![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
70 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
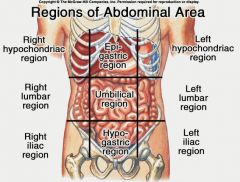
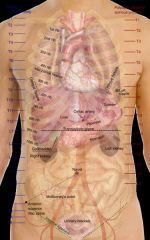
Abdominal Regions
|
|
|
|
|
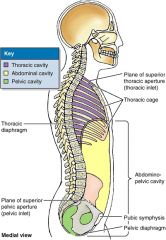
Abdominal Cavities
|
|
|
|
|
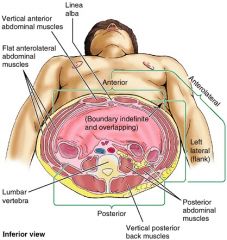
abdominal walls p.117
|
contract to increase intra-abdominal pressure but also distend considerably, musculo-aponeurotic abdominal walls = accommodating expansions caused by ingestion, pregnancy, fat deposition, or pathology.
|
|
|
|
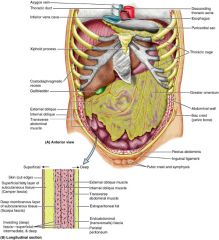
Fascia of Anterolateral Abdominal Wall p. 118
|
facial layers:
-subcutaneous tissue (superficial fascia) - lies deep to the skin and contains variable amounts of fat inferior to the umbilicus, the deepest part of the subcutaneous tissue is reinforced by many elastic and collagen fibers, so the subcutaneous tissue here has two layers : 1. superficial fatty (Camper fascia) 2. deep membranous layer (Scarpa fascia) -investing fascia (epimysium) covers the external aspects of the three muscle layers -endo-abdominal fascia - lines internal aspect of abdominal wall. can be named according to the muscle or aponeurosis it's lining. -parietal peritoneum - lines the abdominal cavity and is located internal to the transversalis fascia by extraperitoneal fat. |
|
|
|
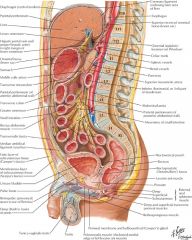
fascia abdominal wall (longitudinal section) p.118
|
|
|
|
|
Clinical significance of fascia and fascial spaces of abdominal wall (p.122)
|
surgeons use Scarpa's fascia (membranous layer of subcu. tissue) to close incisions in the abdomen because of its strength. *note: scarpa continuous with fascia lata
"potential space" where fluid may accumulate - located between the membranous layer and deep fascia covering the rectus abominis and external oblique mus. fascia lata (fascia of the thigh) prevents this fluid from spreading inferiorly into the thigh. |
|
|
|
Abdominal Surgical incisions (p. 123)
|
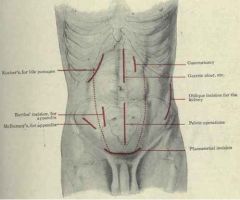
surgeons avoid transecting muscles which causes irreversible necrosis of musc. fibers Instead, they split them between their fibers.
try following Langer's lines aka tension lines (p.8) = natural orientation of collagen fibers in the dermis = less scarring or keloid, and heals faster rectus abdominis = CAN be transected* because its musc. fibers are short and its nerves entering the lateral part of the rectus sheath can be located and preserved. Common incisions: median/midline, paramedian, gridiron, transverse, suprapubic (Pfannesstiel), subcostal, and mcburney point (location of appendix) |
|
|
|
incisional hernia p. 123
|
protrusion of omentum or an organ through a surgical incision or scar.
|
|
|
|
protruberance of abdomen p. 123
|
normal in infants and young children
six F's common causes are: food, fluid, fat, feces, flatus, fetus. eversion of the umbilicus may be a sign of increased intra-abdominal pressure caused by ascites (abnormal accumulation of serous fluid in the peritoneal cavity) or a large mass like tumor, enlarged organ, or a fetus. |
|
|
|
palpation of anterolateral abdominal wall p. 123
|
guarding = involuntary abdominal musc. spasms caused by palpating with cold hands.
intense, involuntary guarding indicates pathology such as appendicitis. constitutes a clinically significant sign of acute abdomen. --> it's an attempt to guard inflamed organs within the abdomen from the pain of pressure upon them. supine position with arms at the sides, and thighs and knees semi-flexed relaxes abdominal wall |
|
|
|
endoscopic surgery . 123
|
abdominopelvic surgical procedures using endoscope
tiny perforations of the abdominal wall allow the entry of remotely operated instruments, replacing the larger conventional incisions potential for nerve injury, incisional hernia, contamination through open wound and time required for healing are minimized. |
|
|
|
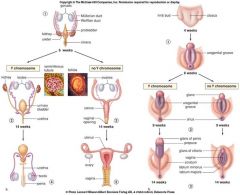
Descent of Gonads p. 133
|
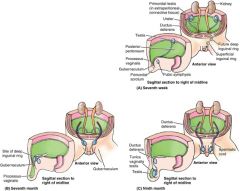
the ovaries and testes develop in the abdomen and descend to their adult anatomical positions before birth.
a fetus at 28 weeks (seventh month) shows the processus vaginalis and the testis passing through the inguinal canal. the processus vaginalis carries fascial layers of the abdominal wall before it. the remains of the processus vaginalis have formed the tunica vaginalis of the testis, and the remnant of the gubernaculum has formed the scrotal ligament or disappeared the final location of the testis usually occurs before or shortly after birth fetal ovaries - develop in the superior lumbar region of the posterior abdominal wall and migrate to the lateral wall of the pelvis (during 12th week) the processus vaginalis of the peritoneum traverses the transversalis fascia at the site of the deep inguinal ring, forming the inguinal canal as in the male, and protrudes into the developing labium majus the inguinal canals in females are narrower than those in males, and the canals in infants of both sexes are shorter and much less oblique than in adults |
|
|
|
hydrocele and hematocele p. 132
|
hydrocele of testis = presence of excess fluid in a persistent processus vaginalis. associated with indirect inguinal hernia.
detection requires transillumination - shine bright light to side of scrotum -transmission of red light indicates excess serous fluid in scrotum inflamation or injury can also produce hydrocele to the spermatic cord hematocele of the testis = collection of blood in the cavity of the tunica vaginalis. blood does not transilluminate. can distinguish b/w hydro/hematocele. |
|
|
|
vasectomy aka deferentectomy p. 132
|
a surgical procedure for male sterilization and/or permanent birth control. During the procedure, the ductus deferens are severed, and then tied/sealed to prevent sperm from entering into the urethra
however, secretions of the auxiliary genital glands (prostate, seminal and bulbourethral glands) can still be ejaculated. the testis continues to function as an endocrine gland for the production of testosterone |
|
|
|
varicocele p. 132
|
the pampiniform plexus of veins may become varicose or dilated and tortuous.
results from defective valves in the testicular vein. the palpable enlargement, which feels like a bundle of worms, usually drains and disappears when pt. lies down. |
|
|
|
testicular cancer p. 132
|
common in 20-39 years, and has one of the highest cure rates of all cancers
testes' lymphatic drainage differs from that of the scrotum. consequentlly: - cancer of the testis metastasize initially to the lumbar lymph nodes -cancer of the scrotum metastasize initially to the superficial inguinal lymph nodes. there is no link between vasectomy and testicular cancer. factors that may increase a man's risk for testicular cancer include: history of undescended testicle, klinefelter syndrome, and abnormal testicular dev. |
|
|
|
cremasteric reflex p. 132
|
light stroking of skin in medial thigh causes contraction of cremaster muscle, retraction of testes
highly active in children area supplied by ilio-inguinal nerve |
|
|
|
inguinal hernias p.134
|
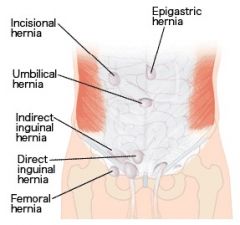
protrusion of parietal peritoneum and viscera.
2/3 are indirect hernia. direct = usual onset: adulthood. herniating bowel passes medial to inferior epigastric vessels, pushing through peritoneum and transversalis fascia in inguinal triangle to enter inguinal canal. hernia PARALLELS spermatic cord. indirect = usual onset: congenital. herniating bowel passes lateral to inferior epigastric vessels to enter deep inguinal ring. hernia is WITHIN spermatic cord. see palpation of superficial inguinal ring |
|
|
|
palpation of superficial inguinal ring p. 135
|
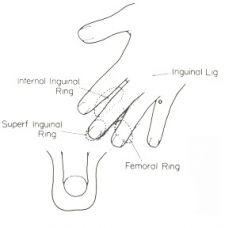
used for examining ing. hernias
palpable superolateral to the pubic tubercle by invaginating the skin of the upper scrotum with the index finger. examiner's finger follows the spermatic cord superolaterally to the superficial ing. ring. detection of impulse during coughing/sneezing at the superficial ring and a lump at the site of the deep ring suggests an INDIRECT hernia. palpation of DIRECT hernia - place finger over the inguinal triangle and ask person to cough. if hernia is present, a forceful impulse is felt against the pad of the finger. |
|
|
|
cysts and hernias of canal of nuck p. 135
|
if processus vaginalis in females persists, it forms a small peritoneal pouch called the canal of Nuck in the ing. canal that may extend to the labium majus.
in infants, it can enlarge and form cysts that have the potential to develop into an indirect ing. hernia. |
|
|
|
peritonitis p. 141
|
infection / inflammation of the peritoneum resulting from surgical contamination or traumatic wound (gas, fecal matter, bacteria enter)
rapid absorption of toxins from peritoneal cavity leads to generalized peritonitis (widespread) which is lethal paradoxical abdominothoracic rhythm and muscle rigidity, if peritonitis and pneumonitis may be present. |
|
|
|
ascites p. 141
|
excess fluid in the peritoneal cavity. also called ascitic fluid.
may occur from from internal bleeding, portal hypertension, cancer metastasis, starvation from pain, people lie with knees flexed, breath shallowly, rapidly most common cause is advanced liver disease or cirrhosis |
|
|
|
abdominal paracentesis
|
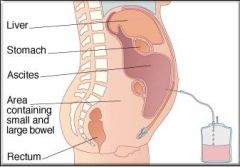
aspiration or drainage of fluid in the peritoneal cavity through linea alba.
used in treatment of generalized peritonitis that includes the removal of ascites (with antibiotics) the needle is inserted superior to the empty urinary bladder and in a location that avoids the inferior epigastric artery. |
|
|
|
peritoneal adhesions and adhesiotomy p. 141
|
injury site releases fibrin, which results in the formation or abnormal attachments (scar tissue - adhesions)
may also form after an abdominal operation. adhesions limit the normal movements of the viscera, which leads to chronic pain caused by intestinal obstruction, or volvulus (gut becomes twisted around an adhesion) tx: adhesiotomy - surgical separation of adhesions. |
|
|
|
functions of greater omentum p. 141
|
prevents the visceral peritoneum from adhering to the parietal peritoneum
it has considerable mobility and moves around the peritoneal cavity with peristaltic movements of the viscera. it often forms adhesions adjacent to an inflamed organ such as appendix, sometimes walling it off and thereby protecting other viscera from it. |
|
|
|
spread of pathological fluids p. 142
|
peritoneal recesses - spaces formed by peritoneum draping over viscera (four spaces in the abdominal cavity; the two paracolic gutters and the two paramesenteric gutters)
the recesses determine the extent and direction of the spread of fluids that may enter the peritoneal cavity when an organ is diseased or injured |
|
|
|
hiatal hernia p. 159
|
hiatal (hiatus) hernia is a protrusion of part of the stomach into the mediastinum through the esophageal hiatus of the diaphragm.
occur most often in people after middle age, because of weakening of the muscular part of the diaphragm and widening of the esophageal hiatus two main types are: paraesophageal and sliding paraesophageal = a pouch of peritoneum, often containing part of the fundus, extends trhough the esophageal hiatus anterior to the esophagus. no regurgitation because cardial orifice is in its normal position sliding = esophagus, the cardia, and parts of the fundus of the stomach slide superiorly though the eso. hiatus into the thorax. possible regurgitation of the stomach. |
|
|
|
carcinoma of stomach and gastrectomy p. 159
|
malignant tumor in the body or pyloric part of the stomach, may be palpable
gastroscopy = inspects the lining of the air inflated stomach, which allows them to observe gastric lesions and take biopsies. partial gastrectomy (removal part of the stomach - also requires removal of all involved lymph) may be performed to remove the affected part of the stomach one or more arteries may be ligate during the procedure (without damage) since the anastomoses of stomach provides good collateral circulation. all gastric nodes drain to the celiac lymph nodes of the stomach and other lymphs such as pyloric lymph, and gastro-omental lymph nodes may be removed |
|
|
|
gastric and peptic ulcers o, 159-160
|
gastric = open lesions or the mucosa of the stomach
peptic = lesions of the mucosa of the pyloric canal or more often, duodenum. caused by infection by Helicobacter pylori (H. pylori) the bacteria inflames the mucosal lining making it more susceptible to gastric acid and digestive enzyme, pepsin. if ulcer erodes into the gastric arteries, it can become life threatening. gastric secretions are controlled by the vagus nerve vagotomy (surgical section of the vagus nerve) is performed in someone with chronic or recurring ulcers to reduce the production of acids. posterior gastric ulcer = referred pain to the back as it erode through the stomach wall into the pancreas erosion of splenic artery = severe hemorrhage into the peritoneal cavity |
|
|
|
duodenal ulcers p. 160
|
inflammatory erosion of the duodenal wall located in the posterior wall of the superior part of the duodenum within 3 cm. of the pylorus.
can cause peritonitis when ulcer perforates the duodenal wall, permitting its contents to enter the peritoneal cavity liver and gallbladder may adhere to and be ulcerated erosion of the gastro-duodenal artery can result in severe hemorrhage into the peritoneal cavity |
|
|
|
appendicitis p. 160
|
acute inflammation of the appendix is a common cause of an acute abdomen (severe abdominal pain arising suddenly)
pressure over the McBurney point produces the max abdominal tenderness. pain around the periumbilical region - afferent pain fibers from T10 severe pain in the RLQ results from irritation of the parietal peritoneum laparoscopic appendectomy = standard procedure used to remove the appendix. peritoneal cavity is first inflated with CO2 to distend abdominal wall. laparascope is passed through an incision near or through the umbilicus malrotation of the intestine - location of the appendix is not in the RLQ, but instead, in the RUQ. |
|
|
|
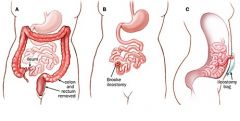
colitis, colectomy, ileostomy, colonoscopy p. 160-161
|
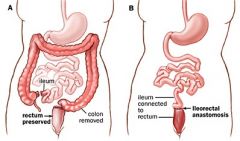
ulcerative colitis/Crohn disease = chronic inflammation of the colon characterized by severe inflammation and ulceration of the colon and rectum
colectomy = terminal ileum and colon as well as the rectum and anal canal are removed ileostomy = constructed to establish an artificial cutaneous opening b/w the ileum and the skin or the anterolateral abdominal wall colostomy/sigmoidostomy = performed after partial colectomy to create an artificial cutaneous opening for the terminal part of the colon. |
colectomy with anastomosis
|
|
|
complete colectomy with ileostomy pic.
|
|
|
|
|
colostomy pic
|
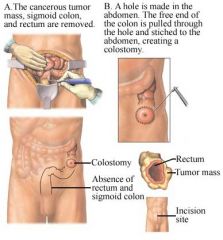
|
|
|
|
colonoscopy p. 161
|
procedure to view internal surface of the colon using a colonoscope inserted into the colon through the anus and rectum.
used for biopsies or removal of polyps, and to look for tumors interior of sigmoid colon = sigmoidscope, in a procedure called sigmoidoscopy |
|
|
|
rupture of spleen p. 165
|
protected by 9th-12th ribs.
severe blows on the left side may fracture one/more ribs and lacerate the spleen. sudden increase in intra-abdominal pressure can also rupture the spleen b/c its capsule is thin, and its parenchyma is soft and pulpy. if ruptured, the spleen bleeds profusly (since it is highly vascularized - filtration of red blood cells) - causes severe intraperitoneal hemorrhage and shock repair is difficult. splenectomy (removal of spleen) and subtotal/partial splenectomy (segments of the spleen) is often performed to prevent the pt. from bleeding to death. splenectomy - no serious side effect. it's fuxns. are assumed by other organs like liver and bone marrow. however, the person will be more susceptible to bac. infection. |
|
|
|
splenomegaly p. 165
|
spleen enlarges up to 10 or more times the normal size.
results from granulocytic leukemia (high leukocyte and WBC count) - cgl - cancer of WBC pain in left upper q sometimes accompanies hypertension. |
|
|
|
rupture pancreas p. 165
|
can result from sudden, severe, forceful compression of the abdomen from a car accident.
rupture frequently tears its duct system, allowing its juice to enter the parenchyma of the gland and to invade adjacent tissues. contact of other tissues by pancreatic juice is very painful |
|
|
|
pancreatic cancer p. 165
|
cancer involving the pancreatic head accounts for most cases of extrahepatic obstruction of the biliary duct.
cancer of the head often compresses and obstructs the bile duct and/or the hepatopancreatic ampulla, resulting in the retention of the bile pigments, enlargement of the gallbladder, and jaundice (obstructive jaundice) presents w/ severe back pain cancer of neck may cause portal or IVCaval obstruction b/c pancreas overlies these veins typical for early metastasis to liver via portal vein - surgical resection of cancerous pancreas nearly futile most people with pancreatic cancer have ductular adenocarcinoma |
|
|
|
hepatic lobectomies and segmentectomy p. 173
|
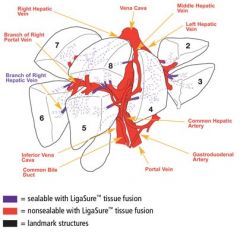
hepatic lobectomies = right/left part of the liver can be removed with minimal bleeding -- since R and L hepatic arteries and ducts, as well as branches of the R/L hepatic portal veins do not communicate significantly.
sementectomy = for a more severe injuries/tumors that involve one segment of adjacent segments. - use intersegmental hepatic veins as guides to interlobar planes. |
|
|
|
liver biopsies p. 173
|
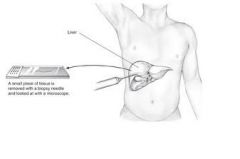
collect hepatic tissue with needle through the right 10th intercostal space in the midaxillary line.
person is asked to hold breath in full expiration to reduce the costodiaphragmatic recess to avoid lung and pleural cavity contamination |
|
|
|
cirrhosis p. 173
|
hepatocytes are destroyed and replaced by fibrous tissue. fibrous tiss. surrounds the intrahepatic blood vessels ad biliary ducts making liver firm/ ischemic
portal hypertension - caused by cirrhosis and freq. develops in chronic alcoholics tx: portosystemic or portocaval shunt (to relieve pressure) s/sx: ascites, splenomegaly... |
|
|
|
rupture of liver p. 173
|
easily injured b/c of its size, fixed position, and friability (crumbles easily)
caused by rib fracture and can result in considerable hemorrhage and RUQ pain surgical discretion to remove liver or simply remove contaminating material |
|
|
|
gallstones p. 173
|
concretion in gallbladder, cystic duct, or bile duct composed of cholesterol crystals
hepatopancreatic ampulla - narrowest and most easily obstructed area must be big enough to produce injury to gallbladder or obstruction of the biliary tract to cause any clinical symptoms can cause biliary colic – stone lodged in the cystic duct (intense, spasmodic pain in the epigastric region) -- can cause cholecystitis cholecystitis – inflammation of gallbladder when stone blocks the cystic duct due to bile accumulation, and enlargement of gallbladder pain in 9th intercostals space at semilunar line, some posterior thoracic wall and shoulder pain with irritation of the diaphragm jaundice – yellowing of skin when bile cannot leave the gallbladder so it enters the blood and causes obstructive jaundice - can be caused by pancreatic cancer* |
|
|
|
portal hypertension p. 174 see also cirrhosis of liver
|
pressure rises in the hepatic portal vein caused by cirrhosis of liver.
produces enlarged varicose veins at the sites of anastomoses b/w portal and systemic viens. as a result, veins become so dilated their walls rupture = hemorrhage. esophageal varices (dilated esophageal veins) = fatal to reduce portal hypertension, create communication b/w portal vein and IVC or join the splenic and left renal veins -> a portacaval anastomosis or portosystemic shunt. |
|
|
|
renal transplant p. 181
|
for tx. of chronic renal failure
site of transplanted kidney is in the iliac fossa of the greater pelvis, where it is firmly supported and where only short lengths of renal vessels and ureters are required. also kidney can be removed from donor leaving the suprarenal gland intact due to a weak septum that separates the two renal artery and vein are joined to the external iliac artery and vein, ureter is sutured into the bladder |
|
|
|
renal and ureteric calculi p. 181
|
renal calculus (kidney stone) = causes severe intermittent pain, ureteric colic from excessive distention of the ureter.
calculus may cause complete/intermittent obstruction of urinary flow. pain may be referred to the lumbar (loin) or inguinal regions (groin) depending on the level of obstruction. may also be felt at the proximal anterior asp. of the thigh, or the external genitalia/testis. pain is referred to the cutaneous areas which supply the ureter -> T11- L2. ureteric calculi can be removed with a nephroscope or lithtripsy (that uses shock wave to break the stones, which then pass with the urine) |
|
|
|
accessory renal vessels p. 181
|
during ascent to final state, the embryonic kidneys receive blood supply and venous drainage from superior vessels, eventually taking over the inferior vessels.
but failure of inf. vessels to degenerate results in accessory (or polar) renal arteries and veins. occur in 25% of pop. |
|
|
|
section of phrenic nerve p. 191
|
section of a phrenic nerve in the neck results in complete paralysis and eventual atrophy of the musc. part of the the diaphragm (unless pt. has accessory phrenic nerve)
paralysis of hemidiaphragm can be recognized radiographically by its permanent elevation and paradoxical movement. |
|
|
|
rupture of diaphragm and herniation of viscera p. 191
|
result from a sudden large increase in intrathoracic/intra-abdominal press. -- from severe trauma
95% on the left said because the substantial mass of the liver, provides phys. barrier. lumbocostal triangle ( http://1.bp.blogspot.com/-MKgus_FUk2E/TVzmar4gk6I/AAAAAAAACPU/6aU7LsvsgOE/s1600/Weak%2Bareas.png) = nonmuscular area b/w costal and lumbar parts of diaphragm is common site of traumatic diaphragmatic hernia hiatal/ hiatus hernia = protrusion of part of stomach into thorax through the esophageal hiatus (vagal trunks, left. inf. phrenic vessels, esophageal branches of the left gastric vessels that runs through it may be injured during surgical procedures on eso. hiatus. eg; repair of hernia) |
|
|
|
AAA p. 198
|
rupture of an aneurysm (localized enlargement) of abdominal aorta causes severe pain in the abdomen or back.
pulsations can be detected to the left of the midline and confirmation of diagnosis with imaging mortality rate of 90% from blood loss repair by opening it, inserting a prosthetic graft, and sewing the wall over the graft to protect it. other tx; endovascular catheterization procedures. compression of aorta against L4 vertebra can control bleeding of pelvis or lower limbs |
|
|
|
anterior ab. wall musc.
|
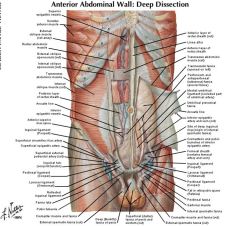
Linear alba: midline where rectus sheath fuses - (formed by the fusion of the aponeuroses of the abdominal muscles), and it separates the left and right rectus abdominis muscles.
*L. Alba doesn't contain important nerves or blood vessels, a median incision through the linea alba is a common surgical approach. Rectus Sheath - formed by the aponeuroses of the Obliqui and Transversus. It contains the Rectus abdominis and Pyramidalis muscles. * the fibers of the rectus sheath are oriented for flexing the trunk. Arcuate line: 5-6cm below umbilicus - level where posterior wall of rectus sheath finishes and where all 3 anterior wall muscles (external and internal oblique and transversalis abdominis) lie anterior to the rectus abdominis Transpyloric plane: 1/2 between suprasternal notch and pubic symphysis |
|
|
|
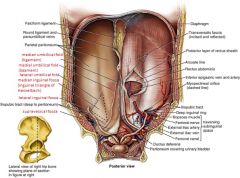
Inguinal and Femoral regions (pic.)
|
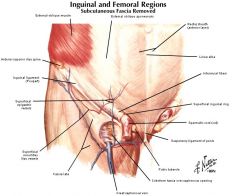
Inguinal ligament: lower free edge of external oblique
Lacunar ligament: medial curved fibres of inguinal ligament that pass upwards and backwards to attach to pectineal line Inguinal canal: 4cm tunnel in lower, anterior abdominal muscles that runs downwards and medially between the deep and superficial rings Deep inguinal ring: hole in transversalis fascia lying 3cm superior to the midpoint of the inguinal ligament Superficial inguinal ring: V-shaped defect in the lower medial fibres of the external oblique just superior and lateral to the pubic tubercle |
|
|
|
Ing. region - internal post. view
|
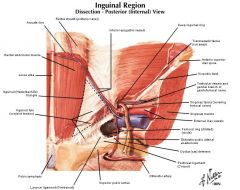
Site of direct inguinal herniation
Borders 1)Lateral: inferior epigastric artery 2)Medial: lateral edge of rectus abdominis 3)Inferior: inguinal ligament |
|
|
|
Post. Ab. wall - internal view
|
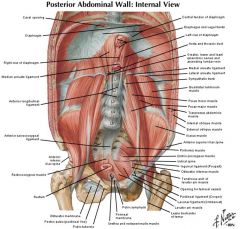
Supracrista plane: transverse line along upper aspects of the iliac crests passing through spinous process of L4 vertebra
Useful aid in lumbar puncture for either L3/4 or L4/5 spaces |
|
|
|
Embryology of internal genitalia P.1
|
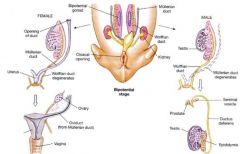
On each side of the embryo, a primitive gonad arises from the genital ridge, a condensation of tissue near the adrenal gland. The gonad develops a cortex and a medulla
Until the sixth week of development, these structures are identical in both sexes. In genetic males, the medulla develops during the seventh and eighth weeks into a testis, and the cortex regresses. Leydig and Sertoli cells appear, and testosterone and MIS are secreted. In genetic females, the cortex develops into an ovary and the medulla regresses. The embryonic ovary does not secrete hormones. Hormonal treatment of the mother has no effect on gonadal (as opposed to ductal and genital) differentiation in humans |
|
|
|
Embryology of int. genitalia P. 2
|
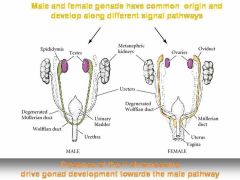
In the seventh week of gestation, the embryo has both male and female primordial genital duct.
In a normal female fetus, the müllerian duct system then develops into uterine tubes (fallopian tubes/oviducts), a uterus, and part of the vagina. - under the influence of ovarian hormones In the normal male fetus, the wolffian duct system on each side develops into the epididymis and vas deferens (under the influence of testosterone* produced in the testes) the mullerian ducts regress in response to anti-mullerian hormone, which is also produced in the testes. When the embryo has functional testes, male internal and external genitalia develop. The Leydig cells of the fetal testis secrete testosterone, and the Sertoli cells secrete müllerian inhibiting substance (MIS; also called müllerian regression factor, or MRF). In their effects on the internal as opposed to the external genitalia, MIS and testosterone act unilaterally. MIS causes regression of the müllerian ducts by apoptosis on the side on which it is secreted, and testosterone fosters the development of the vas deferens and related structures from the wolffian ducts. The testosterone metabolite dihydrotestosterone induces the formation of male external genitalia and male secondary sex characteristics. The external genitalia are similarly bipotential until the eighth week . Thereafter, the urogenital slit disappears and male genitalia form, or, alternatively, it remains open and female genitalia form. |
|
|
|
Dev. of internal and external genitalia
|
|
|
|
|
Rectus Sheath
|
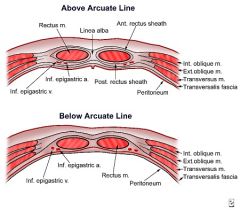
formed by the aponeuroses of the Obliqui and Transversus. It contains the Rectus abdominis and Pyramidalis muscles.
It can be divided into anterior and posterior laminae. superficial layer (fascia of Camper) is a thick superficial layer of the anterior abdominal wall deep layer (fascia of Scarpa) is a layer of the anterior abdominal wall. It is found deep to the Camper Fascia and superficial to the External Oblique muscle. |
|
|
|
constituents of spermatic cord
|
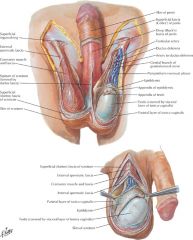
"3 arteries, 3 nerves, 3 other things":
3 arteries: testicular, ductus deferens, cremasteric. 3 nerves: genital branch of the genitofemoral, cremasteric, autonomics. 3 other things: ductus deferens, pampiniform plexus, lymphatics. the deep inguinal ring is a structural weak point in the abd. wall which forms the entrance to the inguinal canal. this canal provides a path for the descent of the testes during normal developments, but also creates a potential route for the herniation of abdominal visceral (indirect ing. hernia) |
|
|
|
Parietal peritoneum
|
peritoneum = divides the abdomen and pelvis into a serous cavity, the peritoneal cavity, and connective-tissue space, the extraperitoneal space.
* peritoneum = greater sac vs. lesser sac --> lesser sac = lesser/greater omentum omental bursa aka lesser sac = the cavity in the abdomen that is formed by the lesser/greater omentum. it is connected with the greater sac via epiploic foramen (aka "foramen of Winslow") the peritoneal cavity = lined by parietal peritoneum and surrounded on all sides by the extraperitoneal cavity (with organs not in contact with the peritoneum when formed). the lowest part of peritoneal cavity for women = rectouterine pouch (cul-de-sac) and male = rectovesical pouch -- blood, pus, or tumor may collect at the site as a result of intra-ab. inflammation--- impt. in needle aspiration* |
|
|
|
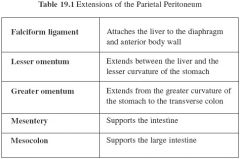
extensions of parietal peritoneum
|
mesentery = transmits the nuerovascular. structures that supply the intraperitoneal organs. -the presence of mesentery causes the intraperitoneal organs to have greater mobility than extraperitoneal organs.
peritoneal/umbilical folds = median umbilical fold --> where the parietal peritoneum covers the median umbilical ligament (incomplete obliteration of this structure's remnant/urachnus may lead to unbilical fistulae) |
|
|
|
retroperitoneal space and organs
|
anatomical space locate behind the peritoneum
organs only have peritoneum on their anterior side *retroperitoneal ogans: Susprarenal Aaorta/ivc Duodenum Pancreas Uterus Colon Kidneys Esophagus Rectum (sadpucker) secondary retroperitoneal organs are: pancreas, duodenum, and colon. the rest are primary |
|
|
|
midgut rotaton
|
see p. 178-179 of THEIME **
|
|
|
|
porto-systemic shunt/anastomosis
|

PSA = is a specific type of anastomosis that occurs between the veins of portal circulation and those of systemic circulation. The lower end of esophagus is one of the important sites for the portosystemic anastomosis . In portal hypertension as in the case of cirrhosis of liver the anastomosis opens and forms venous dilatation called esophageal varices. Their rupture causes severe and dangerous haematesis (hematemesis).
Portosystemic shunts (PSS) are vascular anomalies that divert blood from the abdominal viscera to the heart, bypassing the hepatic sinusoids and carrying intestinal absorption products directly to the systemic circulation. Portosystemic shunts can be classified as extrahepatic or intrahepatic, single or multiple, and congenital or acquired. Types of single congenital portovascular anomalies include intrahepatic portocaval shunts (i.e. patent ductus venosus) and extrahepatic portocaval or portal-azygos shunts. In a small percentage of dogs, the prehepatic portal vein is also congenitally absent. |
|
|
|
functions of anterolateral ab. wall musc. p. 120
|
external and internal oblique = compresses and support ab. viscera; flex and rotate trunk
transverse abdominis = comresses and supports ab. viscera rectus ab. = flexes trunk (lumbar vertebrae) and compresses abdominal viscera; stabilizes and controls tilt of pelvis (antilordosis) all musc. are innervated by thoraco-abdominal nerves T7-T11 + subcostal nerve and first lumbar nerve. |
|
|
|
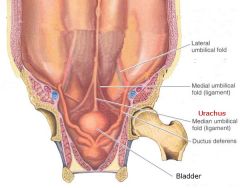
five umbilical peritoneal folds
|
two on each side and one in the median plane pass toward the umbilicus
median = covers median umbilical ligament, the remnant of the urachus that joined the apex of the fetal bladder to the umbilicus two medial folds two lateral umbilical folds |
|
|
|
peritoneal folds and fossae p. 121
|
potential sites for hernia
Five umbilical peritoneal folds two on each side and one in the median plane pass toward the umbilicus: The median umbilical fold extends from the apex of the urinary bladder to the umbilicus and covers the median umbilical ligament, the remnant of the urachus, which joined the apex of the fetal bladder to the umbilicus. Two medial umbilical folds, lateral to the median umbilical fold, cover the medial umbilical ligaments, formed by occluded parts of the umbilical arteries. * also called inguinal triangles (Hesselbach triangles) - common sites for direct inguinal hernias Two lateral umbilical folds, lateral to the medial umbilical folds, cover the inferior epigastric vessels and therefore bleed if cut. |
|
|
|
palpation of superficial inguinal ring
|
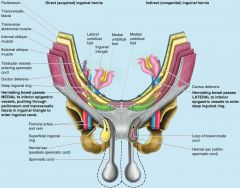
The superficial inguinal ring is palpable superolateral to the pubic tubercle by invaginating the skin of the upper scrotum with the index finger. The examiner's finger follows the spermatic cord superolaterally to the superficial inguinal ring. If the ring is dilated, it may admit the finger without causing pain. Should a hernia be present, a sudden impulse is felt against either the tip or pad of the examining finger when the patient is asked to cough. However, because both inguinal hernia types exit the superficial ring, palpation of an impulse at this site does not discriminate type. With the palmar surface of the finger against the anterior abdominal wall, the deep inguinal ring may be felt as a skin depression superior to the inguinal ligament.
Detection of an impulse at the superficial ring and a mass at the site of the deep ring suggests an indirect hernia. Palpation of a direct inguinal hernia is performed by placing the palmar surface of the index and/or middle finger over the inguinal triangle and asking the person to cough or bear down (strain). If a hernia is present, a forceful impulse is felt against the pad of the finger. The finger can also be placed in the superficial inguinal ring; if a direct hernia is present, a sudden impulse is felt medial to the finger when the person coughs or bears down. |
|
|
|
midgut rotation p. 155
|
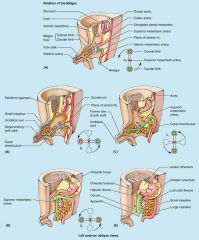
An understanding of the rotation of the midgut clarifies the adult arrangement of the intestines. The primordial gut comprises the foregut, midgut, and hindgut.
Pain arising from foregut derivatives esophagus, stomach, pancreas, duodenum, liver, and biliary ducts localizes in the epigastric region. Pain arising from midgut derivatives the small intestine distal to bile duct, cecum, appendix, ascending colon, and most of the transverse colon localizes in the periumbilical region. Pain arising from hindgut derivatives the distal part of the transverse colon, descending colon, sigmoid colon, and rectum localizes in the hypogastric region. For 4 weeks, the rapidly growing midgut, supplied by the SMA, is physiologically herniated into the proximal part of the umbilical cord. It is attached to the yolk sac by the yolk stalk. As it returns to the abdominal cavity, the midgut rotates 270 degrees around the axis of the SMA. As the relative size of the liver and kidneys decreases, the midgut returns to the abdominal cavity as increased space becomes available. As the parts of the intestine reach their definitive positions, their mesenteric attachments undergo modification. Some mesenteries shorten and others disappear (e.g., most of duodenal mesentery). Malrotation of the midgut results in several congenital anomalies such as volvulus (twisting) of the intestine. |
|

