![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
16 Cards in this Set
- Front
- Back

A teenage boy injured his hip while competing in a track meet. His radiograph is shown in Figure A. Which of the following muscles is most likely injured?
tx? |
Adolescent athletes may sustain an avulsion of the anterior inferior iliac spine (AIIS) which is due to the pull of the rectus femoris. Figure A shows a radio-density overlying the right acetabulum which is consistent with a mildly displaced AIIS avulsion in a skeletally immature patient.
tx-NSAIDS, rest, ice, stretching/strengthening,usually resolves within 4-6 weeks |
|

Rectus femoris strain
Epidemiology- MoI- |
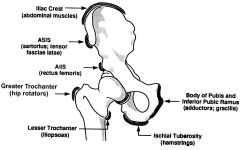
Epidemiology- seen MC in soccer and football players
MoI- sudden, forceful eccentric contraction of the muscle sprinting from standing position kicking soccer ball with great force |
|

PEI/P
provocative maneuvers x-ray findings Origin Insertion Action Arterial Supply |
PE-I/P; tenderness to palpation in the injured area, proximally at origin of rectus femoris muscle belly midthigh region distally at knee; feel for defect in muscle indicating a full tear (unusual finding)
provocative maneuvers- pain elicited with resisted hip flexion or extension x-ray- avulsion at insertion site on anterior inferior iliac spine in adolescent athletes ,normal in most cases Origin-Straight head from anterior inferior iliac spine; reflected head from groove just above acetabulum Insertion-Base of patella to form the more central portion of the quadriceps femoris tendon Action-Extends the knee Innervation-Muscular branches of femoral nerve (L2, L3, L4) Arterial Supply Lateral circumflex femoral artery |
|
|
A 60-year-old man has chronic shoulder pain and weakness. Radiographs show moderate glenohumeral arthritis and narrowing of the acromio-humeral distance. He is scheduled to undergo either hemiarthroplasty or total shoulder arthroplasty. His postoperative function will be most affected by which of the following factors?
|

The integrity of the rotator cuff
If there is an irrepairable rotator cuff tear, TSA is CONTRA-INDICATED. irrepairable rotator cuff tear-Tx options hemiarthroplasty (with limited functional outcomes) or rev TSA |
|
|
A 78-year old female sustained a 4-part proximal humerus fracture on her dominant side 2 days ago and undergoes a shoulder hemiarthroplasty. Intraoperatively, the lesser tuberosity reduction was difficult and placed too close to the greater tuberosity, which was anatomic. What post-operative problem is likely to result due to the position of the lesser tuberosity?
|

external rotation deficit
Placing the lesser tuberosity in a more lateral position will increase tension on the subscapularis and likely lead to a deficit in external rotation. |
|

CONTRA-INDICATED hemiarthroplasty (horse big one)
most common causes of failure? |
Contraindications-1 infection;2 neuropathic joint;3 unmotivated patient; 4 coracoacromial ligament deficiency provides a barrier to humeral head proximal migration in the case of a rotator cuff tear; subcutanous escape will occur if coracoacromial ligament and rotator cuff are deficient
tuberosity migration is one of the most common causes of failure with hemiarthroplasty |
|

SI for hemi artho of shoulder (pins)
|
SI-1 primary arthritis 2 if rotator cuff is deficient 3 glenoid bone stock is inadequate 4risk of glenoid loosening is high-young patients & active laborers
5 rotator cuff arthropathy 6osteonecrosis without glenoid involvement 7 proximal humerus fractures --3-part fractures with poor bone quality; 84-part fractures; 9 head-splitting fractures; 10 fracture with significant destruction of the articular surface |
|

which images?
B2.12 (RXrV &PPFs?) B2.14 RmriP/PS & MRI-fs?)MRI |
(Grashey view) true AP of shoulder- extent of DJD
delineation of fracture pattern axillary view:look for posterior wear of glenoid & helps quantify displacement in cases of fracture CT scan:determine glenoid version and glenoid bone stock, if fracture pattern is poorly understood after radiographic evaluation MRI; evaluation of rotator cuff |
|
|
A 20 year-old distance runner developed proximal tibial pain 6 weeks ago. Initially it was only painful while running, but she now has pain with walking. There is no knee effusion. The radiographs are normal. The MRI is shown. Which of the following is the most appropriate initial management?
|
Protected weight-bearing with crutches and possible use of a bone stimulator is useful early.minimum of 4-6 weeks but surgical intervention may be necessary if symptoms are not responsive to initial nonoperative treatment.
The typical posteromedial stress fracture is considered lower risk, whereas the anterior or “dreaded black line” stress fractures are considered higher risk. Ishibashi showed that MRI was better than bone scan for evaluating these injuries. |
|
|
A college football player has progressive leg pain for over 6 months, is no longer able to run and has failed non-operative treatment. His radiograph shows a linear lucency over the anterior tibia. What is the next most appropriate step to quickly return him to play?
|

Once the radiographs show the fracture especially in the anterior cortex of the tibia, surgical treatment is often recommended. This location is uncommon, but at increased risk for nonunion and propagation to complete fracture.
|
|

Which of the following stress fracture locations has the greatest likelihood of delayed healing or developing a non-union?
|
The anterior tibial cortex is a tension side stress fracture and reportedly in the article below it is a problematic area to heal. Conversely, compression side tibial stress fractures usually heal without a problem. This is true on the femoral neck as well.
|
|

def stress tibial fx
Epidemiology Mechanism Pathophysiology |
An overuse injury where normal or abnormal bone is subjected to repetitive stress, resulting in microfractures
- commonly seen in runners and military recruits seen after change in training routine -linear microfracures in trabecular bone from repetitive loading - callus formation woven bone endochondral bone formation |
|

History
Symptoms Physical exam Tx |
A- 'normal response to abnormal stress' described as a biomechanical failure of bone under repetitive, nonviolent stress. A microfracture occurs which progresses to a stress fracture with continued stress.
Hx- recent increase in running speed, shoe or track error is common. Eating disorders and menstrual irregularities have been associated with stress fractures. sx- onset of symptoms often insidious symptoms initially worse with running, then may develop symptoms with daily activities, usually describe localized pain which is relieved by rest. Pain continues to occur earlier in the training course with continued exercise. PE- point tenderness on the bone, aggravated by percussion. Surgery = reamed unlocked IM nail. |
|

Radiographs, recommended views & findings
other 2 test |
- AP and lateral
lateral xray may show "dreaded black line" anteriorly indicating tension fracture from posterior muscle force endosteal thickening periosteal reaction with cortical thickening Technetium Tc 99m bone scan- focal uptake in cortical and/or trabecular region MRI-replacing bone scan for diagnosis and is most sensitive findings; marrow edema earliest findings on T2-weighted images periosteal high signal T1-weighted images show linear zone of low signal |
|
|
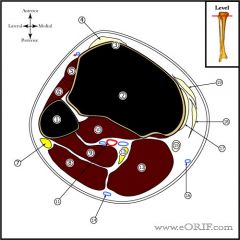
1. Fibula
11. PoplitealVessels 2. Tibia 12.Tibial Nerve 3. Tibia Tuberosity 13. Medial Head of Gastrocnemius 4. Patellar Tendon 14. Lesser Saphenous Vein 5. Tibialis Anterior 15. Gracillis 6. Extensor Digitorum Longus 16. Long Saphenous Vein 7. Common Peroneal Nerve 17. Medial Collateral Ligament 8. Lateral Head of Gastrocnemius 18. Semitendinosus 9. Soleus 19. Sartorius 10. Tibialis Posterior |
|
|
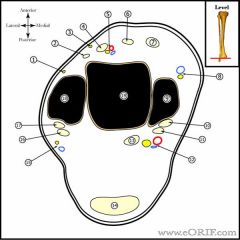
Intermediate Dorsal Cutaneous branch of Superficial peroneal nerve
10. Tibialis Posterior 2. Peroneus tertius 11. Flexor Digitorum Longus(FDL) 3. Medial Dorsal Cutaneous branch of Superficial peroneal nerve 12. Tibial Nerve and Posterior Tibial Vessels 4. Extensor Digitorum Longus 13. Flexor Hallucis Longus 5. Deep Peroneal Nerve and Anterior Tibial Vessels 14. Achilles tendon 6. Extensor Hallucis Longus 15. Sural Nerve and Lesser Saphenous Vein 7. Tibialis Anterior 16. Peroneus longus 8. Great saphenous vein and saphenous nerve 17. Peroneus brevis 9. Medial Malleolus of Tibia 18. Lateral Malleolus of Fibula 19. Talus |

