tumor most likely to be? |
Mucoepidermoid carcinoma = #1 malignant salivary gland tumor
-30% of parotid malignancies -Invasion of deep and superficial glands or facial nerve involvement suggest a malignant tumor -Tx: total parotidectomy c/ facial nerve -If high grade => prophylactic MRND + post-op XRT |
|
|
Mucoepidermoid carcinoma = #1 salivary gland tumor
-Tx is __ -Add __ and __ to tx if __ |
Mucoepidermoid carcinoma = #1 malignant salivary gland tumor
-30% of parotid malignancies -Invasion of deep and superficial glands or facial nerve involvement suggest a malignant tumor -Tx: parotidectomy -If high grade => prophylactic MRND + post-op XRT |
|
|
most common location for myelomeningocele in infant is _
-Tx is _ |
Myelomeningocele (pediatric):
-Neural cord defect - herniation of spinal cord + nerve roots through defect in vertebra -if sac ruptured => surgery to avoid infection -usually in lumbar region |
|
|
Elderly Chinese man presents c/ recent obstructive-type upper airway sx requiring mouth breathing, then nose bleed. Suspect what cancer?
|
Nasopharyngeal SCCa:
-Typical pt elderly, Chinese. Presents c/ obstruction and/or bleeding. -50% present c/ neck mass -Drain to posterior (deep) cervical neck nodes -A/w EBV Tx: XRT primary. MRND for tumors >2 cm or clinically (+) nodes. Postop chemo for advanced dz. In kids, lymphoma = #1 tumor of nasopharynx => chemo Papilloma = #1 benign neoplasm of nose/paranasal sinuses |
|
|
What structures are b/w the subclavian vein and artery?
|
Anterior -> Posterior:
SCV -> phrenic nerve -> anterior scalene -> SCA |
|
|
#1 metastatic brain tumor in kids = _
|
-#1 brain tumor in kids = medulloblastoma
#1 metastatic brain tumor in kids = neuroblastoma |
|
|
The most common parotid tumor is
|
Pleomorphic adenoma = #1 parotid tumor
-architectural pleomorphism on light microscopy.Admixture of epithelial and myoepithelial elements in a variable background stroma that may be mucoid, myxoid, cartilaginous or hyaline. |
|
|
what is the most common malignant tumor of parotid gland?
- What is the 1st/crucial step in parotid surgery? - change of operation if tumor >_ cm |
"Mucoepidermoid carcinoma = #1 malignant tumor of parotid = 30% of parotid malignancies.
(#1 tumor overall = pleomorphic adenoma or benign mixed tumor) 90% of parotid tumors originate in the superficial lobe. -Superficial parotid lobectomy = minimum operation. Appropriate if tumor confined to superficial lobe, low grade, <4 cm, no local invasion, no regional node involvement. -If DEEP lobe tumor, do total parotidectomy. Identification of the facial nerves and branches is the first and most crucial step. |
|
|
Parotiditis:
-Organism = _ -Typical population -Tx |
Parotiditis:
-Staph -Elderly pt, dehydrated -Tx: Abx; I+D if abscess present or not improving |
|
|
Peripheral nerve injuries:
what is definition, prognosis of neuropraxis? |
Peripheral nerve injuries:
-NEUROPRAXIS: focal demyelination. improves -Axonotmesis: loss of axon continuity (nerve + sheath intact). regenerates 1 mm/day -Neurotmesis = loss of nerve continuity. Surgery needed for nerve recovery |
|
|
Peripheral nerve injuries:
what is definition, prognosis of axonotmesis? |
Peripheral nerve injuries:
-Neuropraxis: focal demyelination. improves -AXONOTMESIS: loss of axon continuity (nerve + sheath intact). regenerates 1 mm/day -Neurotmesis = loss of nerve continuity. Surgery needed for nerve recovery |
|
|
Peripheral nerve injuries:
what is definition, prognosis of neurotmesis? |
Peripheral nerve injuries:
-Neuropraxis: focal demyelination. improves -Axonotmesis: loss of axon continuity (nerve + sheath intact). regenerates 1 mm/day -NEUROTMESIS = loss of nerve continuity. Surgery needed for nerve recovery |
|
|
Patient c/ pituitary adenoma undergoing XRT is now in shock
-Diagnosis is __ -Tx is _ |
Pituitary apoplexy:
-Pt c/ pituitary adenoma undergoing XRT develops shock 2/2 infarction or hemorrhage of the pituitary gland -Tx = steroids |
|
|
Most common benign salivary gland tumor is _
Tx is _ |
Pleomorphic adenoma (mixed tumor):
-#1 benign tumor of salivary glands; 75% of parotid neoplasms -Typical pt: middle-aged womain -Tx: superficial parotidectomy (spare CN 7, do not enucleate) -Malignant degeneration in 5% (recurrence post-op in 10%) => need total parotidectomy (take CN7) -High grade => radical neck dissection |
|
|
Pleomorphic adenoma:
-Tx for most cases is __ -If malignant, tx is __ -If high grade, tx is _ |
Pleomorphic adenoma (mixed tumor):
-#1 benign tumor of salivary glands; 75% of parotid neoplasms -Typical pt: middle-aged womain -Tx: superficial parotidectomy (spare CN 7, do not enucleate) -Malignant degeneration in 5% (recurrence post-op in 10%) => need total parotidectomy (take CN7) -High grade => radical neck dissection |
|
|
A 50 yo female secretary presents with a lump along the right jaw line. After MRI an FNA is performed and the pathology report comes back as "mixed tumor."
Tx is... |
Mixed tumor, also known as pleomorphic adenoma = 75% of parotid neoplasms.
-Benign tumor, usually in middle-aged women -Tx:superficial parotidectomy c/ sparing of facial nerve (or total parotidectomy if deep lobe involved) -10% recurrence after surgery -Shelling out of the tumor mass is not recommended because of the risk of incomplete excision and tumor spillage. |
|
|
Radical neck dissection:
-What are the nerve, muscle, vessel, and gland which have to be removed? -What is the most morbid part? |
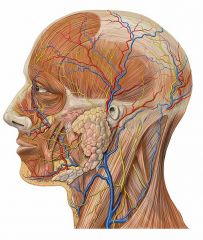
Radical neck dissection:
-takes CN7, SCM, IJ, submandibular gland -Most morbid = CN7 Neck LNs: Level I: Submental and submandibular nodes Level Ia: Submental triangle Level Ib: Submandibular triangle Level II: Upper jugular nodes Level III: Middle jugular nodes Level IV: Lower jugular nodes Level V: Posterior triangle group Level VI: Anterior compartment group |
|
|
Recurrent laryngeal nerve:
-Innervates all of larynx except the _ muscle -what artery does it typically run with? |
Recurrent laryngeal nerve:
-Innervates all of larynx except CRICOTHYROID muscle -Run posterior to thyroid lobes in tracheoesophageal groove -Can tract c/ inferior thyroid artery, but variable -L RLN loops around aorta -R RLN loops around R subclavian = innominate artery, but R is more lateral, more likely than L to be non-recurrent (e.g. 2/2 replaced R subclavian off the descending aorta) -Risk of injury to non-recurrent laryngeal nerve during surgery -Unilateral injury -> hoarseness; Bilat injury -> airway obstruction 2/2 medialization of cords, requires emergent tracheostomy |
|
|
rubrospinal tract: what type of neurons
|
rubrospinal tract: motor neurons
|
|
|
Patient presents c/ severe HA, nausea, lethargy of acute onset.
CT shows __ with bloof in interhemispheric + bilat sylvian fissures. Also rounding of 3rd ventricle, visualization of temporal horns -This is c/w __, which is usually 2/2 _ or __ -Tx is _ -Surgery only if _ |

Subarachnoid hemorrhage (non-traumatic):
-2/2 cerebral aneurysms (50% middle cerebral artery), AVMs -Sx: stiff neck, severe HA, photophobia, neuro defects -Goal = clip to isolate aneurysm from systemic supply, maximize cerebral perfusion to overcome vasospasm, prevent rebleed -Tx: hypervolemia, Ca channel blockers -go to OR only if neurologically intact -SAH can also happen c/ trauma |
|
|
Is salivary gland tumor more likely to be benign in smaller or larger glands?
|
Salivary gland tumor more likely to be benign in the larger glands, e.g. parotid
|
|
|
SCH:
-what shape? -_% mortality |
SDH:
-2/2 torn bridging veins -crescent shape -conforms to brain -50% mortality (higher mortality than epidural hematoma) |
|
|
ADH is produced when ___ is sensed by the supraoptic nucleus of the _ ->
increased free H20 absorbtion @ ___ and ___ |
ADH produced when high OSMOLARITY sensed by SUPRAOPTIC NUCLEUS OF HYPOTHALAMUS ->
increased free H2O absorbtion @ distal tubules, collecting ducts -EtOH, head injury inhibit ADH release = DI (high UOP, low urine SG, high serum osmol/Na) -CHI can cause SAIDH (oliguria, high urine osmol, low serum osmol/Na) |
|
|
what are the 2 main indications for operating on a skull fracture
|
Skull fracture should be taken to OR if open or depressed to ~thickness of the skull
|
|
|
Spinal shock:
-Spinal cord injury above T_ -Therapy is __ |
Spinal shock:
-spinal cord injury above T5 => lose symp tone -bradycardia, warm perfused extremities -Tx: fluids +/- alpha agonist (phenylephrine) |
|
|
trauma pt has spinal injury + areflexia, flaccidity, anesthesia, autonomic paralysis below lesion
-Injury c/w __ |
Spinal cord injury:
-Cord injury + deficit => give high dose steroids to reduce swelling -Complete cord transection -> areflexia, flaccidity, anesthesia, autonomic paralysis below lesion -Spinal shock: hypotension, normal to slow HR, warm extremities. above T5. Tx: Fluids +/- phenylephrine -Anterior spinal artery syndrome: most commonly c/ acutely ruptured cervical disk. Bilat loss of motor, pain, temp sensation below lesion. Preserved position-vibratory sensation and light touch. ~10% recover to ambulation -Brown-Sequard: incomplete transection (hemisection of cord). usually 2/2 penetrating injury. Loss of ipsilateral motor, contralateral pain, and temp below lesion. 90% recover to ambulation. -Central cord syndrome: usually 2/2 hyperflexion of cervical spine. Bilat loss of motor, pain, temp sensation in upper extremities. lower extremities spared. -Cauda equina: pain + weakness in lower extremities 2/2 compression of lumbar nerve roots |
|
|
Spinal cord tumors:
__% are benign __ intra or extradural more likely to be malingnant/metastatic? |
Spinal cord tumors
- 60% benign - #1 type = neurofibroma - extradural likely malignant/metastatic - If paragangionoma, check urine for metanephrine; MIBG for extramedullary chromatin tissue (detects pheochromocytoma and neuroblastoma) |
|
|
_% of trauma patients with head injury have a spinal injury
|
13% of trauma patients with head injury have a spinal injury
- SDH: #1. 2/2 tearing of venous plexus (bridging veins) b/w dura + arachnoid. Crescent shape. Operate for sig. mass effect. Chronic in elderly p/ fall; drain if >1cm or sig. sx. - Epidural hematoma: usually 2/2 middle meningeal artery. Lens-shaped. Lucid interval. Operate for neuro degeneration or shift >5 mm - Intracerebral hematoma: frontal or temporal. can cause sig. mass effect. IVH: ventriculostomy if causing hydrocephalus DAI: dx by MRI. Supportive tx. Craniectomy if ICP elevated. **Keep ICP <20. Na>140, serum Osm 295-310, pCO2 30-35** |
|
|
Spinal tumors: #1 = _
-More likely benign if located ... -Paraganglioma => check for _ in urine. |
Spinal tumors:
-Mostly benign. #1 = neurofibroma -Intradural tumors more likely benign. Extradural more likely malignant -Paraganglioma => check for metanephrine in urine. MIBG for extramedullary chromatin tissue |
|
|
Spinothalamic tract: what type of neurons
|
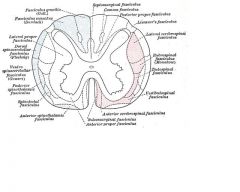
Spinothalamic tract: pain + temp sensory neurons
|
|
|
Pt has a parotid tumor that is found to be squamous cell ca.
Tx is _ |
Sq cell ca of salivary gland:
-Prophylactic MRND + post-op XRT |
|
|
During resection of a _ gland, you must find three nerves
-Mandibular branch of facial nerve -Lingual nerve -Hypoglossal nerve -which one is most likely to be injured? |
Submandibular gland resection: must find three nerves
-Marginal mandibular branch of facial nerve = most likely to be injured -Lingual nerve -Hypoglossal nerve |
|
|
what is the treatment for SAH?
|
SAH:
-2/2 cerebral aneurysms (50% MCA), AVM. also trauma -Sx: stiff neck, severe HA, photophobia, neuro deficits -goal: isolate from systemic circulation (clip vasc supply), maxmize cerebral perfusion to avoid vasospasm, prevent rebleeding -TxL hypervolemia, hypertension, hemodilution, Ca channel blockers |
|
|
Child presents c/ anterior neck mass that moves c/ tongue protrusion and swallow
Most likely is a _ |
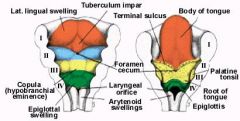
Thyroglossal duct cyst:
-Midline anterior neck mass that moves c/ tongue protrusion and swallowing -2/2 descent of thyroid gland from the foramen cecum. May be the only thyroid tissue a pt has -Resect the cyst and at least the central portion of the hyoid bone to prevent recurrence = SISTRUNK PROCEDURE |
|
|
What is the Sistrunk procedure?
|
Thyroglossal duct cyst:
-Midline anterior neck mass that moves c/ tongue protrusion and swallowing -Resect the cyst and at least the central portion of the hyoid bone to prevent recurrence = SISTRUNK PROCEDURE |
|
|
Unlike thyroglossal duct cysts, thyroid ca and branchial cleft cysts are located…
|
Thyroid ca and branchial cleft cysts are located more lateral than thyroglossal duct cysts
|
|
|
patient presents c/ dysphagia, glossitis, iron deficiency anemia. Has a mass on her tongue. Pt probably has syndrome _. Tx for tongue mass = _
|
Tongue ca:
-usually need surgery + XRT -Increased in Plummer Vinson (cervical dysphagia 2/2 esophageal web, glossitis, spoon fingers, Fe-deficiency anemia) |
|
|
a _ = painless mass on roof of mouth
-Bony exostosis @ midline |
Torus palatini= painless mass on roof of mouth
-Bony exostosis, midline of palate. Do nothing Torus mandibular = same thing on anterior lingual surface of mandible |
|
|
Massive bleeding on POD 7 s/p tracheostomy.
-Suspect _ -Avoid this problem by _ |
Tracheo-Innominate fistula:
-#1 cause of bleeding after tracheostomy -Place finger through tracheostomy site -> compress innominate artery against sternum -> to OR for median sternotomy -> ligate, divide innominate proximal to takeoff of R subclavian - should not result in any neuro dysfx due to collateral flow (some place a graft, but this carries high risk of infection) -Avoid tracheo-innominate fistula by keeping tracheostomy above the 3rd tracheal ring |
|
|
ventral nerve roots:
-afferent or efferent? -what type of fibers? |
ventral nerve roots: generally efferent. motor neuron fibers
|
|
|
Man presents c/ painless mass in parotid gland.
Most likely to be _ Tx is _ |
Warthin's tumor = adenolymphoma:
-#2 benign salivary gland tumor -Males -Bilateral in 10%; 70% of bilateral parotid tumors are Warthin's tumors -Tx: superficial parotidectomy |
|
|
Salivary gland tumor most likely to be bilateral is _
|
Warthin's tumor = adenolymphoma:
-#2 benign salivary gland tumor -Males -Bilateral in 10%; 70% of bilateral parotid tumors are Warthin's tumors -Tx: superficial parotidectomy |
|
|
Wenicke's area is located in __ lobe, responsible for _
|

Wernicke's area:
-temporal lobe -speech comprehension |

