![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
535 Cards in this Set
- Front
- Back
|
A 70yo M with h/o HTN and DM presents with a 2-mo h/o increasing paroxysmal nocturnal dyspnea and SOB with minimal exertion. An echocardiogram shows an ejection fraction of 25%. Which one of the patients current medications should be discontinued?
A. Lisinopril (Zestril) B. Pioglitazone (Actos) C. Glipizide (Glucotrol) D. Metoprolol (Toprol-XL) |
Pioglitzaone
thiazolidinediones (TZDs) are associated with fluid retention, and their use can be complicated by the development of heart failure. Caution is necessary when prescribing TZDs in patients with known heart failure or other heart diseases, those with preexisting edema, and those on concurrent insulin therapy |
|
|
What is the most common cause of hypertension in children under 6 years of age?
|
Renal Parenchymal Disease
The most common cause of hypertension is renal parenchymal disease, and a urinalysis, urine culture, and renal ultrasonography should be ordered for all children presenting with hypertension. |
|
|
A 72-year-old African-American male with New York Heart Association Class III heart failure sees you for follow-up. He has shortness of breath with minimal exertion. The patient is adherent to his medication regimen. His current medications include lisinopril (Prinivil, Zestril), 40 mg twice daily; carvedilol (Coreg), 25 mg twice daily; and furosemide (Lasix), 80 mg daily. His blood pressure is 100/60 mm Hg, and his pulse rate is 68 beats/min and regular. Findings include a few scattered bibasilar rales on examination of the lungs, an S3 gallop on examination of the heart, and no edema on examination of the legs. An EKG reveals a left bundle branch block, and echocardiography reveals an ejection fraction of 25%, but no other abnormalities. What's the appropriate next step?
|
Refer for cardiac resynchronization therapy (CRT)
Note: he's already on maximum doses of ACEI, loop diuretic, beta-blocker Using a pacemaker-like device, CRT aims to get both ventricles contracting simultaneously, overcoming the delayed contraction of the left ventricle caused by the left bundle-branch block. These guidelines were refined by an April 2005 AHA Science Advisory, which stated that optimal candidates for CRT have a dilated cardiomyopathy on an ischemic or nonischemic basis, an LVEF ≤0.35, a QRS complex ≥120 msec, and sinus rhythm, and are NYHA functional class III or IV despite maximal medical therapy for heart failure. |
|
|
What dietary change recommended for the prevention and treatment of cardiovascular disease has been shown to decrease the rate of sudden death?
|
increase intake of omega 3 fatty acids
Omega-3 fats contribute to the production of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), which inhibit the inflammatory immune response and platelet aggregation, are mild vasodilators, and may have antiarrhythmic properties. The American Heart Association guidelines state that omega-3 supplements may be recommended to patients with preexisting disease, a high risk of disease, or high triglyceride levels, as well as to patients who do not like or are allergic to fish. The Italian GISSI study found that the use of 850 mg of EPA and DHA daily resulted in decreased rates of mortality, nonfatal myocardial infarction, and stroke, with particular decreases in the rate of sudden death. |
|
|
A 75-year-old male presents to the emergency department with a several-hour history of back pain in the interscapular region. His medical history includes a previous myocardial infarction (MI) several years ago, a history of cigarette smoking until the time of the MI, and hypertension that is well controlled with hydrochlorothiazide and lisinopril (Prinivil, Zestril). The patient appears anxious, but all pulses are intact. His blood pressure is 170/110 mm Hg and his pulse rate is 110 beats/min. An EKG shows evidence of an old inferior wall MI but no acute changes. A chest radiograph shows a widened mediastinum and a normal aortic arch, and CT of the chest shows a dissecting aneurysm of the descending aorta that is distal to the proximal abdominal aorta but does not involve the renal arteries. Which one of the following would be the most appropriate next step in the management of this patient?
|
Dx: aortic dissection
next step: Intravenous labetalol (Normodyne, Trandate) Initial management should reduce the systolic blood pressure to 100-120 mm Hg or to the lowest level tolerated. The use of a β-blocker such as propranolol or labetalol to get the heart rate below 60 beats/min should be first-line therapy. If the systolic blood pressure remains over 100 mm Hg, intravenous nitroprusside should be added. Without prior beta-blocade, vasodilation from the nitroprusside will induce reflex activation of the sympathetic nervous system, causing increased ventricular contraction and increased shear stress on the aorta. |
|
|
According to the U.S. Preventive Services Task Force, what are the screening recommendations for an abdominal aortic aneurysm?
|
The guideline recommends one-time screening with ultrasonography for AAA in men 65-75 years of age who have ever smoked. No recommendation was made for or against screening women. Men with a strong family history of AAA should be counseled about the risks and benefits of screening as they approach 65 years of age.
|
|
|
A 36-year-old white female presents to the emergency department with palpitations. Her pulse rate is 180 beats/min. An EKG reveals a regular tachycardia with a narrow complex QRS and no apparent P waves. The patient fails to respond to carotid massage or to two doses of intravenous adenosine (Adenocard), 6 mg and 12 mg. The most appropriate next step would be to administer intravenous
|
verapamil (Calan)
If supraventricular tachycardia is refractory to adenosine or rapidly recurs, the tachycardia can usually be terminated by the administration of intravenous verapamil or a β-blocker. If that fails, intravenous propafenone or flecainide may be necessary. It is also important to look for and treat possible contributing causes such as hypovolemia, hypoxia, or electrolyte disturbances. Electrical cardioversion may be necessary if these measures fail to terminate the tachyarrhythmia. |
|
|
The blood pressure goal for a patient who has uncomplicated diabetes mellitus is
|
BP goal: 130/80mmHg
Aggressive control of blood pressure to <135/85 mm Hg in hypertensive patients and to <130/80 mm Hg in diabetic patients is recommended. Lowering blood pressure may reduce stroke rates by 40%-52% and cardiovascular morbidity by 18%-20% |
|
|
A 60-year-old African-American female has a history of hypertension that has been well controlled with hydrochlorothiazide. However, she has developed an allergy to the medication. Successful monotherapy for her hypertension would be most likely with which one of the following?
A. Lisinopril (Prinivil, Zestril) B. Hydralazine (Apresoline) C. Clonidine (Catapres) D. Atenolol (Tenormin) E. Diltiazem (Cardizem) |
Diltiazem (Cardizem)
Monotherapy for hypertension in African-American patients is more likely to consist of diuretics or calcium channel blockers than β-blockers or ACE inhibitors. It has been suggested that hypertension in African-Americans is not as angiotensin II-dependent as it appears to be in Caucasians. |
|
|
An asymptomatic 3-year-old male presents for a routine check-up. On examination you notice a systolic heart murmur. It is heard best in the lower precordium and has a low, short tone similar to a plucked string or kazoo. It does not radiate to the axillae or the back and seems to decrease with inspiration. The remainder of the examination is normal. What is the most likely diagnosis?
|
Still’s murmur
There are several benign murmurs of childhood that have no association with physiologic or anatomic abnormalities. Of these, Still’s murmur best fits the murmur described. The cause of Still’s murmur is unknown, but it may be due to vibrations in the chordae tendinae, semilunar valves, or ventricular wall. |
|
|
A 57-year-old male with severe renal disease presents with acute coronary syndrome. Which one of the following would most likely require a significant dosage adjustment from the standard protocol?
A. Enoxaparin (Lovenox) B. Metoprolol (Lopressor, Toprol) C. Carvedilol (Coreg) D. Clopidogrel (Plavix) E. Tissue plasminogen activator (tPA) |
Enoxaparin
Enoxaparin is eliminated mostly by the kidneys. When it is used in patients with severe renal impairment the dosage must be significantly reduced. For some indications the dose normally given every 12 hours is given only every 24 hours. Although some β-blockers require a dosage adjustment, metoprolol and carvedilol are metabolized by the liver and do not require dosage adjustment in patients with renal failure. Clopidogrel is currently recommended at the standard dosage for patients with renal failure and acute coronary syndrome. Thrombolytics like tPA are given at the standard dosage in renal failure, although hemorrhagic complications are increased. |
|
|
A 55-year-old male who has a long history of marginally-controlled hypertension presents with gradually increasing shortness of breath and reduced exercise tolerance. His physical examination is normal except for a blood pressure of 140/90 mm Hg, bilateral basilar rales, and trace pitting edema. What study would be the preferred diagnostic tool for evaluating this patient?
|
2-dimensional echocardiography with Doppler
The most useful diagnostic tool for evaluating patients with heart failure is two-dimensional echocardiography with Doppler to assess left ventricular ejection fraction (LVEF), left ventricular size, ventricular compliance, wall thickness, and valve function. The test should be performed during the initial evaluation. Radionuclide ventriculography can be used to assess LVEF and volumes, and MRI or CT also may provide information in selected patients. Chest radiography (posteroanterior and lateral) and 12-lead electrocardiography should be performed in all patients presenting with heart failure, but should not be used as the primary basis for determining which abnormalities are responsible for the heart failure. |
|
|
A 23-year-old female sees you with a complaint of intermittent irregular heartbeats that occur once every week or two, but do not cause her to feel lightheaded or fatigued. They last only a few seconds and resolve spontaneously. She has never passed out, had chest pain, or had difficulty with exertion. She is otherwise healthy, and a physical examination is normal. What cardiac study should be ordered initially?
|
EKG
The symptom of an increased or abnormal sensation of one’s heartbeat is referred to as palpitations. This condition is common to primary care, but is often benign. Commonly, these sensations have their basis in anxiety or panic. However, about 50% of those who complain of palpitations will be found to have a diagnosable cardiac condition. It is recommended to start the evaluation for cardiac causes with an EKG, which will assess the baseline rhythm and screen for signs of chamber enlargement, previous myocardial infarction, conduction disturbances, and a prolonged QT interval. |
|
|
What is most appropriate for the initial treatment of claudication?
|
regular exercise
Claudication is exercise-induced lower-extremity pain that is caused by ischemia and relieved by rest. It affects 10% of persons over 70 years of age. However, up to 90% of patients with peripheral vascular disease are asymptomatic. Initial treatment should consist of vigorous risk factor modification and exercise. Patients who follow an exercise regimen can increase their walking time by 150%. A supervised program may produce better results. Risk factors include diabetes mellitus, hypertension, smoking, and hyperlipidemia. |
|
|
In a patient who presents with symptoms of acute myocardial infarction, which one of the following would be an indication for thrombolytic therapy?
A. New-onset ST-segment depression B. New-onset left bundle branch block C. New-onset first degree atrioventricular block D. New-onset Wenckebach second degree heart block E. Frequent unifocal ventricular ectopic beats |
New-onset left bundle branch block
In patients with ischemic chest pain, the EKG is important for determining the need for fibrinolytic therapy. Myocardial infarction is diagnosed by ST elevation ≥1 mm in two or more limb leads and ≥2 mm in two or more contiguous precordial leads. In a patient with an MI, new left bundle branch block suggests occlusion of the left anterior descending artery, placing a significant portion of the left ventricle in jeopardy. Thrombolytic therapy could be harmful in patients with ischemia but not infarction – they will show ST-segment depression only. Frequent unifocal ventricular ectopy may warrant antiarrhythmic therapy, but not thrombolytic therapy. |
|
|
A 68-year-old female has an average blood pressure of 150/70 mm Hg despite appropriate lifestyle modification efforts. Her only other medical problems are osteoporosis and mild depression. The most appropriate treatment at this time would be
A. lisinopril (Prinivil, Zestril) B. clonidine (Catapres) C. propranolol (Inderal) D. amlodipine (Norvasc) E. hydrochlorothiazide |
HCTZ
Randomized, placebo-controlled trials have shown that isolated systolic hypertension in the elderly responds best to diuretics and to a lesser extent, β-blockers. Diuretics are preferred, although long-acting dihydropyridine calcium channel blockers may also be used. In the case described, β-blockers or clonidine may worsen the depression. Thiazide diuretics may also improve osteoporosis, and would be the most cost-effective and useful agent in this instance. |
|
|
A 56-year-old white male presents with a 2-week history of intermittent pain in his left leg. The pain usually occurs while he is walking and is primarily in the calf muscle or Achilles region. Sometimes he will awaken at night with cramps in the affected leg. He has no known risk factors for atherosclerosis. What would be the best initial test for peripheral vascular occlusive disease?
|
Ankle-brachial index (ABI)
The ankle-brachial index (ABI) is an inexpensive, sensitive screening tool and is the most appropriate first test for peripheral vascular occlusive disease (PVOD) in this patient. The ABI is the ratio of systolic blood pressure measured in the ankle to systolic pressure using the standard brachial measurement. A ratio of 0.9-1.2 is considered normal. Severe disease is defined as a ratio <0.50. More invasive and expensive testing using Doppler ultrasonography, arteriography, or magnetic resonance angiography may be useful if the ABI suggests an abnormality. Venous ultrasonography would not detect PVOD, but it could rule out deep venous thrombosis, which is another common etiology for calf pain. |
|
|
A 69-year-old male has a 4-day history of swelling in his left leg. He has no history of trauma, recent surgery, prolonged immobilization, weight loss, or malaise. His examination is unremarkable except for a diffusely swollen left leg. A CBC, chemistry profile, prostate-specific antigen level, chest radiograph, and EKG are all normal; however, compression ultrasonography of the extremity reveals a clot in the proximal femoral vein. He has no past history of venous thromboembolic disease. In addition to initiating therapy with low molecular weight heparin, the American College of Chest Physicians recommends that warfarin (Coumadin) be instituted now and continued for how long?
|
3 months
For patients with a first episode of unprovoked deep venous thrombosis, evidence supports treatment with a vitamin K antagonist for at least 3 months (SOR A). The American College of Chest Physicians recommends that patients be evaluated at that point for the potential risks and benefits of long-term therapy |
|
|
You see a 23-year-old gravida 1 para 0 for her prenatal checkup at 38 weeks gestation. She complains of severe headaches and epigastric pain. She has had an uneventful pregnancy to date and had a normal prenatal examination 2 weeks ago. Her blood pressure is 140/100 mm Hg. A urinalysis shows 2+ protein; she has gained 5 lb in the last week, and has 2+ pitting edema of her legs. The most appropriate management at this point would be:
|
next step: Admitting the patient to the hospital, treating with parenteral magnesium sulfate, and planning prompt delivery either vaginally or by cesarean section
This patient manifests a rapid onset of preeclampsia at term. The symptoms of epigastric pain and headache categorize her preeclampsia as severe. These symptoms indicate that the process is well advanced and that convulsions are imminent. Treatment should focus on rapid control of symptoms and delivery of the infant. |
|
|
A 67-year-old Hispanic male comes to your office with severe periumbilical abdominal pain, vomiting, and diarrhea which began suddenly several hours ago. His temperature is 37.0 degrees C (98.6 degrees F), blood pressure 110/76 mm Hg, and respirations 28/min. His abdomen is slightly distended, soft, and diffusely tender; bowel sounds are normal. Other findings include clear lungs, a rapid and irregularly irregular heartbeat, and a pale left forearm and hand with no palpable left brachial pulse. Right arm and lower extremity pulses are normal. Urine and stool are both positive for blood on chemical testing. His hemoglobin level is 16.4 g/dL (N 13.0–18.0) and his WBC count is 25,300/mm3 (N 4300–10,800). The diagnostic imaging procedure most likely to produce a specific diagnosis of his abdominal pain is:
A. Intravenous pyelography (IVP) B. Sonography of the abdominal aorta C. A barium enema D. Celiac and mesenteric arteriography E. Contrast venography |
Celiac and mesenteric arteriography
The sudden onset of severe abdominal pain, vomiting, and diarrhea in a patient with a cardiac source of emboli and evidence of a separate embolic event makes superior mesenteric artery embolization likely. In this case, evidence of a brachial artery embolus and a cardiac rhythm indicating atrial fibrillation suggest the diagnosis. Some patients may have a surprisingly normal abdominal examination in spite of severe pain. Microscopic hematuria and blood in the stool may both occur with embolization. Severe leukocytosis is present in more than two-thirds of patients with this problem. Diagnostic confirmation by angiography is recommended. Immediate embolectomy with removal of the propagated clot can then be accomplished and a decision made regarding whether or not the intestine should be resected. A second procedure may be scheduled to reevaluate intestinal viability. |
|
|
A 49-year-old white female comes to your office complaining of painful, cold finger tips which turn white when she is hanging out her laundry. While there is no approved treatment for this condition at this time, what drug has been shown to be useful?
|
Nifedipine (Procardia)
At present there is no approved treatment for Raynaud’s disease. However, patients with this disorder reportedly experience subjective symptomatic improvement with calcium channel antagonists. Nifedipine is the calcium channel blocker of choice in patients with Raynaud’s disease. Beta-blockers can produce arterial insufficiency of the Raynaud type, so propranolol and atenolol would be contraindicated. Drugs such as ergotamine preparations and methysergide can produce cold sensitivity, and should therefore be avoided in patients with Raynaud’s disease. |
|
|
You perform a health maintenance examination on a 2-year-old white male. He is asymptomatic and is meeting all developmental milestones. The only significant finding is a grade 3/6 diastolic murmur heard at the right upper sternal border. Which one of the following would be most appropriate at this time?
|
Referral to a pediatric cardiologist
Children who have a murmur that is diastolic or is greater than 2/6 should be referred for cardiovascular evaluation, perhaps after an echocardiogram is obtained. Other reasons for referral include cardiac symptoms, abnormal splitting of S2, a murmur that increases on standing, a holosystolic murmur, or ejection clicks. Digoxin is not indicated at this point in this asymptomatic patient. |
|
|
For long-term therapy, the most effective control of heart rate in atrial fibrillation, both at rest and with exercise, occurs with which class of drugs?
|
Beta-adrenergic blockers
For long-term therapy, beta-adrenergic antagonist drugs provide the most effective control of heart rate in atrial fibrillation, both at rest and during exercise. Although calcium channel blockers also lower heart rate both at rest and with exercise, they are not as effective as beta-blockers. Digitalis is primarily effective in controlling the heart rate at rest, and often does not adequately control heart rate with exercise. The Class 1 antiarrhythmics are most useful in maintaining sinus rhythm and, in fact, may paradoxically increase heart rate. |
|
|
A 75-year-old white female develops deep-vein thrombosis of the left leg 1 week after hip surgery. The patient is started on low–molecular-weight heparin (Lovenox). Daily monitoring while the patient is on low–molecular-weight heparin should include which lab tests?
|
don't need to monitor lovenox with labs, just warfarin!
Routine coagulation tests such as prothrombin time and partial thromboplastin time are insensitive measurements of Lovenox activity. Anti–factor Xa can be measured in patients with renal failure to monitor anticoagulation effects. |
|
|
Elevated levels of _________ are associated with atherosclerosis?
|
homocysteine
Multiple prospective and case-control studies have shown that a moderately elevated plasma homocysteine concentration is an independent risk factor for atherothrombotic vascular disease. |
|
|
A 60-year-old African-American male was recently diagnosed with an abdominal aortic aneurysm. A lipid profile performed a few months ago revealed an LDL level of 125 mg/dL. You would now advise him that his goal LDL level is:
|
<100 mg/dL
Most physicians realize that the goal LDL level for patients with diabetes mellitus or coronary artery disease is <100 mg/dL. Many may not realize that this goal extends to people with CAD-equivalent diseases, including peripheral artery disease, symptomatic carotid artery disease, and abdominal aortic aneurysm. |
|
|
Which one of the following is a risk factor for perioperative arrhythmias?
A. Supraventricular tachycardia B. Congestive heart failure C. Age >60 D. Premature atrial contractions E. Past history of hyperthyroidism |
Congestive heart failure
Significant predictors of intraoperative and perioperative ventricular arrhythmias include preoperative ventricular (not supraventricular) ectopy, a history of congestive heart failure, and a history of cigarette smoking. Age and a history of hyperthyroidism are not significant predictors of perioperative ventricular arrhythmias. |
|
|
A 35-year-old African-American female has just returned home from a vacation in Hawaii. She presents to your office with a swollen left lower extremity. She has no previous history of similar problems. Homan’s sign is positive, and ultrasonography reveals a noncompressible vein in the left popliteal fossa extending distally. Next step?
|
Enoxaparin (Lovenox) should be administered at a dosage of 1 mg/kg subcutaneously twice a day
The use of low-molecular-weight heparin allows patients with acute deep vein thrombosis (DVT) to be managed as outpatients. The dosage is 1 mg/kg subcutaneously twice daily. Patients chosen for outpatient care should have good cardiopulmonary reserve, normal renal function, and no risk for excessive bleeding. Oral anticoagulation with warfarin can be initiated on the first day of treatment after heparin loading is completed. Monotherapy with warfarin is inappropriate. The incidence of thrombocytopenia with low–molecular-weight heparin is lower than with conventional heparin. The INR should be maintained at 2.0–3.0 in this patient. The 2.5–3.5 range is used for patients with mechanical heart valves. The therapeutic INR should be maintained for 3–6 months in a patient with a first DVT related to travel. |
|
|
What historical features is most suggestive of congestive heart failure in a 6-month-old white male presenting with tachypnea?
|
Diaphoresis with feeding
Symptoms of congestive heart failure in infants are often related to feedings. Only small feedings may be tolerated, and dyspnea may develop with feedings. Profuse perspiration with feedings, is characteristic, and related to adrenergic drive. Older children may have symptoms more similar to adults, but the infant’s greatest exertion is related to feeding. |
|
|
In which clinical situation would it be most appropriate to use a beta-blocker that has intrinsic sympathomimetic activity, such as acebutolol (Sectral) or pindolol (Visken)?
|
In a hypertensive patient with symptomatic bradycardia while taking metoprolol (Lopressor)
Beta-blockers with intrinsic sympathomimetic activity (ISA) are less beneficial in reducing mortality post myocardial infarction, and for this reason are not recommended for ischemic heart disease. They have a potential advantage in only one clinical situation. Since they tend to lower heart rates less, they may be beneficial in patients with symptomatic bradycardia while taking other beta-blockers. All beta-blockers should be used cautiously in patients with diabetes or asthma. Only sotalol, which delays ventricular depolarization, has been shown to be effective for maintenance of sinus rhythm in patients with chronic atrial fibrillation. |
|
|
You are treating a 50-year-old white male for diabetes mellitus and hyperlipidemia. At the time of his initial presentation 1 year ago, his hemoglobin A1c was 8.0% (N 3.8–6.4), LDL 130 mg/dL, HDL 28 mg/dL, and triglycerides 450 mg/dL. After treatment with metformin (Glucophage) and high-dose simvastatin (Zocor), his most recent laboratory evaluation revealed a hemoglobin A1c of 6.2%, LDL 95 mg/dL, HDL 32 mg/dL, and triglycerides 300 mg/dL. The patient has not had any documented coronary or peripheral vascular disease. His family history is positive for a myocardial infarction in his father at age 55. He is a nonsmoker. He has a body mass index (BMI) of 28 and has been unable to lose weight. His blood pressure is well controlled on enalapril (Vasotec). What is the most appropriate management of his elevated triglycerides?
|
Addition of a fibrate such as gemfibrozil (Lopid) or fenofibrate (Tricor)
Although the significance of elevated triglycerides and a low HDL in low-risk patients is somewhat uncertain, in a high-risk patient such as a diabetic, improvement in these results will lower the risk of subsequent cardiac events. In diabetics, metformin and thiazolidinediones (e.g., rosiglitazone) are more likely to improve lipid levels than are sulfonylureas. Nicotinic acid is problematic in diabetics, as it tends to cause deterioration in glucose control. Fibrates are good choices for this patient because they will lower the triglyceride level and raise the HDL level. Exercise and weight loss are likely to be helpful as well. |
|
|
What treatment or intervention has been shown to produce the most benefit for patients with peripheral vascular disease?
|
smoking cessation
Patients with peripheral vascular disease who stop smoking have a twofold increase in their 5-year survival rate. Diet modification and lipid-lowering drugs can slow progression, but not as dramatically. Aspirin and pentoxifylline are minimally effective. |
|
|
A 13-year-old male is found to have hypertrophic cardiomyopathy. His father also had hypertrophic cardiomyopathy, and died suddenly at age 38 following a game of tennis. The boy’s mother asks you for advice regarding his condition. What advice should you give her?
|
His siblings should undergo echocardiography
Hypertrophic cardiomyopathy is an autosomal dominant condition and close relatives of affected individuals should be screened. The hypertrophy usually stays the same or worsens with age. This patient should not participate in strenuous sports, even those considered noncontact. Beta-blockers have not been shown to alter the progress of the disease. The mortality rate is believed to be about 1%, with some series estimating 5%. Thus, in most cases lifespan is normal. |
|
|
A 70-year-old white male has a slowly enlarging, asymptomatic abdominal aortic aneurysm. You should usually recommend surgical intervention when the diameter of the aneurysm approaches:
|
5.5 cm
Based on recent clinical trials, the most common recommendation for surgical repair is when the aneurysm approaches 5.5 cm in diameter. Two large studies, the Aneurysm Detection and Management (ADAM) Veteran Affairs Cooperative Study, and the United Kingdom Small Aneurysm Trial, failed to show any benefit from early surgery for men with aneurysms less than 5.5 cm in diameter. The risks of aneurysm rupture were 1% or less in both studies, with 6-year cumulative survivals of 74% and 64%, respectively. Interestingly, the risk for aneurysm rupture was four times greater in women, indicating that 5.5 cm may be too high, but a new evidence-based threshold has not yet been defined. |
|
|
A 75-year-old otherwise healthy white female states that she has passed out three times in the last month while walking briskly during her daily walk with the local senior citizens mall walkers’ club. This history would suggest what etiology of her syncope?
|
aortic stenosis
Syncope with exercise is a manifestation of organic heart disease in which cardiac output is fixed and does not rise (or even fall) with exertion. Syncope, commonly on exertion, is reported in up to 42% of patients with severe aortic stenosis. |
|
|
Which drug class is preferred for treating hypertension in patients who also have diabetes mellitus?
|
ACE-I
ACE inhibitors have proven beneficial in patients who have either early or established diabetic renal disease. They are the preferred therapy in patients with diabetes and hypertension, according to guidelines from the American Diabetes Association, the National Kidney Foundation, the World Health Organization, and the JNC VII report. |
|
|
A 75-year-old Hispanic male presents with dyspnea on exertion which has worsened over the last several months. He denies chest pain and syncope, and was fairly active until the shortness of breath slowed him down recently. You hear a grade 3/6 systolic ejection murmur at the right upper sternal border which radiates into the neck. Echocardiography reveals aortic stenosis, with a mean transvalvular gradient of 55 mm Hg and a calculated valve area of 0.6 cm2. Left ventricular function is normal. Which one of the following is appropriate management for this patient?
|
Aortic valve replacement
Since this patient’s mean aortic-valve gradient exceeds 50 mm Hg and the aortic-valve area is not larger than 1 cm2, it is likely that his symptoms are due to aortic stenosis. As patients with symptomatic aortic stenosis have a dismal prognosis without treatment, prompt correction of his mechanical obstruction with aortic valve replacement is indicated. Medical management is not effective, and balloon valvotomy only temporarily relieves the symptoms and does not prolong survival. Patients who present with dyspnea have only a 50% chance of being alive in 2 years unless the valve is promptly replaced. Exercise testing is unwarranted and dangerous in patients with symptomatic aortic stenosis. |
|
|
A 73-year-old white male nursing-home resident has Alzheimer’s dementia and hypertension. He has been weaker and less responsive over the last week and has gained 8 lb. On physical examination he has normal vital signs with a heart rate of 110 beats/min, but is noted to have marked lower extremity edema and presacral edema. Laboratory evaluation shows a serum sodium level of 122 mmol/L (N 135–145). What is the most likely cause of his hyponatremia?
|
Congestive Heart Failure
Most decision trees for the evaluation of hyponatremia begin with an assessment of volume status; edema reflects volume overload and increased total body sodium caused by congestive heart failure, cirrhosis, or renal failure. If edema is absent, plasma osmolality should be determined. SIADH, Addison’s disease (hypoadrenalism), diuretic use, and renal artery stenosis all lower serum osmolality. Urine electrolytes help distinguish the other conditions: psychogenic polydipsia causes low urine sodium, while SIADH and hypoadrenalism cause inappropriately elevated urine sodium. Diuretic use, a very common cause of hyponatremia in the geriatric population, causes hypovolemic hyponatremia and can be associated with either high or low urine sodium, but there is often concomitant hypokalemia. |
|
|
A 28-year-old gravida 2 para 1 presents to the emergency department at 16 weeks' gestation. She has noted the sudden onset of dyspnea, pleuritic chest pain, and mild hemoptysis. Both calves are mildly edematous and somewhat tender. A lung scan shows a high probability of pulmonary emboli. Which one of the following would be appropriate management at this time?
|
Intravenous heparin for 5–10 days followed by subcutaneous heparin for the duration of the pregnancy
The risk of pulmonary embolism is five times higher in pregnant women than in nonpregnant women of similar age, and venous thromboembolism is a leading cause of illness and death during pregnancy. Warfarin, which readily crosses the placenta, should be avoided throughout pregnancy. It is definitely teratogenic during the first trimester, and extensive fetal abnormalities have been associated with exposure to warfarin in any trimester. Because heparin does not cross the placenta, it is considered the safest anticoagulant to use during pregnancy. Initially, patients with venous thromboembolism during pregnancy should be managed with heparin given according to the recommendations for nonpregnant patients. These women should receive intravenous heparin for 5–10 days followed by subcutaneous heparin for the duration of the pregnancy. Warfarin can be given after delivery, since it is not present in breast milk. The indications for placement of an inferior vena cava filter are not changed by pregnancy, and include any contraindication to anticoagulant therapy, the occurrence of heparin-induced thrombocytopenia, and recurrence of pulmonary embolism in a patient receiving adequate anticoagulant therapy. There are no data to support the use of aspirin for treatment or prophylaxis of pulmonary embolism either during or after pregnancy. |
|
|
Which one of the following is considered a contraindication to the use of beta-blockers for congestive heart failure?
A. Mild asthma B. Symptomatic heart block C. New York Heart Association (NYHA) Class III heart failure D. NYHA Class I heart failure in a patient with a history of a previous myocardial infarction E. An ejection fraction <30% |
symptomatic heart block
According to several randomized, controlled trials, mortality rates are improved in patients with heart failure who receive beta-blockers in addition to diuretics, ACE inhibitors, and occasionally, digoxin. Contraindications to beta-blocker use include hemodynamic instability, heart block, bradycardia, and severe asthma. Beta-blockers may be tried in patients with mild asthma or COPD as long as they are monitored for potential exacerbations. Beta-blocker use has been shown to be effective in patients with NYHA Class II or III heart failure. There is no absolute threshold ejection fraction. Beta-blockers have also been shown to decrease mortality in patients with a previous history of myocardial infarction, regardless of their NYHA classification. |
|
|
What is the leading cause of death in women?
|
Cardiovascular disease is the leading cause of death among women. According to the CDC, 29.3% of deaths in females in the U.S. in 2001 were due to cardiovascular disease and 21.6% were due to cancer, with most resulting from lung cancer. Breast cancer is the third most common cause of cancer death in women, and ovarian cancer is the fifth most common.
|
|
|
A 72-year-old African-American male comes to your office for surgical clearance to undergo elective hemicolectomy for recurrent diverticulitis. The patient suffered an uncomplicated acute anterior-wall myocardial infarction approximately 18 months ago. A stress test was normal 2 months after he was discharged from the hospital. Currently, the patient feels well, walks while playing nine holes of golf three times per week, and is able to walk up a flight of stairs without chest pain or significant dyspnea. Findings are normal on a physical examination. Which one of the following would be most appropriate for this patient prior to surgery?
|
12-lead resting EKG
The current recommendations from the American College of Cardiology and the American Heart Association on preoperative clearance for noncardiac surgery state that preoperative intervention is rarely needed to lower surgical risk. Patients who are not currently experiencing unstable coronary syndrome, severe valvular disease, uncompensated congestive heart failure, or a significant arrhythmia are not considered at high risk, and should be evaluated for most surgery primarily on the basis of their functional status. If these patients are capable of moderate activity (greater than 4 METs) without cardiac symptoms, they can be cleared with no stress testing or coronary angiography for an elective minor or intermediate-risk operation such as the one this patient is to undergo. A resting 12-lead EKG is recommended for males over 45, females over 55, and patients with diabetes, symptoms of chest pain, or a previous history of cardiac disease. |
|
|
Patients with Wolff-Parkinson-White syndrome who have episodic symptomatic supraventricular tachycardia or atrial fibrillation benefit most from:
|
Radiofrequency catheter ablation of bypass tracts
Radiofrequency catheter ablation of bypass tracts is possible in over 90% of patients and is safer and more cost effective than surgery, with a similar success rate. Intravenous and oral digoxin can shorten the refractory period of the accessory pathway, and increase the ventricular rate, causing ventricular fibrillation. Beta-blockers will not control the ventricular response during atrial fibrillation when conduction proceeds over the bypass tract. |
|
|
A 67-year-old white male sees you for a new patient visit. He is asymptomatic and has not seen a doctor in 10 years. He does not smoke or drink and takes no medication. He says he has a history of “mild high blood pressure” but has never been treated for this. His blood pressure today is 180/90 mm Hg. He has a decreased arteriovenous ratio on funduscopic examination, his point of maximal intensity is displaced laterally, and he has decreased pedal pulses. The most appropriate management at this point would be to:
|
Prescribe a diuretic
Elevated blood pressure along with physical findings of cardiovascular disease establishes the diagnosis of hypertension in this patient, so it is not necessary to take follow-up blood pressure readings prior to starting treatment. Since he has no symptoms or physical findings suggestive of secondary hypertension it is also not necessary to perform a laboratory workup prior to treatment. Because he has Stage 3 hypertension with evidence of end-organ disease, treatment with antihypertensives is indicated at this point. At least three large clinical trials, including the European Working Party on High Blood Pressure in the Elderly (EWPHE) trial, have shown that diuretics are the most effective single agents for hypertension in the elderly. A low-sodium diet can be added, as can a beta-blocker if the hypertension fails to respond to diuretics alone. |
|
|
A male infant weighing 3000 g (6 lb 10 oz) is born at 36 weeks' gestation, with normal Apgar scores and an unremarkable initial examination. At 48 hours of age he is noted to have dusky episodes while feeding, and does not feed well. On repeat examination the child is tachypneic, with subcostal retractions. Lung sounds are clear and there is no heart murmur. Pulse oximetry on room air is 82%. Arterial blood gases on 100% oxygen show a pCO2 of 26 mm Hg (N 27–40), a pO2 of 66 mm Hg (N 83–108), a blood pH of 7.50 mg/dL (N 7.35–7.45), and a base excess of –2 mmol/L (N –10 to –2). Laboratory Findings: Hemoglobin - 22.0 g/dL (N 13.0–20.0) Hematocrit - 66% (N 42–66) WBCs - 19,000/mm3 (N 9000–30,000) Chest radiograph - increased vascular markings; large thymus Blood culture results are pending. Which one of the following is the most likely diagnosis?
|
Congenital Heart Disease
Cyanotic congenital heart disease can appear at the time of ductus closure. A heart murmur is not usually audible, and murmurs heard this early are usually not due to heart disease. The failure to correct hypoxemia with 100% oxygen is diagnostic for abnormal mixing of blood from the right and left circulations. Transient tachypnea presents earlier, and the hypoxia corrects with supplemental oxygen. Hyaline membrane disease can occur at 36 weeks, but would cause problems in the first hours of life. It can make oxygenation difficult, but would cause extreme distress with CO2 retention in such cases. This patient has the energy to hyperventilate and has slight respiratory alkalosis as a result. Neonatal sepsis can cause V/Q mismatching and hypoxia, and can have a delayed presentation. Concern would be high enough in this case that the patient would probably receive broad-spectrum antibiotics while awaiting culture results. On the other hand, the clinician would not want to be distracted from the evidence for congenital heart disease. The baby is polycythemic from poor intake in the first 2 days of life. The hyperviscosity syndrome can occur when the hematocrit is over 65%. It can cause poor feeding, tachypnea, and sluggishness, but does not cause hypoxia. |
|
|
A 73-year-old male with COPD presents to the emergency department with increasing dyspnea. Examination reveals no sign of jugular venous distention. A chest examination reveals decreased breath sounds and scattered rhonchi, and the heart sounds are very distant but no gallop or murmur is noted. There is +1 edema of the lower extremities. Chest radiographs reveal cardiomegaly but no pleural effusion. The patient’s B-type natriuretic peptide level is 850 pg/mL (N <100) and his serum creatinine level is 0.8 mg/dL (N 0.6–1.5). Which one of the following would be the most appropriate initial management?
|
Furosemide (Lasix), 40 mg intravenously
B-type natriuretic peptide (BNP) is secreted in the ventricles and is sensitive to changes in left ventricular function. Concentrations correlate with end-diastolic pressure, which in turn correlates with dyspnea and congestive heart failure. BNP levels can be useful when trying to determine whether dyspnea is due to cardiac, pulmonary, or deconditioning etiologies. A value of less than 100 pg/mL excludes congestive heart failure as the cause for dyspnea. If it is greater than 400 pg/mL, the likelihood of congestive heart failure is 95%. Patients with values of 100–400 pg/mL need further investigation. There are some pulmonary problems that may elevate BNP, such as lung cancer, cor pulmonale, and pulmonary embolus. However, these patients do not have the same extent of elevation that those with acute left ventricular dysfunction will have. If these problems can be ruled out, then individuals with levels between 100–400 pg/mL most likely have congestive heart failure. Initial therapy should be a loop diuretic. It should be noted that BNP is partially excreted by the kidneys, so levels are inversely proportional to creatinine clearance. |
|
|
A 25-year-old female at 36 weeks gestation presents for a routine prenatal visit. Her blood pressure is 118/78 mm Hg and her urine has no signs of protein or glucose. Her fundal height shows appropriate fetal size and she says that she feels well. On palpation of her legs, you note 2+ pitting edema bilaterally. Which one of the following is true regarding this patient’s condition?
|
Her leg swelling requires no further evaluation
Lower-extremity edema is common in the last trimester of normal pregnancies and can be treated symptomatically with compression stockings. Edema has been associated with preeclampsia, but the majority of women who have lower-extremity edema with no signs of elevated blood pressure will not develop preeclampsia or eclampsia. For this reason, edema has recently been removed from the diagnostic criteria for preeclampsia. Disproportionate swelling in one leg versus another, especially associated with leg pain, should prompt a workup for deep venous thrombosis but is unlikely given this patient’s presentation, as are cardiac or renal conditions. |
|
|
What is the medical treatment of choice for acute delirium in the intensive care unit?
|
Intravenous haloperidol (Haldol) in increasing doses every 30 minutes as needed
Intravenous haloperidol has been found to be more effective than lorazepam and has minimal physiologic side effects. |
|
|
A 72-year-old male with a history of previous inferior myocardial infarction sees you prior to surgery for symptomatic gallstones. He denies chest pain or dyspnea. His current medications include aspirin, 81 mg daily; ramipril (Altace), 10 mg daily; and pravastatin (Pravachol), 40 mg daily. He is in good health otherwise and has no other health complaints. He has been cleared for surgery by his cardiologist.What medication should be considered before and after surgery, assuming no contraindications?
|
Atenolol (Tenormin)
A recent development in the prophylaxis of surgery-related cardiac complications is the use of beta-blockers perioperatively for patients with cardiac risk factors. In a randomized, double-blind, placebo-controlled trial involving 200 patients who were undergoing elective noncardiac surgery that required general anesthesia, the effect of atenolol on perioperative cardiac complications was evaluated. Patients were eligible for beta-blocker therapy if they had known coronary artery disease or two or more risk factors. Atenolol was not used if the resting heart rate was <55 beats/min, systolic blood pressure was <100 mm Hg, or there was evidence of congestive heart failure, third degree heart block, or bronchospasm. A 5-mg dose of intravenous atenolol was given 30 minutes before surgery and then again immediately after surgery. Oral atenolol, 50–100 mg, was then given until hospital discharge or 7 days postoperatively. The results of the study showed that mortality from cardiac causes was 65% lower in the patients receiving atenolol. Another study showed similar perioperative benefit using the beta-blocker bisoprolol. |
|
|
A 34-year-old white female at 32 weeks' gestation develops a venous thromboembolism. Following 5 days of IV heparin in the hospital, what regimen would be most appropriate as an outpatient?
|
Subcutaneous heparin every 12 hours until delivery
Heparin does not cross the placenta and is safe for the fetus, whereas coumarin derivatives can cause fetal bleeding and are teratogenic during weeks 6–12. Therefore, pregnant women with venous thromboembolism should receive intravenous heparin for 5 days, followed by adjusted-dose subcutaneous heparin every 12 hours until delivery. Increasingly, low–molecular-weight heparins are being used instead of unfractionated heparin because of ease of administration and the reduced need for coagulation monitoring. Intravenous heparin is not necessary after the patient leaves the hospital, and aspirin has not been shown to be beneficial. |
|
|
A 52-year-old white male is being considered for pharmacologic treatment of hyperlipidemia because of an LDL cholesterol level of 180 mg/dL. Before beginning medication for his hyperlipidemia, he should be screened for:
|
Hypothyroidism
According to the Summary of the National Cholesterol Education Program (NCEP) Adult Treatment Panel III Report of 2001, any person with elevated LDL cholesterol or any other form of hyperlipidemia should undergo clinical or laboratory assessment to rule out secondary dyslipidemia before initiation of lipid-lowering therapy. Causes of secondary dyslipidemia include diabetes mellitus, hypothyroidism, obstructive liver disease, chronic renal failure, and some medications. |
|
|
A 56-year-old African-American male with longstanding hypertension and a 30-pack-year smoking history has a 2-day history of dyspnea on exertion. Physical examination is unremarkable except for rare crackles at the bases. Which serologic test would be most helpful for detecting left ventricular dysfunction?
|
Beta-natriuretic peptide (BNP)
Beta-natriuretic peptide (BNP) is a 32-amino acid polypeptide secreted from the cardiac ventricles in response to ventricular volume expansion and pressure overload. The major source of BNP is the cardiac ventricles, and because of its minimal presence in storage granules, its release is directly proportional to ventricular dysfunction. It is a simple and rapid test that reliably predicts the presence or absence of left ventricular dysfunction on an echocardiogram. |
|
|
A 35-year-old white male with known long QT syndrome has a brief episode of syncope requiring cardiopulmonary resuscitation. Which one of the following is most likely responsible for this episode?
|
Torsades de pointes
Patients with long QT syndrome that have sudden arrhythmia death syndrome usually have either torsades de pointes or ventricular fibrillation. |
|
|
An 83-year-old female presents to your office as a new patient. She recently moved to the area to be closer to her family. A history reveals that she has been in excellent health, has no complaints, and is on no medications except occasional acetaminophen for knee pain. She has never been in the hospital and has not had any operations. She says that she feels well. The examination is normal, with expected age-related changes, except that her blood pressure on three different readings averages 175/70 mm Hg. These readings are confirmed on a subsequent follow-up visit. In addition to lifestyle changes, which one of the following would be most appropriate for the initial management of this patient’s hypertension?
|
A thiazide diuretic
Clinical trials support the treatment of systolic hypertension in the older person with a systolic blood pressure of at least 160 mm Hg. (Systolic hypertension is defined as systolic blood pressure of at least 140 mm Hg and a diastolic blood pressure of less than 90 mm Hg.) The studies most strongly support the use of thiazide diuretics and long-acting calcium channel blockers as first-line therapy. Alpha-blockers are not recommended. ACE inhibitors, beta-blockers, and angiotensin receptor blockers are used when certain compelling indications are present, e.g., in a patient with diabetes or who has had a myocardial infarction. |
|
|
What is the INITIAL treatment of choice in the management of severe hypertension during pregnancy?
|
Labetalol (Trandate, Normodyne) intravenously
In pregnant women with severe hypertension, the primary objective of treatment is to prevent cerebral complications such as encephalopathy and hemorrhage. Intravenous hydralazine, intravenous labetalol, or oral nifedipine may be used. Sublingual nifedipine can cause severe hypotension, and reserpine is not indicated. Nitroprusside can be used for short intervals in patients with hypertensive encephalopathy, but fetal cyanide toxicity is a risk with infusions lasting more than 4 hours. ACE inhibitors are never indicated for hypertensive therapy during pregnancy. |
|
|
What would be a contraindication to initiating beta-blocker therapy in a patient with congestive heart failure?
|
Recent hospital admission for decompensated heart failure
In general, it is advisable to avoid initiating beta-blocker therapy during or immediately after admission for decompensated heart failure. |
|
|
What medication is preferred for chronic treatment of congestive heart failure due to left ventricular systolic dysfunction?
|
ACE inhibitors
ACE inhibitors are the preferred drugs for congestive heart failure due to left ventricular systolic dysfunction, because they are associated with the lowest mortality. The combination of hydralazine/isosorbide dinitrate is a reasonable alternative, and diuretics should be used cautiously. It is not known whether digoxin affects mortality, although it can help with symptoms. |
|
|
Which one of the following is most predictive of increased perioperative cardiovascular events associated with noncardiac surgery in the elderly?
A. An age of 80 years B. Left bundle-branch block C. Atrial fibrillation with a rate of 80 beats/min D. A history of previous stroke E. Renal insufficiency (creatinine 2.0 mg/dL) |
Renal insufficiency (creatinine 2.0 mg/dL)
Clinical predictors of increased perioperative cardiovascular risk for elderly patients include major risk factors such as ● unstable coronary syndrome (acute or recent myocardial infarction, unstable angina) ● decompensated congestive heart failure ● significant arrhythmia (high-grade AV block, symptomatic ventricular arrhythmia ● supraventricular arrhythmias with uncontrolled ventricular rate) ● severe valvular disease Intermediate predictors are: ● mild angina ● previous myocardial infarction ● compensated congestive heart failure ● diabetes mellitus ● renal insufficiency Minor predictors are: ● advanced age ● an abnormal EKG - left ventricular hypertrophy, left bundle-branch block, ST and T-wave abnormalities, rhythm other than sinus, ● low functional capacity ● history of stroke ● uncontrolled hypertension. |
|
|
The use of automated external defibrillators by lay persons in out-of-hospital settings:
|
Has been shown to contribute to significant gains in full neurologic and functional recovery
The use of automated external defibrillators (AEDs) by lay persons, trained and otherwise, has been quite successful, with up to 40% of those treated recovering full neurologic and functional capacity. At present, 45 states have passed Good Samaritan laws covering the use of AEDs by well-intentioned lay persons. There are initiatives for widespread placement of AEDs, to include commercial airlines and other public facilities |
|
|
A 74-year-old white male complains of pain in the right calf that recurs on a regular basis. He smokes 1 pack of cigarettes per day and is hypertensive. He has a history of a previous heart attack but is otherwise in fair health. Which one of the following findings would support a diagnostic impression of peripheral vascular disease?
|
Treadmill arterial flow studies showing a 20-mm Hg decrease in ankle systolic blood pressure immediately following exercise
Peripheral vascular disease (PVD) is a clinical manifestation of atherosclerotic disease and is caused by occlusion of the arteries to the legs. Patients with significant arterial occlusive disease will have a prominent decrease in the ankle-brachial index from baseline following exercise, and usually a 20-mm Hg or greater decrease in systolic blood pressure. Pain during rest and exercise and the presence of swelling and soreness behind the knee and in the calf is found in those with Baker’s cysts. Peripheral nerve pain commonly begins immediately upon walking and is unrelieved by rest. Doppler waveform analysis is useful in the diagnosis of PVD and will reveal attenuated waveforms at a point of decreased blood flow. Employment of the ankle-brachial index is encouraged in daily practice as a simple means to diagnose the presence of PVD. Generally, ankle-brachial indices in the range of 0.91–1.30 are thought to be normal. |
|
|
In a 34-year-old primigravida at 35 weeks' gestation, which one of the following supports a diagnosis of MILD preeclampsia rather than severe preeclampsia?
A. A blood pressure of 150/100 mm Hg B. A 24-hr protein level of 6 g C. A platelet count <100,000/mm3 D. Liver enzyme elevation with epigastric tenderness E. Altered mental status |
A blood pressure of 150/100 mm Hg
The criteria for severe preeclampsia is: ● blood pressure of 160/110 mm Hg or above on two occasions, 6 hours apart. Other criteria include ● proteinuria above 5 g/24 hr ● thrombocytopenia with a platelet count <100,000/mm3 ● liver enzyme abnormalities ● epigastric or right upper quadrant pain ● alteration of mental status. |
|
|
A 72-year-old white female is scheduled to undergo a total knee replacement for symptomatic osteoarthritis. She is otherwise healthy, with no history of vascular disease or deep vein thrombosis. She takes no routine medications. What medication is most appropriate for prophylaxis against deep vein thrombosis?
|
Enoxaparin (Lovenox), 30 mg subcutaneously every 12 hours
Prophylaxis is indicated with total knee or hip replacements. The two regimens recommended are low–molecular-weight heparin and adjusted-dose warfarin. These may be augmented by intermittent pneumatic compression. |
|
|
What medication is contraindicated in the treatment of patients with cocaine-induced arrhythmias?
|
Metoprolol (Lopressor)
When treating arrhythmias related to cocaine toxicity, hypertonic sodium bicarbonate and benzodiazepines may be given when the distinction between sodium channel blockade–induced QRS-complex widening and ischemia-induced ventricular tachycardia is unclear. Lidocaine may subsequently be utilized if necessary. Verapamil has been shown to reverse cocaine-induced coronary vasospasm. Beta-adrenergic blocking drugs have been shown to exacerbate coronary vasospasm by resulting in unopposed alpha-adrenergic activity. Beta-blockers are therefore contraindicated in the treatment of cocaine-induced cardiac problems. |
|
|
A 34-year-old white primigravida in her first trimester had established moderate hypertension before becoming pregnant. She currently has a blood pressure of 168/108 mm Hg. You are considering how to best manage her hypertension during the pregnancy. What medication is associated with the greatest risk of fetal growth retardation if used for hypertension throughout pregnancy?
|
Atenolol (Tenormin)
Atenolol and propranolol are associated with intrauterine growth retardation when used for prolonged periods during pregnancy. They are class D agents during pregnancy. Other beta-blockers may not share this risk. Methyldopa, hydralazine, and calcium channel blockers have not been associated with intrauterine growth retardation. They are generally acceptable agents to use for established, significant hypertension during pregnancy |
|
|
A 72-year-old male with class III congestive heart failure (CHF) due to systolic dysfunction asks if he can take ibuprofen for his “aches and pains.” Appropriate counseling regarding NSAID use and heart failure should include:
|
NSAIDs, including high-dose aspirin, should be avoided in CHF patients because they can cause fluid retention
|
|
|
A 72-year-old male presents to your clinic in atrial fibrillation with a rate of 132 beats/min. He has hypertension, but no history of congestive heart failure or structural heart disease. He is otherwise healthy and active. The best INITIAL approach to his atrial fibrillation would be:
|
NSAIDs, including high-dose aspirin, should be avoided in CHF patients because they can cause fluid retention
If possible, NSAIDs should be avoided in patients with heart failure. They cause sodium and water retention, as well as an increase in systemic vascular resistance which may lead to cardiac decompensation. Patients with heart failure who take NSAIDs have a tenfold increased risk of hospitalization for exacerbation of their CHF. NSAIDs alone in patients with normal ventricular function have not been associated with initial episodes of heart failure. NSAIDs, including high-dose aspirin (325 mg/day), may decrease or negate entirely the beneficial unloading effects of ACE inhibition. They have been shown to have a negative impact on the long-term morbidity and mortality benefits that ACE inhibitors provide. Sulindac and low-dose aspirin (81 mg/day) are less likely to cause these negative effects. |
|
|
Cilostazol (Pletal) has been found to be a useful drug for the treatment of intermittent claudication. This drug is contraindicated in patients with:
|
Ventricular rate control with a calcium channel blocker or beta-blocker, and warfarin for anticoagulation
Five recent randomized, controlled trials have indicated that in most patients with atrial fibrillation, an initial approach of rate control is best. Patients who were stratified to the rhythm control arm of the trials did NOT have a morbidity or mortality benefit and were more likely to suffer from adverse drug effects and increased hospitalizations. The most efficacious drugs for rate control are calcium channel blockers and beta-blockers. Digoxin is less effective for rate control and should be reserved as an add-on option for those not controlled with a beta-blocker or calcium channel blocker, or for patients with significant left ventricular systolic dysfunction. In patients 65 years of age or older or with one or more risk factors for stroke, the best choice for anticoagulation to prevent thromboembolic disease is warfarin. Of note, in patients who are successfully rhythm controlled and maintained in sinus rhythm, the thromboembolic rate is equivalent to those managed with a rate control strategy. Thus, the data suggest that patients who choose a rhythm control strategy should be maintained on anticoagulation regardless of whether they are consistently in sinus rhythm. Ref: Snow V, Weiss K, LeFevre M, et al: Management of newly detected atrial fibrillation: A clinical practice guideline from the AAFP and the ACP. |
|
|
What medication has been shown to decrease mortality late after a myocardial infarction?
|
Congestive heart failure
Cilostazol is a drug with phosphodiesterase inhibitor activity introduced for the symptomatic treatment of arterial occlusive disease and intermittent claudication. Cilostazol should be avoided in patients with congestive heart failure. There are no limitations on its use in patients with previous stroke or a history of diabetes. It has been found to have beneficial effects on HDL cholesterol levels and in the treatment of third degree heart block. |
|
|
A 72-year-old white male has new-onset hypertension with a current blood pressure of 190/110 mm Hg. What medication can be used as part of a test for diagnosing renovascular hypertension, but would also increase the risk for azotemia if used for treatment?
|
Beta-blockers and ACE inhibitors have been found to decrease mortality late after myocardial infarction.
Aspirin has been shown to decrease nonfatal myocardial infarction, nonfatal stroke, and vascular events. Nitrates, digoxin, thiazide diuretics, and calcium channel antagonists have not been found to reduce mortality after myocardial infarction. |
|
|
Patients with symptomatic congestive heart failure associated with a reduced systolic ejection fraction or left ventricular remodeling should be initially treated with?
|
Captopril (Capoten)
ACE inhibitors can significantly worsen renal failure in patients with hypertension caused by renovascular disease. Hyperkalemia is an associated problem. Captopril renography is a useful diagnostic screening test. The other agents are useful for lowering blood pressure but may cause mild creatinine elevations. They do not, however, cause the significant elevations of creatinine seen with ACE inhibitors in cases of significant renovascular disease. |
|
|
A 62-year-old male presents for surgical clearance prior to transurethral resection of the prostate. His past history is significant for a pulmonary embolus after a cholecystectomy 15 years ago. His examination is unremarkable except that he is 23 kg (50 lb) overweight. The most appropriate recommendation to the urologist would be to:
|
An ACE inhibitor
It has been shown that congestive heart failure (CHF) patients treated with ACE inhibitors survive longer, and all such patients should take these agents if tolerated. Warfarin and/or antiarrhythmic drugs should be given only to selected CHF patients. Verapamil may adversely affect cardiac function and should be avoided in patients with CHF. Hydralazine can be used, but because of its side effect profile would be a second-line agent. |
|
|
A 62-year-old male presents for surgical clearance prior to transurethral resection of the prostate. His past history is significant for a pulmonary embolus after a cholecystectomy 15 years ago. His examination is unremarkable except that he is 23 kg (50 lb) overweight. The most appropriate recommendation to the urologist would be to:
|
Start the patient on subcutaneous enoxaparin (Lovenox), 40 mg 1–2 hr prior to surgery and once a day after surgery
A patient with a past history of postoperative venous thromboembolism is at risk for similar events with subsequent major operations. The most appropriate treatment of the choices listed would be subcutaneous enoxaparin. Aspirin is ineffective for prophylaxis of venous thromboembolism. Warfarin is effective at an INR of 2.0–3.0. Full anticoagulation with heparin is unnecessary for prophylaxis and can result in a higher rate of postoperative hemorrhage. |
|
|
A 34-year-old African-American female presents to you for preconception counseling regarding the management of her chronic hypertension. Her blood pressure has been well controlled on benazepril (Lotensin), 20 mg/day, without any side effects. The patient’s blood pressure was 145/95 mm Hg prior to beginning benazepril. She has been pregnant once before, and her physician switched her to methyldopa (Aldomet) during that pregnancy, but she suffered from drowsiness and a dry mouth during much of that time. The pregnancy and delivery were otherwise uncomplicated. She has no history of diabetes mellitus, renal insufficiency, or asthma. She is a nonsmoker. Which one of the following would you do when she becomes pregnant?
|
Discontinue the benazepril and monitor closely throughout the pregnancy for signs of preeclampsia or fetal growth restriction
Most women with mild, uncomplicated essential hypertension are at minimal risk for cardiac complications within the short time frame of pregnancy. There is no evidence available that treatment of mild essential hypertension during pregnancy provides any benefit to the mother. Given the potential for short- and long-term risk to the fetus from antihypertensive treatment, it is advisable to discontinue antihypertensive treatment, monitor the mother for signs of preeclampsia, and monitor fetal growth and development. Medication is not necessary as long as the systolic blood pressure remains below 160 mm Hg, the diastolic blood pressure remains below 105–110 mm Hg, and there are no signs of preeclampsia or fetal growth restriction. Should the mother develop severe hypertension, treatment can be initiated with long-acting nifedipine, labetalol, a thiazide diuretic, or methyldopa. Atenolol has been associated with reduced fetal growth, and ACE inhibitors are contraindicated in the second and third trimesters. |
|
|
An asymptomatic 55-year-old male visits a health fair, where he has a panel of blood tests done. He brings the results to you because he is concerned about the TSH level of 12.0 µU/mL (N 0.45-4.5). His free T4 level is normal. Which one of the following is most likely to be associated with this finding?
|
elevated LDL level
With subclinical thyroid dysfunction, TSH is either below or above the normal range, free T3 or T4 levels are normal, and the patient has no symptoms of thyroid disease. Subclinical hypothyroidism (TSH >10 µU/mL) is likely to progress to overt hypothyroidism, and is associated with increased LDL cholesterol. Subclinical hyperthyroidism (TSH <0.1 µU/mL) is associated with the development of atrial fibrillation, decreased bone density, and cardiac dysfunction. Neither type of subclinical thyroid dysfunction is associated with diabetes mellitus. There is insufficient evidence of benefit to warrant early treatment of either condition |
|
|
A 67-year-old female presents with progressive weakness, dry skin, lethargy, slow speech, and eyelid edema. What medication currently taken by this patient, could be causing her symptoms?
|
Lithium
This patient has classic signs of hypothyroidism. Of the drugs listed, only lithium is associated with the development of hypothyroidism. In patients taking lithium, it is recommended that in addition to regular serum lithium levels, thyroid function tests including total free T4, and TSH be obtained yearly. |
|
|
A 49-year-old female who takes multiple medications has a chemistry profile as part of her routine monitoring. She is found to have an elevated calcium level. All other values on the profile are normal, and the patient is not currently symptomatic. Follow-up testing reveals a serum calcium level of 11.2 mg/dL (N 8.4-10.2) and an intact parathyroid hormone level of 80 pg/mL (N 10-65). Which medication should be discontinued for 3 months before repeat laboratory evaluation and treatment?
|
Lithium
Lithium therapy can elevate calcium levels by elevating parathyroid hormone secretion from the parathyroid gland. This duplicates the laboratory findings seen with mild primary hyperparathyroidism. If possible, lithium should be discontinued for 3 months before reevaluation (SOR C). This is most important for avoiding unnecessary parathyroid surgery. Other choices for this questions were: VitD/Calcium supplementation, Lasix, Raloxifene Vitamin D and calcium supplementation could contribute to hypercalcemia in rare instances, but they would not cause elevation of parathyroid hormone. Raloxifene has actually been shown to mildly reduce elevated calcium levels, and furosemide is used with saline infusions to lower significantly elevated calcium levels ["Loops Lose Ca++"] |
|
|
What medication should be discontinued in a patient with diabetic gastroparesis?
|
Exenatide (Byetta)
Delayed gastric emptying may be caused or exacerbated by medications for diabetes, including amylin analogues (e.g., pramlintide) and glucagon-like peptide 1 (e.g., exenatide). Delayed gastric emptying has a direct effect on glucose metabolism, in addition to being a means of reducing the severity of postprandial hyperglycemia. In a clinical trial of exenatide, nausea occurred in 57% of patients and vomiting occurred in 19%, which led to the cessation of treatment in about one-third of patients. |
|
|
A frail 83-year-old male with a 10-year history of diabetes mellitus is admitted to a nursing home. His blood glucose level, which he rarely checks, is typically over 200 mg/dL. His serum creatinine level is 1.9 mg/dL. He also has had several episodes of heart failure. His current medications include glipizide (Glucotrol), lisinopril (Prinivil, Zestril), and furosemide (Lasix). Which one of the following would be most appropriate to add to this patients regimen to treat his diabetes mellitus?
|
Insulin glargine (Lantus)
NOT metformin!! For geriatric patients in long-term care facilities, the predictable glucose control of glargine is the best approach to consider initially. The American Diabetes Association does not recommend a strict diet for frail diabetic patients in nursing homes. Exenatide is not recommended for the frail elderly because of concerns about weight loss and nausea. Heart failure precludes the use of pioglitazone, and renal failure precludes the use of metformin. |
|
|
A 54-year-old female takes levothyroxine (Synthroid), 0.125 mg/day, for central hypothyroidism secondary to a pituitary adenoma. The nurse practitioner in your office orders a TSH level, which is found to be 0.1 mIU/mL (N 0.5-5.0). What would you recommend?
|
Order a free T4 level before adjusting the dose of Levothyroxine
Although uncommon, pituitary disease can cause secondary hypothyroidism. The characteristic laboratory findings are a low serum free T4 and a low TSH. A free T4 level is needed to evaluate the proper dosage of replacement therapy in secondary hypothyroidism. The TSH level is not useful for determining the adequacy of thyroid replacement in secondary hypothyroidism since the pituitary is malfunctioning. In the initial evaluation of secondary hypothyroidism, a TRH stimulation test would be useful if TSH failed to rise in response to stimulation. It is not necessary in this case, since the diagnosis has already been made. |
|
|
A 55-year-old white male sees you for a routine annual visit. His fasting blood glucose level is 187 mg/dL. Repeat testing 1 week later reveals a fasting glucose level of 155 mg/dL and an HbA1c of 9.4%. His BMI is 30 kg/m2. He does not seem to have any symptoms of diabetes mellitus. In addition to lifestyle changes, which one of the following would you prescribe initially?
|
Metformin (Glucophage)
Metformin is widely accepted as the first-line drug for type 2 diabetes mellitus. It is relatively effective, safe, and inexpensive, and has been used widely for many years. Unlike other oral hypoglycemics and insulin, it does not cause weight gain. It should be started at the same time as lifestyle modifications, rather than waiting to see if a diet and exercise regimen alone will work. If metformin is not effective, a sulfonylurea, a thiazolidinedione, or insulin can be added, with the choice based on the severity of the hyperglycemia. |
|
|
What medication most increases insulin sensitivity in an overweight patient with diabetes mellitus?
A. Metformin (Glucophage) B. Acarbose (Precose) C. Glyburide (DiaBeta, Micronase) D. NPH insulin |
Metformin (Glucophage)
Metformin increases insulin sensitivity much more than sulfonylureas or insulin. This means lower insulin levels achieve the same level of glycemic control, and may be one reason that weight changes are less likely to be seen in diabetic patients on metformin. Acarbose is an α-glucosidase inhibitor that delays glucose absorption. |
|
|
A 40-year-old female comes to your office for a routine examination. She has been in good health and has no complaints other than obesity. Her mother is diabetic and the patient has had a child that weighed 9 lb at birth. Her examination is negative except for her obesity. A fasting glucose level is 128 mg/dL, and when repeated 2 days later it is 135 mg/dL. What intervention would be most appropriate at this point?
|
Diagnose type 2 diabetes mellitus and begin diet and exercise therapy
The criteria for diagnosing diabetes mellitus include any one of the following: symptoms of diabetes (polyuria, polydipsia, weight loss) plus a casual glucose level ≥200 mg/dL; a fasting plasma glucose level ≥126 mg/dL; or a 2-hour postprandial glucose level ≥200 mg/dL after a 75 gram glucose load. In the absence of unequivocal hyperglycemia the test must be repeated on a different day. The criteria for impaired glucose homeostasis include either a fasting glucose level of 100-125 mg/dL (impaired fasting glucose) or a 2-hour glucose level of 140-199 mg/dL on an oral glucose tolerance test. Normal values are now considered <100 mg/dL for fasting glucose and <140 mg/dL for the 2-hour glucose level on an oral glucose tolerance test. |
|
|
A 35-year-old male with a previous history of kidney stones presents with symptoms consistent with a recurrence of this problem. The initial workup reveals elevated serum calcium. What test would be most appropriate at this point?
|
Serum parathyroid hormone
A patient with a recurrent kidney stone and an elevated serum calcium level most likely has hyperparathyroidism, and a parathyroid hormone (PTH) level would be appropriate. Elevated PTH is caused by a single parathyroid adenoma in approximately 80% of cases. The resultant hypercalcemia is often discovered in asymptomatic persons having laboratory work for other reasons. An elevated PTH by immunoassay confirms the diagnosis. In the past, tests based on renal responses to elevated PTH were used to make the diagnosis. These included blood phosphate, chloride, and magnesium, as well as urinary or nephrogenous cyclic adenosine monophosphate. These tests are not specific for this problem, however, and are therefore not cost-effective. Serum calcitonin levels have no practical clinical use. |
|
|
A healthy 72-year-old female comes to your office for a follow-up visit. She has hypertension which is well controlled with an ACE inhibitor. Routine laboratory tests are normal except for a serum calcium level of 10.8 mg/dL (N 8.5–10.5). A repeat calcium level is 11.1 mg/dL. Which one of the following would be most appropriate at this point?
A. Radiographs of the hands B. An osteocalcin level C. An intact parathyroid hormone (PTH) level D. Bone densitometry |
An intact parathyroid hormone (PTH) level
In primary hyperparathyroidism, hypercalcemia is the result of excessive PTH secretion by one or more abnormal, enlarged parathyroid glands. Laboratory findings in most patients with primary hyperparathyroidism reflect the mild clinical presentation of the disorder. The serum calcium level is often 1 mg/dL or more above the upper limits of normal. Bone radiographs may show the classic changes of subperiosteal bone resorption in the occasional patient with hyperparathyroidism, but in most cases they are normal or may show osteopenia. Osteocalcin is an osteoblast-specific protein. It is a marker of increased skeletal turnover, and it is usually not indicated clinically. The development of highly sensitive and specific assays for intact, largely active PTH has simplified the assessment of parathyroid activity. Bone densitometry is a test to determine the degree of osteoporosis. |
|
|
A 68-year-old white female is hospitalized for pneumonia. She appears acutely ill and slightly lethargic. Her examination is consistent with right lower lobe pneumonia but is otherwise normal. Her pulse rate is 90 beats/min and regular. Her weight is normal for height. Her TSH level is 9.0 _U/mL (N 1.0–5.0). The most appropriate initial step for managing her thyroid abnormality is:
A. Follow-up testing after discharge B. Free T4 and rT3 levels now |
f/u testing after discharge
The likelihood that this patient has significant thyroid disease is very low given the minimal elevation of TSH, normal clinical examination, and concomitant pneumonia. The elevated TSH level is likely due to her illness rather than to any underlying thyroid condition. Even if she had a palpable thyroid, her risk of hypothyroidism would be on the order of 5%. A TSH level µU/mL in an acutely ill patient reflects true hypothyroidism only about 40% of the time. It is likely that this patient has sick euthyroid syndrome and that follow-up thyroid testing after discharge when she has recovered is appropriate and is very likely to be normal. Free T4, rT3, and TSH levels would be appropriate for subsequent evaluation if the patient’s laboratory values did not return to normal after resolution of the pneumonia. |
|
|
A 75-year-old white male with well-controlled type 2 diabetes mellitus is scheduled for an abdominal CT scan with oral and intravenous iodinated contrast. Which medication should be withheld 48 hours before and after the procedure?
|
Metformin (Glucophage)
Metformin should be withheld before and after radiographic procedures with contrast, due to its interaction with iodinated contrast materials. This interaction may cause impaired renal function or lactic acidosis. |
|
|
A 70-year-old white female comes to your office for an initial visit. She has taken levothyroxine (Synthroid), 0.3 mg/day, for the last 20 years. Although a recent screening TSH was fully suppressed at <0.1 µU/mL, she claims that she has felt “awful” when previous physicians have attempted to lower her dosage. You explain that a serious potential complication of her current thyroid medication is:
|
Hip fracture
Women older than 65 years of age who have low serum TSH levels, indicating physiologic hyperthyroidism, are at increased risk for new hip and vertebral fractures. Use of thyroid hormone itself does not increase the risk of fracture if TSH levels are normal. |
|
|
In evaluating an adult with anemia, which one of the following findings most reliably indicates a diagnosis of iron deficiency anemia?
A. Low total iron-binding capacity B. Low serum iron C. Low serum ferritin D. Microcytosis E. Hypochromia |
Low serum ferritin
The total iron-binding capacity is elevated, not decreased, in iron deficiency anemia. As an acute-phase reactant, serum iron may be decreased in response to inflammation even when total body stores of iron are not decreased. Microcytosis and hypochromia are both features of iron deficiency anemia occurring late in its development, but both can also be seen in the thalassemias. Serum ferritin is also an acute-phase reactant but is normal or elevated in the face of an inflammatory process. A low serum ferritin, however, is diagnostic for iron deficiency even in its early stages. |
|
|
Use of the artificial sweetener aspartame (NutraSweet) is contraindicated in patients who have:
|
Phenylketonuria
Aspartame is completely hydrolyzed in the gut to methanol, aspartic acid, and phenylalanine, and is therefore contraindicated in patients with phenylketonuria. |
|
|
The recommended time to screen asymptomatic pregnant women without risk factors for gestational diabetes is
|
At 24–28 weeks' gestation
The recommended time to screen for gestational diabetes is 24–28 weeks' gestation. The patient may be given a 50-g oral glucose load followed by a glucose determination 1 hour later. |
|
|
Routine blood tests frequently reveal elevated calcium levels. When this elevation is associated with elevated parathyroid hormone levels, what are the indications for parathyroid surgery?
|
Indications for parathyroid surgery include
● Age < 50 ● Kidney stones ● Serum calcium 1.0 mg/dL above the upper limit of normal ● Decreased bone density |
|
|
What is a cause of thyrotoxicosis characterized by a decreased radioactive iodine uptake?
|
Subacute thyroiditis
[distractors: Grave's disease, toxic nodule] Thyrotoxicosis with a high 24-hour radioactive iodine uptake (RAIU) is caused by Graves’ disease, toxic multinodular goiter, a solitary hot nodule, a TSH-secreting pituitary tumor, molar pregnancy, and choriocarcinoma. Thyrotoxicosis with a low 24-hour RAIU may be the result of subacute thyroiditis, sporadic silent thyroiditis, postpartum lymphocytic thyroiditis, radiation-induced thyroiditis, iodine-induced thyroiditis, thyrotoxicosis factitia, metastatic follicular thyroid cancer, and struma ovarii. |
|
|
At a routine visit, a 50-year-old white female with a 10-year history of type 2 diabetes mellitus has a blood pressure of 145/90 mm Hg and significant microalbuminuria. What would be an absolute contraindication to use of an ACE inhibitor in this patient?
|
A previous history of angioneurotic edema
[other choices: Renal insufficiency, Asthma, A history of recent myocardial infarction , A cardiac ejection fraction <25% ] Angioneurotic edema can be life-threatening, and ACE inhibitors should not be given to patients with a history of this condition from any cause. Elevated creatinine levels are not an absolute contraindication to ACE inhibitor therapy. Myocardial infarction and a reduced cardiac ejection fraction are indications for ACE inhibitor therapy. ACE inhibitors do not affect asthma |
|
|
Your 57-year-old white male patient has been in the ICU for the past 10 days recovering from an exploratory laparotomy performed for a perforated duodenal ulcer. Postoperatively he developed acute renal failure and sepsis. When the patient became hypothermic 3 days ago, the resident on duty ordered a thyroid function panel and obtained the following results: T4 RIA 4 µg/dL (N 5–12) T3 RIA 60 ng/dL (N 70–190) TSH 2.0 µU/mL (N 0.5–5.0) The patient has no previous history of thyroid disease. His gland is normal in size. His condition today is critical but stable. The most appropriate management at this time is to:
|
Continue present management
This patient in all probability has the euthyroid-sick syndrome, also known as nonthyroid illness syndrome (NTI)—the association of severe nonthyroidal illness with biochemical parameters indicative of thyroid hypofunction. Low T3 with normal T4 and low T3 with low T4 are the most common variants of this syndrome. TSH is usually normal but may be high or low. A TSH level >20 µU/mL would be inconsistent with NTI and indicates hypothyroidism. |
|
|
In a patient with a solitary thyroid nodule, what findings are associated with a higher incidence of malignancy?
|
When evaluating a patient with a solitary thyroid nodule, red flags indicating possible thyroid cancer include:
● male gender ● age <20 years or >65 years ● rapid growth of the nodule ● symptoms of local invasion such as dysphagia, neck pain, and hoarseness ● a history of head or neck radiation ● a family history of thyroid cancer ● a hard, fixed nodule >4 cm ● cervical lymphadenopathy. |
|
|
What medication can contribute to serum calcium elevation?
|
Hydrochlorothiazide
While thiazide diuretics do not cause hypercalcemia by themselves, they can exacerbate the hypercalcemia associated with primary hyperparathyroidism. Thiazides decrease the renal clearance of calcium by increasing distal tubular calcium reabsorption. Furosemide tends to lower serum calcium levels and is used in the treatment of hypercalcemia |
|
|
A 60-year-old type 2 diabetic requires urgent appendectomy. Which medication should be withheld until normal kidney function is documented at 24 and 48 hours after the surgery?
|
Metformin (Glucophage)
Administration of general anesthesia may cause hypotension, which leads to renal hypoperfusion and peripheral tissue hypoxia, with subsequent lactate accumulation. Therefore, if administration of radiocontrast material is required or urgent surgery is needed, metformin should be withheld and hydration maintained until preserved kidney function is documented at 24 and 48 hours after the intervention. |
|
|
What side effect is more likely to occur with glipizide (Glucotrol) than with metformin (Glucophage)?
|
Hypoglycemia
Metformin is a biguanide used as an oral antidiabetic agent. One of its main advantages over some other oral agents is that it does not cause hypoglycemia. Lactic acidosis, while rare, can occur in patients with renal impairment. In contrast to most other agents for the control of elevated glucose, which often cause weight gain, metformin reduces insulin levels and more frequently has a weight-maintaining or even a weight loss effect. Gastrointestinal distress is a common side-effect of metformin, particularly early in therapy. |
|
|
In a patient with HIV infection, the threshold for initiating treatment for tuberculosis after PPD screening is induration greater than or equal to:
|
5.0 mm
|
|
|
Hemoglobin A1c assays are INACCURATE in patients with:
|
Sickle cell disease
The glycosylated hemoglobin assay is rendered inaccurate by conditions affecting red blood cell survival, such as sickle cell disease or the presence of hemoglobin C. |
|
|
A small child with failure to thrive is found to have a bone age that is markedly delayed relative to height age and chronologic age. The most likely etiology is:
|
Hypothyroidism
Hypothyroidism is associated with markedly delayed bone age relative to height age and chronologic age. In cystic fibrosis, bone age and height age are equivalent, but both lag behind chronologic age. Children with chromosomal anomalies such as trisomy 21 (Down syndrome) or XO have a height age which is delayed relative to bone age. This pattern is also seen as a result of maternal substance abuse. |
|
|
Chronic excess thyroid hormone replacement over a number of years in postmenopausal women can lead to:
|
Osteoporosis
Even mild chronic excess thyroid hormone replacement over many years can cause bone mineral resorption, increase serum calcium levels, and lead to osteoporosis. The elevated calcium decreases parathyroid hormone. Goiter is an indicator, not a cause, for hormone replacement. Osteoarthritis is not related to thyroid hormone replacement. |
|
|
A 36-hour-old male is noted to have jaundice extending to the abdomen. He is breastfeeding well, 10 times a day, and is voiding and passing meconium-stained stool. He was born by normal spontaneous vaginal delivery at 38 weeks gestation after an uncomplicated pregnancy. The mother's blood type is A positive with a negative antibody screen. The infants total serum bilirubin is 13.0 mg/dL. Which one of the following would be the most appropriate management of this infants jaundice?
|
Continue breastfeeding, evaluate for risk factors, and initiate phototherapy if at risk
In 2004 the American Academy of Pediatrics published updated clinical practice guidelines on the management of hyperbilirubinemia in the newborn infant at 35 or more weeks gestation. These guidelines focus on frequent clinical assessment of jaundice, and treatment based on the total serum bilirubin level, the infants age in hours, and risk factors. Phototherapy should not be started based solely on the total serum bilirubin level. The guidelines encourage breastfeeding 8-12 times daily in the first few days of life to prevent dehydration. There is no evidence to support supplementation with water or dextrose in water in a nondehydrated breastfeeding infant. This infant is not dehydrated and is getting an adequate number of feedings, and there is no reason to discontinue breastfeeding at this time. |
|
|
A 3-week-old male is brought to your office because of a sudden onset of bilious vomiting of several hours duration. He is irritable and refuses to breastfeed, but stools have been normal. He was delivered at term after a normal pregnancy, and has had no health problems to date. A physical examination shows a fussy child with a distended abdomen. Radiography of the abdomen shows a double bubble sign. Which one of the following is the most likely diagnosis?
|
midgut volvulus
(Other choices:Infantile colic , Necrotizing enterocolitis, Hypertrophic pyloric stenosis, Intussusception) Volvulus may present in one of three ways: as a sudden onset of bilious vomiting and abdominal pain in a neonate; as a history of feeding problems with bilious vomiting that appears to be a bowel obstruction; or less commonly, as failure to thrive with severe feeding intolerance. The classic finding on abdominal plain films is the double bubble sign, which shows a paucity of gas (airless abdomen) with two air bubbles, one in the stomach and one in the duodenum. However, the plain film can be entirely normal. The upper gastrointestinal contrast study is considered the gold standard for diagnosing volvulus. Infantile colic usually begins during the second week of life and typically occurs in the evening. It is characterized by screaming episodes and a distended or tight abdomen. Its etiology has yet to be determined. There are no abnormalities on physical examination and ancillary studies, and symptoms usually resolve spontaneously around 12 weeks of age. Necrotizing enterocolitis is typically seen in the distressed neonate in the intensive-care nursery, but it may occasionally be seen in the healthy neonate within the first 2 weeks of life. The child will appear ill, with symptoms including irritability, poor feeding, a distended abdomen, and bloody stools. Abdominal plain films will show pneumatosis intestinalis, caused by gas in the intestinal wall, which is diagnostic of the condition. Hypertrophic pyloric stenosis is a narrowing of the pyloric canal caused by hypertrophy of the musculature. It usually presents during the third to fifth weeks of life. Projectile vomiting after feeding, weight loss, and dehydration are common. The vomitus is always nonbilious, because the obstruction is proximal to the duodenum. If a small olive-size mass cannot be felt in the right upper or middle quadrant, ultrasonography will confirm the diagnosis. Intussusception is seen most frequently between the ages of 3 months and 5 years, with 60% of cases occurring in the first year and a peak incidence at 6-11 months of age. The disorder occurs predominantly in males. The classic triad of intermittent colicky abdominal pain, vomiting, and bloody, mucous stools is encountered in only 20%-40% of cases. At least two of these findings will be present in approximately 60% of patients. The abdomen may be distended and tender, and there may be an elongated mass in the right upper or lower quadrants. Rectal examination may reveal either occult blood or frankly bloody, foul-smelling stool, classically described as currant jelly. An air enema using fluoroscopic guidance is useful for both diagnosis and treatment. |
|
|
A previously healthy 3-year-old male is brought to your office with a 4-hour history of abdominal pain followed by vomiting. Just after arriving at your office he passes bloody stool. A physical examination reveals normal vital signs, and guarding and tenderness in the right lower quadrant. A rectal examination shows blood on the examining finger. Which one of the following is the most likely diagnosis?
|
Meckels diverticulum
Meckels diverticulum is the most common congenital abnormality of the small intestine. It is prone to bleeding because it may contain heterotopic gastric mucosa. Abdominal pain, distention, and vomiting may develop if obstruction has occurred, and the presentation may mimic appendicitis. Children with appendicitis have right lower quadrant pain, abdominal tenderness, guarding, and vomiting, but not rectal bleeding. With acute viral gastroenteritis, vomiting usually precedes diarrhea (usually without blood) by several hours, and abdominal pain is typically mild and nonfocal with no localized tenderness. The incidence of midgut volvulus peaks during the first month of life, but it can present anytime in childhood. Volvulus may present in one of three ways: as a sudden onset of bilious vomiting and abdominal pain in the neonate; as a history of feeding problems with bilious vomiting that now appears to be due to bowel obstruction; or, less commonly, as a failure to thrive with severe feeding intolerance. Necrotizing enterocolitis is typically seen in the neonatal intensive-care unit, occurring in premature infants in their first few weeks of life. The infants are ill, and signs and symptoms include lethargy, irritability, decreased oral intake, abdominal distention, and bloody stools. A plain abdominal film showing pneumatosis intestinalis, caused by gas in the intestinal wall, is diagnostic of this disease. |
|
|
The mother of an 4-week-old male asks about the viral gastroenteritis vaccine. You advise that it is
|
initiated at 6-12 weeks of age
Rotavirus vaccine (RotaTeq) was licensed in February 2006 to protect against viral gastroenteritis. The Advisory Committee on Immunization Practices recommends the routine vaccination of infants with three doses to be given at 2, 4, and 6 months of age. The first dose should be given between 6 and 12 weeks of age, and subsequent doses should be given at 4- to 10-week intervals, but all three doses should be administered by 32 weeks of age. Unlike the vaccine RotaShield, which was marketed in 1999, RotaTeq is not known to increase the risk for intussusception. |
|
|
What is a risk factor for acute pancreatitis?
|
Gallstones
Pancreatitis is most closely associated with gallstones, extreme hypertrigliceridemia, and excessive alcohol use. Gastroesophageal reflux disease, pyelonephritis, drug abuse (other than alcohol), and angiotensin receptor blocker use are not risk factors for the development of pancreatitis. |
|
|
Treatment for Helicobacter pylori infection will reduce or improve which one of the following?
A. The risk of peptic ulcer bleeding from chronic NSAID therapy B. The risk of developing gastric cancer in asymptomatic patients C. Symptoms of nonulcer dyspepsia D. Symptoms of gastroesophageal reflux disease |
The risk of peptic ulcer bleeding from chronic NSAID therapy
Eradication of Helicobacter pylori significantly reduces the risk of ulcer recurrence and rebleeding in patients with duodenal ulcer, and reduces the risk of peptic ulcer development in patients on chronic NSAID therapy. Eradication has minimal or no effect on the symptoms of nonulcer dyspepsia and gastroesophageal reflux disease. Although H. pylori infection is associated with gastric cancer, no trials have shown that eradication of H. pylori purely to prevent gastric cancer is beneficial. |
|
|
Which one of the following is associated with ulcerative colitis rather than Crohn’s disease?
A. The absence of rectal involvement B. Transmural involvement of the colon C. Segmental noncontinuous distribution of inflammation D. Fistula formation E. An increased risk of carcinoma of the colon |
an increased risk of carcinoma of the colon
Long-standing ulcerative colitis (UC) is associated with an increased risk of colon cancer. The greater the duration and anatomic extent of involvement, the greater the risk. Initial colonoscopy for patients with pancolitis of 8-10 years duration (regardless of the patient's age) should be followed up with surveillance examinations every 1-2 years, even if the disease is in remission. All of the other options listed are features typically associated with Crohn’s disease. Virtually all patients with UC have rectal involvement, even if that is the only area affected. In Crohn’s disease, rectal involvement is variable. Noncontinuous and transmural inflammation are also more common with Crohn’s disease. Transmural inflammation can lead to eventual fistula formation, which is not seen in UC. |
|
|
A 54-year-old white female has been taking amoxicillin for 1 week for sinusitis. She has developed diarrhea and has had 6-8 stools per day for the past 2 days. Examination shows the patient to be well hydrated with normal vital signs and a normal physical examination. The stool is positive for occult blood, and a stool screen for Clostridium difficile toxin is positive. The most appropriate treatment at this time would be
|
metronidazole (Flagyl) orally
Many antibiotics can induce pseudomembranous colitis. Although oral vancomycin was once the initial drug of choice for C. difficile, oral metronidazole is now the first-line agent because of cost considerations and because of concerns about the development of vancomycin-resistant organisms. If the patient has refractory symptoms despite treatment with oral metronidazole, then oral vancomycin would be appropriate. Vancomycin given orally is not absorbed, leading to high intraluminal levels of the drug. |
|
|
Current thinking regarding infantile colic is that the cause is
|
unknown
Colic is a frustrating condition for parents and doctors alike. The parents would like an explanation and relief, and physicians would like to offer these things. At this time, however, in spite of numerous studies and theories, the cause of colic remains unknown. |
|
|
An outbreak of pediatric diarrhea has swept your community. You evaluate a 30-month-old male who developed diarrhea yesterday. He is still breastfed. He is alert, his mucous membranes are moist, and his skin turgor is good. He passes a liquid stool in your office. Which one of the following would be the best advice with regard to his diet?
|
He should consume a normal age-appropriate diet, and continue breastfeeding
Continued oral feeding in diarrhea aids in recovery, and an age-appropriate diet should be given. Breastfeeding or regular formula should be continued. Foods with complex carbohydrates (e.g., rice, wheat, potatoes, bread, and cereals), lean meats, yogurt, fruits, and vegetables are well tolerated. Foods high in simple sugars (e.g., juices, carbonated sodas) should be avoided because the osmotic load can worsen the diarrhea. Fatty foods should be avoided as well. The BRAT diet (bananas, rice, applesauce, and toast) has not been shown to be effective. |
|
|
A 70-year-old Asian male presents with hematochezia. He has stable vital signs. Lower endoscopy is performed, but is unsuccessful due to active bleeding. What would be the next appropriate investigation?
|
next step: A technetium-99m blood pool scan
In most patients with heavy gastrointestinal bleeding, localizing the bleeding site, rather than diagnosing the cause of the bleeding, is the most important task. A lower GI series is usually nondiagnostic during heavy, active bleeding. A small-bowel radiograph may be helpful after the active bleeding has stopped, but not during the acute phase of the bleeding. A blood pool scan allows repeated scanning over a prolonged period of time, with the goal of permitting enough accumulation of the isotope to direct the arteriographer to the most likely source of the bleeding. If the scan is negative, arteriography would also be unlikely to reveal the active source of bleeding. It is also a more invasive procedure. Exploratory laparotomy may be indicated if a blood pool scan or an arteriogram is nondiagnostic and the patient continues to bleed heavily. |
|
|
A 48-year-old unemployed house painter presents to the emergency department with a gradual onset of lethargy and weakness. A physical examination is remarkable for 4+ pitting edema of the lower extremities and a prominent abdomen. Laboratory Findings Serum sodium 122 mEq/L (N 135–145) Serum osmolality 260 mOsm/kg H2O (N 280–296) Urine sodium 5 mEq/L Urine osmolality 250 mOsm/kg H2O The most likely diagnosis in this case is:
|
cirrhosis
The individual described in this case has symptomatic hyponatremia. Headache, mental confusion, nausea, and malaise are common. Seizures, stupor, and coma generally do not occur until sodium concentrations fall below 120 mEq/L. The presence of significant peripheral edema in this patient indicates extracellular fluid volume expansion, and his serum osmolality is low. In this situation, hyponatremia is usually a manifestation of an edematous state, such as hepatic cirrhosis, congestive heart failure, or the nephrotic syndrome. Although these patients have increased extracellular fluid, their intravascular fluid is depleted, and their body’s attempt to conserve sodium at the level of the kidney produces urine with a sodium concentration <20 mEq/L. They have appropriately increased arginine vasopressin (AVP) levels, resulting in a urine osmolality that is less than maximally dilute and often >100 mOsm/kg H2O. Patients with the syndrome of inappropriate antidiuretic hormone (SIADH) have normal volume status and urine sodium levels which are typically >20 mEq/L. Patients with primary polydipsia often have an underlying psychiatric disorder. They have normal volume status, and produce large volumes of very dilute urine (<50 mOsm/kg H2O). Patients with adrenal insufficiency typically have normal volume status, but may be dehydrated. Patients with salt-wasting nephropathy are typically dehydrated despite producing urine with a sodium concentration >20 mEq/L. |
|
|
A 75-year-old male complains of pain with defecation, and loose stools. This problem seems to have developed gradually over the last several months. His past medical history includes prostate cancer treated with radiation therapy 5 years ago, hypertension, and osteoarthritis. Medications include hydrochlorothiazide (HydroDIURIL), a beta-blocker, and acetaminophen. On colonoscopy, no polyps or cancer are found, but the rectal and sigmoid areas show pallor with friability and telangiectasias. The most likely diagnosis is:
|
Radiation proctitis
Chronic radiation proctitis develops months to years after radiation and is characterized by pain with defecation, diarrhea, and sometimes rectal bleeding. On colonoscopy, the mucosa is pale and friable with telangiectases which are sometimes large, multiple, and serpiginous. |
|
|
Traveler’s diarrhea can be effectively treated in the great majority of cases by a 3-day course of:
|
Ciprofloxacin (Cipro)
Fluoroquinolones such as ciprofloxacin have been shown to significantly reduce the duration and severity of traveler’s diarrhea when given for 1–3 days. Penicillin and erythromycin are not effective against the most common cause of traveler’s diarrhea, enterotoxigenic E. coli. |
|
|
In addition to routine immunizations, which vaccine is specifically indicated for adolescent males who have sex with other males?
|
Hepatitis A vaccine
Hepatitis A vaccine should be administered to unvaccinated adolescents who plan to travel to or work in an area of high endemicity of hepatitis A virus infection, those who receive clotting factors, those who have chronic liver disease or use illegal drugs, and males who have sex with males. Routine hepatitis A vaccination of all children has been proposed and implementation strategies are being studied. |
|
|
Now that the blood supply is routinely screened for antibody to hepatitis C virus (HCV), what has become the leading mode of transmission of HCV?
|
Injection drug use
Illegal drug use is currently the leading cause of new cases of hepatitis C. It is estimated that 60% of new cases of hepatitis C in the United States are due to injection drug use. Intranasal cocaine use has been associated with hepatitis C, but its importance as a route of transmission is controversial and it occurs at a much lower frequency, if it all. Sexual transmission of hepatitis C is a less frequent cause of initial infection. Hepatitis B and HIV are transmitted more efficiently by sexual contact. Men who engage in homosexual intercourse have rates of hepatitis C similar to those of heterosexuals who engage in high-risk sexual practices. Among partners who are hepatitis C–positive, male-to-female transmission seems to be more efficient. Maternal-child perinatal transmission rates are thought to be less than 6%. Breastfeeding is not thought to be a risk. Occupational transmission is infrequent. No significant household or day-care risk is thought to exist in the absence of blood exposure. |
|
|
A 53-year-old white female undergoes abdominal ultrasonography for suspected gallbladder disease. A 3-cm thin-walled, fluid-filled cyst is seen on the left kidney. What's the appropriate next step?
|
No further intervention
Simple renal cysts are incidentally seen on abdominal imaging studies in over 30% of people over age 50, and are present in up to 50% in some autopsy series. No further evaluation is indicated for cysts that meet ultrasound criteria (i.e., thin-walled, homogeneous, fluid-filled). With cysts that appear to be complex, a renal CT with contrast is indicated. MRI has been shown to be statistically superior to CT in correctly characterizing benign lesions, and may be helpful when results of a CT scan are equivocal. Simple cysts do not require aspiration or other treatment. Referral is indicated for symptomatic or complex cysts or solid masses. |
|
|
A painful thrombosed external hemorrhoid diagnosed within the first 24 hours after occurrence is ideally treated by:
|
Thrombectomy under local anesthesia
A thrombosed external hemorrhoid is described as the sudden development of a painful, tender perirectal lump. Because there is somatic innervation, the pain is intense, and increases with edema. Treatment involves excision of the acutely thrombosed tissue under local anesthesia, mild pain medication, and sitz baths. It is inappropriate to use procedures that would increase the pain, such as banding or cryotherapy. Total hemorrhoidectomy is inappropriate and unnecessary. |
|
|
Which one of the following is the best screening test for hereditary hemochromatosis?
|
Serum transferrin saturation
Hereditary hemochromatosis is the most common genetic disorder in the United States. Serum transferrin is the best and most sensitive screening test. Liver biopsy, long considered the gold standard for diagnosing hemochromatosis, is far too invasive. |
|
|
A 24-year-old mother is discharged from the hospital with her baby 24 hours after an uncomplicated labor and delivery. The baby was delivered at term, and this is her first child. You receive a call from the mother the next day because she is concerned that the baby “looks a little orange.” Which one of the following bilirubin levels would prompt phototherapy?
|
21 mg/dL at 72 hours
Bilirubin levels >17 mg/dL in full-term infants are considered pathologic rather than physiologic. In one study, infants with bilirubin concentrations over 21 mg/dL at 18–72 hours after birth had a 40% probability of severe hyperbilirubinemia developing later on. The American Academy of Pediatrics recommends initiating phototherapy for bilirubin levels based on the infant’s age: 15 mg/dL at 25–48 hours, 18 mg/dL at 49–72 hours, and 20 mg/dL at 72 hours or more. |
|
|
For 2 weeks, a 62-year-old male with biopsy-documented cirrhosis and ascites has had diffuse abdominal discomfort, fever, and night sweats. His current medications are furosemide (Lasix) and spironolactone (Aldactone). On examination, his temperature is 38.0° C (100.4° F), blood pressure 100/60 mm Hg, heart rate 92 beats/min and regular. The heart and lung examination is normal. The abdomen is soft with vague tenderness in all quadrants. There is no rebound or guarding. The presence of ascites is easily verified. Bowel sounds are quiet. The rectal examination is normal, and the stool is negative for occult blood. You perform diagnostic paracentesis and send a sample of fluid for analysis. Which one of the following findings would best establish the suspected diagnosis of spontaneous bacterial peritonitis?
|
Neutrophil count >300/mL
Diagnostic paracentesis is recommended for patients with ascites of recent onset, as well as for those with chronic ascites who present with new clinical findings such as fever or abdominal pain. A neutrophil count >250/mL is diagnostic for peritonitis. Once peritonitis is diagnosed, antibiotic therapy should be started immediately without waiting for culture results. Bloody ascites with abnormal cytology may be seen with hepatoma, but is not typical of peritonitis. The ascitic fluid pH does not become abnormal until well after the neutrophil count has risen, so it is a less reliable finding for treatment purposes. A protein level >1 g/dL is actually evidence against spontaneous bacterial peritonitis. |
|
|
A 70-year-old white male whom you are treating for hypertension has several abnormal liver function tests. He is a nondrinker and is not taking any prescription medications likely to cause hepatotoxicity. However, during more extensive history taking, he tells you that he does use some over-the-counter medications. What OTC medication is most likely responsible for the abnormal laboratory findings?
|
One long-acting niacin tablet per day
Hepatotoxicity resulting from timed-release formulations of niacin has been reported in elderly individuals. Patients may be taking this drug without their physician’s knowledge, feeling it is safe because it is a vitamin. |
|
|
A 70-year-old African-American male who has been hospitalized for 2 and a half weeks for congestive heart failure develops severe, persistent diarrhea. For the past 3 days he has had abdominal cramps and profuse semi-formed stools without mucus or blood. The patient’s current medications include captopril (Capoten), digoxin, furosemide (Lasix), subcutaneous heparin, spironolactone (Aldactone), and loperamide (Imodium). He has coronary artery disease, but has been relatively pain free since undergoing coronary artery bypass surgery 4 years ago. An appendectomy and cholecystectomy were performed in the past, and the patient has since been free of gastrointestinal disease. On physical examination his blood pressure is 100/80 mm Hg, pulse 100 beats/min and regular, and temperature 37.0° C (98.6° F). He has mild jugular venous distention and crackles at both lung bases. Examination of his heart is unremarkable, although there is 1+ dependent edema. His abdomen is diffusely tender without masses or organomegaly. Rectal examination is normal. The results of routine laboratory tests, including a CBC, chemistry profile, EKG, and urinalysis, are all normal. The stool examination shows numerous white blood cells. Of the following, the most likely diagnosis is:
|
Clostridium difficile colitis
This patient most likely has Clostridium difficile colitis, suggested by semiformed rather than watery stool, fecal leukocytes (not seen in viral gastroenteritis or sprue), and a hospital stay greater than 2 weeks. While this disease has traditionally been associated with antibiotic use, it is posing an increasing threat to patients in hospitals and chronic-care facilities who have not been given antibiotics. The primary sources for infection in such cases have been toilets, bedpans, floors, and the hands of hospital personnel. Prompt recognition and treatment is essential to prevent patient relapse and to minimize intramural epidemics. |
|
|
In an 80-year-old homebound female with constipation not adequately responding to increased fluid and psyllium (Metamucil) supplementation, the safest stimulant laxative to add to her regimen is:
|
Senna
Senna has been shown to be safe, free of significant intestinal side effects, and beneficial over the long term. Phenolphthalein and castor oil can cause malabsorption, dehydration, lipoid pneumonia, and cathartic colon. Bisacodyl suppositories used daily can cause rectal burning, and oral bisacodyl can cause hypokalemia, abdominal cramps, and vomiting. Milk of Magnesia is a saline cathartic that can cause elevated magnesium levels and dehydration, watery stools, and fecal incontinence. |
|
|
A pregnant patient is positive for hepatitis B surface antigen (HBsAg). Which one of the following would be most appropriate for her infant?
|
Hepatitis B immune globulin (HBIG) and hepatitis B vaccine at birth
Infants born to hepatitis B–positive mothers should receive both immune globulin and hepatitis B vaccine. They should receive the entire series of the vaccine, with testing for seroconversion only after completion of the vaccination series; the recommended age for testing is 9–12 months of age. |
|
|
When presenting with appendicitis, patients over the age of 65 are more likely than younger patients to have?
|
Perforation
Older patients with appendicitis are more likely to present without classic signs and symptoms. Elevated WBC counts, rebound tenderness, guarding, and fever are less reliably seen. As a result of delays in diagnosis, perforation is found in over 65% of elderly patients at the time of diagnosis. |
|
|
Your community recently experienced an outbreak of infectious diarrheal illness due to the protozoan Cryptosporidium, a chlorine-resistant organism. A reporter from the local newspaper asks you if there are other chlorine-resistant fecal organisms that could contaminate public drinking water. You would tell the reporter that such organisms include:
|
Giardia lamblia
Organisms that can persist in water environments and survive disinfection, especially chlorination, are most likely to cause disease outbreaks related to drinking water. Cryptosporidium oocysts and Giardia cysts are resistant to chlorine and are important causes of gastroenteritis from drinking water. Entamoeba histolytica and hepatitis A virus are also relatively chlorine resistant. |
|
|
Hepatitis C screening is routinely recommended for:
|
Persons with a history of illicit intravenous drug use
Patients should be routinely screened for hepatitis C if they have a history of any of the following: intravenous drug abuse no matter how long or how often, receiving clotting factor produced before 1987, persistent alanine aminotransferase elevations, or recent needle stick with HCV-positive blood. |
|
|
A nurse who completed a hepatitis B vaccine series a year ago is accidentally stuck by a needle that has just been used on a dialysis patient. The patient is known to be HBsAg-positive. Your first response should be to:
|
Test the nurse for hepatitis B antibody
Postexposure prophylaxis after hepatitis B exposure via the percutaneous route depends upon the source of the exposure and the vaccination status of the exposed person. In the case described, a vaccinated person has been exposed to a known positive individual. The exposed person should be tested for hepatitis B antibodies; if antibody levels are inadequate (<10 IU/L by radioimmunoassay, negative by enzyme immunoassay) HBIG should be administered immediately, as well as a hepatitis B vaccine booster dose. An unvaccinated individual in this same setting should receive HBIG immediately (preferably within 24 hours after exposure) followed by the hepatitis B vaccine series (injection in 1 week or less, followed by a second dose in 1 month and a third dose in 6 months). |
|
|
A 57-year-old African-American female has a partial resection of the colon for cancer. The surgical specimen has clean margins, and there is no lymph node involvement. There is no evidence of metastasis. You recommend periodic colonoscopy for surveillance, and also plan to monitor which one of the following tumor markers for recurrence?
|
Carcinoembryonic antigen (CEA)
Prostate-specific antigen (PSA) is a marker that is used to screen for prostate cancer. It is elevated in more than 70% of organ-confined prostate cancers. Alpha-tetoprotein is a marker for hepatocellular carcinoma and nonseminomatous germ cell tumor, and is elevated in 80% of hepatocellular carcinomas. CA-125 is a marker for ovarian cancer. Although it is elevated in 85% of ovarian cancers, it is elevated in only 50% of early-stage ovarian cancers. Carcinoembryonic antigen (CEA) is a marker for colon, esophageal, and hepatic cancers. It is expressed in normal mucosal cells and is overexpressed in adenocarcinoma, especially colon cancer. Though not specific for colon cancer, levels above 10 ng/mL are rarely due to benign disease. CEA levels typically return to normal within 4–6 weeks after successful surgical resection. CEA elevation occurs in nearly half of patients with a normal preoperative CEA level that have cancer recurrence. Cancer antigen 27.29 (CA 27-29) is a tumor marker for breast cancer. It is elevated in about 33% of early-stage breast cancers and about 67% of late-stage breast cancers. Some tumor markers, such as CEA, alpha-fetoprotein, and CA-125, may be more helpful in monitoring response to therapy than in detecting the primary tumor. |
|
|
A 60-year-old male indicates that he occasionally brings up what appears to be undigested food long after his meal. He also admits that he sometimes chokes on food, and that his wife says he has bad breath. The most likely diagnosis is:
|
Zenker’s diverticulum
The combination of halitosis, late regurgitation of undigested food, and choking suggests Zenker’s diverticulum. Patients may also have dysphagia and weight loss. The diagnosis is usually made with a barium swallow. The treatment is surgical. |
|
|
A healthy 8-month-old white male has suddenly developed recurrent bouts of what appears to be severe abdominal pain. He cries inconsolably and draws up his legs, but does not seem ill between episodes. He has vomited and on examination has a small amount of bloody mucoid stool in his diaper and a palpable mass in his undistended right upper abdomen. The most likely diagnosis is:
|
Intussusception
This case presentation is fairly typical for intussusception, the “telescoping” of a portion of the intestine into itself with obstruction and crampy pain. It generally occurs between the ages of 6 months and 24 months. A sausage-shaped mass is often palpable as a result of the ileum being trapped within the colon. The presence of bloody mucus supports the diagnosis. Pyloric stenosis generally occurs in the first 4–6 weeks of life (although it can occur as late as the fifth month) with a striking first-born male predominance. Emesis is the most prominent feature of pyloric stenosis; it is usually painless, and there are no bloody stools. The small pyloric mass, which feels like an olive, may be palpable at the margin of the right rectus muscle. The onset is more insidious than with intussusception. Duodenal atresia presents shortly after birth with vomiting and a “double-bubble” on a radiograph, indicating a gas-filled stomach and proximal duodenum. A Meckel’s diverticulum may rarely be found at the lead point of an intussusception, but it usually presents as a cause of recurrent abdominal pain in later life. Gastrochisis is an antenatal evisceration through a small paraumbilical defect that is present at birth. |
|
|
A 19-year-old white male with a history of fever, fatigue, weight loss, and mild diarrhea of 2 months’ duration is found to have a palpable mass in the right lower quadrant of the abdomen. The most likely diagnosis is:
|
Crohn’s disease (regional enteritis)
When Crohn’s disease affects primarily the distal small intestine (regional enteritis), a most characteristic clinical pattern emerges. A young person, usually in the second or third decade, will present with a period of episodic abdominal pain, largely postprandial and often periumbilical, occasionally with low-grade fever and mild diarrhea. Anorexia, nausea, and vomiting may also be present. Weight loss is frequent. Some patients may be aware of tenderness in the right lower quadrant and even of a palpable mass in that region. |
|
|
A 52-year-old white male has chronic musculoskeletal pain. He has been using frequent doses of Extra-Strength Tylenol with good results. He is concerned that he may be taking too much and asks what his maximum daily dosage of acetaminophen should be. He weighs 70 kg (154 lb).
|
max = 4000 mg
The maximum daily dosage for all acetaminophen preparations is 4000 mg. Acetaminophen is used in more combination products than any other drug, for a number of different indications. An FDA panel has recommended that stronger warnings about hepatotoxicity be added to the label information for acetaminophen. Because it is used so frequently and is present in so many different preparations, care must be taken not to exceed the maximum 24-hour dosage in order to avoid hepatotoxicity. |
|
|
Outbreaks of diarrheogenic Escherichia coli 0157:H7 have been associated with what type of food?
|
Ground beef
Recent outbreaks of E. coli 0157:H7-related illnesses have been associated with contaminated ground beef bought either uncooked in supermarkets or as cooked hamburgers at fast-food restaurants. |
|
|
What patients should be screened for hepatitis C virus (HCV) infection?
|
Hepatitis C (HCV) screening is indicated for:
● recipients of a transfusion prior to July 1992 ● patients with needlestick or mucosal exposure to HCV ● children born to mothers with HCV infection. |
|
|
Are serum antibody tests useful in the diagnosis of celiac disease (gluten-sensitive enteropathy) in adults?
|
Serum antibody testing, especially IgA antiendomysial antibody, is highly sensitive and specific and readily available at a cost of about $100 to $200. Definitive diagnosis generally requires esophagogastroduodenoscopy with a biopsy of the distal duodenum to detect characteristic villous flattening.
|
|
|
A 72-year-old Asian female is found to have asymptomatic gallstones on abdominal ultrasonography performed to evaluate an abdominal aortic aneurysm. Which one of the following would be the most appropriate management for the gallstones?
|
Observation
Gallstones are frequently discovered on a diagnostic workup for an unrelated problem. Only 1%–2% of persons with asymptomatic gallstones will require cholecystectomy in a given year, and two-thirds of patients with asymptomatic gallstones will remain symptom free over a 20-year period. The longer the patient remains asymptomatic, the more likely that no symptoms will develop in the future. This patient may have had gallstones for several years, and the best management would be to do nothing unless symptoms develop. |
|
|
A patient with ascites is suspected to have secondary hyperaldosteronism. What would be typical levels of electrolytes in an aliquot specimen of urine?
|
Sodium 2 mEq/L, potassium 40 mEq/L
Secondary hyperaldosteronism is characterized by sodium retention, and thus decreased urinary sodium excretion, while potassium secretion is normal to increased |
|
|
A 15-year-old African-American male presents to the emergency department with a chief complaint of fever, abdominal pain, nausea, and anorexia. In addition to the usual laboratory evaluation, which imaging modalities would be most helpful for confirming a diagnosis of appendicitis?
|
A spiral CT scan of the abdomen
A retrospective review of 650 patients with suspected appendicitis showed a sensitivity of 97% and a specificity of 98% for spiral CT. In patients in whom the clinical diagnosis was uncertain, sensitivity was 92% and specificity was 85%. Two prospective studies comparing ultrasonography with spiral CT have favored spiral CT. Ultrasonography is used in women who are pregnant and women in whom there is a high degree of suspicion of gynecologic disease. Abdominal radiography has low specificity and sensitivity for the diagnosis of acute appendicitis. Air contrast barium enema also has low accuracy. Limitations of MRI include increased cost, decreased availability, and increased examination time compared to CT. |
|
|
A 38-year-old male who is a new patient reports mild intermittent jaundice without other associated symptoms for the past several years. His liver function tests are normal except for a total bilirubin of 1.3 mg/dL (N 0.3–1.0) and an indirect or unconjugated bilirubin of 1.0 mg/dL (N 0.2–0.8). His CBC is normal. His past medical and surgical history is unremarkable. Findings are similar on repeat laboratory testing. The most likely diagnosis is:
|
Gilbert’s syndrome
Gilbert’s syndrome is the most common inherited disorder of bilirubin metabolism. In patients with a normal CBC and liver function tests, except for recurrent mildly elevated total and unconjugated hyperbilirubinemia, the most likely diagnosis is Gilbert’s syndrome. Fasting, heavy physical exertion, sickle cell anemia, and drug toxicity can also cause hyperbilirubinemia. |
|
|
A 24-year-old white female presents to the office with a 6-month history of abdominal pain. A physical examination, including pelvic and rectal examinations, is normal. What complaint would indicate a need for further evaluation?
|
Worsening of symptoms at night
Irritable bowel syndrome (IBS) is a benign, chronic symptom complex of altered bowel habits and abdominal pain. It is the most common functional disorder of the gastrointestinal tract. The presence of nocturnal symptoms is a red flag which should alert the physician to an alternate diagnosis and may require further evaluation. |
|
|
Which one of the following is the most common cause of infectious enteritis in children in temperate climates?
|
Human rotavirus
|
|
|
A family of four, consisting of the parents, a 4-year-old daughter, and a teenage son, is planning a trip to Guatemala with a church group. Which one of the following is appropriate advice concerning traveler’s diarrhea?
|
All family members may use an antimotility agent such as loperamide (Imodium) for mild disease
Loperamide may be used for mild non-dysenteric traveler’s diarrhea in patients greater than 2 years of age. Parasites rarely cause traveler’s diarrhea. Ciprofloxacin is a good choice for self-treatment of severe or dysenteric diarrhea in adults, but should not be used in children. Prophylactic antibiotics are rarely indicated. |
|
|
Which one of the following is true regarding gastroesophageal reflux (GER) in infants and children?
|
GER in infants usually resolves by 1 year of age without treatment
Gastroesophageal reflux (GER) is a functional process occuring in a healthy infant. It is common and self-limited, and represents a physiologic process of “spitting up.” GER occurs in the absence of poor weight gain, irritability, cough, pain, or anemia. The majority of infants with GER are thriving. It is important to consider other systemic disorders, and rule them out when appropriate. Possible causes of spitting up include pyloric stenosis, infections (e.g., gastrointestinal, genitourinary), and metabolic disorders. It is not necessary to perform a diagnostic evaluation prior to starting drug therapy unless a structural defect is highly suspected. GER in infants is usually self-limited and resolves by 1 year of age. |
|
|
A 36-year-old female makes an appointment because her husband of 12 years was just diagnosed with hepatitis C when he tried to become a blood donor for the first time. He recalls multiple blood transfusions following a motorcycle crash in 1988. His wife denies past liver disease, blood transfusions, and intravenous drug use. She has had no other sexual partners. The couple has three children. Which one of the following is the best advice about testing the wife and their three children?
|
She should be offered testing because sexual transmission is possible
Key risk factors for hepatitis C infection are long-term hemodialysis, intravenous drug use, blood transfusion or organ transplantation prior to 1992, and receipt of clotting factors before 1987. Sexual transmission is very low but possible, and the likelihood increases with multiple partners. The lifetime transmission risk of hepatitis C in a monogamous relationship is less than 1%, but the patient should be offered testing because she may choose to confirm that her test is negative. If the mother is seronegative, the children are at no risk. Maternal-fetal transmission is rare except in the setting of co-infection with HIV. Hepatitis C is insidious, and symptoms do not correlate with the extent of the disease. Normal liver enzyme levels do not indicate lack of infectivity. There is no risk to household contacts. Current HCV antibody tests are more than 99% sensitive and specific and are recommended for screening at-risk populations. |
|
|
In elderly patients with asymptomatic gallstones, which one of the following is an indication for elective cholecystectomy because of the increased risk of gallbladder carcinoma?
|
Chronic calculous cholecystitis (“porcelain” gallbladder)
Carcinoma of the gallbladder is a rare condition, and prophylactic cholecystectomy to prevent its occurrence is therefore usually not justified. The exception is when chronic calculous cholecystitis is present. This condition is associated with a 20% incidence of gallbladder carcinoma. |
|
|
A moderately obese 50-year-old African-American female presents with colicky right upper quadrant pain that radiates to her right shoulder. What is considered the best study to confirm the likely cause of the patient’s symptoms?
|
Abdominal ultrasonography
The symptom complex presented is typical of cholelithiasis. Plain radiography of the abdomen may reveal radiopaque gallstones, but will not reveal radiolucent stones or biliary dilatation. Although rarely used, oral cholecystography is 98% accurate, but only when compliance is assured, the contrast agent is absorbed, and liver function is normal. Abdominal ultrasonography is considered the best study to confirm this diagnosis because of its high sensitivity and its accuracy in detecting gallstones. A barium swallow will identify some functional and structural esophageal abnormalities, but will not focus on the suspected organ in this case. The same is true of esophagogastroscopy. |
|
|
A 32-year-old white female at 16 weeks' gestation presents to your office with right lower quadrant pain. Which one of the following imaging studies would be most appropriate for initial evaluation of this patient?
|
Ultrasonography of the abdomen
CT has demonstrated superiority over transabdominal ultrasonography for identifying appendicitis, associated abscess, and alternative diagnoses. However, ultrasonography is indicated for the evaluation of women who are pregnant and women in whom there is a high degree of suspicion for gynecologic disease. |
|
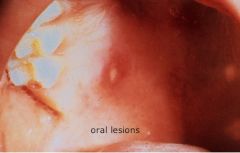
A 4-year-old white male is brought to your office in late August. His mother tells you that over the past few days he has developed a rash on his hands and sores in his mouth. On examination you note a vesicular exanthem on his hands, with lesions ranging from 3 to 6 mm in diameter. The oral lesions are shallow, whitish, 4- to 8-mm ulcerations distributed randomly over the hard palate, buccal mucosa, gingiva, tongue, lips, and pharynx. Except for a temperature of 37.4°C (99.3°F), the remainder of the examination is normal. The most likely diagnosis is
|

hand, foot, and mouth disease
Hand, foot, and mouth disease is a mild infection occurring in young children, and is caused by coxsackievirus A16, or occasionally by other strains of coxsackie- or enterovirus. In addition to the oral lesions, vesicular lesions may occur on the feet and nonvesicular lesions may occur on the buttocks. A low-grade fever may also develop. Herpangina is also caused by coxsackieviruses, but it is a more severe illness characterized by severe sore throat and vesiculo-ulcerative lesions limited to the tonsillar pillars, soft palate, and uvula, and occasionally the posterior oropharynx. Temperatures can range to as high as 41°C (106°F). |
|

A newborn male has a skin eruption on his forehead, nose, and cheeks. The lesions are mostly closed comedones with a few open comedones, papules, and pustules. No significant erythema is seen. Which one of the following is the most likely diagnosis?
|

Acne neonatorum
Acne neonatorum occurs in up to 20% of newborns. It typically consists of closed comedones on the forehead, nose, and cheeks, and is thought to result from stimulation of sebaceous glands by maternal and infant androgens. Parents should be counseled that lesions usually resolve spontaneously within 4 months without scarring. |
|

A 5-year-old white male has an itchy lesion on his right foot. He often plays barefoot in a city park that is subject to frequent flooding. The lesion is located dorsally between the web of his right third and fourth toes, and extends toward the ankle. It measures approximately 3 cm in length, is erythematous, and has a serpiginous track. The remainder of his examination is within normal limits. What is the most likely cause of these findings?
|
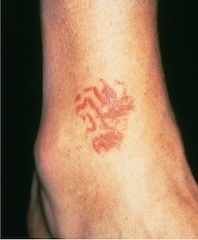
Dog or cat hookworm (Ancylostoma species)
This patient has cutaneous larva migrans, a common condition caused by dog and cat hookworms. Fecal matter deposited on soil or sand may contain hookworm eggs that hatch and release larvae, which are infective if they penetrate the skin. Walking barefoot on contaminated ground can lead to infection. |
|

A middle-aged hairdresser presents with a complaint of soreness of the proximal nail folds of several fingers on either hand, which has slowly worsened over the last 6 months. The nails appear thickened and distorted. Otherwise she is healthy and has no evidence of systemic disease. What would be the most effective initial treatment?
|

Topical betamethasone dipropionate (Diprolene) applied twice daily to the nail folds for 3-4 weeks
Chronic paronychia is a common condition in workers whose hands are exposed to chemical irritants or are wet for long periods of time. This patient is an otherwise healthy hairdresser, with frequent exposure to irritants. The patient should be advised to avoid exposure to harsh chemicals and water. In addition, the use of strong topical corticosteroids over several weeks can greatly reduce the inflammation, allowing the nail folds to return to normal and helping the cuticles recover their natural barrier to infection. Soaking in iodine solution would kill bacteria, but would also perpetuate the chronic irritation. Because the condition is related to chemical and water irritation, a prolonged course of antibiotics should not be the first treatment step, and could have serious side effects. |
|
|
A 46-year-old female presents to your office with a 2-week history of pain in her left shoulder. She does not recall any injury, and the pain is present when she is resting and at night. Her only chronic medical problem is type 2 diabetes mellitus.
On examination, she has limited movement of the shoulder and almost complete loss of external rotation. Radiographs of the shoulder are normal, as is her erythrocyte sedimentation rate. Which one of the following is the most likely diagnosis? |
Frozen shoulder
Frozen shoulder is an idiopathic condition that most commonly affects patients between the ages of 40 and 60. Diabetes mellitus is the most common risk factor for frozen shoulder. Symptoms include shoulder stiffness, loss of active and passive shoulder rotation, and severe pain, including night pain. Laboratory tests and plain films are normal; the diagnosis is clinical (SOR C). Frozen shoulder is differentiated from chronic posterior shoulder dislocation and osteoarthritis on the basis of radiologic findings. Both shoulder dislocation and osteoarthritis have characteristic plain film findings. A patient with a rotator cuff tear will have normal passive range of motion. Impingement syndrome does not affect passive range of motion, but there will be pain with elevation of the shoulder |
|
|
Intravenous magnesium is used to correct which type of arrhythmia?
|
Ventricular tachycardia of torsades de pointes
A well-known use of intravenous magnesium is for correcting the uncommon ventricular tachycardia of torsades de pointes. Results of a meta-analysis suggest that 1.2–10.0 g of intravenous magnesium sulfate also is a safe and effective strategy for the acute management of rapid atrial fibrillation. |
|
|
A 52-year-old female with a 60-pack-year history of cigarette smoking and known COPD presents with a 1-week history of increasing purulent sputum production and shortness of breath on exertion. Should antibiotics be given?
|
Antibiotics should be prescribed
Antibiotic use in moderately or severely ill patients with a COPD exacerbation reduces the risk of treatment failure or death, and may also help patients with mild exacerbations. Brief courses of systemic corticosteroids shorten hospital stays and decrease treatment failures. |
|

During rounds, you notice a new rash on a full-term 2-day-old white female. It consists of 1-mm pustules surrounded by a flat area of erythema, and is located on the face, trunk, and upper arms. An examination is otherwise normal, and she does not appear ill.
Which one of the following is the most likely diagnosis? |

Erythema toxicum neonatorum
This infant has the typical “flea-bitten” rash of erythema toxicum neonatorum (ETN). ETN is completely benign and will resolve spontaneously. Other choices: - Transient neonatal pustular melanosis is most common in African-American newborns, and the lesions lack the surrounding erythema typical of ETN. - Acne neonatorum is associated with closed comedones, mostly on the face. - As the infant described is not ill, infectious etiologies are unlikely. |
|
|
What are the recommendations to reduce the risk of sudden infant death syndrome (SIDS)?
|
Having the infant sleep in a separate bed
Having the infant sleep in a supine position (back to bed) also the risk of SIDS increases with higher room temperatures and soft bedding. |
|
|
A critically ill adult male is admitted to the intensive-care unit because of sepsis. He has no history of diabetes mellitus, but his glucose level on admission is 215 mg/dL and insulin therapy is ordered.
What is the target glucose range for this patient? |
140–180 mg/dL
The 2009 consensus guidelines on inpatient glycemic control issued by the American Association of Clinical Endocrinologists and the American Diabetes Association recommend insulin infusion with a target glucose level of 140–180 mg/dL in critically ill patients. This recommendation is based on clinical trials in critically ill patients. In the groups studied, there was no reduction in mortality from intensive treatment targeting near-euglycemic glucose levels compared to conventional management with a target glucose level of <180 mg/dL. There also were reports of harm resulting from intensive glycemic control, including higher rates of severe hypoglycemia and even increased mortality. |
|
|
Which one of the following is the recommended duration of dual antiplatelet therapy after placement of a drug-eluting coronary artery stent?
|
1 year
The recommended duration of dual antiplatelet therapy following placement of a drug-eluting coronary artery stent is 1 year (SOR C). The recommended dosages of dual antiplatelet therapy are aspirin, 162–325 mg, and clopidogrel, 75 mg, or prasugrel, 10 mg. Ticlopidine is an option for patients who do not tolerate clopidogrel or prasugrel. The minimum recommended duration of dual antiplatelet therapy is 1 month with bare-metal stents, 3 months with sirolimus-eluting stents, and 6 months with other drug-eluting stents. |
|
|
A 21-year-old primigravida at 28 weeks gestation complains of the recent onset of itching. On examination she has no obvious rash. The pruritus started on her palms and soles and spread to the rest of her body. Laboratory evaluation reveals elevated serum bile acids and mildly elevated bilirubin and liver enzymes.
The most effective treatment for this condition is: |
ursodiol (Actigall)
This patient’s symptoms and laboratory values are most consistent with intrahepatic cholestasis of pregnancy. Ursodiol has been shown to be highly effective in controlling the pruritus and decreased liver function (SOR A) and is safe for mother and fetus. Topical antipruritics and oral antihistamines are not very effective. Cholestyramine may be effective in mild or moderate intrahepatic cholestasis, but is less effective and safe than ursodiol. |
|
|
Which one of the following is an appropriate rationale for antibiotic treatment of Bordetella pertussis infections?
A. It delays progression from the catarrhal stage to the paroxysmal stage B. It reduces the severity of symptoms C. It reduces the duration of illness D. It reduces the risk of transmission to others E. It reduces the need for hospitalization |
It reduces the risk of transmission to others
Antibiotic treatment for pertussis is effective for eradicating bacterial infection but not for reducing the duration or severity of the disease. The eradication of infection is important for disease control because it reduces infectivity. Antibiotic treatment is thought to be most effective if started early in the course of the illness, characterized as the catarrhal phase. The paroxysmal stage follows the catarrhal phase. The CDC recommends macrolides for primary treatment of pertussis. The preferred antimicrobial regimen is azithromycin for 3–5 days or clarithromycin for 7 days. These regimens are as effective as longer therapy with erythromycin and have fewer side effects. Children under 1 month of age should be treated with azithromycin. There is an association between erythromycin and hypertrophic pyloric stenosis in young infants. Trimethoprim/sulfamethoxazole can be used in patients who are unable to take macrolides or where macrolide resistance may be an issue, but should not be used in children under the age of 2 months. Fluoroquinolones have been shown to reduce pertussis in vitro but have not been shown to be clinically effective (SOR A). |
|

A 16-year-old female cross-country runner has pain around both ankles. On examination, pain is elicited on foot inversion and there is decreased motion of the hind foot and peroneal tightness. A rigid flat foot also is observed.
What is the most likely diagnosis? |

Tarsal coalition
Tarsal coalition is the fusion of two or more tarsal bones. It occurs in mid-to late adolescence and is bilateral in 50% of those affected. Pain occurs around the ankle, and there is decreased range of motion of the hindfoot and pain on foot inversion on examination. Os trigonum results from non-ossification of cartilage. It usually is unilateral and causes palpable tenderness of the heel. Sever’s apophysitis is inflammation of the calcaneal apophysis, and causes pain in the heel. Plantar fasciitis causes tenderness over the anteromedial heel. Navicular stress fractures are tender over the dorsomedial navicular. |
|
|
Breast cancer screening - has it been shown to decrease mortality? to decrease more aggressive cancers? has it lead to more harm?
|
Breast cancer screening has resulted in an increase in the diagnosis of localized disease without a commensurate decrease in the incidence of more widespread disease.
Unfortunately, it cannot predict which of the discovered cancers are more aggressive, and cannot accurately detect premalignant lesions. The decrease in the mortality rate of breast cancer is due both to earlier detection and better follow-up medical care. JAMA 2009 |
|
|
You make a diagnosis of depression in a 26-year-old female. Her BMI is 32 kg/m² and she has been trying to lose weight. What antidepressants would be LEAST likely to cause her to gain weight?
|
Bupropion (Wellbutrin)
Bupropion is the antidepressant least likely to cause weight gain, and may induce modest weight loss. All of the other choices are more likely to cause weight gain. Among SSRIs, paroxetine is associated with the most weight gain and fluoxetine with the least. Mirtazapine has been associated with more weight gain than the SSRIs. |
|
|
Medicare pays for which preventative health care measures?
|
Medicare pays for some preventive measures, including pneumococcal vaccine, influenza vaccine, annual mammography, and a Papanicolaou test every 3 years. Medicare does not pay for custodial care, nursing-home care (except limited skilled nursing care), dentures, routine dental care, eyeglasses, hearing aids, routine physical checkups and related tests, or prescription drugs.
|
|
|
A 24-year-old female presents to your clinic with a 5-day history of fever to 103°F. She has no localizing symptoms or overt physical findings. Initial testing shows an elevated WBC count with a disproportionate number of reactive lymphocytes.
Dx? |
Viral infection
The presence of reactive lymphocytes will often be reported on a manual differential, since they have a distinctive appearance. The most common conditions that produce a reactive lymphocytosis are viral infections. Most notable are Epstein-Barr virus, infectious mononucleosis, and cytomegalovirus. Other viral infections known to cause this finding include herpes simplex, herpes zoster, HIV, hepatitis, and adenovirus. |
|
|
A 70-year-old male complains of lower-extremity pain. Increased pain with which motion would be most consistent with lumbar spinal stenosis?
|
Lumbar spine extension
Extension that increases lumbar lordosis decreases the cross-sectional area of the spinal canal, thereby compressing the spinal cord further. Walking downhill can cause this. Spinal flexion that decreases lordosis has the opposite effect, and will usually improve the pain, as will sitting. Pain with internal hip rotation is characteristic of hip arthritis and is often felt in the groin. Pain in the lateral hip is more typical of trochanteric bursitis. Increased pain walking uphill is more typical of vascular claudication. |
|
|
Notes on the use of short-acting inhaled β-agonists for asthma
|
Their effects begin within 5 minutes and last 4–6 hours
The effects of short-acting inhaled β-agonists begin within 5 minutes and last 4–6 hours. In the past, giving inhaled β-agonists just before inhaled corticosteroids was felt to improve the delivery and effectiveness of the corticosteroids. However, this has been proven to be ineffective and is no longer recommended. β-Blockers do diminish the effectiveness of inhaled β-agonists, but this effect is not severe enough to contraindicate using these drugs together. Oral β-agonists are less potent than inhaled forms. Similarly, anticholinergic drugs cause less bronchodilation than inhaled β-agonists and are not recommended as first-line therapy. |
|
|
In which patients are NSAIDs not appropriate?
|
They should be avoided in persons with cirrhotic liver disease
NSAIDs are prescribed commonly and many are available over the counter. It is important for clinicians to understand when they are not appropriate for clinical use. They should be avoided, if possible, in persons with hepatic cirrhosis (SOR C). While hepatotoxicity with NSAIDs is rare, they can increase the risk of bleeding in cirrhotic patients, as they further impair platelet function. In addition, NSAIDs decrease blood flow to the kidneys and can increase the risk of renal failure in patients with cirrhosis. NSAIDs differ from aspirin in terms of their cardiovascular effects. They have the potential to increase cardiovascular morbidity, worsen heart failure, increase blood pressure, and increase events such as ischemia and acute myocardial infarction. There are no known teratogenic effects of NSAIDs in humans. This drug class is considered to be safe in pregnancy in low, intermittent doses, although discontinuation of NSAID use within 6–8 weeks of term is recommended. Ibuprofen, indomethacin, and naproxen are considered safe for lactating women, according to the American Academy of Pediatrics. |
|
|
A 5-year-old female is seen for a kindergarten physical and is noted to be below the 3rd percentile for height. A review of her chart shows that her height curve has progressively fallen further below the 3rd percentile over the past year. She was previously at the 50th percentile for height. The physical examination is otherwise normal, but your workup shows that her bone age is delayed.
What is the most likely cause of her short stature? |
Growth hormone deficiency
This patient has delayed bone age coupled with a reduced growth velocity, which suggests an underlying systemic cause. Growth hormone deficiency is one possible cause for this. Although bone age can be delayed with constitutional growth delay, after 24 months of age growth curves are parallel to the 3rd percentile. Bone age would be normal with genetic short stature. Patients with Turner syndrome or skeletal dysplasia have dysmorphic features, and bone age would be normal. |
|
|
A 16-year-old female presents with a complaint of pelvic cramps with her menses over the past 2 years. She describes her periods as heavy, and says they occur once a month and last for 7 days, with no spotting in between. She has never been sexually active and does not expect this to change in the foreseeable future. An abdominal examination is normal. Which one of the following would be the most appropriate next step?
|
Naproxen prior to and during menses
(does not need pap smear) This patient is experiencing primary dysmenorrhea, a common finding in adolescents, with estimates of prevalence ranging from 20% to 90%. Because symptoms started at a rather young age and she has pain only during menses, endometriosis or other significant pelvic pathology is unlikely. An infection is doubtful, considering that she is not sexually active and that symptoms have been present for 2 years. In the absence of red flags, a pelvic examination, laboratory evaluation, and pelvic ultrasonography are not necessary at this time. However, they can be ordered if she does not respond to simple treatment. NSAIDs such as naproxen have a slight effect on platelet function, but because they inhibit prostaglandin synthesis they actually decrease the volume of menstrual flow and lessen the discomfort of pelvic cramping. Acetaminophen would have no effect on prostaglandins |
|
|
A 34-year-old female who delivered a healthy infant 18 months ago complains of a milky discharge from both nipples. She reports that normal periods have resumed since cessation of breastfeeding 6 months ago. She takes ethinyl estradiol/norgestimate (Ortho Tri-Cyclen) for birth control. A complete review of systems is otherwise negative. The most likely cause of the discharge is
|
a medication side effect
This patient has galactorrhea, which is defined as a milk-like discharge from the breast in the absence of pregnancy in a non-breastfeeding patient who is more than 6 months post partum. It is more common in women ages 20-35 and in women who are previously parous. It also can occur in men. Medication side effect is the most common etiology. The most common pharmacologic cause of galactorrhea is oral contraceptives. Oral contraceptives that contain estrogen can both suppress prolactin inhibitory factor and stimulate the pituitary directly, both of which can cause galactorrhea. Other medications that can cause galactorrhea include metoclopramide, cimetidine, risperidone, methyldopa, codeine, morphine, verapamil, SSRIs, butyrophenones, dopamine-receptor blockers, tricyclics, phenothiazines, and thioxanthenes. Breast cancer is unlikely to present with a bilateral milky discharge. The nipple discharge associated with cancer is usually unilateral and bloody. Pituitary tumors are a pathologic cause of galactorrhea due to the hyperprolactinemia that is caused by the blockage of dopamine from the hypothalamus, or by the direct production of prolactin. However, patients often have symptoms such as headache, visual disturbances, temperature intolerance, seizures, disordered appetite, polyuria, and polydipsia. Patients with prolactinomas often have associated amenorrhea. These tumors are associated with marked levels of serum prolactin, often >200 ng/mL. Hypothalamic lesions such as craniopharyngioma, primary hypothalamic tumor, metastatic tumor, histiocytosis X, tuberculosis, sarcoidosis, and empty sella syndrome are significant but infrequent causes of galactorrhea, and generally cause symptoms similar to those of pituitary tumors, particularly headache and visual disturbances. It is rare for primary hypothyroidism to cause galactorrhea in adults. Symptoms that would be a clue to this diagnosis include fatigue, constipation, menstrual irregularity, weight changes, and cold intolerance. |
|
|
The most common cause of abnormal vaginal discharge in a sexually active 19-year-old female is
A. Candida albicans B. Trichomonas vaginalis C. Staphylococcus D. Group B Streptococcus E. Bacterial vaginosis |
Bacterial vaginosis
Bacterial vaginosis (BV) is the most common cause of acute vaginitis, accounting for up to 50% of cases in some populations. It is usually caused by a shift in normal vaginal flora. BV is considerably more common as a cause of vaginal discharge than C. albicans and T. vaginalis. |
|
|
A 35-year-old female is planning a second pregnancy. Her last pregnancy was complicated by placental abruption caused by a large fibroid tumor of the uterus, which is still present. Which one of the following would be the most appropriate treatment for the fibroid tumor?
|
Myomectomy
There are numerous options for the treatment of uterine fibroids. When pregnancy is desired, myomectomy offers the best chance for a successful pregnancy when prior pregnancies have been marked by fibroid-related complications. Endometrial ablation eliminates fertility, and there is a lack of long-term data on fertility after uterine artery embolization. Observation without treatment would not remove the risk for recurrent complications during subsequent pregnancies. |
|
|
An asymptomatic 24-year-old white female comes to your office for a refill of oral contraceptive pills. A speculum examination is normal with the exception of a slightly friable, well-demarcated, 1.4-cm raised lesion involving a portion of the cervix. All previous Papanicolaou (Pap) tests have been normal and she has no history of abnormal bleeding or leukorrhea. What's the appropriate management of this patient?
|
A Pap test and a colposcopically-directed biopsy
The finding of a red, raised, friable lesion on the cervix, or a well-demarcated cervical lesion, mandates a biopsy to exclude cervical carcinoma, and treatment for chronic cervicitis should not be started until the biopsy results are available. A Papanicolaou test by itself is insufficient if there is a grossly visible lesion, as false-negatives occur in 10%-50% of tests. |
|
|
In patients with breast cancer, the most reliable predictor of survival is
|
stage (not grade)
The most reliable predictor of survival in breast cancer is the stage at the time of diagnosis. Tumor size and lymph node involvement are the main factors to take into account. Other prognostic parameters (tumor grade, histologic type, and lymphatic or blood vessel involvement) have been proposed as important variables, but most microscopic findings other than lymph node involvement correlate poorly with prognosis. Estrogen receptor (ER) status may also predict survival, with ER-positive tumors appearing to be less aggressive than ER-negative tumors. |
|
|
Which fetal ultrasound measurements gives the most accurate estimate of gestational age in the first trimester (up to 14 weeks)?
|
Crown-rump length
Because the growth pattern of the fetus varies throughout pregnancy, the accuracy of measurements and their usefulness in determining gestational age and growth vary with each trimester. Crown-rump length is the distance from the top of the head to the bottom of the fetal spine. It is most accurate as a measure of gestational age at 7-14 weeks. After that, other measurements are more reliable. In the second trimester, biparietal diameter and femur length are used. During the third trimester, biparietal diameter, abdominal circumference, and femur length are best for estimating gestational age. |
|
|
Late decelerations on fetal monitoring are thought to indicate :
|
Uteroplacental insufficiency
Late decelerations are thought to be associated with uteroplacental insufficiency and fetal hypoxia due to decreased blood flow in the placenta. This pattern is a warning sign and is associated with increasing fetal compromise, worsening fetal acidosis, fetal central nervous system depression, and/or direct myocardial hypoxia. Early decelerations are thought to result from vagus nerve response to fetal head compression, and are not associated with increased fetal mortality or morbidity. Variable decelerations are thought to be due to acute, intermittent compression of the umbilical cord between fetal parts and the contracting uterus. |
|
|
A 20-year-old female long-distance runner presents with a 3-month history of amenorrhea. A pregnancy test is negative, and other blood work is normal. She has no other medical problems and takes no medications. With respect to her amenorrhea, you advise her
|
to increase her caloric intake
Amenorrhea is an indicator of inadequate calorie intake, which may be related to either reduced food consumption or increased energy use. This is not a normal response to training, and may be the first indication of a potential developing problem. Young athletes may develop a combination of conditions, including eating disorders, amenorrhea, and osteoporosis (the female athlete triad). Amenorrhea usually responds to increased calorie intake or a decrease in exercise intensity. It is not necessary for patients such as this one to stop running entirely, however. |
|
|
A 2-year-old white male is brought to your office by his mother, who says he has “infected ant bites.” He was playing in his cousin’s yard yesterday in south Texas and cried when small brown ants crawled on his feet and legs. A physical examination is normal except for about 20 pustular-appearing lesions on erythematous bases on his lower extremities. The lesions are 1–2 mm in size. The most appropriate management of this problem is to:
|
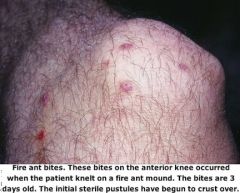
Recommend that the lesions be kept clean
The lesions described are typical of fire ant bites and are not infected. Fire ants are aggressive and these lesions do not imply abuse or neglect of the child. The lesions should be thoroughly cleaned with soap and water. Corticosteroids should be employed in severe cases, although their maximum effect is not achieved until several hours after administration. |
|

A diabetic patient has a deep 2×3-cm dorsal foot ulcer, and you are concerned about the presence of osteomyelitis. Which one of the following would be most cost-effective for evaluating this problem?
|
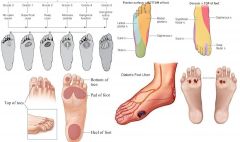
Probing for bone at the base of the ulcer
From CURRENT: Open wounds should be probed with a sterile cotton swab or other appropriate instrument to evaluate the extent of involvement of deeper structures, such as tendons, joints, and bone. A positive probe-to-bone test usually indicates the presence of osteomyelitis. AAFP: A recent study of foot ulcers in diabetics showed that finding palpable bone at the base of an ulcer with no intervening soft tissue had a higher positive predictive value than any type of imaging study, and correlated highly with the presence of underlying osteomyelitis. Other tests listed (MRI, CT scan, bone scan) are less likely to be diagnostic and are much more expensive than simple probing of a wound (NEJM 2000) |
|

A 6-month-old white male is brought to your office because he has “blisters” in his diaper area. You find large bullae filled with cloudy yellow fluid. Some of the blisters have ruptured and the bases are covered with a thin crust. What is the most appropriate management of this condition?
|
A course of a penicillinase-resistant penicillin or a cephalosporin
Bullous impetigo is a localized skin infection characterized by large bullae; it is caused by a group 2 phage type of Staphylococcus aureus. Cultures of fluid from an intact blister will reveal the causative agent. |
|

A 3-month-old infant is brought to your office with small pustules on the soles of the feet and a few similar lesions on the palms of her hands. Scabies is identified in scrapings of the lesions. Treatment?
|
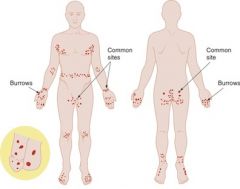
prescribe permethrin (Elimite) 5% cream to be applied to the entire body, including the scalp
Scabies is usually not seen on the head, neck, palms, and soles in adults, but these areas are often affected in infants. Lindane may be hazardous to young infants because of its percutaneous absorption and potential neurotoxicity. Permethrin is at least equally effective, and because it is poorly absorbed and rapidly metabolized, its toxicity is low. Crotamiton cream and sulphur in petrolatum are safe options, but must be applied continuously over 3–5 days. Laundering of clothing and bedclothes is sufficient to prevent reinfestation. In fact, clothes may simply be hung outside for 3–4 days, because the isolated mite dies within 2–3 days. |
|
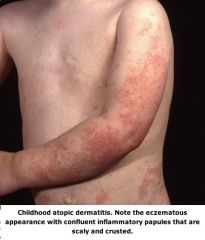
A 7-year-old male with moderately severe atopic dermatitis has been treated with a variety of moisturizers and topical corticosteroid preparations over the past year. The results have been less than satisfactory. Which topical medication is appropriate at this time?
|
Tacrolimus (Protopic)
Tacrolimus is an immunomodulator indicated for the treatment of atopic dermatitis when corticosteroids and other conventional remedies are inadvisable, ineffective, or not tolerated. It is approved for use in patients over 2 years of age. |
|

Cutaneous larva migrans is transmitted via:
[Picture: Cutaneous Larva Migrans. A serpiginous, linear, raise, tunnel-like erythematous lesion outlining the path of migration in the larva. Upon palpation, it feels like a thread within the superficial layers of the skin.] |

Skin contact with soil
Larva migrans is transmitted by skin contact with soil contaminated with hookworm larvae from dog and cat feces in tropical and subtropical areas. Wearing shoes and sitting on a towel rather than directly on the ground are protective measures. Ref: Kitchen LW: Case studies in international travelers. |
|
|
In the evaluation of foot ulcerations, a neuropathic etiology is suggested by which one of the following?
A. Distal foot pain when supine B. Absence of toe hair C. Erectile dysfunction D. Thickened toenails E. Abnormal monofilament testing |

Abnormal monofilament testing
Arterial insufficiency is suggested by a history of underlying cardiac or cerebrovascular disease, leg claudication, impotence, or pain in the distal foot when the patient is supine (the “rest pain” syndrome). Findings of diminished or absent pulses, pallor on elevation, redness of the foot on lowering of the leg (dependent rubor), sluggish refilling of toe capillaries, and thickened nails or absence of toe hair are consistent with impaired arterial perfusion to the foot. Measurement of cutaneous pressure perception with the use of Semmes-Weinstein monofilaments has been widely considered an ideal method of screening because of its simplicity, sensitivity, and low cost. (NEJM 2000) |
|

About a month after returning from the Middle East, an American soldier develops a papule on his forearm that subsequently ulcerates to form a shallow annular lesion with a raised margin. The lesion shows no signs of healing 3 months after it first appeared. He has no systemic symptoms. The most likely diagnosis is:
|
Leishmaniasis
|
|
|
A 35-year-old female volleyball coach consults you about a pruritic, vesicular eruption on the medial aspect of both feet, which she says has spread to her hands, causing a vesicular eruption resembling dyshidrosis. She is not using any drugs internally or topically. The most likely diagnosis is:
|

Tinea pedis
This presentation is typical of tinea pedis, with the associated dermatophytid reaction. Treatment of the fungal illness will usually control both conditions. |
|
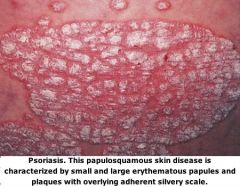
What would be considered first-line therapy for mild to moderately severe psoriasis confined to the elbows and knees?
A. Phototherapy using ultraviolet B light B. Methotrexate C. Etretinate (Tegison) D. Betamethasone dipropionate (Diprolene) |

Betamethasone dipropionate (Diprolene)
The majority of psoriasis patients can be managed with topical agents such as betamethasone dipropionate. Systemic treatment is reserved for patients with disabling psoriasis that does not respond to topical treatment. This would include phototherapy, methotrexate, and etretinate. |
|

What is the most effective initial treatment of head lice in an 8-year-old child?
|
Malathion (Ovide)
Malathion is currently the most effective treatment for head lice and is less toxic than lindane. Permethrin and pyrethrins are less effective than malathion, although they are acceptable alternatives. These insecticides, as well as lindane, are not recommended in children 2 years of age or younger. Wet combing may be effective, but is less than half as effective as malathion. Head shaving is only temporarily effective and is traumatic. Petrolatum is not proven to be effective. |
|

How is scabies transmitted?
|
The scabies mite is predominantly transmitted by direct personal contact. Infestation from indirect contact with clothing or bedding is believed to be infrequent. Hats are frequent transmitters of head lice, but not scabies.
|
|
|
You see a healthy 7-year-old male who was bitten on the cheek 1 hour ago by a neighbor’s dog. On examination you find a jagged laceration about 2 cm long that extends into the fatty tissue. What is the appropriate management of this injury?
|
Copiously irrigate the wound with normal saline and suture
Dog bites are a common medical problem. Timely and copious irrigation with normal saline or Ringer’s lactate will reduce the rate of infection markedly. Recent wounds and wounds on the face are usually closed primarily. Cultures are usually not helpful unless the wound appears infected. Amoxicillin/clavulanate is the antibiotic of choice for a dog bite. Since this is a neighbor’s dog, it can be observed at home for 10 days if the rabies vaccination is current, or at a veterinarian’s office if vaccination status is unknown. Ref: Presutti RJ: Prevention and treatment of dog bites. |
|
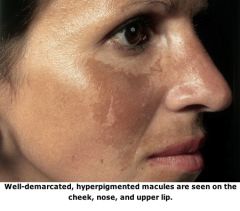
A 23-year-old Hispanic female at 18 weeks' gestation presents with a 4-week history of a new facial rash. She has noticed worsening with sun exposure. Her past medical history and review of systems is normal. On examination, you note symmetric, hyperpigmented patches on her cheeks and upper lip. The remainder of her examination is normal. The most likely diagnosis is:
|
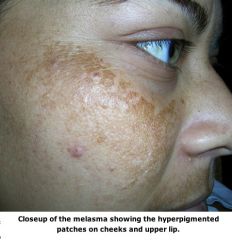
Melasma (chloasma)
Melasma or chloasma is common in pregnancy, with approximately 70% of pregnant women affected. It is an acquired hypermelanosis of the face, with symmetric distribution usually on the cheeks, nose, eyebrows, chin, and/or upper lip. The pathogenesis is not known. UV sunscreen is important, as sun exposure worsens the condition. Melasma often resolves or improves post partum. Persistent melasma can be treated with hydroquinone cream, retinoic acid, and/or chemical peels performed post partum by a dermatologist. The facial rash of lupus is usually more erythematous, and lupus is relatively rare. Pemphigoid gestationis is a rare autoimmune disease with extremely pruritic, bullous skin lesions that usually spare the face. Prurigo gestationis involves pruritic papules on the extensor surfaces and is usually associated with significant excoriation by the uncomfortable patient. |
|
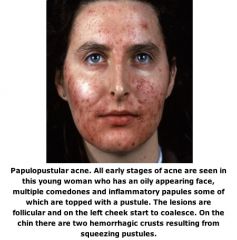
You see a 16-year-old white female for a preparticipation evaluation for sports, and she asks for advice about the treatment of acne. She has a few inflammatory papules on her face. No nodules are noted. She says she has not tried any over-the-counter acne treatments. Which one of the following would be considered first-line therapy for this condition?
|
Topical benzoyl peroxide
The American Academy of Dermatology grades acne as mild, moderate, and severe. Mild acne is limited to a few to several papules and pustules without any nodules. Patients with moderate acne have several to many papules and pustules with a few to several nodules. Patients with severe acne have many or extensive papules, pustules, and nodules. The patient has mild acne according to the American Academy of Dermatology classification scheme. Topical treatments including benzoyl peroxide, retinoids, and topical antibiotics are useful first-line agents in mild acne. Topical sulfacetamide is not considered first-line therapy for mild acne. Oral antibiotics are used in mild acne when there is inadequate response to topical agents and as first-line therapy in more severe acne. Caution must be used to avoid tetracycline in pregnant females. Oral isotretinoin is used in severe nodular acne, but also must be used with extreme caution in females who may become pregnant. Special registration is required by physicians who use isotretinoin, because of its teratogenicity |
|

The most appropriate initial treatment for scabies in an 8-year-old male is:
|
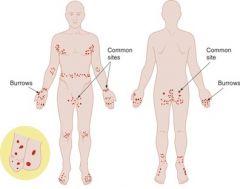
5% permethrin cream (Elimite)
In adults and children over 5 years of age, 5% permethrin cream is standard therapy for scabies. This agent is highly effective, minimally absorbed, and minimally toxic. |
|

Painful ingrown toenails that display granulation tissue and lateral nail fold hypertrophy are best treated by:
|
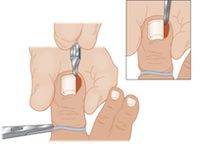
Excision of the lateral nail plate combined with lateral matricectomy
Excision of the lateral nail plate with lateral matricectomy yields the best results in the treatment of painful ingrown toenails that display granulation tissue and lateral nail fold hypertrophy. Antibiotic therapy and cotton-wick elevation are acceptable for very mildly inflamed ingrown toenails. Partial nail avulsion often leaves a spicule of nail that will grow and become an ingrown nail. Phenol produces irregular tissue destruction and significant inflammation and discharge after the matricectomy procedure. |
|
|
A 55-year-old white female presents with redness at the scar from a lumpectomy performed for stage I cancer of her right breast 4 months ago. The patient has completed radiation treatments to the breast. She is afebrile and there is no axillary adenopathy. There is no wound drainage, crepitance, or bullous lesions. Which one of the following organisms would be the most likely cause of cellulitis in this patient?
|
Non-group A Streptococcus
Cellulitis in patients after breast lumpectomy is thought to be related to lymphedema. Axillary dissection and radiation predispose to these infections. Non–group A hemolytic Streptococcus is the most common organism associated with this infection. The onset is often several weeks to several months after surgery. |
|

A 12-year-old male middle-school wrestler comes to your office complaining of a recurrent painful rash on his arm. There appear to be several dry vesicles. Most likely diagnosis?
|
Herpes gladiatorum
The most common infection transmitted person-to-person in wrestlers is herpes gladiatorum caused by the herpes simplex virus. Molluscum contagiosum causes keratinized plugs. Human papillomavirus causes warts. Tinea corporis is ringworm, which is manifested by round to oval raised areas with central clearing. |
|
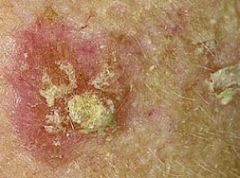
You are evaluating a 45-year-old male construction worker with regard to his skin and sun exposure history. Which one of the following lesions should be considered premalignant?
A. Sebaceous hyperplasia B. Actinic keratosis C. Seborrheic keratosis D. A de Morgan spot E. A halo nevus |
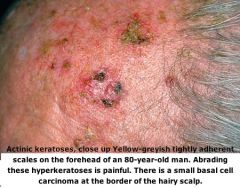
Actinic keratosis
Family physicians should advise patients of the dangers of sun exposure especially those with a fair complexion who work outdoors. Although malignant melanoma is the most serious condition of those listed, actinic keratosis may lead to squamous cell carcinoma with significant morbidity |
|
|
The preferred method for diagnosing psychogenic nonepileptic seizures is:
|
video-electroencephalography (vEEG) monitoring
Inpatient video-electroencephalography (vEEG) monitoring is the preferred test for the diagnosis of psychogenic nonepileptic seizures (PNES), and is considered the gold standard (SOR B). Video-EEG monitoring combines extended EEG monitoring with time-locked video acquisition that allows for analysis of clinical and electrographic features during a captured event. Many other types of evidence have been used, including the presence or absence of self-injury and incontinence, the ability to induce seizures by suggestion, psychologic tests, and ambulatory EEG. While useful in some cases, these alternatives have been found to be insufficient for the diagnosis of PNES. Elevated postictal prolactin levels (at least two times the upper limit of normal) have been used to differentiate generalized and complex partial seizures from PNES, but are not reliable (SOR B). While prolactin levels are often elevated after an epileptic seizure, they do not always rise, and the timing of measurement is crucial, making this a less sensitive test than was previously believed. Other serum markers have also been used to help distinguish PNES from epileptic seizures, including creatine phosphokinase, cortisol, WBC counts, lactate dehydrogenase, pCO2 , and neuron-specific enolase. These also are not reliable, as threshold levels for abnormality, sensitivity, and specificity have not been determined. MRI is not reliable because abnormal brain MRIs have been documented in as many as one-third of patients with PNES. In addition, patients with epileptic seizures often have normal brain MRIs. |
|

A 4-year-old white male is brought to your office because he has had a low-grade fever and decreased oral intake over the past few days. On examination you note shallow oral ulcerations confined to the posterior pharynx. Most likely diagnosis?
|
Herpangina
Herpangina is a febrile disease caused by coxsackieviruses and echoviruses. Vesicles and subsequent ulcers develop in the posterior pharyngeal area (SOR C). Herpes infection causes a gingivostomatitis that involves the anterior mouth. Mononucleosis may be associated with petechiae of the soft palate, but does not usually cause pharyngeal lesions. The exanthem in roseola usually coincides with defervescence. Mucosal involvement is not noted. Rubella may cause an enanthem of pinpoint petechiae involving the soft palate (Forschheimer spots), but not the pharynx. |
|

A 45-year-old female presents with a rash on the central portion of her face. She states that she has intermittent flushing and intense erythema that feels as if her face is stinging. She has noticed that her symptoms can be worsened by sun exposure, emotional stress, alcohol, or eating spicy foods. She has been in good health and has taken conjugated estrogens (Premarin), 0.625 mg daily, since a hysterectomy for benign reasons. A general examination is normal except for erythema of the cheeks and chin. No pustules or comedone formation is noted around her eyes, but telangiectasias are present.
Most appropriate management of this problem? |
Metronidazole gel (MetroGel)
Rosacea is a relatively common condition seen most often in women between the ages of 30 and 60. Central facial erythema and telangiectasias are prominent early features that may progress to a chronic infiltrate with papules and sometimes sterile pustules. Facial edema also may occur. Some patients develop rhinophyma due to hypertrophy of the subcutaneous glands of the nose. The usual presenting symptoms are central facial erythema and flushing that many patients find socially embarrassing. Flushing can be triggered by food, environmental, chemical, or emotional triggers. Ocular problems occur in half of patients with rosacea, often in the form of an intermittent inflammatory conjunctivitis with or without blepharitis. Management includes avoidance of precipitating factors and use of sunscreen. Oral metronidazole, doxycycline, or tetracycline also can be used, especially if there are ocular symptoms. These are often ineffective for the flushing, so low-dose clonidine or a nonselective β-blocker may be added. Topical treatments such as metronidazole and benzoyl peroxide may also be effective, particularly for mild cases. Other illnesses to consider include acne, photodermatitis, systemic lupus erythematosus, seborrheic dermatitis, carcinoid syndrome, and mastocytosis. |
|
|
Which one of the following confirmed findings in a 3-year-old female is diagnostic of sexual abuse?
A. Bacterial vaginosis B. Genital herpes C. Gonorrhea D. Anogenital warts E. Hepatitis |
Gonorrhea
The diagnosis of any sexually transmitted or associated infection in a postnatal prepubescent child should raise immediate suspicion of sexual abuse and prompt a thorough physical evaluation, detailed historical inquiry, and testing for other common sexually transmitted diseases. Gonorrhea, syphilis, and postnatally acquired Chlamydia or HIV are virtually diagnostic of sexual abuse, although it is possible for perinatal transmission of Chlamydia to result in infection that can go unnoticed for as long as 2–3 years. Although a diagnosis of genital herpes, genital warts, or hepatitis B should raise a strong suspicion of possible inappropriate contact and should be reported to the appropriate authorities, other forms of transmission are common. Genital warts or herpes may result from autoinoculation, and most cases of hepatitis B appear to be contracted from nonsexual household contact. Bacterial vaginosis provides only inconclusive evidence for sexual contact, and is the only one of the options listed for which reporting is neither required nor strongly recommended. |
|
|
A 63-year-old male with type 2 diabetes mellitus is seen in the emergency department for an acute, superficial, previously untreated infected great toe. Along with Staphylococcus aureus, which one of the following is the most common pathogen in this situation?
|
Streptococcus
The most common pathogens in previously untreated acute superficial foot infections in diabetic patients are aerobic gram-positive Staphylococcus aureus and β-hemolytic streptococci (groups A, B, and others). Previously treated and deep infections are often polymicrobial. |
|
|
An obese, hypertensive 53-year-old physician suffers a cardiac arrest while making rounds. He is resuscitated after 15 minutes of CPR, but remains comatose.
Which one of the following is associated with the lowest likelihood of neurologic recovery in this situation? A. Duration of CPR >10 minutes B. No pupillary light reflex at 30 minutes C. No corneal reflex at 2 hours D. No motor response to pain at 6 hours E. Myoclonic status epilepticus at 24 hours |
Myoclonic status epilepticus at 24 hours
It is difficult to establish a prognosis in a comatose patient after a cardiac arrest. The duration of CPR is not a factor, and the absence of pupillary and corneal reflexes, as well as motor responses to pain, are not reliable predictors before 72 hours. Myoclonic status epilepticus at 24 hours suggests no possibility of a recovery. |
|
|
A 61-year-old female is found to have a serum calcium level of 11.6 mg/dL (N 8.6–10.2) on routine laboratory screening. To confirm the hypercalcemia you order an ionized calcium level, which is 1.49 mmol/L (N 1.14–1.32). Additional testing reveals an intact parathyroid hormone level of 126 pg/mL (N 15–75) and a urine calcium excretion of 386 mg/24 hr (N 100–300).
What is the most likely cause of the patient’s hypercalcemia? |
Primary hyperparathyroidism
Primary hyperparathyroidism and malignancy account for more than 90% of hypercalcemia cases. These conditions must be differentiated early to provide the patient with optimal treatment and an accurate prognosis. Humoral hypercalcemia of malignancy implies a very limited life expectancy—often only a matter of weeks. On the other hand, primary hyperparathyroidism has a relatively benign course. Intact parathyroid hormone (PTH) will be suppressed in cases of malignancy-associated hypercalcemia, except for extremely rare cases of parathyroid carcinoma. Thyrotoxicosis-induced bone resorption elevates serum calcium, which also results in suppression of PTH. Patients with familial hypocalciuric hypercalcemia (FHH) have moderate hypercalcemia but relatively low urinary calcium excretion. PTH levels can be normal or only mildly elevated despite the hypercalcemia. This mild elevation can lead to an erroneous diagnosis of primary hyperparathyroidism. The conditions can be differentiated by a 24-hour urine collection for calcium; calcium levels will be high or normal in patients with hyperparathyroidism and low in patients with FHH. |
|
|
A 40-year-old male who recently immigrated from central Africa presents to a public health clinic where you are working. He was referred by a physician in the local emergency department, who made a diagnosis of type 2 diabetes mellitus. The patient has no history of fever or night sweats, weight loss, or cough. He does have a history of receiving bacille Calmette-Guérin (BCG) vaccine in the past. Screening tests for HIV and hepatitis performed in the emergency department were negative.
What do you know about screening for latent tuberculosis infection by in vitro interferon-gamma release assay (IGRA) compared to screening by the traditional targeted tuberculin skin test (TST) in this patient? |
IGRA differentiates Mycobacterium tuberculosis from nontuberculous mycobacteria
In vitro interferon-gamma release assays (IGRAs) are a new way of screening for latent tuberculosis infection. One of the advantages of IGRA is that it targets antigens specific to Mycobacterium tuberculosis. These proteins are absent from the BCG vaccine strains and from commonly encountered nontuberculous mycobacteria. Unlike skin testing, the results of IGRA are objective. It is unnecessary for IGRA to be done in tandem with skin testing, and it eliminates the need for two-step testing in high-risk patients. IGRAs are labor intensive, however, and the blood sample must be received by a qualified laboratory and incubated with the test antigens within 8-16 hours of the time it was drawn,depending upon the brand of cuurently available IGRAs |
|
|
An 11-year-old female has been diagnosed with "functional abdominal pain" by a pediatric gastroenterologist. Her mother brings her to see you because of concerns that another diagnosis may have been overlooked despite a very thorough and completely normal evaluation for organic causes.
What's the "next step" you would recommend? |
Stress reduction and participation in usual activities as much as possible
The diagnosis of functional abdominal pain is made when no structural, infectious, inflammatory, or biochemical cause for the pain can be found. It is the most common cause of recurrent abdominal pain in children 4–16 years of age. The use of medications may be helpful in reducing (but rarely eradicating) functional symptoms, and remaining open to the possibility of a previously unrecognized organic disorder is appropriate. However, continuing to focus on organic causes, invasive tests, or physician visits can actually perpetuate a child’s complaints and distress. It is estimated that approximately 30%–50% of children with functional abdominal pain will have resolution of their symptoms within 2 weeks of diagnosis. Recommendations for managing this problem include focusing on participation in normal age-appropriate activities, reducing stress and addressing emotional distress, and teaching the family to cope with the symptoms in a way that prevents secondary gain on the part of the child. |
|
|
Amiodarone (Cordarone) is most useful for which one of the following?
A. Prophylactic perioperative use for emergency surgery B. Primary prevention of nonischemic cardiomyopathy C. Treatment of atrial flutter D. Treatment of multi-focal premature ventricular contractions following acute myocardial infarction E. Treatment of sustained ventricular tachyarrhythmias in patients with poor hemodynamic stability |
Treatment of sustained ventricular tachyarrhythmias in patients with poor hemodynamic stability
Amiodarone is one of the most frequently prescribed antiarrhythmic medications in the U.S. It is useful in the acute management of sustained ventricular tachyarrhythmias, regardless of hemodynamic stability. Amiodarone is appropriate first-line treatment for atrial fibrillation only in symptomatic patients with left ventricular dysfunction and heart failure. It has a very limited role in the treatment of atrial flutter. The only role for prophylactic amiodarone is in the perioperative period of cardiac surgery. The use of prophylactic antiarrhythmic agents in the face of “warning dysrhythmias” or after myocardial infarction is no longer recommended. Prophylactic amiodarone is not indicated for primary prevention in patients with nonischemic cardiomyopathy. |
|
|
A 75-year-old white female presents with back pain of several months’ duration, which is worsened by movement. Her examination is unremarkable except for mild pallor. She takes furosemide (Lasix) for hypertension. Laboratory Findings Hemoglobin 10.0 g/dL (N 12.0–16.0) Serum creatinine 2.0 mg/dL (N 0.6–1.5) BUN 40 mg/dL (N 8–25) Serum uric acid 8.0 mg/dL (N 3.0–7.0) Serum calcium 12.0 mg/dL (N 8.5–10.5) Total serum protein 9.8 g/dL (N 6.0–8.4) Globulin 6.1 g/dL (N 2.3–3.5) Albumin 3.7 g/dL (N 3.5–5.0) Serum IgG 3700 mg/dL (N 639–1349) Urine positive for Bence-Jones protein Which one of the following would be most appropriate at this point?
|
Obtain a bone marrow examination
This patient has typical symptoms and laboratory findings of multiple myeloma, which accounts for 1% of all malignant diseases and has a mean age at diagnosis of 61 years. The diagnosis is confirmed by a bone marrow examination showing >10% plasma cells in the marrow. The serum level of M-protein is typically >3 g/dL. |
|
|
A 34-year-old white male letter carrier has developed progressively worsening dysphagia for liquids and solids over the past 3 months. He says that he has lost about 30 lb during that time. On examination, you note that he is emaciated and appears ill. His pulse rate is 98 beats/min, temperature 37.8° C (100.2° F), respiratory rate 24/min, and blood pressure 95/60 mm Hg. His weight is 45 kg (99 lb) and his height is 170 cm (67 in). His dentition is poor, and there is evidence of oral thrush. His mucous membranes are dry. You palpate small posterior cervical and axillary nodes. The heart, lung, and abdominal examinations are normal. You promptly consult a gastroenterologist, who performs upper endoscopy which reveals numerous small ulcers scattered throughout the esophagus with otherwise normal mucosa. As you continue to investigate, you take a more detailed history. Which one of the following findings is most likely to be related to the patient’s problem?
|
Intravenous drug use
A young man with weight loss, oral thrush, lymphadenopathy, and ulcerative esophagitis is likely to have HIV infection. Intravenous drug use is responsible for over a quarter of HIV infections in the United States. Esophageal disease develops in more than half of all patients with advanced infection during the course of their illness. The most common pathogens causing esophageal ulceration in HIV-positive patients include Candida, herpes simplex virus, and cytomegalovirus. Identifying the causative agent through culture or tissue sampling is important for providing prompt and specific therapy. |
|
|
The mother of a 5-day-old white male brings the infant to your office because of profuse bleeding from his circumcision site. A plastibell technique was used, and the bell is partially on. The mother reports that there was some scrotal bruising after the procedure. The remainder of the pre- and postnatal history is unremarkable. The infant appears healthy and vigorous. There is no heart murmur. Capillary refill is good. There is no bruising and no petechiae. Laboratory Findings Hematocrit 54% (N 41–65) Hemoglobin 18.0 g/dL (N 13.4–19.8) WBCs 14,000/mm3 (N 6000–17,500) Platelets 278,000/mm3 (N 150,000–400,000) Prothrombin time 12 sec (N 10–16) Activated partial pro- thrombin time 87 sec (N 31–54) Which one of the following additional tests will most likely help you to make the correct diagnosis?
|
Factor VIII level
Hemophilia is X-linked and occurs in approximately 1 in 5000 male births, with 85% having factor VIII deficiency (hemophilia A) and the remaining 15% having factor IX (hemophilia B) and factor XI (hemophilia C) deficiency. Because factor VIII does not cross the placenta, bleeding symptoms may be present from birth, with the most dreaded manifestation being intracranial hemorrhage. About 30% of affected male infants will bleed from the circumcision site. The only “routine” laboratory test that is affected by a reduced level of factor VIII is the activated partial thromboplastin time. Once hemophilia is suspected, the specific assay for factor VIII will confirm the diagnosis. Factor VIII levels in affected persons vary from less than 1% to approximately 25% of normal activity. Clinical severity of the disease varies with the degree of deficiency of factor VIII activity. Recently developed recombinant factor VIII for treating patients with hemophilia can help prevent transfusion-related infections. Deficiencies of antithrombin III, protein S and protein C, and mutations of the gene for factor V (factor V Leiden) are associated with thrombotic conditions, not bleeding. |
|
|
What intervention has proven most useful in preventing vertical transmission of HIV infection from mother to neonate?
|
Zidovudine (Retrovir) for both the mother and neonate
Antiretroviral treatment has been proven to reduce vertical transmission of HIV from mother to child. Benefits have been shown for antenatal, intrapartum, and postpartum treatments. Zidovudine and nevirapine have the most well-established track record. |
|
|
A 72-year-old female is found to have a complex splenic mass on a CT scan done for another reason. Because of concerns regarding possible malignancy and the potential for spontaneous splenic rupture, an elective splenectomy is planned. What immunizations should be given prior to her surgery?
|
Pneumococcal vaccine (Pneumovax)
Asplenic and functionally asplenic patients are susceptible to overwhelming infection from encapsulated organisms, and should be immunized with pneumococcal, meningococcal, and Hib vaccines. The vaccines’ immunogenicity may be reduced when given after splenectomy or during chemotherapy; thus, they should be given at least 2 weeks before performing elective splenectomy or starting chemotherapy if possible. |
|
|
Which vitamin deficiency is most likely in a child who is fed a strict vegetarian diet which excludes meat, eggs, and dairy products?
|
Vitamin B12
There is no known vegetable source for vitamin B12. If the diet contains milk and eggs, however, the requirement will be satisfied. Vitamin C is present in high concentrations in fruits and vegetables. Vitamin A is found in green, leafy vegetables. Thiamine is present in grains, especially the outer coatings. |
|
|
You regularly volunteer your professional services to a free clinic in an underserved community in a large U.S. city where various infectious diseases are prevalent. You are helping the staff develop some recommendations regarding infectious diseases that place infants at risk during breastfeeding. Which maternal infectious disease should be included as an ABSOLUTE contraindication to breastfeeding in otherwise healthy infants?
|
HIV infection
HIV and HTLV-1 (human T-cell lymphotropic virus) infections are the only infectious diseases that are considered absolute contraindications to breastfeeding in developed countries such as the U.S. The other infections listed may require temporary isolation of the baby from the mother, prophylactic treatment, or immunization of the baby and/or feeding pumped breast milk, but none are absolute contraindications to breastfeeding. For example, if the diagnosis of maternal hepatitis A is made within the period of contagiousness (approximately 3 weeks), careful handwashing by the mother is appropriate, and the infant can receive immunoglobulin and hepatitis A virus vaccine. Studies have shown that in full-term, healthy infants, acquisition of cytomegalovirus from breast milk does not result in significant clinical disease and is considered natural vaccination. Since breast milk does not contain tubercle bacilli, mothers with active tuberculosis may pump their milk to be bottle-fed to the infant by another person. For some common infections, such as the common cold, infants have already been exposed by maternal contact during the prodromal period, and interrupting breastfeeding would be counterproductive given that it provides the infant with antibodies and other anti-inflammatory and immunomodulating substances. |
|
|
What is the best initial screening test for hereditary hemochromatosis?
|
Serum transferrin saturation
The diagnosis of hereditary hemochromatosis is based on a combination of clinical, laboratory, and pathologic criteria. Serum transferrin saturation is the best initial screening value. Serum ferritin concentration is a sensitive measure of iron overload, but ferritin is an acute-phase reactant and is therefore elevated in a variety of infectious and inflammatory conditions in the absence of iron overload. |
|
|
A 40-year-old female is scheduled for a cholecystectomy and you wish to estimate her risk for postoperative bleeding. What is the most sensitive method for identifying her risk?
|
Bleeding history
Bleeding time, activated partial thromboplastin time (aPTT), and prothrombin time (PT) are relatively poor predictors of bleeding risk. Studies have shown that baseline coagulation assays do not predict postoperative bleeding in patients undergoing general or vascular surgery who have no history that suggests a bleeding disorder. Obtaining a history for evidence of prior bleeding problems is the most sensitive and accurate method of determining a patient’s risk. |
|
|
A 1-year-old infant is brought to your office for a well child visit. A screening CBC reveals her hemoglobin to be 10.5 g/dL (N 11.0–14.0) with a mean corpuscular volume of 69 µm3 (N 70–84). What is the most likely cause of her anemia?
|
Iron deficiency
This child has evidence of a mild microcytic anemia, which is most commonly caused by iron deficiency related to reduced dietary intake. Less common causes are thalassemia and lead poisoning. Hemolysis usually causes a normocytic anemia with an elevated reticulocyte count. Chronic liver disease and hypothyroidism result in macrocytic anemias. |
|
|
A 6-day-old white male is brought to your office with a 12-hour history of the sudden onset of vomiting and apparent abdominal pain. The emesis was initially clear, but over the last few hours it has become quite bilious. The pregnancy was uncomplicated and the child was delivered at term. On examination the child is lethargic with a tender abdomen, but no bowel distention. Of the following, which one is the most likely diagnosis?
A. Duodenal atresia B. Malrotation and midgut volvulus C. Pyloric stenosis D. Necrotizing enterocolitis E. Jejunoileal atresia |
Malrotation and midgut volvulus
Infants with malrotation and midgut volvulus often present in the first week of life with symptoms of bilious vomiting and bowel obstruction. Both duodenal and jejunoileal atresia most commonly present within the first 24 hours of life. Vomiting associated with pyloric stenosis is always non-bilious, and the diagnosis is most commonly made after the first week of life. Necrotizing enterocolitis may also be associated with bilious vomiting, but typically occurs at 10–12 days of life and is accompanied by abdominal distention and visible and/or palpable loops of bowel. |
|
|
A 65-year-old white female comes to your office with evidence of a fecal impaction which you successfully treat. She relates a history of chronic laxative use for most of her adult years. After proper preparation, you perform sigmoidoscopy and note that the anal and rectal mucosa contain scattered areas of bluish-black discoloration. What is the most likely explanation for the sigmoidoscopic findings?
|
Melanosis coli
This patient has typical findings of melanosis coli, the term used to describe black or brown discoloration of the mucosa of the colon. It results from the presence of dark pigment in large mononuclear cells or macrophages in the lamina propria of the mucosa. The coloration is usually most intense just inside the anal sphincter and is lighter higher up in the sigmoid colon. The condition is thought to result from fecal stasis and the use of anthracene cathartics such as cascara sagrada, senna, and danthron. |
|
|
What is the most common cause of bleeding in patients with Meckel’s diverticulum?
|
Ectopic (heterotrophic) gastric mucosa causing acid-induced bleeding of ileal mucosa
Most bleeding in Meckel’s diverticulum is secondary to heterotrophic gastric mucosa, causing acid-induced ileal ulceration. Helicobacter pylori has not been shown to be an etiologic agent. Intussusception is fairly common in patients with Meckel’s diverticulum but is not a frequent cause of bleeding. |
|
|
A 55-year-old white male smoker has had daily severe gastroesophageal reflux symptoms unrelieved by intensive medical therapy with proton pump inhibitors. A recent biopsy performed during upper endoscopy identified Barrett’s esophagus. What is true about this condition?
|
It is associated with an increased risk of adenocarcinoma
Barrett’s esophagus is an acquired intestinal metaplasia of the distal esophagus associated with longstanding gastroesophageal acid reflux, although a quarter of patients with Barrett’s esophagus have no reflux symptoms. It is more common in white and Hispanic men over 50 with longstanding severe reflux symptoms, and possible risk factors include obesity and tobacco use. It is a risk factor for adenocarcinoma of the esophagus, with a rate of about one case in every 200 patients with Barrett’s esophagus per year. Treatment is directed at reducing reflux, thus reducing symptoms. Neither medical nor surgical treatment has been shown to reduce the carcinoma risk. One reasonable screening suggestion is to perform esophagoduodenoscopy in all men over 50 with gastroesophageal reflux disease (GERD), but these recommendations are based only on expert opinion (level C evidence), and no outcomes-based guidelines are available. |
|
|
What animal has been shown to transmit Salmonella infections to humans?
|
Iguanas
Pet-associated salmonellosis was a significant problem in the 1970s. In 1975, Canada banned the importation of turtles, and in the same year the FDA prohibited the sale of small turtles in the U.S. However, the popularity of iguanas and other reptiles is increasing; these reptiles can also transmit Salmonella to humans. Reptile-associated salmonellosis causes febrile gastroenteritis, septicemia, and meningitis. |
|
|
What is the most common cause of bacterial diarrhea?
|
Campylobacter jejuni
|
|
|
A 25-year-old white male truck driver complains of 1 day of throbbing rectal pain. Your examination shows a large, thrombosed external hemorrhoid. What is the preferred initial treatment for this patient?
|
Elliptical excision of the thrombosed hemorrhoid
The appropriate management of a thrombosed hemorrhoid presenting within 48 hours of onset of symptoms is an elliptical excision of the hemorrhoid and overlying skin under local anesthesia (i.e., 0.5% bupivacaine hydrochloride [Marcaine] in 1:200,000 epinephrine) infiltrated slowly with a small (27 gauge) needle for patient comfort. Incision and clot removal may provide inadequate drainage with rehemorrhage and clot reaccumulation. Most thrombosed hemorrhoids contain multilocular clots which may not be accessible through a simple incision. Rubber band ligation is an excellent technique for management of internal hemorrhoids. Banding an external hemorrhoid would cause exquisite pain. When pain is already subsiding or more time has elapsed (in the absence of necrosis or ulceration), measures such as sitz baths, bulk laxatives, stool softeners, and local analgesia may all be helpful. Some local anesthetics carry the risk of sensitization, however counseling to avoid precipitating factors (e.g., prolonged standing/sitting, constipation, delay of defecation) is also appropriate. |
|
|
A positive spot urine test for homovanillic acid (HMA) and vanillylmandelic acid (VMA) is a marker for which condition?
|
Neuroblastoma
Tumor markers are useful in determining the diagnosis and sometimes the prognosis of certain tumors. They can aid in assessing response to therapy and detecting tumor recurrence. Serum neuron-specific enolase (NSE) testing, as well as spot urine testing for homovanillic acid (HVA) and vanillylmandelic acid (VMA), should be obtained if neuroblastoma or pheochromocytoma is suspected; both should be collected before surgical intervention. Quantitative beta-human chorionic gonadotropin (hCG) levels can be elevated in liver tumors and germ cells tumors. Alpha-fetoprotein is excreted by many malignant teratomas and by liver and germ cell tumors. |
|
|
A slender 22-year-old female is concerned about a recent weight loss of 10 lb, frequent mild abdominal pain, and significant diarrhea of 2 months’ duration. Her physical examination is unremarkable, and laboratory studies reveal only a moderate microcytic, hypochromic anemia. Based on this presentation, what is the most likely diagnosis?
|
Celiac disease
This constellation of symptoms strongly suggests celiac disease, a surprisingly common disease with a prevalence of 1:13 in the U.S. Half the adults in the U.S. with celiac disease or gluten-sensitive enteropathy present with anemia or osteoporosis, without gastrointestinal symptoms. Individuals with more significant mucosal involvement present with watery diarrhea, weight loss, and vitamin and mineral deficiencies. |
|
|
A 72-year-old male has had persistent interscapular pain with movement since rebuilding his deck 1 week ago. He rates the pain as 6 on a 10-point scale. A chest radiograph shows a thoracic vertebral compression fracture.
What's the appropriate next step? |
Markedly decreased activity until the pain lessens, and follow-up in 1 week
This patient has suffered a thoracic vertebral compression fracture. Most can be managed conservatively with decreased activity until the pain is tolerable, possibly followed by some bracing. Vertebroplasty is an option when the pain is not improved in 2 weeks. Complete bed rest is unnecessary and could lead to complications. Physical therapy is not indicated, and NSAIDs should be used with caution. |
|
|
On his first screening colonoscopy, a 67-year-old male is found to have a 0.5-cm adenomatous polyp with low-grade dysplasia.
According to current guidelines, when should this patient have his next colonoscopy? |
5 years
Overuse of colonoscopy has significant costs. In response to these concerns, the American Cancer Society and the U.S. Multi-Society Task Force on Colorectal Cancer collaborated on a consensus guideline on the use of surveillance colonoscopy. According to these guidelines, patients with one or two small (<1 cm) tubular adenomas, including those with only low-grade dysplasia, should have their next colonoscopy in 5–10 years (SOR B). |
|
|
A 25-year-old female has been trying to conceive for over 1 year without success. Her menstrual periods occur approximately six times per year. Laboratory evaluation of her hormone status has been negative, and her husband has a normal semen analysis. Her only other medical problem is hirsutism, which has not responded to topical treatment. Pelvic ultrasonography of her uterus and ovaries is unremarkable.
What would be the most appropriate treatment for her infertility? |
Metformin (Glucophage)
This patient fits the criteria for polycystic ovary syndrome (oligomenorrhea, acne, hirsutism, hyperandrogenism, infertility). Symptoms also include insulin resistance. Evidence of polycystic ovaries is not required for the diagnosis. Metformin has the most evidence supporting its use in this situation, and is the only treatment listed that is likely to decrease hirsutism and improve insulin resistance and menstrual irregularities. Metformin and clomiphene alone or in combination are first-line agents for ovulation induction. |
|
|
When treating acute adult asthma in the emergency department, using a metered-dose inhaler (MDI) with a spacer has been shown to result in what outcome measures, compared to use of a nebulizer?
|
Shorter stays in the emergency department
Compared to nebulizers, MDIs with spacers have been shown to lower pulse rates, provide greater improvement in peak-flow rates, lead to greater improvement in arterial blood gases, and decrease required albuterol doses. They have also been shown to lower costs, shorten emergency department stays, and significantly lower relapse rates at 2 and 3 weeks compared to nebulizers. There is no difference in hospital admission rates. |
|
|
A 31-year-old female who is a successful professional photographer complains of hoarseness that started suddenly 3 weeks ago. She says she can remember exactly what day it was, because her divorce became final the next day. The day the problem began, she was only able to whisper from the time she woke up, and she is able to speak only in a weak whisper while relating her history. She does not appear to strain while speaking. She does not smoke, has had no symptoms of an upper respiratory infection, and has no pain, cough, or wheezing.
She is on a proton pump inhibitor prescribed by an urgent care provider 2 weeks ago. This has not changed her symptoms. She takes no other medications and has no known allergies. A head and neck examination, including indirect laryngoscopy, is within normal limits. Which one of the following is the most likely diagnosis? A. Muscle tension aphonia B. Laryngopharyngeal reflux C. Spasmodic dysphonia D. Vocal abuse E. Conversion aphonia |
Conversion aphonia
This patient has conversion aphonia. In this condition, the patient loses his or her spoken voice, but the whispered voice is maintained. The vocal cords appear normal, but if observed closely by an otolaryngologist, there is a loss of vocal cord adduction during phonation, but normal adduction with coughing or throat clearing. This often occurs after a traumatic event (in this case a divorce) (SOR C). Muscle tension aphonia presents with strained, effortful phonation, vocal fatigue, and normal vocal cords. It is caused by excessive laryngeal or extralaryngeal tension associated with a variety of factors, including poor breath control and stress, for example. The patient with laryngopharyngeal reflux presents with a raspy or harsh voice. The hoarseness is usually worse early in the day and improves as the day goes by. There is usually associated heartburn, dysphagia, and/or throat clearing. The patient with spasmodic dysphonia (also known as laryngeal dystonia) has a halting, strangled vocal quality. It is a distinct neuromuscular disorder of unknown cause. Uncontrolled contractions of the laryngeal muscles cause focal laryngeal spasm. The hoarseness of vocal abuse is usually worse later in the day after effortful singing or talking. The history usually reveals vocal cord abuse, such as with an untrained singer or some other situation that increases demands on the voice. Nodules or cysts may be seen on the vocal cords with this condition. |
|
|
A 62-year-old diabetic with stage 2 renal dysfunction is evaluated for knee pain that has mildly interfered with his usual activities over the past 3 months. On examination he is mildly tender over the medial joint line. A knee radiograph shows moderate medial joint space narrowing.
In addition to low-impact exercise, which one of the following would you recommend initially? A. Intra-articular hyaluronic acid B. Intra-articular corticosteroids C. Celecoxib (Celebrex) D. Naproxen E. Acetaminophen |
Acetaminophen
Intra-articular injections should not be considered first-line treatment for symptomatic osteoarthritis of the knee. They are recommended for short-term pain control, with the evidence for hyaluronic acid being somewhat weak. Renal dysfunction is a contraindication to the use of NSAIDs. Acetaminophen is the first-line treatment in this case. |
|
|
A 24-year-old female presents with pelvic pain. She says that the pain is present on most days, but is worse during her menses. Ibuprofen has helped in the past but is no longer effective. Her menses are normal and she has only one sexual partner. A physical examination is normal.
What's the next step in the work-up of this patient? |
Transvaginal ultrasonography
The initial evaluation for chronic pelvic pain should include a urinalysis and culture, cervical swabs for gonorrhea and Chlamydia, a CBC, an erythrocyte sedimentation rate, a β-hCG level, and pelvic ultrasonography. CT and MRI are not part of the recommended initial diagnostic workup, but may be helpful in further assessing any abnormalities found on pelvic ultrasonography. Referral for diagnostic laparoscopy is appropriate if the initial workup does not reveal a source of the pain, or if endometriosis or adhesions are suspected. Colonoscopy would be indicated if the history or examination suggests a gastrointestinal source for the pain after the initial evaluation |
|
|
A 7-year-old male presents with a fever of 38.5°C (101.3°F), a sore throat, tonsillar inflammation, and tender anterior cervical adenopathy. He does not have a cough or a runny nose. His younger sister was treated for streptococcal pharyngitis last week and his mother would like him to be treated for streptococcal infection.
Is empiric antibiotic treatment for streptococcal pharyngitis is warranted? |
Yes
The patient has a score of 5 under the Modified Centor scoring system for management of sore throat. Patients with a score ≥4 are at highest risk (at least 50%) of having group A β-hemolytic streptococcal (GABHS) pharyngitis, and empiric treatment with antibiotics is warranted. Various national and international organizations disagree about the best way to manage pharyngitis, with no consensus as to when or how to test for GABHS and who should receive treatment. |
|
|
A 24-year-old female with a 2-year history of dyspnea on exertion has been diagnosed with exercise-induced asthma by another physician. Which one of the following findings on pulmonary function testing would raise concerns that she actually has vocal cord dysfunction?
|
Flattening of the inspiratory portion of the flow-volume loop, but a normal expiratory phase
The diagnosis of vocal cord dysfunction should be considered in patients diagnosed with exercise-induced asthma who do not have a good response to β-agonists before exercise. Pulmonary function testing with a flow-volume loop typically shows a normal expiratory portion but a flattened inspiratory phase (SOR C). A decreased FEV1 and normal FVC would be consistent with asthma. |
|
|
A 45-year-old female presents to your office with a 1-month history of pain and swelling posterior to the medial malleolus. She does not recall any injury, but reports that the pain is worse with weight bearing and with inversion of the foot. Plantar flexion against resistance elicits pain, and the patient is unable to perform a single-leg heel raise.
What's the appropriate next step in the management of this patient? |
Immobilization in a cast boot for 3 weeks is indicated
The diagnosis of tendinopathy of the posterior tibial tendon is important, in that the tendon’s function is to perform plantar flexion of the foot, invert the foot, and stabilize the medial longitudinal arch. An injury can, over time, elongate the midfoot and hindfoot ligaments, causing a painful flatfoot deformity. The patient usually recalls no trauma, although the injury may occur from twisting the foot by stepping in a hole. This is most commonly seen in women over the age of 40. Without proper treatment, progressive degeneration of the tendon can occur, ultimately leading to tendon rupture. Pain and swelling of the tendon is often noted, and is misdiagnosed as a medial ankle sprain. With the patient standing on tiptoe, the heel should deviate in a varus alignment, but this does not occur on the involved side. A single-leg toe raise should reproduce the pain, and if the process has progressed, this maneuver indicates progression of the problem. While treatment with acetaminophen or NSAIDs provides short-term pain relief, neither affects long-term outcome. Corticosteroid injection into the synovial sheath of the posterior tibial tendon is associated with a high rate of tendon rupture and is not recommended. The best initial treatment is immobilization in a cast boot or short leg cast for 2–3 weeks. |
|
|
A 70-year-old male presents to your office for a follow-up visit for hypertension. He was started on lisinopril (Prinivil, Zestril), 20 mg daily, 1 month ago. Laboratory tests from his last visit, including a CBC and a complete metabolic panel, were normal except for a serum creatinine level of 1.5 mg/dL (N 0.6–1.5). A follow-up renal panel obtained yesterday shows a creatinine level of 3.2 mg/dL and a BUN of 34 mg/dL (N 8–25).
Which one of the following is the most likely cause of this patient’s increased creatinine level? |
Bilateral renal artery stenosis
Classic clinical clues that suggest a diagnosis of renal-artery stenosis include the onset of stage 2 hypertension (blood pressure >160/100 mm Hg) after 50 years of age or in the absence of a family history of hypertension; hypertension associated with renal insufficiency, especially if renal function worsens after the administration of an agent that blocks the renin-angiotensin-aldosterone system; hypertension with repeated hospital admissions for heart failure; and drug-resistant hypertension (defined as blood pressure above the goal despite treatment with three drugs of different classes at optimal doses). |
|
|
A 58-year-old male presents with a several-day history of shortness of breath with exertion, along with pleuritic chest pain. His symptoms started soon after he returned from a vacation in South America. He has a history of deep-vein thrombosis (DVT) in his right leg after surgery several years ago, and also has a previous history of prostate cancer. You suspect pulmonary embolism (PE.).
Which one of the following is true regarding the evaluation of this patient? A. CT angiography would reliably either confirm or rule out PE B. Compression ultrasonography of the lower extremities will reveal a DVT in the majority of patients with PE C. No further testing is needed if a ventilation-perfusion lung scan shows a low probability of PE D. No further testing is needed if a D-dimer level is normal E. An elevated D-dimer level would confirm the diagnosis of PE |
CT angiography would reliably either confirm or rule out PE
This patient has a high clinical probability for pulmonary embolism (PE). About 40% of patients with PE will have positive findings for deep-vein thrombosis in the lower extremities on compression ultrasonography. A normal ventilation-perfusion lung scan rules out PE, but inconclusive findings are frequent and are not reassuring. A normal D-dimer level reliably rules out the diagnosis of venous thromboembolism in patients at low or moderate risk of pulmonary embolism, but the negative predictive value of this test is low for high-probability patients. A positive D-dimer test does not confirm the diagnosis; it indicates the need for further testing, and is thus not necessary for this patient. A multidetector CT angiogram or ventilation-perfusion lung scan should be the next test, as these are reliable to confirm or rule out PE. |
|
|
A 30-year-old white gravida 2 para 1 who has had no prenatal care presents for urgent care at 33 weeks gestation. Her symptoms include vaginal bleeding, uterine tenderness, uterine pain between contractions, and fetal distress. Her first pregnancy was uncomplicated, with a vaginal delivery at term.
Which one of the following is the most likely diagnosis? |
Placental abruption
Late pregnancy bleeding may cause fetal morbidity and/or mortality as a result of uteroplacental insufficiency and/or premature birth. The condition described here is placental abruption (separation of the placenta from the uterine wall before delivery). There are several causes of vaginal bleeding that can occur in late pregnancy that might have consequences for the mother, but not necessarily for the fetus, such as cervicitis, cervical polyps, or cervical cancer. Even advanced cervical cancer would be unlikely to cause the syndrome described here. The other conditions listed may bring harm to the fetus and/or the mother. Uterine rupture usually occurs during active labor in women with a history of a previous cesarean section or with other predisposing factors, such as trauma or obstructed labor. Vaginal bleeding is an unreliable sign of uterine rupture and is present in only about 10% of cases. Fetal distress or demise is the most reliable presenting clinical symptom. Vasa previa (the velamentous insertion of the umbilical cord into the membranes in the lower uterine segment) is typically manifested by the onset of hemorrhage at the time of amniotomy or by spontaneous rupture of the membranes. There are no prior maternal symptoms of distress. The hemorrhage is actually fetal blood, and exsanguination can occur rapidly. Placenta previa (placental implantation that overlies or is within 2 cm of the internal cervical os) is clinically manifested as vaginal bleeding in the late second or third trimester, often after sexual intercourse. The bleeding is typically painless, unless labor or placental abruption occurs. |
|
|
A 43-year-old female complains of a several-month history of unpleasant sensations in her legs and an urge to move her legs. These symptoms only occur at night and improve when she gets up and stretches. The sensations often awaken her, and she feels very tired. She has no other medical problems and takes no medication. Laboratory tests reveal a serum calcium level of 8.9 mg/dL (N 8.5–10.5), a serum potassium level of 4.1 mmol/L (N 3.5–5.0), a serum ferritin level of 15 ng/mL (N 10–200), and a serum magnesium level of 1.5 mEq/L (N 1.4–2.0).
What therapy may improve her symptoms? |
Iron supplementation
This patient has restless legs syndrome, which includes unpleasant sensations in the legs and can cause sleep disturbances. The symptoms are relieved by movement. Recommendations for treatment include lower-body resistance training and avoiding or changing medications that may exacerbate symptoms (e.g., antihistamines, caffeine, SSRIs, tricyclic antidepressants, etc.). It is also recommended that patients with a serum ferritin level below 50 ng/mL take an iron supplement (SOR C). Magnesium supplementation does not improve restless legs syndrome. Ropinirole may be used if nonpharmacologic therapies are ineffective. |
|
|
A 56-year-old female with well-controlled diabetes mellitus and hypertension presents with an 18-hour history of progressive left lower quadrant abdominal pain, low-grade fever, and nausea. She has not been able to tolerate oral intake over the last 6 hours. An abdominal examination reveals significant tenderness in the left lower quadrant with slight guarding but no rebound tenderness. Bowel sounds are hypoactive. Rectal and pelvic examinations are unremarkable.
Which one of the following is recommended as the initial diagnostic procedure in this situation? |
CT of the abdomen and pelvis
Based on the history and physical examination, this patient most likely has acute diverticulitis. CT has a very high sensitivity and specificity for this diagnosis, provides information on the extent and stage of the disease, and may suggest other diagnoses. Ultrasonography may be helpful in suggesting other diagnoses, but it is not as specific or as sensitive for diverticulitis as CT. Limited-contrast studies of the distal colon and rectum may occasionally be useful in distinguishing between diverticulitis and carcinoma, but would not be the initial procedure of choice. Water-soluble contrast material is used in this situation instead of barium. Colonoscopy to detect other diseases, such as cancer or inflammatory bowel disease, is deferred until the acute process has resolved, usually for 6 weeks. The risk of perforation or exacerbation of the disease is greater if colonoscopy is performed acutely. Diagnostic laparoscopy is rarely needed in this situation. Laparoscopic or open surgery to drain an abscess or resect diseased tissue is reserved for patients who do not respond to medical therapy. Elective sigmoid resection may be considered after recovery in cases of recurrent episodes. |
|
|
A 53-year-old male presents to your office with a several-day history of hiccups. They are not severe, but have been interrupting his sleep, and he is becoming exasperated.
What should be the primary focus of treatment in this individual? |
Finding the underlying pathology causing the hiccups
Hiccups are caused by a respiratory reflex that originates from the phrenic and vagus nerves, as well as the thoracic sympathetic chain. Hiccups that last a matter of hours are usually benign and self-limited, and may be caused by gastric distention. Treatments usually focus on interrupting the reflex loop of the hiccup, and can include mechanical means (e.g., stimulating the pharynx with a tongue depressor) or medical treatment, although only chlorpromazine is FDA-approved for this indication. If the hiccups have lasted more than a couple of days, and especially if they are waking the patient up at night, there may be an underlying pathology causing the hiccups. In one study, 66% of patients who experienced hiccups for longer than 2 days had an underlying physical cause. Identifying and treating the underlying disorder should be the focus of management for intractable hiccups. |
|
|
An 82-year-old male nursing-home resident is sent to the emergency department with lower abdominal pain and bloody diarrhea. He has a history of multi-infarct dementia, hypertension, and hyperlipidemia. On examination he is afebrile, and a nasogastric aspirate is negative for evidence of bleeding.
Which one of the following is the most likely cause of this patient’s bleeding? |
Ischemic colitis
This patient most likely has ischemic colitis, given the abdominal pain, bloody diarrhea, and cardiovascular risks. Peptic ulcer disease is unlikely because the nasogastric aspirate was negative. Diverticular bleeding and angiodysplasia are painless. Infectious colitis is associated with fever. |
|
|
A 62-year-old female undergoes elective surgery and is discharged on postoperative day 3. A week later she is hospitalized again with pneumonia. A CBC shows that her platelet count has dropped to 150,000/mm3 (N 150,000–300,000) from 350,000 /mm3 a week ago. She received prophylactic heparin postoperatively during her first hospitalization.
The patient is started on intravenous antibiotics for the pneumonia and subcutaneous heparin for deep-vein thrombosis prophylaxis. On hospital day 2, she has an acute onset of severe dyspnea and hypoxia; CT of the chest reveals bilateral pulmonary emboli. Her platelet count is now 80,000/mm3 . What is the appropriate next step? |
Discontinue heparin and start a non-heparin anticoagulant such as argatroban or desirudin (Iprivask)
This patient needs prompt evaluation and treatment for probable heparin-induced thrombocytopenia (HIT). HIT is a potentially life-threatening syndrome that usually occurs within 1–2 weeks of heparin administration and is characterized by the presence of HIT antibodies in the serum, associated with an otherwise unexplained 30%–50% decrease in the platelet count, arterial or venous thrombosis, anaphylactoid reactions immediately following heparin administration, or skin lesions at the site of heparin injections. Postoperative patients receiving subcutaneous unfractionated heparin prophylaxis are at highest risk for HIT. Because of this patient’s high-risk scenario and the presence of acute thrombosis, it is advisable to begin immediate empiric treatment for HIT pending laboratory confirmation. Management should include discontinuation of heparin and treatment with a non-heparin anticoagulant. |
|
|
A 64-year-old male presents with a 3-month history of difficulty sleeping. A history and physical examination, followed by appropriate ancillary testing, leads to a diagnosis of chronic primary insomnia.
Tx? |
Cognitive-behavioral therapy
Chronic insomnia is defined as difficulty with initiating or maintaining sleep, or experiencing nonrestorative sleep, for at least 1 month, leading to significant daytime impairment. Primary insomnia is not caused by another sleep disorder, underlying psychiatric or medical condition, or substance abuse disorder. Cognitive-behavioral therapy is effective for managing this problem, and should be used as the initial treatment for chronic insomnia. It has been shown to produce sustained improvement at both 12 and 24 months after treatment is begun. One effective therapy is stimulus control, in which patients are taught to eliminate distractions and associate the bedroom only with sleep and sex. Reading and television watching should occur in a room other than the bedroom. Pharmacotherapy alone does not lead to sustained benefits. SSRIs can cause insomnia, as can alcohol. |
|
|
What medication would be most appropriate for stroke prevention in a patient with hypertension, diabetes mellitus, and atrial fibrillation?
|
Warfarin (Coumadin)
The CHADS2 score is a validated clinical prediction rule for determining the risk of stroke and who should be anticoagulated. Points are assigned based on the patient’s comorbidities. One point is given for each of the following: history of congestive heart failure (C), hypertension (H), age ³75 (A), and diabetes mellitus (D). Two points are assigned for a previous stroke or TIA (S2 ). For patients with a score of 0 or 1, the risk of stroke is low and warfarin would not be recommended. Warfarin is the agent of choice for the prevention of stroke in patients with atrial fibrillation and a score ³2. In these patients, the risk of stroke is higher than the risks associated with taking warfarin. Enoxaparin is an expensive injectable anticoagulant and is not indicated for the long-term prevention of stroke. |
|
|
An elevation of serum methylmalonic acid is both sensitive and specific for a cellular deficiency of which vitamin?
|
Vitamin B 12
|
|
|
According to the guidelines of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, for hypertensive patients who also have diabetes mellitus, the blood pressure goal is below a threshold of:
|
130/80 mm Hg
Hypertension and diabetes mellitus are very common, both separately and in combination. End-organ damage to the heart, brain, and kidneys is more common in patients with both diabetes mellitus and hypertension, occurring at lower blood pressure levels than in patients with only hypertension. JNC 7, an evidence-based consensus report, recommends that patients with diabetes and hypertension be treated to reduce blood pressure to below 130/80 mm Hg, as opposed to 140/90 mm Hg for other adults. It should be noted, however, that the recently published ACCORD blood pressure trial found no significant cardiovascular benefit from targeting systolic blood pressure at <120 mm Hg rather than <140 mm Hg in patients with type 2 diabetes. This finding may affect the JNC 8 guidelines, which are currently being developed. |
|
|
A hospitalized patient is being treated with vancomycin for an infection due to methicillin-resistant Staphylococcus aureus (MRSA). What lab is most important to monitor?
|
Trough serum levels
The best predictor of vancomycin efficacy is the trough serum concentration, which should be over 10 mg/L to prevent development of bacterial resistance. Peak serum concentration is not a predictor of efficacy or toxicity. Monitoring for ototoxicity is not currently recommended. Older vancomycin products had impurities, which apparently caused the ototoxicity seen with these early formulations of the drug. |
|
|
A 35-year-old male amateur rugby player seeks your advice because right hip pain of several months’ duration has progressed to the point of interfering with his athletic performance. The pain is accentuated when he transitions from a seated to a standing position, and especially when he pivots on the hip while running, but he cannot recall any significant trauma to the area and finds no relief with over-the-counter analgesics. On examination his gait is stable. The affected hip appears normal and is neither tender to palpation nor excessively warm to touch. Although he has a full range of passive motion, obvious discomfort is evident with internal rotation of the flexed and adducted right hip.
What dx is most strongly suggested by this clinical picture? |
Impingement
Choices: Osteoarthritis, Avascular necrosis, Bursitis, Pathologic fracture Gradually worsening anterolateral hip joint pain that is sharply accentuated when pivoting laterally on the affected hip or moving from a seated to a standing position is consistent with femoroacetabular impingement. Reproduction of the pain on range-of-motion examination by manipulating the hip into a position of flexion, adduction, and internal rotation (FADIR test) is the most sensitive physical finding. Special radiographic imaging of the flexed and adducted hip can emphasize the anatomic abnormalities associated with impingement that may go unnoticed on standard radiographic series views. Although the pain associated with avascular necrosis is similarly insidious and heightened when bearing weight, tenderness is usually evident with hip motion in any direction. Osteoarthritis of the hip generally occurs in individuals of more advanced age than this patient, and the pain produced is typically localized to the groin area and can be elicited by flexion, abduction, and external rotation (FABER test) of the affected hip.Bursitis manifests as soreness after exercise and tenderness over the affected bursa. |
|
|
A 39-year-old African-American multigravida at 36 weeks gestation presents with a temperature of 40.0°C (104.0°F), chills, backache, and vomiting. On physical examination, the uterus is noted to be nontender, but there is slight bilateral costovertebral angle tenderness. A urinalysis reveals many leukocytes, some in clumps, as well as numerous bacteria.
The most appropriate therapy at this time would be: |
intravenous ceftriaxone (Rocephin)
Pyelonephritis is the most common medical complication of pregnancy. The diagnosis is usually straightforward, as in this case. Since the patient is quite ill, treatment is best undertaken in the hospital with parenteral agents, at least until the patient is stabilized and cultures are available. Ampicillin plus gentamicin or a cephalosporin is typically used. Sulfonamides are contraindicated late in pregnancy because they may increase the incidence of kernicterus. Tetracyclines are contraindicated because administration late in pregnancy may lead to discoloration of the child’s deciduous teeth. Nitrofurantoin may induce hemolysis in patients who are deficient in G-6-PD, which includes approximately 2% of African-American women. The safety of levofloxacin in pregnancy has not been established, and it should not be used unless the potential benefit outweighs the risk. |
|
|
A patient who takes fluoxetine (Prozac), 40 mg twice daily, develops shivering, tremors, and diarrhea after taking an over-the-counter cough and cold medication. On examination he has dilated pupils and a heart rate of 110 beats/min. His temperature is normal.
Which one of the following medications in combination with fluoxetine could contribute to this patient’s symptoms? A. Dextromethorphan (Robitussin, Vicks 44 Cough Relief) B. Pseudoephedrine (Sudafed, Dimetapp, Allegra-D, Claritin-D, Zyrtec-D) C. Phenylephrine (Vicks Sinex, Nasop, Mydfrin) D. Guaifenesin (Mucinex, Robitussin) E. Diphenhydramine (Benadryl) |
Dextromethorphan (Robitussin, Vicks 44 Cough Relief)
Dextromethorphan is commonly found in cough and cold remedies, and is associated with serotonin syndrome. SSRIs such as fluoxetine are also associated with serotonin syndrome, and there are many other medications that increase the risk for serotonin syndrome when combined with SSRIs. The other medications listed here are not associated with serotonin syndrome, however. |
|
|
Brain natriuretic peptide (BNP) is a marker for
|
Heart failure
Brain-type natriuretic peptide (BNP) is synthesized, stored, and released by the ventricular myocardium in response to volume expansion and pressure overload. It is a marker for heart failure. This hormone is highly accurate for identifying or excluding heart failure, as it has both high sensitivity and high specificity. BNP is particularly valuable in differentiating cardiac causes of dyspnea from pulmonary causes. In addition, the availability of a bedside assay makes BNP useful for evaluating patients in the emergency department. |
|
|
A 68-year-old female presents with a several-month history of weight loss, fatigue, decreased appetite, and vague abdominal pain. The most appropriate initial test to rule out adrenal insufficiency is:
|
morning serum cortisol
A single morning serum cortisol level >13µg/dL reliably excludes adrenal insufficiency. If the morning cortisol level is lower than this, further evaluation with a 1µg ACTH stimulation test is necessary, although the test is somewhat difficult. It requires dilution of the ACTH prior to administration, and requires multiple blood draws. The insulin tolerance test and metyrapone test, although historically considered to be “gold standards,” are not widely available or commonly used in clinical practice. MRI does not provide information about adrenal function. |
|
|
A healthy 48-year-old female consults you about continuing the use of her estrogen/progestin oral contraceptives. She has regular menstrual periods, is not hypertensive or diabetic, and does not smoke.
What advice would you give her? |
It is safe to continue the oral contraceptives
Healthy women may continue combination birth control pills into their fifties, and this patient has no contraindications. Screening for thrombophilic conditions is not indicated due to the low yield. FSH levels are not specific enough to evaluate the effect of stopping the contraceptive |
|
|
What finding is necessary to make a diagnosis of polymyalgia rheumatica?
|
Bilateral shoulder or hip stiffness and aching
There must be bilateral shoulder or hip stiffness and aching for at least one month in order to make the diagnosis of polymyalgia rheumatica. The erythrocyte sedimentation rate should be ≥40 mm/hr. |
|
|
The Centers for Disease Control and Prevention currently recommends that all patients between the ages of 13 and 64 years be screened for:
|
HIV infection
The focus of screening for HIV has been shifted from testing only high-risk individuals to routine testing of all individuals in health-care settings. There are an estimated 1.1 million people in the United States with HIV, and 25% are undiagnosed. Only 36.6% of adults have had an HIV test. Screening for hepatitis B and for tuberculosis is recommended only for certain at-risk populations. There is no generally used test for human papillomavirus. The CDC has not made any recommendations regarding screening for high cholesterol. |
|
|
A 71-year-old female with end-stage lung cancer was recently extubated and is awaiting transfer to hospice. She is awake and confused and has significant respiratory secretions.
Which medication used for reducing respiratory secretions is LEAST likely to cause central nervous system effects such as sedation? |
Glycopyrrolate (Robinul)
Glycopyrrolate does not cross the blood-brain barrier, and is therefore least likely to cause central nervous system effects such as sedation. The other medications listed [Atropine, Transdermal scopolamine (Transderm Scop), Hyoscyamine (Levsin)] do cross the blood-brain barrier. |
|
|
A 25-year-old female comes to your office requesting a referral to an otolaryngologist for surgery on her nose. She states that her nose is too large and that “something must be done.” She has already seen multiple family physicians, as well as several otolaryngologists. She is 168 cm (66 in) tall and weighs 64 kg (141 lb). A physical examination is normal, and even though she initially resists a nasal examination, it also is normal. The size of her nose is normal.
Which one of the following is the most likely cause of this patient’s concern about her nose? |
Body dysmorphic disorder
Body dysmorphic disorder is an increasingly recognized somatoform disorder that is clinically distinct from obsessive-compulsive disorder, eating disorders, and depression. Patients have a preoccupation with imagined defects in appearance, which causes emotional stress. Body dysmorphic disorder may coexist with anorexia nervosa, atypical depression, obsessive-compulsive disorder, and social anxiety. Cosmetic surgery is often sought. SSRIs and behavior modification may help, but cosmetic procedures are rarely helpful. |
|
|
A 78-year-old male presents for a routine follow-up visit for hypertension. He is a smoker, but has no known coronary artery disease and is otherwise healthy. On examination you note an irregular pulse. An EKG reveals multiple premature ventricular contractions (PVCs), but no other abnormalities.
Current guidelines recommend which one of the following? |
next step: Evaluation for underlying coronary artery disease
In patients with no known coronary artery disease (CAD), the presence of frequent premature ventricular contractions (PVCs) is linked to acute myocardial infarction and sudden death. The Framingham Heart Study defines frequent as >30 PVCs per hour. The American College of Cardiology and the American Heart Association recommend evaluation for CAD in patients who have frequent PVCs and cardiac risk factors, such as hypertension and smoking (SOR C). Evaluation for CAD may include stress testing, echocardiography, and ambulatory rhythm monitoring (SOR C). Strong evidence from randomized, controlled trials suggests that PVCs should not be suppressed with antiarrhythmic agents. The CAST I trial showed that using encainide or flecainide to suppress PVCs increases mortality (SOR A). |
|

While playing tennis, a 55-year-old male tripped and fell, landing on his outstretched hand with his elbow in slight flexion at impact. Pronation and supination of the forearm are painful on examination, as are attempts to flex the elbow. There is tenderness of the radial head without significant swelling. A radiograph of the elbow shows no fracture, but a positive fat pad sign is noted.
Appropriate management would include: |
a posterior splint and a repeat radiograph in 1–2 weeks
Nondisplaced radial head fractures can be treated by the primary care physician and do not require referral. Conservative therapy includes placing the elbow in a posterior splint for 5–7 days, followed by early mobilization and a sling for comfort. Sometimes the joint effusion may be aspirated for pain relief and to increase mobility. One study compared immediate mobilization with mobilization beginning in 5 days and found no differences at 1 and 3 months, but early mobilization was associated with better function and less pain 1 week after the injury. Radiographs should be repeated in 1–2 weeks to make sure that alignment is appropriate. |
|
|
Which hypoglycemic agent has been shown to reduce cardiovascular effects?
|
Metformin (Glucophage) reduces cardiovascular mortality rates
Metformin is the only hypoglycemic agent shown to reduce mortality rates in patients with type 2 diabetes mellitus. A recent systematic review concluded that cardiovascular events are neither increased nor decreased with the use of sulfonylureas. The effect of incretin mimetics and incretin enhancers on cardiovascular events has not been determined. The STOP-NIDDM study suggests that α-glucosidase inhibitors reduce the risk of cardiovascular events in patients with impaired glucose tolerance. (JAMA 2003) |
|
|
A 46-year-old female presents to your office for follow-up of elevated blood pressure on a pre-employment examination. She is asymptomatic, and her physical examination is normal with the exception of a blood pressure of 160/100 mm Hg. Screening blood work reveals a potassium level of 3.1 mEq/L (N 3.7–5.2). You consider screening for primary hyperaldosteronism with which test?
|
A serum aldosterone-to-renin ratio
Primary hyperaldosteronism is relatively common in patients with stage 2 hypertension (160/100 mm Hg or higher) or treatment-resistant hypertension. It has been estimated that 20% of patients referred to a hypertension specialist suffer from this condition. Experts recommend screening for this condition using a ratio of morning plasma aldosterone to plasma renin. A ratio >20:1 with an aldosterone level >15 ng/dL suggests the diagnosis. The level of these two values is affected by several factors, including medications (especially most blood pressure medicines), time of day, position of the patient, and age. Patients who are identified as possibly having this condition should be referred to an endocrinologist for further confirmatory testing. |
|
|
A 45-year-old male presents with a 4-month history of low back pain that he says is not alleviated with either ibuprofen or acetaminophen. On examination he has no evidence of weakness or focal tenderness. Laboratory studies, including a CBC, erythrocyte sedimentation rate, C-reactive protein, and complete metabolic profile, are all normal. MRI of the lumbosacral region shows mild bulging of the L4-L5 disc without impingement on the thecal sac.
What intervention has been shown to be beneficial in this situation? |
Acupuncture
Most chronic back pain (up to 70%) is nonspecific or idiopathic in origin. Treatment options that have the best evidence for effectiveness include analgesics (acetaminophen, tramadol, NSAIDs), multidisciplinary rehabilitation, and acupuncture (all SOR A). Other treatments likely to be beneficial include herbal medications, tricyclics, antidepressants, exercise therapy, behavior therapy, massage, spinal therapy, opioids, and short-term muscle relaxants (all SOR B). There is conflicting data regarding the effectiveness of back school, low-level laser therapy, lumbar supports, viniyoga, antiepileptic medications, prolotherapy, short-wave diathermy, traction, transcutaneous electrical nerve stimulation, ultrasound, and epidural corticosteroid injections (all SOR C). |
|
|
A 45-year-old white female with elevated cholesterol and coronary artery disease comes in for a periodic fasting lipid panel and liver enzyme levels. She began statin therapy about 2 months ago and reports no problems. Laboratory testing reveals an LDL-cholesterol level of 70 mg/dL, an HDL-cholesterol level of 55 mg/dL, an alanine aminotransferase (ALT) level of 69 U/L (N 7–30), and an aspartate aminotransferase (AST) level of 60 U/L (N 9–25).
Which one of the following would be most appropriate at this time? |
Continue the current therapy with routine monitoring
The patient is at her LDL and HDL goals and has no complaints, so she should be continued on her current regimen with routine monitoring (SOR C). Research has proven that up to a threefold increase above the upper limit of normal in liver enzymes is acceptable for patients on statins. Too often, slight elevations in liver enzymes lead to unnecessary dosage decreases, discontinuation of statin therapy, or additional testing. Ref: Onusko E: Statins and elevated liver tests: What’s the fuss? J Fam Pract 2008;57(7):449-452. |
|
|
In a patient with chronic hepatitis B, which lab finding would suggest that the infection is in the active phase?
|
Elevated levels of ALT
Chronic hepatitis B develops in a small percentage of adults who fail to recover from an acute infection, in almost all infants infected at birth, and in up to 50% of children infected between the ages of 1 and 5 years. Chronic hepatitis B has three major phases: immune-tolerant, immune-active, and inactive-carrier.There usually is a linear transition from one phase to the next, but reactivation from immune-carrier phase to immune-active phase also can be seen. Active viral replication occurs during the immune-tolerant phase when there is little or no evidence of disease activity, and this can last for many years before progressing to the immune-active phase (evidenced by elevated liver enzymes, indicating liver inflammation, and the presence of HBeAg, indicating high levels of HBV DNA). Most patients with chronic hepatitis B eventually transition to the inactive-carrier phase, which is characterized by the clearance of HBeAg and the development of anti-HBeAg, accompanied by normalization of liver enzymes and greatly reduced levels of hepatitis B virus in the bloodstream. |
|
|
A 42-year-old male presents with anterior neck pain. His thyroid gland is markedly tender on examination, but there is no overlying erythema. He also has a bilateral hand tremor. His erythrocyte sedimentation rate is 82 mm/hr (N 1–13) and his WBC count is 11,500/mm3 (N 4300–10,800). His free T4 is elevated, TSH is suppressed, and radioactive iodine uptake is abnormally low.
Which treatment option would be most helpful at this time? |
Prednisone
This patient has signs and symptoms of painful subacute thyroiditis, including a painful thyroid gland, hyperthyroidism, and an elevated erythrocyte sedimentation rate. It is unclear whether there is a viral etiology to this self-limited disorder. Thyroid function returns to normal in most patients after several weeks, and may be followed by a temporary hypothyroid state. Treatment is symptomatic. Although NSAIDs can be helpful for mild pain, high-dose glucocorticoids provide quicker relief for the more severe symptoms. Levothyroxine is not indicated in this hyperthyroid state. Neither thyroidectomy nor antibiotics is indicated for this problem. |
|
|
A 60-year-old female with moderate COPD presents with ongoing dyspnea in spite of treatment with both an inhaled long-acting β-agonist and a long-acting anticholinergic agent. Your evaluation reveals an oxygen saturation of 88% and a PaO2 of 55%. Echocardiography reveals a normal ejection fraction but moderate pulmonary hypertension.
What would be the most appropriate at this time? |
Supplemental oxygen
This patient with moderate COPD and moderate nonpulmonary arterial hypertension pulmonary hypertension is hypoxic and meets the criteria for use of supplemental oxygen (SOR A). Sildenafil and nifedipine are utilized in pulmonary arterial hypertension, but evidence is lacking for their use in pulmonary hypertension associated with chronic lung disease and/or hypoxemia. Low-dose prednisone may be a future option. |
|
|
A 48-year-old female with type 2 diabetes has been hospitalized for 4 days with persistent fever. Her diabetes has been controlled with diet and glyburide (Micronase, DiaBeta). You saw her 2 weeks ago in the office with urinary frequency, urgency, and dysuria. At that time a urinalysis showed 25 WBCs/hpf, and a urine culture subsequently grew Escherichia coli sensitive to all antibiotics. She was placed on trimethoprim/sulfamethoxazole (Bactrim, Septra) empirically, and this was continued after the culture results were reported.
She improved over the next week, but then developed flank pain, fever to 39.5°C (103.1°F), and nausea and vomiting. She was hospitalized and intravenous cefazolin (Kefzol) and gentamicin were started while blood and urine cultures were performed. This urine culture also grew E. coli sensitive to the current antibiotics. Her temperature has continued to spike to 39.5°C since admission, without any change in her symptoms. What would be most appropriate at this time? |
Order CT of the abdomen
Perinephric abscess is an elusive diagnostic problem that is defined as a collection of pus in the tissue surrounding the kidney, generally in the space enclosed by Gerota’s fascia. Mortality rates as high as 50% have been reported, usually from failure to diagnose the problem in a timely fashion. The difficulty in making the diagnosis can be attributed to the variable constellation of symptoms and the sometimes indolent course of this disease. The diagnosis should be considered when a patient has fever and persistence of flank pain. Most perinephric infections occur as an extension of an ascending urinary tract infection, commonly in association with renal calculi or urinary tract obstruction. Patients with anatomic urinary tract abnormalities or diabetes mellitus have an increased risk. Clinical features may be quite variable, and the most useful predictive factor in distinguishing uncomplicated pyelonephritis from perinephric abscess is persistence of fever for more than 4 days after initiation of antibiotic therapy. The radiologic study of choice is CT. This can detect perirenal fluid, enlargement of the psoas muscle (both are highly suggestive of the diagnosis), and perirenal gas (which is diagnostic). The sensitivity and specificity of CT is significantly greater than that of either ultrasonography or intravenous pyelography. Drainage, either percutaneously or surgically, along with appropriate antibiotic coverage reduces both morbidity and mortality from this condition. |
|
|
A 72-year-old female sees you for preoperative evaluation prior to cataract surgery. Her history and physical examination are unremarkable, and she has no medical problems other than bilateral cataracts.
Which test is recommended prior to surgery in this patient? |
No testing
According to a recent Cochrane review, routine preoperative testing prior to cataract surgery does not decrease intraoperative or postoperative complications (SOR A). The American Heart Association recommends against routine preoperative testing in asymptomatic patients undergoing low-risk procedures, since the cardiac risk associated with such procedures is less than 1%. Routine preoperative medical testing for cataract surgery. Cochrane Database Syst Rev 2009 |
|
|
You see a 9-year-old female for evaluation of her asthma. She and her mother report that she has shortness of breath and wheezing 3–4 times per week, which improves with use of her albuterol inhaler. She does not awaken at night due to symptoms, and as long as she has her albuterol inhaler with her she does not feel her activities are limited by her symptoms. About once per year she requires prednisone for an exacerbation, often triggered by a viral infection.
Based on this information you classify her asthma severity as: |
mild persistent
The 2007 update to the guidelines for the diagnosis and management of asthma published by the National Heart, Lung, and Blood Institute outlines clear definitions of asthma severity. Severity is determined by the most severe category in which any feature occurs. This patient has mild persistent asthma, based on her symptoms occurring more than 2 days per week, but not daily, and use of her albuterol inhaler more than 2 days per week, but not daily. Clinicians can use this assessment to help guide therapy. |
|
|
What s/s is found most consistently in patients diagnosed with irritable bowel syndrome?
|
Abdominal pain
A large review of multiple studies identified abdominal pain as the most consistent feature found in irritable bowel syndrome (IBS), and its absence makes the diagnosis less likely. Of the symptoms listed, passage of blood is least likely with IBS, and passage of mucus, constipation, and diarrhea are less consistent than abdominal pain (SOR A). |
|
|
What is diagnostic for type 2 diabetes mellitus?
|
A fasting plasma glucose level ≥126 mg/dL on two separate occasions
The American Diabetes Association (ADA) first published guidelines for the diagnosis of diabetes mellitus in 1997 and updated its diagnostic criteria in 2010. With the increasing incidence of obesity, it is estimated that over 5 million Americans have undiagnosed type 2 diabetes mellitus. Given the long-term risks of microvascular (renal, ocular) and macrovascular (cardiac) complications, clear guidelines for screening are critical. The ADA recommends screening for all asymptomatic adults with a BMI >25.0 kg/m whohave one or more additional risk factors for diabetes mellitus, and screening for all adults with no risk factors every 3 years beginning at age 45. Current criteria for the diagnosis of diabetes mellitus include a hemoglobin A 1c ³6.5%, a fasting plasma glucose level ³126 mg/dL, a 2-hour plasma glucose level ³200 mg/dL, or, in a symptomatic patient, a random blood glucose level ³200 mg/dL. In the absence of unequivocal hyperglycemia, results require confirmation by repeat testing. |
|
|
A 62-year-old male is admitted to the hospital for urosepsis. His medical history is significant only for hypertension. On examination he has a temperature of 36.5°C (97.7°F), a TSH level of 0.2 μU/mL (N 0.4–5.0), and a free T4 level of 0.4 ng/dL (N 0.6–1.5). Most likely dx?
|
Euthyroid sick syndrome
The euthyroid sick syndrome refers to alterations in thyroid function tests seen frequently in hospitalized patients, and decreased thyroid function tests may be seen early in sepsis. These changes are statistically much more likely to be secondary to the euthyroid sick syndrome than to unrecognized pituitary or hypothalamic disease (SOR C). Graves’ disease generally is a hyperthyroid condition associated with low TSH and elevated free T4 . Subclinical hypothyroidism is diagnosed by high TSH and normal free T4 levels. Subacute thyroiditis most often is a hyperthyroid condition. |
|
|
An 8-year-old female is brought to your office because she has begun to limp. She has had a fever of 38.8°C (101.8°F) and says that it hurts to bear weight on her right leg. She has no history of trauma.
On examination, she walks with an antalgic gait and hesitates to bear weight on the leg. Range of motion of the right hip is limited in all directions and is painful. Her sacroiliac joint is not tender, and the psoas sign is negative. Laboratory testing reveals an erythrocyte sedimentation rate of 55 mm/hr (N 0–10), a WBC count of 15,500/mm 3 (N 4500–13,500), and a C-reactive protein level of 2.5 mg/dL (N 0.5–1.0). What test would provide the most useful diagnostic information to further evaluate this patient’s problem? |
Ultrasonography (not MRI or XRAY)
This child meets the criteria for possible septic arthritis. In this case ultrasonography is recommended over other imaging procedures. It is highly sensitive for detecting effusion of the hip joint. If an effusion is present, urgent ultrasound-guided aspiration should be performed. Bone scintigraphy is excellent for evaluating a limping child when the history, physical examination, and radiographic and sonographic findings fail to localize the pathology. CT is indicated when cortical bone must be visualized. MRI provides excellent visualization of joints, soft tissues, cartilage, and medullary bone. It is especially useful for confirming osteomyelitis, delineating the extent of malignancies, identifying stress fractures, and diagnosing early Legg-Calvé-Perthes disease. Plain film radiography is often obtained as an initial imaging modality in any child with a limp. However, films may be normal in patients with septic arthritis, providing a false-negative result. |
|
|
A 17-year-old female sees you for a preparticipation evaluation. She has run 5 miles a day for the last 6 months, and has lost 6 lb over the past 2 months. Her last menstrual period was 3 months ago. Other than the fact that she appears to be slightly underweight, her examination is normal.
To fit the criteria for the female athlete triad, she must have which finding? |
A history of a stress fracture resulting from minimal trauma
The initial definition of the female athlete triad was amenorrhea, osteoporosis, and disordered eating. The American College of Sports Medicine modified this in 2007, emphasizing that the triad components occur on a continuum rather than as individual pathologic conditions. The definitions have therefore expanded. Disordered eating is no longer defined as the formal diagnosis of an eating disorder. Energy availability,defined as dietary energy intake minus exercise energy expenditures, is now considered a risk factor for the triad, as dietary restrictions and substantial energy expenditures disrupt pituitary and ovarian function. Primary amenorrhea is defined as lack of menstruation by age 15 in females with secondary sex characteristics. Secondary amenorrhea is the absence of three or more menstrual cycles in a young woman previously experiencing menses. For those with secondary amenorrhea, a pregnancy test should be performed. If this is not conclusive, a progesterone challenge test may be performed. If there is withdrawal bleeding, the cause would be anovulation. Those who do not experience withdrawal bleeding have hypothalamic amenorrhea, and fit one criterion for the triad. Athletes who have amenorrhea for 6 months, disordered eating, and/or a history of a stress fracture resulting from minimal trauma should have a bone density test. Low bone mineral density for age is the term used to describe at-risk female athletes with a Z-score of –1 to –2. Osteoporosis is defined as having clinical risk factors for experiencing a fracture, along with a Z-score <–2. |
|
|
Which bug is the most common cause of recurrent and persistent acute otitis media in children?
|
Penicillin-resistant Streptococcus pneumoniae
Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis are the most common bacterial isolates from the middle ear fluid of children with acute otitis media. Penicillin-resistant S. pneumoniae is the most common cause of recurrent and persistent acute otitis media. |
|
|
A 65-year-old asymptomatic female is found to have extensive sigmoid diverticulosis on screening colonoscopy. She asks whether there are any dietary changes she should make.
In addition to increasing fiber intake, what else would you recommend? |
No limitations on other intake
Patients with diverticulosis should increase dietary fiber intake or take fiber supplements to reduce progression of the diverticular disease. Avoidance of nuts, corn, popcorn, and small seeds has not been shown to prevent complications of diverticular disease. |
|
|
What should be used first for ventricular fibrillation when an initial defibrillation attempt fails?
|
Vasopressin (Pitressin)
For persistent ventricular fibrillation (VF), in addition to electrical defibrillation and CPR, patients should be given a vasopressor, which can be either epinephrine or vasopressin. Vasopressin may be substituted for the first or second dose of epinephrine. Amiodarone should be considered for treatment of VF unresponsive to shock delivery, CPR, and a vasopressor. Lidocaine is an alternative antiarrhythmic agent, but should be used only when amiodarone is not available. Magnesium may terminate or prevent torsades de pointes in patients who have a prolonged QT interval during normal sinus rhythm. Adenosine is used for the treatment of narrow complex, regular tachycardias and is not used in the treatment of ventricular fibrillation. |
|
|
What is the best test for confirming the diagnosis of renal colic?
|
CT
CT is the gold standard for the diagnosis of renal colic. Its sensitivity and specificity are superior to those of ultrasonography and intravenous pyelography. Noncalcium stones may be missed by plain radiography but visualized by CT. MRI is a poor tool for visualizing stones. |
|
|
A 50-year-old male has a pre-employment chest radiograph showing a pulmonary nodule. There are no previous studies available.
Which radiographic finding would raise the most suspicion that this is a malignant lesion? |
The absence of calcification
Pulmonary nodules are a common finding on routine studies, including plain chest radiographs, and require evaluation. Radiographic features of benign nodules include a diameter <5 mm, a smooth border, a solid appearance, concentric calcification, and a doubling time of less than 1 month or more than 1 year. Features of malignant nodules include a size >10 mm, an irregular border, a “ground glass” appearance, either no calcification or an eccentric calcification, and a doubling time of 1 month to 1 year (SOR B). |
|
|
A previously healthy 67-year-old male sees you for a routine health maintenance visit. During the physical examination you discover a harsh systolic murmur that is loudest over the second right intercostal space and radiates to the carotid arteries. The patient denies any symptoms of dyspnea, angina, syncope, or decreased exertional tolerance. An echocardiogram shows severe aortic stenosis, with an aortic valve area of <1 cm 2, a mean gradiant >40 mm Hg, and an ejection fraction of 60%.
What's the most appropriate next step? |
Watchful waiting
Watchful waiting is recommended for most patients with asymptomatic aortic stenosis, including those with severe disease (SOR B). This is because the surgical risk of aortic valve replacement outweighs the approximately 1% annual risk of sudden death in asymptomatic patients with aortic stenosis. Peripheral α-blockers, such as prazosin, should be avoided because of the risk of hypotension or syncope. Coronary angiography should be reserved for symptomatic patients who do not have evidence of severe aortic stenosis on echocardiography performed to evaluate their symptoms, or for preoperative evaluation prior to aortic valve replacement. Exercise stress testing is not safe with severe aortic stenosis because of the risk of death during the test. |
|
|
A 43-year-old female presents to your office for evaluation of a chronic cough that has been present for the past 6 months. She is not a smoker, and is not aware of any exposure to environmental irritants. She does not have any systemic complaints such as fever or weight loss, and does not have any symptoms of heartburn or regurgitation. She is not on any regular medications.
Auscultation of the lungs and a chest radiograph show no evidence of acute disease. A trial of an inhaled bronchodilator and antihistamine therapy does not improve the patient’s symptoms. What is the most appropriate next step? |
A trial of a proton pump inhibitor
Gastroesophageal reflux disease (GERD) is one of the most common causes of chronic cough. Patients with chronic cough have a high likelihood of having GERD, even in the absence of gastrointestinal symptoms (level of evidence 3). In fact, up to 75% of patients with a cough caused by GERD may have no gastrointestinal symptoms. The cough is thought to be triggered by microaspiration of acidic gastric contents into the larynx and upper bronchial tree. The American College of Chest Physicians states that patients with a chronic cough should be given a trial of antisecretory therapy (SOR B). Aggressive acid reduction using a proton pump inhibitor twice daily before meals for 3–4 months is the best way to demonstrate a causal relationship between GERD and extra-esophageal symptoms (SOR B). Methacholine inhalation testing is not necessary in this patient, since symptomatic asthma has been ruled out by the lack of response to bronchodilator therapy. Chest CT and pulmonary function tests are not indicated given the lack of findings from the history, physical examination, and chest film to suggest underlying pulmonary disease. An initial therapeutic trial of proton pump inhibitors is favored over 24-hour pH monitoring because it is less uncomfortable to the patient and has a better clinical correlation. |
|
|
A 27-year-old white male construction worker suffers from severe plaque-type psoriasis that has required systemic therapy. Which one of the following is associated with this condition?
|
An increased risk for the condition in the children of affected individuals
Psoriasis is a genetic inflammatory condition that has been associated with a significant risk of cardiovascular morbidity and mortality. Children of patients with the disorder are at increased risk. This is especially true if both parents have the disorder. Life expectancy is somewhat reduced in patients with severe psoriasis, particularly if the disease had an early onset. Plaque psoriasis is usually a lifelong disease; this is in contrast to guttate psoriasis, which may be self-limited and never recur. Cigarette smoking may increase the risk of developing psoriasis. Psoriasis is also associated with an increased likelihood of obesity, diabetes mellitus, and metabolic syndrome. |
|
|
A 29-year-old gravida 2 para 1 presents for pregnancy confirmation. Her last menstrual period began 6 weeks ago. Her medical history is significant for hypothyroidism, which has been well-controlled on levothyroxine (Synthroid), 150 μg daily, for the past 2 years.
Which one of the following would be the most appropriate next step in the treatment of this patient’s hypothyroidism during her pregnancy? |
Increase the levothyroxine dosage
Maternal hypothyroidism can have serious effects on the fetus, so thyroid dysfunction should be treated during pregnancy. Because of hormonal and metabolic changes in early pregnancy, the levothyroxine dosage often needs to be increased at 4–6 weeks gestation, and the patient eventually may require a 30%–50% increase in dosage in order to maintain her euthyroid status. |
|
|
A 37-year-old recreational skier is unable to lift his right arm after falling on his right side with his arm elevated. Radiographs of the right shoulder are negative, but diagnostic ultrasonography shows a complete rotator cuff tear.
Which one of the following is most accurate with regard to treatment? |
Surgery is most likely to be beneficial if performed less than 6 weeks after the injury
Surgery for rotator cuff tears is most beneficial in young, active patients. In cases of acute, traumatic, complete rotator cuff tears, repair is recommended in less than 6 weeks, as muscle atrophy is associated with reduced surgical benefit (SOR B). Advanced age and limited strength are also associated with reduced surgical benefit. NSAIDs are used for analgesia. Their benefit has not been shown to exceed that of other simple analgesics, and the side-effect profile may be higher. Corticosteroid injections will not improve a complete tear. Some experts also recommend avoiding their use in partial or complete tendon tears. Therapeutic ultrasound does not add to the benefit from range-of-motion exercises and exercises to strengthen the involved muscle groups |
|
|
A 72-year-old male with a history of hypertension and a previous myocardial infarction is diagnosed with heart failure. Echocardiography reveals systolic dysfunction, and recent laboratory tests indicated normal renal function, with a serum creatinine level of 1.1 mg/dL (N <1.5), a sodium level of 139 mEq/L (N 136–145), and a potassium level of 3.5 mEq/L (N 3.5–5.0). He is currently asymptomatic.
Which medication would be the best choice for initial management in this patient? |
Lisinopril (Prinivil, Zestril)
ACE inhibitors such as lisinopril are indicated for all patients with heart failure due to systolic dysfunction, regardless of severity. ACE inhibitors have been shown to reduce both morbidity and mortality, in both asymptomatic and symptomatic patients, in randomized, controlled trials. Unless absolutely contraindicated, ACE inhibitors should be used in all heart failure patients. No ACE inhibitor has been shown to be superior to another, and no study has failed to show benefit from an ACE inhibitor (SOR A). Direct-acting vasodilators such as isosorbide dinitrate also could be used in this patient, but ACE inhibitors have been shown to be superior in randomized, controlled trials (SOR B). β-Blockers are also recommended in heart failure patients with systolic dysfunction (SOR A), except those who have dyspnea at rest or who are hemodynamically unstable. These agents have been shown to reduce mortality from heart failure. A diuretic such as furosemide may be indicated to relieve congestion in symptomatic patients. Aldosterone antagonists such as spironolactone are also indicated in patients with symptomatic heart failure. In addition, they can be used in patients with a recent myocardial infarction who develop symptomatic systolic dysfunction and in those with diabetes mellitus (SOR B). Digoxin currently is recommended for patients with heart failure and atrial fibrillation, and can be considered in patients who continue to have symptoms despite maximal therapy with other agents. |
|
|
A 14-year-old female with a history of asthma is having daytime symptoms about once a week and symptoms that awaken her at night about once a month. Her asthma does not interfere with normal activity, and her FEV1 is >80% of predicted.
What is the most appropriate treatment plan for this patient? |
A short-acting inhaled β-agonist as needed
Based on this patient’s reported frequency of asthma symptoms, she should be classified as having intermittent asthma. The preferred first step in managing intermittent asthma is an inhaled short-acting β-agonist as needed. Daily medication is reserved for patients with persistent asthma (symptoms >2 days per week for mild, daily for moderate, and throughout the day for severe) and is initiated in a stepwise approach, starting with a daily low-dose inhaled corticosteroid or leukotriene receptor antagonist and then progressing to a medium-dose inhaled corticosteroid or low-dose inhaled corticosteroid plus a long-acting inhaled β-agonist. |
|
|
A 55-year-old female with diabetes mellitus, hypertension, and hyperlipidemia presents to your office for routine follow-up. Her serum creatinine level is 1.5 mg/dL (estimated creatinine clearance 50 mL/min).
Which diabetes medications would be contraindicated in this patient? |
Metformin (Glucophage)
Metformin is contraindicated in patients with chronic kidney disease. It should be stopped in females with a creatinine level ≥1.4 mg/dL and in males with a creatinine level ≥1.5 mg/dL. Pioglitazone should not be used in patients with hepatic disease. Acarbose should be avoided in patients with cirrhosis or a creatinine level >2.0 mg/dL. Exenatide is not recommended in patients with a creatinine clearance <30 mL/min. Insulin glargine can be used in patients with renal disease at any stage, but the dosage may need to be decreased. |
|
|
A 54-year-old female presents with a 2-month history of intense vulvar itching that has not improved with topical antifungal treatment. On examination you note areas of white, thickened, excoriated skin. Concerned about malignancy you perform punch biopsies, which reveal lichen sclerosus.
The treatment of choice for this condition is topical application of: |
fluorinated corticosteroids
Lichen sclerosus is a chronic, progressive, inflammatory skin condition found in the anogenital region. It is characterized by intense vulvar itching. The treatment of choice is high-potency topical corticosteroids. Testosterone has been found to be no more effective than petrolatum. Fluorouracil is an antineoplastic agent most frequently used to treat actinic skin changes or superficial basal cell carcinomas. |
|
|
Staff members of an assisted-living facility ask for your advice regarding aerobic exercise programs for their older residents. The evidence is greatest for which one of the following benefits of physical activity in the elderly?
|
Reducing the risk of falls
There is strong evidence that physical activity will prevent falls in the elderly. The evidence for maintaining weight, improving sleep, and increasing bone density is not as strong. |
|
|
The U.S. Preventive Services Task Force (USPSTF) has stated that the potential cardiovascular benefits of daily aspirin use outweigh the potential harms of gastrointestinal hemorrhage in certain populations. The USPSTF currently recommends daily aspirin use for which population?
|
Females 55–79 years of age
The U.S. Preventive Services Task Force (USPSTF) recommends daily aspirin use for males 45–79 years of age when the potential benefit of a reduction in myocardial infarction outweighs the potential harm of an increase in gastrointestinal hemorrhage, and for females 55–79 years of age when the potential benefit of a reduction in ischemic strokes outweighs the potential harm of an increase in gastrointestinal hemorrhage (SOR A, USPSTF A Recomendation). The USPSTF has concluded that the current evidence is insufficient to assess the balance of benefits and harms of aspirin for cardiovascular disease prevention in men and women 80 years of age or older (USPSTF I Recommendation). It recommends against the use of aspirin for stroke prevention in women younger than 55, and for myocardial infarction prevention in men younger than 45 (USPSTF D Recommendation). Ann Intern Med 2009; |
|
|
You see a newly adopted 5-month-old for his first well child visit. The parents ask when the child can sit in a safety seat in the car facing forward.
You would advise that the child should face rearward until he is at least: |
12 months of age AND weighs 20 lb
If a child faces forward in a crash, the force is distributed via the harness system across the shoulders, torso, and hips, but the head and neck have no support. Without support, the infant’s head moves rapidly forward in flexion while the body stays restrained, causing potential injury to the neck, spinal cord, and brain. In a rear-facing position, the force of the crash is distributed evenly across the baby’s torso, and the back of the child safety seat supports and protects the head and neck. For these reasons, the rear-facing position should be used until the child is at least 12 months old and weighs at least 20 lb (9 kg). For example, a 13-month-old child who weighs 19 lb should face rearward, and a 6-month-old child who weighs 21 lb should also face rearward. |
|
|
Which medication is most appropriate for the treatment of fibromyalgia syndrome?
|
Amitriptyline (Elavil)
A meta-analysis of antidepressant medications for the treatment of fibromyalgia syndrome concluded that short-term use of amitriptyline and duloxetine can be considered for the treatment of pain and sleep disturbance in patients with fibromyalgia. In addition, a 2008 evidence-based review for the management of fibromyalgia syndrome performed for the European League Against Rheumatism recommends heated pool treatment with or without exercise, tramadol for the management of pain, and certain antidepressants,including amitriptyline. Evidence for long-term effectiveness of antidepressants in fibromyalgia syndrome is lacking, however. |
|
|
In the secondary prevention of ischemic cardiac events, which one of the following is most likely to be beneficial in a 68-year-old female with known coronary artery disease and preserved left ventricular function?
|
ACE inhibitors
Secondary prevention of cardiac events consists of long-term treatment to prevent recurrent cardiac morbidity and mortality in patients who have either already had an acute myocardial infarction or are at high risk because of severe coronary artery stenosis, angina, or prior coronary surgical procedures. Effective treatments include aspirin, β-blockers after myocardial infarction, ACE inhibitors in patients at high risk after myocardial infarction, angiotensin II receptor blockers in those with coronary artery disease, and amiodarone in patients who have had a myocardial infarction and have a high risk of death from cardiac arrhythmias. Oral glycoprotein IIb/IIIa receptor inhibitors appear to increase the risk of mortality when compared with aspirin. Calcium channel blockers, class I anti-arrhythmic agents, and sotalol all appear to increase mortality compared with placebo in patients who have had a myocardial infarction. Contrary to decades of large observational studies, multiple randomized, controlled trials show no cardiac benefit from hormone therapy in postmenopausal women. |
|
|
A chest radiograph of the driver of an automobile involved in a head-on collision shows a widened mediastinum. This suggests:
|
partial rupture of the thoracic aorta
Deceleration-type blows to the chest can produce partial or complete transection of the aorta. A chest radiograph shows an acutely widened mediastinum and/or a pleural effusion when the condition is severe. The other conditions listed would produce mediastinal emphysema (esophageal or bronchial rupture), a widened heart, or pulmonary edema (acute heart failure, myocardial contusion). |
|
|
The most common initial symptom of Hodgkin lymphoma is:
|
painless lymphadenopathy
The most common presenting symptom of Hodgkin lymphoma is painless lymphadenopathy. Approximately one-third of patients with Hodgkin lymphoma present with unexplained fever, night sweats, and recent weight loss, collectively known as “B symptoms.” Other common symptoms include cough, chest pain, dyspnea, and superior vena cava obstruction caused by adenopathy in the chest and mediastinum. |
|
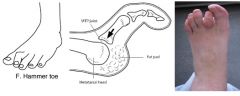
A 91-year-old white male presents with a 6-month history of a painless ulcer on the dorsum of the proximal interphalangeal joint of the second toe. Examination reveals a hallux valgus and a rigid hammer toe of the second digit. His foot has mild to moderate atrophic skin changes, and the dorsal and posterior tibial pulses are absent.
Appropriate treatment includes |

Custom-made shoes to protect the hammer toe
The treatment of foot problems in the elderly is difficult because of systemic and local infirmities, the most limiting being the poor vascular status of the foot. Conservative, supportive, and palliative therapy replace definitive reconstructive surgical therapy. Surgical correction of a hammer toe and bunionectomy could be disastrous in an elderly patient with a small ulcer and peripheral vascular disease. The best approach with this patient is to prescribe custom-made shoes and a protective shield with a central aperture of foam rubber placed over the hammer toe. Metatarsal pads are not useful in the treatment of hallux valgus and a rigid hammer toe. |
|
|
Hantavirus pulmonary syndrome results from exposure to the excreta of:
|
mice
Hantavirus pulmonary syndrome results from exposure to rodent droppings, mainly the deer mouse in the southwestern U.S. About 10% of deer mice are estimated to be infected with hantavirus. In other parts of the country the virus is carried by the white-footed mouse. While other rodents are carriers of the virus, they are less likely to live near dwellings, and populations are less dense. |
|
|
A 28-year-old white female consults you with a complaint of irregular heavy menstrual periods. A general physical examination, pelvic examination, and Papanicolaou test are normal and a pregnancy test is negative. A CBC and chemistry profile are also normal.
The next step in her workup should be: |
cyclic administration of progesterone for 3 months
Abnormal uterine bleeding is a relatively common disorder that may be due to functional disorders of the hypothalamus, pituitary, or ovary, as well as uterine lesions. However, the patient who is younger than 30 years of age will rarely be found to have a structural uterine defect. Once pregnancy, hematologic disease, and renal impairment are excluded, administration of intramuscular or oral progesterone will usually produce definitive flow and control the bleeding. No further evaluation should be necessary unless the bleeding recurs. Endometrial aspiration, dilatation and curettage, and other diagnostic procedures are appropriate for recurrent problems or for older women. Estrogen would only increase the problem, which is usually due to anovulation with prolonged estrogen secretion, producing a hypertrophic endometrium. |
|
|
A 45-year-old male with chronic nonmalignant back pain is on a chronic narcotic regimen. Which one of the following behaviors is LEAST likely to be associated with pseudoaddiction, as opposed to true addiction?
|
Concurrent abuse of alcohol or illicit drugs
The use of narcotics for chronic nonmalignant pain is becoming more commonplace. Guidelines have been developed to help direct the use of these medications when clinically appropriate. However, even when given appropriately, the use of opioid medications for pain relief can cause both the physician and the patient to be concerned about the possibility of addiction. Addiction is a neurobiologic, multifactorial disease characterized by impaired control, compulsive drug use, and continued use despite harm. Pseudoaddiction is a term used to describe patient behaviors that may occur when pain is undertreated. Patients with unrelieved pain may become focused on obtaining specific medications, seem to watch the clock, or engage in other behaviors that appear to be due to inappropriate drug seeking. Pseudoaddiction can be distinguished from true addiction because the behaviors will resolve when the pain is effectively treated. The concurrent use of alcohol and/or illicit drugs complicates the management of chronic pain in patients. If these are known problems, patients should be referred for psychiatric or pain specialty evaluation before the decision is made to use opioids. Agreements for use of chronic opioids should include the expectation that alcohol and illicit drugs will not be used concurrently, and doing so suggests addiction rather than pseudoaddiction. |
|
|
A 10-week-old term male infant is brought to your office with a 2-day history of difficulty breathing. He has been healthy since birth, with the exception of a 3-day episode of wheezing and rhinorrhea 3 weeks ago. Your initial examination shows an alert infant with increased work of breathing, rhinorrhea, and wheezing. His oxygen saturation is 93% and his temperature is 38.4°C (101.1°F).
What's the appropriate next step? |
A trial of nebulized albuterol (AccuNeb)
The American Academy of Pediatrics guideline on the diagnosis and management of bronchiolitis recommends against the use of laboratory or radiographic studies to make the diagnosis, although additional testing may be appropriate if there is no improvement. Bronchiolitis can be caused by a number of different viruses, alone or in combination, and the knowledge gained from virologic testing rarely influences management decisions or outcomes for the vast majority of children. While the guideline does not support routine use of bronchodilators in the management of bronchiolitis, it does allow for a trial of bronchodilators as an option in selected cases, and continuation of the treatment if the patient shows objective improvement in respiratory status. Bronchodilators have not been shown to affect the course of bronchiolitis with respect to outcomes. The guideline places considerable emphasis on hygienic practices, including the use of alcohol-based hand sanitizers before and after contact with the patient or inanimate objects in the immediate vicinity. Education of the family about hygienic practices is recommended as well. Returning the child to day care the next day is potentially harmful. |
|
|
What is the preferred treatment for Paget’s disease of bone?
|
Both bone formation and bone resorption are increased
Paget’s disease of bone is a focal disorder of skeletal metabolism in which all elements of skeletal remodeling (resorption, formation, and mineralization) are increased. There is no known relationship between Paget’s disease and multiple myeloma, although most cases of sarcoma in patients over 50 arise in pagetic bone. The preferred treatment for nearly all patients with symptomatic disease is one of the newer bisphosphonates. Treatment of bone pain resulting from Paget’s disease is generally very satisfactory, and in fact, relief may continue for many months or years after treatment is stopped, lending support for intermittent symptomatic therapy. Finally, despite the massive bone turnover, extracellular calcium homeostasis is almost invariably normal. |
|
|
The FDA recommends that over-the-counter cough and cold products not be used in children below the age of:
|
2 years
In 2008 the FDA issued a public health advisory for parents and caregivers, recommending that over-the-counter cough and cold products not be used to treat infants and children younger than 2 years of age, because serious and potentially life-threatening side effects can occur from such use. These products include decongestants, expectorants, antihistamines, and antitussives. |
|
|
In a patient with hyperuricemia who has experienced an attack of gout, which one of the following is LEAST likely to precipitate another gout attack?
A. Red meat B. Milk C. Seafood D. Nuts E. Beans |
Milk
Reducing consumption of red meat, seafood, and alcohol may help reduce the risk of a gout attack. Dairy products, in contrast to other foods high in protein, decrease the risk of another attack. Nuts and beans are high in purines and will worsen gout. |
|
|
Which one of the pharmacologic effects of transdermal medications changes the LEAST with aging?
A. Liver metabolism of the drugs B. Renal excretion of the drugs C. Distribution within the body D. Transdermal absorption of the drugs |
Transdermal absorption of medications changes very little with age. Due to an increase in the ratio of fat to lean body weight, the volume of distribution changes with aging, especially for fat-soluble drugs. Both liver metabolism and renal excretion of drugs decrease with aging, increasing serum concentrations.
|
|
|
A patient presents with a pigmented skin lesion that could be a melanoma. Its largest dimension is 0.5 cm.
What should be the first step in management? |
Excision with a 1-mm margin
The diagnosis of melanoma should be made by simple excision with clear margins. A shave biopsy should be avoided because determining the thickness of the lesion is critical for staging. Wide excision with or without node dissection is indicated for confirmed melanoma, depending on the findings from the initial excisional biopsy. |
|
|
What's the treatment for generalized anxiety disorder?
|
Cognitive-behavioral therapy has been shown to be at least as effective as medication for treatment of generalized anxiety disorder (GAD), but with less attrition and more durable effects. Many SSRIs and SNRIs have proven effective for GAD in clinical trials, but only paroxetine, escitalopram, duloxetine, and venlafaxine are approved by the FDA for this indication. Benzodiazepines have been widely used because of their rapid onset of action and proven effectiveness in managing GAD symptoms. SSRI or SNRI therapy is more beneficial than benzodiazepine or buspirone therapy for patients with GAD and comorbid depression.
|
|
|
A 20-month-old male presents with a history of a fever up to 38.5°C (101.3°F), pulling at both ears, drainage from his right ear, and a poor appetite following several days of nasal congestion. This is his first episode of acute illness, and he has no history of drug allergies.
The fever is confirmed on examination and the child is found to be fussy but can be distracted. He is eating adequately and shows no signs of dehydration. Positive findings include mild nasal congestion, a purulent discharge from the right auditory canal, and a red, bulging, immobile tympanic membrane in the left auditory canal. Which one of the following would be first-line treatment for this patient? |
Amoxicillin
This patient has acute bilateral otitis media, with presumed tympanic membrane perforation, and qualifies by any criterion for treatment with antibiotics. Amoxicillin, 80–90 mg/kg/day, should be the first-line antibiotic for most children with acute otitis media (SOR B). The other medications listed are either ineffective because of resistance (e.g., penicillin), are second-line treatments (e.g., amoxicillin/clavulanate), or should be used in patients with a penicillin allergy or in other special situations. |
|
|
An asymptomatic 68-year-old male sees you for a health maintenance visit. He is a former cigarette smoker, but quit 20 years ago.
According to the U.S. Preventive Services Task Force, evidence shows that the potential benefit exceeds the risk for which one of the following screening tests in this patient? A. A chest radiograph B. Abdominal ultrasonography C. Ophthalmic tonometry D. A prostate-specific antigen level E. An EKG |
Abdominal ultrasonography
The U.S. Preventive Services Task Force (USPSTF) recommends one-time screening for abdominal aortic aneurysm (AAA) by ultrasonography in men aged 65–75 who have ever smoked (SOR B, USPSTF B Recommendation). The USPSTF found good evidence that screening these patients for AAA and surgical repair of large AAAs (≥5.5 cm) leads to decreased AAA-specific mortality. There is good evidence that abdominal ultrasonography, performed in a setting with adequate quality assurance (i.e., in an accredited facility with credentialed technologists), is an accurate screening test for AAA. There is also good evidence of important harms from screening and early treatment, including an increased number of operations, with associated clinically significant morbidity and mortality, and short-term psychological harms. Based on the moderate magnitude of net benefit, the USPSTF concluded that the benefits of screening for AAA in men aged 65–75 who have ever smoked outweighs the potential harm. While they may be considered for making the diagnosis in patients who have symptoms, none of the other tests listed have evidence to support a net benefit from their use as routine screening tools in patients like the one described here. |
|
|
A 52-year-old hypertensive male has had two previous myocardial infarctions. In spite of his best efforts, he has not achieved significant weight loss and he finds it difficult to follow a heart-healthy diet. He takes rosuvastatin (Crestor), 20 mg/day, and his last lipid profile showed a total cholesterol level of 218 mg/dL, a triglyceride level of 190 mg/dL, an HDL-cholesterol level of 45 mg/dL, and an LDL-cholesterol level of 118 mg/dL.
What would be the most appropriate change in management? |
Increase the rosuvastatin dosage
This patient’s goal LDL-cholesterol level is 70 mg/dL, and he is not at the maximum dosage of a potent statin. There is no data that shows that adding a different statin will be beneficial, and outcomes data for the other actions is lacking. For patients not at their goal LDL-cholesterol level, the maximum dosage of a statin should be reached before alternative therapy is chosen. |
|
|
A hemoglobin A1c of 7.0% would correspond to what mean (average) plasma glucose levels?
|
154 mg/dL
A hemoglobin A1c(HbA1c) of 6.0% correlates with a mean plasma glucose level of 126 mg/dL or 7.0 1c 1c mmol/dL. A calculator to convert HbA1clevels into estimated average glucose levels is available at http://professional.diabetes.org/eAG. A rough guide for estimating average plasma glucose levels assumes that an 1cof 6.0% equals an average glucose level of 120 mg/dL. Each percentage point increase in 1c is equivalent to a 30-mg/dL rise in average glucose. An HbA1cof 7.0% is therefore roughly equivalent to an average glucose level of 150 mg/dL, and an HbA1c of 8.0% translates to an average glucose level of 180 mg/dL. |
|
|
A 50-year-old male is brought to the emergency department with shortness of breath, chest tightness, tremulousness, and diaphoresis. Aside from tachypnea, the physical examination is normal. Arterial blood gases on room air show a pO2 of 98 mm Hg (N 80–100), a pCO2 of 24 mm Hg (N 35–45), and a pH of 7.57 (N 7.38–7.44).
The most likely cause of the patient’s blood gas abnormalities is: |
anxiety disorder with hyperventilation
The elevated pH, normal oxygen saturation, and low pCO2 are characteristic of acute respiratory alkalosis, as seen with acute hyperventilation states. In patients with a pulmonary embolism, pO2 and pCO2 are decreased, while the pH is elevated, indicating the acute nature of the disorder. With the other diagnoses, findings on the physical examination would be different than those seen in this patient. Vital signs would be normal with carbon monoxide poisoning, and patients with an asthma exacerbation have a prominent cough and wheezing, and possibly other abnormalities. Tension pneumothorax causes severe cardiac and respiratory distress, with significant physical findings including tachycardia, hypotension, and decreased mental activity. |
|
|
A 58-year-old male presents with recent behavior and personality changes, and you suspect dementia. Which one of the following is most likely to present in this manner?
|
Frontotemporal dementia
Frontotemporal dementia is the second most common cause of early-onset dementia. It often presents with behavioral and personality changes. Examples include disinhibition, impairment of personal conduct, loss of emotional sensitivity, loss of insight, and executive dysfunctions. Alzheimer’s disease presents with memory loss and visuospatial problems. Vascular dementia is associated with risk factors for stroke, or occurs in relation to a stroke, with a stepwise progression. Alzheimer’s disease and vascular dementia can occur together, with features of both. Progressive supranuclear palsy is characterized by early falls, vertical (especially downward) gaze, axial rigidity greater than appendicular rigidity, and levodopa resistance. |
|
|
A 60-year-old female receiving home hospice care was taking oral morphine, 15 mg every 2 hours, to control pain. When this was no longer effective, she was transferred to an inpatient facility for pain control. She required 105 mg of morphine in a 24-hour period, so she was started on intravenous morphine, 2 mg/hr with a bolus of 2 mg, and was well controlled for 5 days. However, her pain has worsened over the past 2 days.
What is the most likely cause of this patient’s increased pain? |
Tolerance to morphine
This patient has become tolerant to morphine. The intravenous dose should be a third of the oral dose, so the starting intravenous dose was adequate. Addiction is compulsive narcotic use. Pseudoaddiction is inadequate narcotic dosing that mimics addiction because of unrelieved pain. Physical dependence is seen with abrupt narcotic withdrawal. |
|
|
A 72-year-old white male presents with a complaint of headache, blurred vision, and severe right eye pain. His symptoms began acutely about 1 hour ago. Examination of the eye reveals a mid-dilated, sluggish pupil; a hazy cornea; and a red conjunctiva.
What is the most likely diagnosis? |
Acute angle-closure glaucoma
This patient presents with acute angle-closure glaucoma, manifested by an acute onset of severe pain, blurred vision, halos around lights, increased intraocular pressure, red conjunctiva, a mid-dilated and sluggish pupil, and a normal or hazy cornea. Findings with retinal detachment include either normal vision or peripheral or central vision loss; absence of pain; increasing floaters; and a normal conjunctiva, cornea, and pupil. Central retinal artery occlusion findings include amaurosis fugax, a red conjunctiva, a pale fundus, a cherry-red spot at the fovea, and “boxcarring” of the retinal vessels. In patients with mechanical injury to the globe, findings include moderate to severe pain, normal or decreased vision, subconjunctival hemorrhage completely surrounding the cornea, and a pupil that is irregular or deviated toward the injury (SOR B). |
|
|
The mother of an 8-year-old female is concerned about purple “warts” on her daughter’s hands. The mother explains that the lesions started a few months ago on the right hand along the top of most of the knuckles and interphalangeal joints, and she has recently noticed them on the left hand. The child has no other complaints and the mother denies any unusual behaviors. A physical examination is unremarkable except for the slightly violaceous, flat-topped lesions the mother described.
What is the most likely cause for this patient’s finger lesions? |
Dermatomyositis
One of the most characteristic findings in dermatomyositis is Gottron’s papules, which are flat-topped, sometimes violaceous papules that often occur on most, if not all, of the knuckles and interphalangeal joints |
|
|
A 20-year-old patient comes to the emergency department complaining of shortness of breath. On examination his heart rate is 180 beats/min, and his blood pressure is 122/68 mm Hg. An EKG reveals a narrow complex tachycardia with a regular rhythm.
What would be the most appropriate initial treatment? |
Adenosine (Adenocard)
After vagal maneuvers are attempted in a stable patient with supraventricular tachycardia, the patient should be given a 6-mg dose of adenosine by rapid intravenous push. If conversion does not occur, a 12-mg dose should be given. This dose may be repeated once. If the patient is unstable, immediate synchronized cardioversion should be administered. |
|
|
A patient complains of throbbing bone pain in her lower back and legs. She also has felt weaker recently. What tests would confirm a vitamin D deficiency?
|
25-hydroxyvitamin D
Serum 25-hydroxyvitamin D should be obtained in any patient with suspected vitamin D deficiency because it is the major circulating form of vitamin D (SOR A). 1,25-Dihydroxyvitamin D is the most active metabolite, but levels can be increased by secondary hyperparathyroidism. In persons with vitamin D deficiency, ergocalciferol (vitamin D ) or cholecalciferol (vitamin D ) can be used to replenish stores (SOR 2 3B). |
|
|
A patient is sent to you by his employer after falling down some steps and twisting his ankle and foot. Which one of the following would be the most appropriate reason to obtain foot or ankle radiographs?
|
Pain in the maleolar zone and bone tenderness of the posterior medial malleolus
The Ottawa ankle and foot rules are prospectively validated decision rules that help clinicians decrease the use of radiographs for foot and ankle injuries without increasing the rate of missed fracture. The rules apply in the case of blunt trauma, including twisting injuries, falls, and direct blows. According to these guidelines, an ankle radiograph series is required only if there is pain in the malleolar zone and bone tenderness of either the distal 6 cm of the posterior edge or the tip of either the lateral malleolus or the medial malleolus. Inability to bear weight for four steps, both immediately after the injury and in the emergency department, is also an indication for ankle radiographs. Foot radiographs are required only if there is pain in the midfoot zone and bone tenderness at the base of the 5th metatarsal or the navicular, or if the patient is unable to bear weight both immediately after the injury and in the emergency department. A positive Thompson sign, seen with Achilles tendon rupture, is the absence of passive plantar foot flexion when the calf is squeezed. |
|
|
A 77-year-old white male complains of urinary incontinence of more than one year’s duration. The incontinence occurs with sudden urgency. No association with coughing or positional change has been noted, and there is no history of fever or dysuria. He underwent transurethral resection of the prostate (TURP) for benign prostatic hypertrophy a year ago, and he says his urinary stream has improved. A rectal examination reveals a smoothly enlarged prostate without nodularity, and normal sphincter tone. No residual urine is found with post-void catheterization.
What is the most likely cause of this patient’s incontinence? |
Detrusor instability
In elderly patients, detrusor instability is the most common cause of urinary incontinence in both men and women. Incontinence may actually become worse after surgical relief of obstructive prostatic hypertrophy. Infection is unlikely as the cause of persistent incontinence in this patient in the absence of fever or symptoms of urinary tract infection. Overflow is unlikely in the absence of residual urine. Impaction is a relatively rare cause of urinary incontinence, and associated findings would be present on rectal examination. Normalization of the urinary stream and the absence of residual urine reduce the likelihood of recurrent obstruction. The prostate would be expected to remain enlarged on rectal examination after transurethral resection of the prostate (TURP). |
|
|
A 47-year-old male is preparing for a 3-day trip to central Mexico to present the keynote address for an international law symposium. He asks you for an antibiotic to be taken prophylactically to prevent bacterial diarrhea.
Which one of the following would you recommend? |
Rifaximin (Xifaxan)
While prophylactic antibiotics are not generally recommended for prevention of traveler’s diarrhea, they may be useful under special circumstances for certain high-risk hosts, such as the immunocompromised, or for those embarking on critical short trips for which even a short period of diarrhea might cause undue hardship. Rifaximin, a nonabsorbable antibiotic, has been shown to reduce the risk for traveler’s diarrhea by 77%. Trimethoprim/sulfamethoxazole and doxycycline are no longer considered effective antimicrobial agents against enteric bacterial pathogens. Increasing resistance to the fluoroquinolones, especially among Campylobacter species, is limiting their use as prophylactic agents. |
|
|
A 34-year-old female with a history of bilateral tubal ligation consults you because of excessive body and facial hair. She has a normal body weight, no other signs of virilization, and regular menses.
Which one of the following is the most appropriate treatment for her mild hirsutism? |
Spironolactone (Aldactone)
Antiandrogens such as spironolactone, along with oral contraceptives, are recommended for treatment of hirsutism in premenopausal women (SOR C). In addition to having side effects, prednisone is only minimally helpful for reducing hirsutism by suppressing adrenal androgens. Leuprolide, although better than placebo, has many side effects and is expensive. Metformin can be used to treat patients with polycystic ovarian syndrome, but this patient does not meet the criteria for this diagnosis. |
|
|
An 80-year-old male nursing-home resident is brought to the emergency department because of a severe, productive cough associated with a high fever, hypoxia, and hypotension. The patient is found to have a left lower lobe pneumonia, and admission to the intensive-care unit is advised.
What is the most appropriate antibiotic therapy for this patient? |
Ceftazidime (Fortaz), imipenem/cilastatin (Primaxin), and vancomycin (Vancocin)
Empiric coverage for methicillin-resistant Staphylococcus aureus and double coverage for pseudomonal pneumonia should be prescribed in patients with nursing home–acquired pneumonia requiring intensive-care unit admission (SOR B). |
|
|
A 67-year-old white female has a DXA scan with a resulting T-score of –2.7. She has a strong family history of breast cancer.
What would be the most appropriate treatment for this patient? |
Raloxifene (Evista)
Raloxifene is a selective estrogen receptor modulator. While it increases the risk of venous thromboembolism, it is indicated in this patient to decrease the risk of invasive breast cancer (SOR A). Bisphosphonates inhibit osteoclastic activity. Zoledronic acid, alendronate, and risedronate decrease both hip and vertebral fractures, whereas ibandronate decreases fracture risk at the spine only. Calcitonin nasal spray is an antiresorptive spray that decreases the incidence of vertebral compression fractures. Teriparatide is a recombinant human parathyroid hormone with potent bone anabolic activity, effective against vertebral and nonvertebral fractures. Hormone replacement therapy is recommended for osteoporosis only in women with moderate or severe vasomotor symptoms. The lowest possible dose should be used for the shortest amount of time possible (SOR C). |
|
|
A 50-year-old white female comes to you because she has found a breast mass. Your examination reveals a firm, fixed, nontender, 2-cm mass. No axillary nodes are palpable, nor is there any nipple discharge. You send her for a mammogram, and fine-needle aspiration is performed to obtain cells for cytologic examination. The mammogram is read as “suspicious” and the fine-needle cytology report reads, “a few benign ductal epithelioid cells and adipose tissue.”
What would be the most appropriate next step? |
An excisional biopsy of the mass
In the ideal setting, the accuracy of fine-needle aspiration may be over 90%. Clinical information is critical for interpreting the results of fine-needle aspiration, especially given the fact that the tissue sample is more limited than with a tissue biopsy. It is crucial to determine whether the findings on fine-needle aspiration explain the clinical findings. Although the report from the mammogram and the biopsy are not ominous in this patient, they do not explain the clinical findings. Immediate repeat fine-needle aspiration or, preferably, a tissue biopsy is indicated. Proceeding directly to therapy, whether surgery or irradiation, is inappropriate because the diagnosis is not clearly established. Likewise, any delay in establishing the diagnosis is not appropriate |
|
|
A 67-year-old female comes to your office because she noticed flashing lights in her left eye 2 hours ago, and since then has had decreased vision in the lateral aspect of that eye. On examination she has a blind spot in the lateral visual field of her left eye. Her fundus is difficult to examine because of an early cataract.
What is the most likely diagnosis? |
Retinal detachment
In a patient complaining of flashes of light and a visual field defect, retinal detachment is the most likely diagnosis. Many cases of vitreous detachment are asymptomatic, and it does not cause sudden visual field defects in the absence of a retinal detachment. A vitreous hemorrhage would cause more blurring of vision in the entire field of vision. Ocular migraine causes binocular symptoms. |
|
|
A 27-year-old white female at 12 weeks gestation comes to your office complaining of a vaginal discharge. On speculum examination you note a purulent cervical discharge with a friable cervix. A gonorrhea culture is negative. You make a diagnosis of Chlamydia trachomatis cervicitis.
What is the appropriate treatment? |
Azithromycin (Zithromax)
Azithromycin is the drug of choice for Chlamydia trachomatis infections in pregnant patients. Metronidazole is used to treat trichomoniasis and Gardnerella vaginitis after 12 weeks gestation. The use of tetracycline is not appropriate in pregnant women, and miconazole is used to treat vaginal candidiasis. |
|
|
A previously alert, otherwise healthy 74-year-old African-American male has a history of slowly developing progressive memory loss and dementia associated with urinary incontinence and gait disturbance resembling ataxia. This presentation is most consistent with:
|
normal pressure hydrocephalus
In normal pressure hydrocephalus a mild impairment of memory typically develops gradually over weeks or months, accompanied by mental and physical slowness. The condition progresses insidiously to severe dementia. Patients also develop an unsteady gait and urinary incontinence, but there are no signs of increased intracranial pressure. In Alzheimer’s disease the brain very gradually atrophies. A disturbance in memory for recent events is usually the first symptom, along with some disorientation to time and place; otherwise, there are no symptoms for some period of time. Subacute sclerosing panencephalitis usually occurs in children and young adults between the ages of 4 and 20 years and is characterized by deterioration in behavior and work. The most characteristic neurologic sign is mild clonus. Multiple sclerosis is characteristically marked by recurrent attacks of demyelinization. The clinical picture is pleomorphic, but there are usually sufficient typical features of incoordination, paresthesias, and visual complaints. Mental changes may occur in the advanced stages of the disease. About two-thirds of those affected are between the ages of 20 and 40. |
|
|
You see a 1-year-old male for a routine well child examination. Laboratory tests reveal a hemoglobin level of 10 g/dL (N 9–14), a hematocrit of 31% (N 28–42), a mean corpuscular volume of 68 :m3 (N 70–86), and a mean corpuscular hemoglobin concentration of 25 g/dL (N 30–36). A trial of iron therapy results in no improvement and a serum lead level is normal.
What would be the most appropriate test at this time? |
Hemoglobin electrophoresis
This patient has a microcytic, hypochromic anemia, which can be caused by iron deficiency, thalassemia, sideroblastic anemia, and lead poisoning. In a child with a microcytic anemia who does not respond to iron therapy, hemoglobin electrophoresis is appropriate to diagnose thalassemia. Hypothyroidism, vitamin B12 deficiency, and folate deficiency result in macrocytic anemias. |
|
|
A 42-year-old white male develops respiratory distress 12 hours after he sustained a closed head injury and a femur fracture. A physical examination reveals a respiratory rate of 40/min. He has a pO2 of 45 mm Hg (N 75–100), a pCO2 of 25 mm Hg (N 35–45), and a blood pH of 7.46 (N 2 2 7.35–7.45). His hematocrit is 30.0% (N 37.0–49.0).
the most likely diagnosis is: |
adult respiratory distress syndrome (ARDS)
Acute respiratory failure following severe injury and critical illness has received increasing attention over the last decade. With advances in the management of hemorrhagic shock and support of circulatory and renal function in injured patients, it has become apparent that 1%–2% of significantly injured patients develop acute respiratory failure in the post-injury period. Initially this lung injury was thought to be related to a particular clinical situation. This is implied by such names as “shock lung” and “traumatic wet lung,” which have been applied to acute respiratory insufficiency. It is now recognized that the pulmonary problems that follow a variety of insults have many similarities in their clinical presentation and physiologic and pathologic findings. This has led to the theory that the lung has a limited number of ways of reacting to injury and that several different types of acute, diffuse lung injury result in a similar pathophysiologic response. The common denominator of this response appears to be injury at the alveolar-capillary interface, with resulting leakage of proteinaceous fluid from the intravascular space into the interstitium and subsequently into alveolar spaces. It has become acceptable to describe this entire spectrum of acute diffuse injury as adult respiratory distress syndrome (ARDS). The syndrome of ARDS can occur under a variety of circumstances and produces a spectrum of clinical severity from mild dysfunction to progressive, eventually fatal, pulmonary failure. Fortunately, with proper management, pulmonary failure is far less frequent than milder abnormalities. |
|
|
A 40-year-old white male presents with a 5-year history of periodic episodes of severe right-sided headaches. During the most recent episode the headaches occurred most days during January and February and lasted about 1 hour.
The most likely diagnosis is: |
Cluster Headache
Cluster headache is predominantly a male disorder. The mean age of onset is 27–30 years. Attacks often occur in cycles and are unilateral. Migraine headaches are more common in women, start at an earlier age (second or third decade), and last longer (4–24 hours). Temporal arteritis occurs in patients above age 50. Trigeminal neuralgia usually occurs in paroxysms lasting 20–30 seconds. |
|
|
A 24-year-old male presents with a fever of 38.9°C (102.0°F), generalized body aches, a sore throat, and a cough. His symptoms started 24 hours ago. He is otherwise healthy. You suspect novel influenza A H1N1 infection, as there have been numerous cases in your community recently. A rapid influenza diagnostic test is positive, and you recommend over-the-counter symptomatic treatment. You see him 2 days later after he is admitted to the hospital through the emergency department with dehydration and mild respiratory distress. A specimen is sent to the state laboratory for PCR testing.
Most appropriate treatment? |
Oseltamivir (Tamiflu)
The currently circulating novel influenza A H1N1 virus is almost always susceptible to neuraminidase inhibitors (oseltamivir and zanamivir) and resistant to the adamantanes (amantadine and rimantadine). Zanamivir should not be used in patients with COPD, asthma, or respiratory distress. Antiviral treatment of influenza is recommended for all persons with clinical deterioration requiring hospitalization, even if the illness started more than 48 hours before admission. Antiviral treatment should be started as soon as possible. Waiting for laboratory confirmation is not recommended. |
|
|
A 59-year-old white male is being evaluated for hypertension. His blood pressure is 150/95 mm Hg. His medical history includes impotence, asthma, gout, first degree heart block, diet-controlled diabetes mellitus, and depression, but he is currently taking no medications. He has a past history of alcohol abuse, but quit drinking 10 years ago.
Which one of the following would be the best choice for INITIAL therapy of his hypertension? |
Enalapril (Vasotec)
NOT HCTZ or Propanolol Because of their favorable side-effect profile, ACE inhibitors (e.g., enalapril) may be the drugs of first choice for the majority of unselected hypertensive patients. ACE inhibitors are not associated with depression or sedation, and they are safe to use in patients with diabetes mellitus. Centrally-acting α-blockers can be associated with depression. Calcium-channel blockers, β-blockers, and other sympatholytic drugs affect cardiac conductivity.β-Blockers are contraindicated in patients with asthma, and are also associated with impotence. Thiazide diuretics raise uric acid and blood glucose levels. |
|
|
A 51-year-old immigrant from Vietnam presents with a 3-week history of nocturnal fever, sweats, cough, and weight loss. A chest radiograph reveals a right upper lobe cavitary infiltrate. A PPD produces 17 mm of induration, and acid-fast bacilli are present on a smear of induced sputum.
While awaiting formal laboratory identification of the bacterium,what would be most appropriate empiric treatment? |
INH, ethambutol, rifampin (Rifadin), and pyrazinamide
Leading authorities, including experts from the American Thoracic Society, CDC, and Infectious Diseases Society of America, mandate aggressive initial four-drug treatment when tuberculosis is suspected. Delays in diagnosis and treatment not only increase the possibility of disease transmission, but also lead to higher morbidity and mortality. Standard regimens including INH, ethambutol, rifampin, and pyrazinamide are recommended, although one regimen does not include pyrazinamide but extends coverage with the other antibiotics. Treatment regimens can be modified once culture results are available. |
|
|
An incidental 2-cm adrenal nodule is discovered on renal CT performed to evaluate hematuria in a 57-year-old female with flank pain. She has no past medical history of palpitations, headache, hirsutism, sweating, osteoporosis, diabetes mellitus, or hypertension. A physical examination is normal, with the exception of a blood pressure of 144/86 mm Hg. Laboratory evaluation reveals a serum sodium level of 140 mmol/L (N 135–145) and a serum potassium level of 3.8 mmol/L (N 3.5–5.0).
What is the most appropriate next step in the evaluation of this patient? |
Evaluation for adrenal hormonal secretion
The incidental discovery of adrenal masses presents a common clinical challenge. Such masses are found on abdominal CT in 4% of cases, and the incidence of adrenal masses increases to 7% in adults over 70 years of age. While the majority of masses are benign, as many as 11% are hypersecreting tumors and approximately 7% are malignant tumors; the size of the mass and its appearance on imaging are major predictors of malignancy. Once an adrenal mass is identified, adrenal function must be assessed with an overnight dexamethasone suppression test. A morning cortisol level >5 μg/dL after a 1-mg dose indicates adrenal hyperfunction. Additional testing should include 24-hour fractionated metanephrines and catecholamines to rule out pheochromocytoma. If the patient has hypertension, morning plasma aldosterone activity and plasma renin activity should be assessed to rule out a primary aldosterone-secreting adenoma. Nonfunctioning masses require assessment with CT attenuation, chemical shift MRI, and/or scintigraphy to distinguish malignant masses. PET scanning is useful to verify malignant disease. Nonfunctioning benign masses can be monitored for changes in size and for the onset of hypersecretory states, although the appropriate interval and studies are controversial. MRI may be preferred over CT because of concerns about excessive radiation exposure. Fine-needle aspiration of the mass can be performed to differentiate between adrenal and non-adrenal tissue after malignancy and pheochromocytoma have been excluded. |
|
|
What population has been shown to benefit from screening for asymptomatic bacteriuria?
|
Women who are pregnant
Clinical guidelines published by the U.S. Preventive Services Task Force in 2008 reaffirmed the 2004 recommendations regarding screening for asymptomatic bacteriuria in adults. The only group in which screening is recommended is asymptomatic pregnant women at 12–16 weeks gestation, or at the first prenatal visit if it occurs later (SOR A). |
|
|
In a patient with microcytic anemia, what pattern of laboratory abnormalities would be most consistent with iron deficiency as the underlying cause?
|
Ferritin low, TIBC high, serum iron low
Ferritin and serum iron levels fall with iron deficiency. Total iron binding capacity rises, indicating a greater capacity for iron to bind to transferrin (the plasma protein that binds to iron for transport throughout the body) when iron levels are low. |
|
|
A 12-year-old female is brought to your office with an 8-day history of sore throat and fever, along with migratory aching joint pain. She is otherwise healthy and has no history of travel, tick exposure, or prior systemic illness. A physical examination is notable for exudative pharyngitis; a blanching, sharply demarcated macular rash over her trunk; and a III/VI systolic ejection murmur. Joint and neurologic examinations are normal. A rapid strep test is positive and her C-reactive protein level is elevated.
Of the following, the most likely diagnosis is: |
acute rheumatic fever
Acute rheumatic fever is very common in developing nations. It was previously rare in the U.S., but had a resurgence in the mid-1980s. It is most common in children ages 5–15 years. The diagnosis is based on the Jones criteria. Two major criteria, or one major criterion and two minor criteria, plus evidence of a preceding streptococcal infection, indicate a high probability of the disease. Major criteria include carditis, migratory polyarthritis, erythema marginatum, chorea, and subcutaneous nodules. Minor criteria include fever, arthralgia, an elevated erythrocyte sedimentation rate or C-reactive protein (CRP) level, and a prolonged pulse rate interval on EKG. The differential diagnosis is extensive and there is no single laboratory test to confirm the diagnosis. This patient meets one major criterion (erythema marginatum rash) and three minor criteria (fever, elevated CRP levels, and arthralgia). Echocardiography should be performed if the patient has cardiac symptoms or an abnormal cardiac examination, to rule out rheumatic carditis. |
|
|
A 73-year-old female presents with complaints of dyspnea and decreasing exercise tolerance over the past few months. She says she has to prop herself up on two pillows in order to breathe better. She also complains of palpitations, even at rest. She has long-standing hypertension, but has not taken any antihypertensive medications for several years. She has no history of ischemic heart disease. On examination her blood pressure is 155/92 mm Hg, her pulse rate is 108 beats/min and irregular, and her lungs have bibasilar crackles. An EKG reveals atrial fibrillation, but no changes of acute ischemia.
What test or lab finding would be most useful for determining her initial treatment? |
Echocardiography
This patient’s history and clinical examination suggest heart failure. The most important distinction to make is whether it is diastolic or systolic, as the drug treatment may be somewhat different. Physical findings and chest radiographs do not distinguish systolic from diastolic heart failure. An echocardiogram is the study of choice, as it will assess left ventricular function. In diastolic dysfunction, the left ventricular ejection fraction is normal or slightly elevated. Diastolic failure is more common in elderly females and patients with hypertension, and less common in patients with a previous history of coronary artery disease. Diuretics and angiotensin receptor blockers (ARBs) are useful treatments. Because of their effects on diastolic filling times, tachycardia and atrial fibrillation often cause decompensation in patients with diastolic heart failure. At this time, cardiac catheterization is not indicated, and a stress test will not provide useful information. If the patient had systolic failure, a workup for ischemic disease would be needed, but most cases of diastolic dysfunction are not caused by ischemia. While hyperthyroidism can cause tachycardia and atrial fibrillation, the more immediate issue in this patient is the heart failure, which requires diagnosis and treatment. A pulmonary embolus can cause shortness of breath but usually has an acute onset, so a D-dimer level would not help at this time. |
|
|
A 62-year-old male on hemodialysis develops a pruritic rash on his arms and chest, with erythematous, thickened plaques and edema. He had brain imaging with a gadolinium-enhanced MRI for neurologic symptoms 10 days ago.
Which one of the following is true regarding this problem? |
A skin biopsy is diagnostic
This patient has gadolinium-associated nephrogenic systemic fibrosis, which is associated with the use of gadolinium-based contrast material in patients with severe renal dysfunction, often on dialysis. Associated proinflammatory states, such as recent surgery, malignancy, and ischemia, are often present as well. This condition occurs without regard to gender, race, or age. Dermatologic manifestations are usually seen, but multiple organ systems may be involved. There is no effective treatment, and mortality is approximately 30%. A deep biopsy of the affected skin is diagnostic. |
|
|
A 3-year-old male is brought to the emergency department by his parents, who report seeing him swallow a handful of adult ibuprofen tablets 20 minutes ago.What would be the most appropriate initial management of this patient?
|
Oral activated charcoal
A single dose of activated charcoal is the decontamination treatment of choice for most medication ingestions. It should be used within 1 hour of ingestion of a potentially toxic amount of medication (SOR C). Gastric lavage, cathartics, or whole bowel irrigation is best for ingestion of medications that are poorly absorbed by activated charcoal (iron, lithium) or medications in sustained-release or enteric-coated formulations. Ipecac has no role in home use or in the health care setting (SOR C). |
|
|
A 26-year-old gravida 3 para 2 was diagnosed with gestational diabetes mellitus at 24 weeks gestation. She was prescribed appropriate nutritional therapy and an exercise program. After 4 weeks, her fasting plasma glucose levels remain in the range of 105–110 mg/dL.
What would be the most appropriate treatment for this patient at this time? |
A combination of intermediate-acting insulin (e.g., NPH) and a short-acting insulin (e.g., lispro) twice daily
In addition to an appropriate diet and exercise regimen, pharmacologic therapy should be initiated in pregnant women with gestational diabetes mellitus whose fasting plasma glucose levels remain above 100 mg/dL despite diet and exercise. There is strong evidence that such treatment to maintain fasting plasma glucose levels below 95 mg/dL and 1-hour postprandial levels below 140 mg/dL results in improved fetal well-being and neonatal outcomes. While oral therapy with metformin or glyburide is considered safe and possibly effective, insulin therapy is the best option for the pharmacologic treatment of gestational diabetes. Thiazolidinediones such as pioglitazone have not been shown to be effective or safe in pregnancy. The use of long-acting basal insulin analogues, such as glargine and detemir, has not been sufficiently evaluated in pregnancy. Sliding-scale coverage with ultra-short-acting insulin or insulin analogues, such as lispro and aspart, is generally not required in most women with gestational diabetes. While it may be effective, it involves four daily glucose checks and injections. Most patients are successfully treated with a twice-daily combination of an intermediate-acting insulin and a short-acting insulin while continuing a diet and exercise program. |
|
|
A 45-year-old Hispanic male with schizophrenia presents with an exacerbation of his COPD. He currently takes only ziprasidone (Geodon). He asks for a prescription for clarithromycin (Biaxin) because it has worked well for previous exacerbations.
What effects of this drug combination should you be alert for? |
Prolonged QT interval
Ziprasidone is a second-generation antipsychotic used in the treatment of schizophrenia. These drugs cause QT-interval prolongation, which can in turn lead to torsades de pointes and sudden cardiac death. This risk is further increased when these drugs are combined with certain antibiotics (e.g., clarithromycin), antiarrhythmics (class I and III), and tricyclic antidepressants. The FDA has issued a black box warning for both first- and second-generation antipsychotic drugs due to a 1.6- to 1.7-fold increase in the risk of sudden cardiac death and cerebrovascular accidents associated with their use in the elderly population (SOR A). None of the other conditions listed is associated with this drug combination. |
|
|
A 44-year-old female presents with a complaint of increasingly dry eyes over the past 3–4 months, and says she can no longer wear contacts due to the discomfort and itching. She also apologizes for chewing gum during the visit, explaining that it helps keep her mouth moist. On examination you note decreased tear production, decreased saliva production, and new dental caries. She stopped taking a daily over-the-counter allergy medication about 1 month ago.
What is the most likely diagnosis? |
Sjögren’s syndrome
Sjögren’s syndrome is one of the three most common systemic autoimmune diseases. It results from lymphocytic infiltration of exocrine glands and leads to acinar gland degeneration, necrosis, atrophy, and decreased function. A positive anti-SS-A or anti-SS-B antigen test or a positive salivary gland biopsy is a criterion for classification of this diagnosis. In addition to ocular and oral complaints, clinical manifestations include arthralgias, thyroiditis, pulmonary disease, and GERD. Most patients with sarcoidosis present with shortness of breath or skin manifestations, and patients with lupus generally have fatigue and joint pain. Ocular rosacea causes eye symptoms very similar to those of Sjögren’s syndrome, but oral findings would not be expected. Drugs such as anticholinergics can cause a dry mouth, but this would be unlikely a month after the medication was discontinued (SOR B). |
|
|
A 14-year-old female is brought to your office by her mother because of a 3-month history of irritability, hypersomnia, decline in school performance, and lack of interest in her previous extracurricular activities. The mother is also your patient, and you know that she has a history of depression and has recently separated from her husband. After an appropriate workup, you diagnose depression in the daughter.
For initial therapy you recommend: |
cognitive-behavioral therapy
This patient has multiple risk factors for depression: the hormonal changes of puberty, a family history of depression, and psychosocial stressors. Cognitive-behavioral therapy is effective in treating mild to moderate depression in children and adolescents (SOR A). SSRIs are an adjunctive treatment reserved for treatment of severe depression, and have limited evidence for effectiveness in children and adolescents. Amitriptyline should not be used because of its limited effectiveness and adverse effects (SOR A). Methylphenidate is used for treating attention deficit disorder, not depression. Divalproex sodium is used to treat bipolar disorder. |
|
|
A 55-year-old hospitalized white male with a history of rheumatic aortic and mitral valve disease has a 3-day history of fever, back pain, and myalgias. No definite focus of infection is found on your initial examination. His WBC count is 24,000/mm3(N 4300–10,800) with 40% polymorphonuclear leukocytes and 40% band forms. The following day, two blood cultures have grown gram-positive cocci in clusters.
Until the specific organism sensitivity is known, the most appropriate antibiotic treatment would be: |
vancomycin and gentamicin
This patient has endocarditis caused by a gram-positive coccus. Until sensitivities of the organism are known, treatment should include intravenous antibiotic coverage for Enterococcus, Streptococcus, and methicillin-sensitive and methicillin-resistant Staphylococcus. A patient who does not have a prosthetic valve should be started on vancomycin and gentamicin, with monitoring of serum levels. Enterococcus and methicillin-resistant Staphylococcus are often resistant to cephalosporins. If the organism proves to be Staphylococcus sensitive to nafcillin, the patient can be switched to a regimen of nafcillin and gentamicin. |
|
|
A 40-year-old white female lawyer sees you for the first time. When providing a history, she describes several problems, including anxiety, sleep disorders, fatigue, persistent depressed mood, and decreased libido. These symptoms have been present for several years and are worse prior to menses, although they also occur to some degree during menses and throughout the month. Her menstrual periods are regular for the most part.
The most likely diagnosis at this time is: |
dysthymia
Psychological disorders, including anxiety, depression, and dysthymia, are frequently confused with premenstrual syndrome (PMS), and must be ruled out before initiating therapy. Symptoms are cyclic in true PMS. The most accurate way to make the diagnosis is to have the patient keep a menstrual calendar for at least two cycles, carefully recording daily symptoms. Dysthymia consists of a pattern of ongoing, mild depressive symptoms that have been present for 2 years or more and are less severe than those of major depression. This diagnosis is consistent with the findings in the patient described here. |
|
|
A mother brings her 2-month-old infant to the emergency department because of profuse vomiting and severe diarrhea. The infant is dehydrated, has a cardiac arrhythmia, appears to have ambiguous genitalia, and is in distress.
This presentation suggests a diagnosis of: |
congenital adrenal hyperplasia
Congenital adrenal hyperplasia is a family of diseases caused by an inherited deficiency of any of the enzymes necessary for the biosynthesis of cortisol. In patients with the salt-losing variant, symptoms begin shortly after birth with failure to regain birth weight, progressive weight loss, and dehydration. Vomiting is prominent, and anorexia is also present. Disturbances in cardiac rate and rhythm may occur, along with cyanosis and dyspnea. In the male, various degrees of hypospadias may be seen, with or without a bifid scrotum or cryptorchidism. |
|
|
A 62-year-old African-American female undergoes a workup for pruritus. Laboratory findings include a hematocrit of 55.0% (N 36.0–46.0) and a hemoglobin level of 18.5 g/dL (N 12.0–16.0).
What additional findings would help establish the diagnosis of polycythemia vera? |
A platelet count >400,000/mm3
Polycythemia vera should be suspected in African-Americans or white females whose hemoglobin level is >16 g/dL or whose hematocrit is >47%. For white males, the thresholds are 18 g/dL and 52%. It should also be suspected in patients with portal vein thrombosis and splenomegaly, with or without thrombocytosis and leukocytosis. Major criteria include an increased red cell mass, a normal O2 saturation,and the presence ofsplenomegaly. Minor criteria includeelevated vitamin B 12 levels, elevated leukocyte alkaline phosphatase, a platelet count >400,000/mm3 and a WBC count >12,000/mm3 . Patients with polycythemia vera may present with gout and an elevated uric acid level, but neither is considered a criterion for the diagnosis. |
|
|
Over the last 6 months a developmentally normal 12-year-old white female has experienced intermittent abdominal pain, which has made her quite irritable. She also complains of joint pain and general malaise. She has lost 5 kg (11 lb) and has developed an anal fissure.
What is the most likely cause of these symptoms? |
Crohn’s disease
The most common age of onset for inflammatory bowel disease is during adolescence and young adulthood, with a second peak at 50–80 years of age. The manifestations of Crohn’s disease are somewhat dependent on the site of involvement, but systemic signs and symptoms are more common than with ulcerative colitis. Perianal disease is also common in Crohn’s disease. Irritable colon and other functional bowel disorders may mimic symptoms of Crohn’s disease, but objective findings of weight loss and anal lesions are extremely uncommon. This is also true for viral hepatitis and giardiasis. In addition, the historical and epidemiologic findings in this case are not consistent with either of these infections. Celiac disease and giardiasis can produce Crohn’s-like symptoms of diarrhea and weight loss, but are not associated with anal fissures. |
|
|
Which one of the following is considered first-line therapy for nausea and vomiting of pregnancy?
|
Vitamin B6
A number of alternative therapies have been used for problems related to pregnancy, although vigorous studies are not always possible. For nausea and vomiting, however, vitamin B6 is considered first-line therapy, sometimes combined with doxylamine. Other measures that have been found to be somewhat useful include ginger and acupressure. |
|
|
A 45-year-old female presents to your office because she has had a lump on her neck for the past 2 weeks. She has no recent or current respiratory symptoms, fever, weight loss, or other constitutional symptoms. She has a history of well-controlled hypertension, but is otherwise healthy. On examination you note a nontender, 2-cm, soft node in the anterior cervical chain. The remainder of the examination is unremarkable.
What would be most appropriate at this point? |
Monitoring clinically for 4–6 weeks, then a biopsy if the node persists or enlarges
There is limited evidence to guide clinicians in the management of an isolated, enlarged cervical lymph node, even though this is a common occurrence. Evaluation and management is guided by the presence or absence of inflammation, the duration and size of the node, and associated patient symptoms. In addition, the presence of risk factors for malignancy should be taken into account. Immediate biopsy is warranted if the patient does not have inflammatory symptoms and the lymph node is >3 cm, if the node is in the supraclavicular area, or if the patient has coexistent constitutional symptoms such as night sweats or weight loss. Immediate evaluation is also indicated if the patient has risk factors for malignancy. Treatment with antibiotics is warranted in patients who have inflammatory symptoms such as pain, erythema, fever, or a recent infection. In a patient with no risk factors for malignancy and no concerning symptoms, monitoring the node for 4–6 weeks is recommended. If the node continues to enlarge or persists after this time, then further evaluation is indicated. This may include a biopsy or imaging with CT or ultrasonography. The utility of serial ultrasound examinations to monitor lymph nodes has not been demonstrated. |
|
|
A 45-year-old male is seen in the emergency department with a 2-hour history of substernal chest pain. An EKG shows an ST-segment elevation of 0.3 mV in leads V4–V6.
In addition to evaluation for reperfusion therapy, which one of the following would be appropriate? |
Oral clopidogrel (Plavix)
This patient has an ST-segment elevation myocardial infarction (STEMI). STEMI is defined as an ST-segment elevation of greater than 0.1 mV in at least two contiguous precordial or adjacent limb leads. The most important goal is to begin fibrinolysis less than 30 minutes after the first contact with the health system. The patient should be given oral clopidogrel, and should also chew 162–325 mg of aspirin. Enteric aspirin has a delayed effect. Intravenous β-blockers such as metoprolol should not be routinely given, and warfarin is not indicated. Delaying treatment until cardiac enzyme results are available in a patient with a definite myocardial infarction is not appropriate. |
|
|
You see a 68-year-old mechanic for a routine evaluation. He has a 2-year history of hypertension. His weight is normal and he adheres to his medication regimen. His current medications are metoprolol (Lopressor), 100 mg twice daily; olmesartan (Benicar), 40 mg/day; and hydrochlorothiazide, 25 mg/day. His serum glucose levels have always been normal, but his lipid levels are elevated.
A physical examination is unremarkable except for an enlarged prostate and a blood pressure of 150/94 mm Hg. Laboratory studies show a serum creatinine level of 1.6 mg/dL (N 0.6–1.5) and a serum potassium level of 4.9 mmol/L (N 3.5–5.0). The patient’s record shows blood pressures ranging from 145/80 mm Hg to 148/96 mm Hg over the past year. What would be the appropriate next step at this point? |
Substitute furosemide (Lasix) for hydrochlorothiazide
Resistant or refractory hypertension is defined as a blood pressure ≥140/90 mm Hg, or ≥130/80 mm Hg in patients with diabetes mellitus or renal disease (i.e., with a creatinine level >1.5 mg/dL or urinary protein excretion >300 mg over 24 hours), despite adherence to treatment with full doses of at least three antihypertensive medications, including a diuretic. JNC 7 guidelines suggest adding a loop diuretic if serum creatinine is >1.5 mg/dL in patients with resistant hypertension. |
|
|
Actinic keratoses of the skin may progress to:
|
squamous cell cancer
Actinic keratoses are scaly lesions that develop on sun-exposed skin, and are believed to be carcinoma in situ. While most actinic keratoses spontaneously regress, others progress to squamous cell cancers. |
|
|
A 52-year-old male presents with a small nodule in his palm just proximal to the fourth metacarpophalangeal joint. It has grown larger since it first appeared, and he now has mild flexion of the finger, which he is unable to straighten. He reports that his father had similar problems with his fingers. On examination you note pitting of the skin over the nodule.
The most likely diagnosis is: |
Dupuytren’s contracture
Dupuytren’s contracture is characterized by changes in the palmar fascia, with progressive thickening and nodule formation that can progress to a contracture of the associated finger. The fourth finger is most commonly affected. Pitting or dimpling can occur over the nodule because of the connection with the skin. Degenerative joint disease is not associated with a palmar nodule. Trigger finger is related to the tendon, not the palmar fascia, and causes the finger to lock and release. Ganglions also affect the tendons or joints, are not located in the fascia, and are not associated with contractures. Flexor tenosynovitis, an inflammation, is associated with pain, which is not usually seen with Dupuytren’s contracture. |
|
|
Which one of the following is NOT considered a first-line treatment for head lice?
A. Lindane 1% B. Malathion 0.5% (Ovide) C. Permethrin 1% (Nix) D. Pyrethrins 0.33%/pipernyl butoxide 4% (RID) |
Lindane 1%
Lindane’s efficacy has waned over the years and it is inconsistently ovicidal. Because of its neurotoxicity, lindane carries a black box warning and is specifically recommended only as second-line treatment by the FDA. Pyrethroid resistance is widespread, but permethrin is still considered to be a first-line treatment because of its favorable safety profile. The efficacy of malathion is attributed to its triple action with isopropyl alcohol and terpineol, likely making this a resistance-breaking formulation. The probability of simultaneously developing resistance to all three substances is small. Malathion is both ovicidal and pediculicidal. |
|
|
What food is a frequent cause of cross-reactive food-allergy symptoms in latex-allergic individuals?
|
Avocadoes
The majority of patients who are latex-allergic are believed to develop IgE antibodies that cross-react with some proteins in plant-derived foods. These food antigens do not survive the digestive process, and thus lack the capacity to sensitize after oral ingestion in the traditional food-allergy pathway. Antigenic similarity with proteins present in latex, to which an individual has already been sensitized, results in an indirect allergic response limited to the exposure that occurs prior to alteration by digestion, localized primarily in and around the oral cavity. The frequent association with certain fruits has been labeled the “latex-fruit syndrome.” Although many fruits and vegetables have been implicated, fruits most commonly linked to this problem are bananas, avocadoes, and kiwi. |
|
|
A 42-year-old female is found to have a thyroid nodule during her annual physical examination. Her TSH level is normal. Ultrasonography of her thyroid gland shows a solitary nodule measuring 1.2 cm.
What is the most appropriate next step at this point? |
A fine-needle aspiration biopsy of the nodule
All patients who are found to have a thyroid nodule on a physical examination should have their TSH measured. Patients with a suppressed TSH should be evaluated with a radionuclide thyroid scan; nodules that are “hot” (show increased isotope uptake) are almost never malignant and fine-needle aspiration biopsy is not needed. For all other nodules, the next step in the workup is a fine-needle aspiration biopsy to determine whether the lesion is malignant (SOR B). |
|
|
Treatment with donepezil (Aricept) is associated with an increased risk for :
|
bradycardia requiring pacemaker implantation
A large population study has established a significant increased risk of bradycardia, syncope, and pacemaker therapy with cholinesterase inhibitor therapy. Elevation of liver enzymes with the potential for hepatic dysfunction has been seen with tacrine, but it has not been noted with the other approved cholinesterase inhibitors. Cataract formation and thrombosis with pulmonary embolism do not increase with this therapy. Although improvement in mental function is often marginal with cholinesterase inhibitor therapy, the therapy has not been shown to increase the need for institutionalization. |
|
|
An 8-year-old female is brought to your office with a 3-day history of bilateral knee pain. She has had no associated upper respiratory symptoms. On examination she is afebrile. Her knees have full range of motion and no effusion, but she has a purpuric papular rash on both lower extremities.
What is the most likely cause of her symptoms? |
Henoch-Schönlein purpura
The combination of arthritis with a typical palpable purpuric rash is consistent with a diagnosis of Henoch-Schönlein purpura. This most often occurs in children from 2 to 8 years old. Arthritis is present in about two-thirds of those affected. Gastrointestinal and renal involvement are also common. Rocky Mountain spotted fever presents with a rash, but arthralgias are not typical. These patients are usually sick with a fever and headache. Juvenile rheumatoid arthritis is associated with a salmon-pink maculopapular rash, but not purpura. The rash associated with Lyme disease is erythema migrans, which is a bull’s-eye lesion at the site of a tick bite. The rash associated with rheumatic fever is erythema marginatum, which is a pink, raised, macular rash with sharply demarcated borders. |
|
|
What hospitalized patients are the most appropriate candidate for thromboembolism prophylaxis with enoxaparin (Lovenox)?
|
example: A 67-year-old female with hemiparesis, admitted for community-acquired pneumonia
Venous thromboembolism is a frequent cause of preventable death and illness in hospitalized patients. Approximately 10%–15% of high-risk patients who do not receive prophylaxis develop venous thrombosis. Pulmonary embolism is thought to be associated with 5%–10% of deaths in hospitalized patients. Anticoagulant prophylaxis significantly reduces the risk of pulmonary embolism and should be used in all high-risk patients. Prophylaxis is generally recommended for patients over the age of 40 who have limited mobility for 3 days or more and have at least one of the following risk factors: acute infectious disease, New York Heart Association class III or IV heart failure, acute myocardial infarction, acute respiratory disease, stroke, rheumatic disease, inflammatory bowel disease, previous venous thromboembolism, older age (especially >75 years), recent surgery or trauma, immobility or paresis, obesity (BMI >30 kg/m2), central venouscatheterization, inherited or acquired thrombophilic disorders, varicose veins, or estrogen therapy. Pharmacologic therapy with an anticoagulant such as enoxaparin is clearly indicated in the 67-year-old who has limited mobility secondary to hemiparesis and is being admitted for an acute infectious disease. The patient on chronic anticoagulation, the patient with severe thrombocytopenia, and the patient with coagulopathy are at high risk for bleeding if given anticoagulants, and are better candidates for nonpharmacologic therapies such as foot extension exercises, graduated compression stockings, or pneumatic compression devices. Although the 22-year-old is obese and recently had surgery, his young age and ambulatory status make anticoagulant prophylaxis less necessary. |
|
|
A 25-year-old white male who has a poorly controlled major seizure disorder and a 6-week history of recurrent fever, anorexia, and persistent, productive coughing visits your office. On physical examination he is noted to have a temperature of 38.3°C (101.0°F), a respiratory rate of 16/min, gingival hyperplasia, and a fetid odor to his breath. Auscultation of the lungs reveals rales in the mid-portion of the right lung posteriorly.
What is most likely to be found on a chest radiograph? |
A lung abscess
Anaerobic lung abscesses are most often found in a person predisposed to aspiration who complains of a productive cough associated with fever, anorexia, and weakness. Physical examination usually reveals poor dental hygiene, a fetid odor to the breath and sputum, rales, and pulmonary findings consistent with consolidation. Patients who have sarcoidosis usually do not have a productive cough and have bilateral physical findings. A persistent productive cough is not a striking finding in disseminated tuberculosis, which would be suggested by miliary calcifications on a chest film. The clinical presentation and physical findings are not consistent with a simple mass in the right hilum nor with a right pleural effusion. |
|
|
What medication should be given intravenously in the initial treatment of status epilepticus?
|
Lorazepam (Ativan)
Status epilepticus refers to continuous seizures or repetitive, discrete seizures with impaired consciousness in the interictal period. It is an emergency and must be treated immediately, since cardiopulmonary dysfunction, hyperthermia, and metabolic derangement can develop, leading to irreversible neuronal damage. Lorazepam, 0.1–0.15 mg/kg intravenously, should be given as anticonvulsant therapy after cardiopulmonary resuscitation. This is followed by phenytoin, given via a dedicated peripheral intravenous line. Fosphenytoin, midazolam, or phenobarbital can be used if there is no response to lorazepam. Propofol has been used for refractory status epilepticus to induce general anesthesia when the initial drugs have failed, but reports of fatal propofol infusion syndrome have led to a decline in its use. |
|
|
According to JNC 7, the risk of cardiovascular disease begins to increase when the systolic blood pressure exceeds a threshold of :
|
115 mm Hg
According to JNC 7, the risk of both ischemic heart disease and stroke increases progressively when systolic blood pressure exceeds 115 mm Hg and diastolic blood pressure exceeds 75 mm Hg. |
|
|
How does an anterior shoulder dislocation present differently than a posterior shoulder dislocation?
|

|
|
|
What is the treatment for an acute shoulder dislocation presenting to the ER?
|

|
|
|
A 56-year-old female has been on combined continuous hormone therapy for 6 years. This is associated with a reduced risk for ?
|
Bone fracture
Hormone replacement therapy that includes estrogen has been shown to decrease osteoporosis and bone fracture risk. The risk for colorectal cancer also is reduced after 5 years of estrogen use. The risk for myocardial infarction, stroke, breast cancer, and venous thromboembolism increases with long-term use. |
|
|
A 2-week-old female is brought to the office for a well child visit. The physical examination is completely normal except for a clunking sensation and feeling of movement when adducting the hip and applying posterior pressure. Which one of the following would be the most appropriate next step?
|
Referral for orthopedic consultation
Developmental dysplasia of the hip encompasses both subluxation and dislocation of the newborn hip, as well as anatomic abnormalities. It is more common in firstborns, females, breech presentations, oligohydramnios, and patients with a family history of developmental dysplasia. Experts are divided with regard to whether hip subluxation can be merely observed during the newborn period, but if there is any question of a hip problem on examination by 2 weeks of age, the recommendation is to refer to a specialist for further testing and treatment. Studies show that these problems disappear by 1 week of age in 60% of cases, and by 2 months of age in 90% of cases. Triple diapering should not be used because it puts the hip joint in the wrong position and may aggravate the problem. Plain radiographs may be helpful after 4-6 months of age, but prior to that time the ossification centers are too immature to be seen. Because the condition can be difficult to diagnose, and can result in significant problems, the current recommendation is to treat all children with developmental dysplasia of the hip. Closed reduction and immobilization in a Pavlik harness, with ultrasonography of the hip to ensure proper positioning, is the treatment of choice until 6 months of age. The American Academy of Pediatrics recommends ultrasound screening at 6 weeks for breech girls, breech boys (optional), and girls with a positive family history of developmental dysplasia of the hip. Other countries have recommended universal screening, but a review of the literature has not shown that the benefits of early diagnosis through universal screening outweigh the risks and potential problems of overtreating. |
|
|
A 55-year-old overweight male presents with a complaint of pain in the left big toe. He recently started jogging 2 miles a day to try to lose weight, but has not changed his diet and says he drinks 4 cans of beer every night. The pain has developed gradually over the last 2 weeks and is worse after running. An examination shows a normal foot with tenderness and swelling of the medial plantar aspect of the left first metatarsophalangeal joint. Passive dorsiflexion of the toe causes pain in that area. Plantar flexion produces no discomfort, and no numbness can be appreciated. Which one of the following is the most likely diagnosis?
|
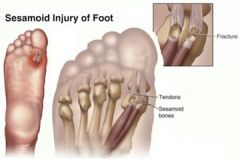
Sesamoid fracture
Pain involving the big toe is a common problem. The first metatarsophalangeal (MTP) joint has two sesamoid bones, and injuries to these bones account for 12% of big-toe injuries. Overuse, a sharp blow, and sudden dorsiflexion are the most common mechanisms of injury. Gout commonly involves the first MTP joint, but the onset is sudden, with warmth, redness, and swelling, and pain on movement of the joint is common. Morton’s neuroma commonly occurs between the third and fourth toes, causes numbness involving the digital nerve in the area, and usually is caused by the nerve being pinched between metatarsal heads in the center of the foot. Cellulitis of the foot is common, and can result from inoculation through a subtle crack in the skin. However, there would be redness and swelling, and the process is usually more generalized. Sesamoiditis is often hard to differentiate from a true sesamoid fracture. Radiographs should be obtained, but at times they are nondiagnostic. Treatment, fortunately, is similar, unless the fracture is open or widely displaced. Limiting weight bearing and flexion to control discomfort is the first step. More complex treatments may be needed if the problem does not resolve in 4-6 weeks. |
|
|
A mother brings in her 2-month-old infant for a routine checkup. The baby is exclusively breastfed, and the mother has no concerns or questions. Which one of the following would you recommend at this time in addition to continued breastfeeding?
|
Vitamin D supplementation
Although breast milk is the ideal source of nutrition for healthy term infants, supplementation with 200 IU/day of vitamin D is recommended beginning at 2 months of age and continuing until the child is consuming at least 500 mL/day of formula or milk containing vitamin D (SOR B). The purpose of supplementation is to prevent rickets. Unless the baby is anemic or has other deficiencies, neither iron nor a multivitamin is necessary. Parents often mistakenly think babies need additional water, which can be harmful because it decreases milk intake and can cause electrolyte disturbances. Cereal should not be started until 4 to 6 months of age. |
|
|
A 62-year-old white male complains of fatigue and proximal extremity discomfort without any localized joint pain. Which condition is associated with a consistently normal creatine kinase enzyme level at all phases of disease?
|
Polymyalgia rheumatica (PMR)
Polymyalgia rheumatica is a disease of the middle-aged and elderly. Discomfort is common in the neck, shoulders, and hip girdle areas. There is an absence of objective joint swelling, and findings tend to be symmetric. Characteristically, the erythrocyte sedimentation rate and C-reactive protein levels are significantly elevated; however, these tests are nonspecific. Occasionally there are mild elevations of liver enzymes, but muscle enzymes, including creatine kinase, are not elevated in this disorder. Elevation of muscle enzymes strongly suggests another diagnosis. Polymyositis and dermatomyositis are associated with variable levels of muscle enzyme elevations during the active phases of the disease. Drug-induced myopathies such as those seen with the cholesterol-lowering statin medications tend to produce some elevation of muscle enzymes during the course of the disorder. Hypothyroidism is associated with creatine kinase elevation. It should be strongly considered in the patient with unexplained, otherwise asymptomatic creatine kinase elevation found on a routine chemistry profile. Hyperthyroidism may cause muscle disease and loss of muscle, but it is not associated with creatine kinase elevation. |
|
|
What are the risk factors for osteoarthritis of the hip?
|
Risk factors for osteoarthritis of the hip include obesity, high bone mass, old age, participation in weight-bearing sports, and hypothyroidism.
|
|
|
The daily intake of vitamins and minerals recommended by the Food and Nutrition Board varies according to sex, age, and condition. The recommended daily allowance of vitamin D is greatest for which patient population?
|
A 75-year-old female
The current Dietary Reference Intake (DRI – which has replaced RDA’s) recommendation for vitamin D is 200 IU/day for all women between the ages of 9 and 50 years; pregnancy or lactation does not affect the recommendation. The DRI doubles to 400 IU daily for women age 51-70 and triples to 600 IU daily for women over the age of 70. The maximum daily oral intake of vitamin D thought to be safe is 2000 IU/day for all females over the age of 12 months. |
|
|
In addition to calcium and vitamin D supplementation, patients who are beginning long-term treatment with prednisone (≥3 months at a dosage ≥5 mg/day) should also receive
|
bisphosphonate therapy
The American College of Rheumatology recommends that patients who are beginning long-term treatment with prednisone (≥3 months at a dosage ≥5 mg/day), or an equivalent, receive bisphosphonate therapy in addition to calcium and vitamin D supplementation, regardless of their DEXA-scan T score. The other treatments are not recommended for prevention of glucocorticoid-induced osteoporosis. |
|
|
A 79-year-old male is admitted to the hospital because of a sudden inability to ambulate. He has a past history of gout. On examination his temperature is 38.2°C (100.8°F) and he has bilateral knee effusions. His WBC count is 14,000/mm3 with 82% segs. His serum uric acid level is 8.5 mg/dL (N <6.5). Which one of the following would be most appropriate at this point?
|
Arthrocentesis
Polyarticular arthritis often presents with fever, knee and other joint effusions, and leukocytosis. A 24-hour urine collection is not routine, is difficult for the patient, and typically does not change therapy. Especially in cases where a joint effusion is accompanied by fever, diagnostic arthrocentesis should be performed to help guide therapy. Allopurinol should not be initiated during an acute gouty attack, but may be started after a patient has recovered. Diuretics increase uric acid levels. |
|
|
An overweight 13-year-old male presents with a 3-week history of right lower thigh pain. He first noticed the pain when jumping while playing basketball, but now it is present even when he is just walking. On examination he can bear his full weight without an obvious limp. There is no localized tenderness, and the patella tracks normally without subluxation. Internal rotation of the hip is limited on the right side compared to the left. Based on the examination alone, which one of the following is the most likely diagnosis?
|
Slipped capital femoral epiphysis
This is a classic presentation for slipped capital femoral epiphysis (SCFE) in an adolescent male who has probably had a recent growth spurt. Pain with activity is the most common presenting symptom, as opposed to the nighttime pain that is typical of malignancy. Obese males are affected more often. The pain is typically in the anterior thigh, but in a high percentage of patients the pain may be referred to the knee, lower leg, or foot. Limited internal rotation of the hip, especially with the hip in 90°; flexion, is a reliable and specific finding for SCFE and should be looked for in all adolescents with hip, thigh, or knee pain. Meralgia paresthetica is pain in the thigh related to entrapment of the lateral femoral cutaneous nerve, often attributed to excessively tight clothing. Legg-Calvé-Perthes disease (avascular or aseptic necrosis of the femoral head) is more likely to occur between the ages of 4 and 8 years. Juvenile rheumatoid arthritis typically is associated with other constitutional symptoms including stiffness, fever, and pain in at least one other joint, with the pain not necessarily associated with activity. |
|
|
A 70-year-old female consults you about osteoporosis treatment. Two years ago her DEXA scan T score was -2.6, and she began taking risedronate (Actonel), 35 mg/week. Her BMI is 24 kg/m2, she takes appropriate doses of calcium and vitamin D, and she takes walks almost every day. Her current T score is -2.5, and she is concerned about the minimal change in spite of therapy. She has never had a fracture, but asks if more could be done to reduce her fracture risk. Which one of the following would be the most appropriate recommendation?
|
continue current therapy
There is not a linear correlation between bone mineral density and fracture risk. Bone architecture may be changed by bisphosphonate therapy, which may result in a decreased fracture risk. This patient has not had a fracture and is on adequate medical therapy that should be continued. |
|
|
A 36-year-old male presents with pain over the lumbar paraspinal muscles. He says the pain began suddenly while he was shoveling snow. What management recommendations would you give regarding this patients injury?
|
Continued activity rather than bed rest helps speed recovery
Multiple studies have demonstrated that bed rest is detrimental to recovery from low back pain. Patients should be encouraged to remain as active as possible. Exercises designed specifically for the treatment of low back pain have not been shown to be helpful. Neither opioids nor trigger-point injections have shown superiority over placebo, NSAIDs, or acetaminophen in relieving acute back pain. There is no good evidence to suggest that systemic corticosteroids are effective for low back pain with or without sciatica. |
|
|
A 44-year-old African-American female reports diffuse aching, especially in her upper legs and shoulders. The aching has increased, and she now has trouble going up and down stairs because of weakness. She has no visual symptoms, and a neurologic examination is normal except for proximal muscle weakness. Laboratory tests reveal elevated levels of serum creatine kinase and aldolase. Her symptoms improve significantly when she is treated with corticosteroids. Which one of the following is the most likely diagnosis?
|
Polymyositis
The patient described has an inflammatory myopathy of the polymyositis/dermatomyositis group. Proximal muscle involvement and elevation of serum muscle enzymes such as creatine kinase and aldolase are characteristic. Corticosteroids are the accepted treatment of choice. It is extremely unlikely that Duchenne’s muscular dystrophy would present after age 30. In amyotrophic lateral sclerosis, an abnormal neurologic examination with findings of upper motor neuron dysfunction is characteristic. Patients with myasthenia gravis characteristically have optic involvement, often presenting as diplopia. The predominant symptom of aseptic necrosis of the femoral head is pain rather than proximal muscle weakness. |
|
|
You see a 5-year-old white female with in-toeing due to excessive femoral anteversion. She is otherwise normal and healthy, and her mobility is unimpaired. Her parents are greatly concerned with the cosmetic appearance and possible future disability, and request that she be treated. You recommend which one of the following?
|
Observation
There is little evidence that femoral anteversion causes long-term functional problems. Studies have shown that shoe wedges, torque heels, and twister cable splints are not effective. Surgery should be reserved for children 8-10 years of age who still have cosmetically unacceptable, dysfunctional gaits. Major complications of surgery occur in approximately 15% of cases, and can include residual in-toeing, out-toeing, avascular necrosis of the femoral head, osteomyelitis, fracture, valgus deformity, and loss of position. Thus, observation alone is appropriate treatment for a 5-year-old with uncomplicated anteversion. |
|
|
Which medication used to treat rheumatoid arthritis can delay the progression of the disease?
|
Hydroxychloroquine (Plaquenil)
Hydroxychloroquine, originally developed as an antimalarial drug, is a well-known disease-modifying agent that can slow the progression of rheumatoid arthritis. Aspirin, indomethacin, and ibuprofen are anti-inflammatory agents. They relieve pain and improve mobility, but do not alter the progression of the disease. Capsaicin, a topical substance-P depleter, can relieve pain symptoms. |
|
|
A 75-year-old white female presents with severe pain of the carpometacarpal joint at the base of her thumb. Examination of her hands also reveals hypertrophic changes of the distal interphalangeal and proximal interphalangeal joints of her fingers. These findings are most consistent with
|
osteoarthritis
Osteoarthritis causes changes predominantly in the proximal interphalangeal (PIP) and distal interphalangeal (DIP) joints of the hands known as Bouchard’s and Heberden’s nodes respectively, and the carpometacarpal joints of the thumbs. While rheumatoid arthritis commonly causes subluxations in the metacarpophalangeal joints, this patient’s hypertrophic changes are most likely due to osteoarthritis. The other choices are less likely to cause this presentation. |
|
|
A 60-year-old male presents with an acute onset of pain and swelling in the right big toe. He can recall no mechanism of injury. He has hypertension which is well controlled with hydrochlorothiazide. On examination the area around the base of the toe is reddened, slightly warm, and very tender on palpation. Which medication should be AVOIDED in this patient at this time?
|
Allopurinol (Zyloprim)
This patient likely has gout. Aspiration should be attempted to get a specific diagnosis. The initial treatment for gout is NSAIDs, colchicine, or cortisone injections (SOR B). Allopurinol should be avoided until the episode of gout is controlled, because it may cause temporary worsening. In addition to medication, recommended management includes addressing risk factors such as obesity, diuretic use, high-purine diet, and alcohol intake (SOR B). |
|
|
A 55-year-old African-American male with osteoarthritis of the knees asks for advice on improving the function of his knees and controlling arthritis pain. Which one of the following would be appropriate advice?
|
A therapeutic exercise program will improve both pain and function
A therapeutic exercise program will reduce both pain and disability in patients with osteoarthritis of the knee (SOR A). There is no evidence to support the use of capsaicin cream, but NSAIDs will reduce pain and there are proven therapies that will improve function of the patients knee. While intra-articular corticosteroids are effective in relieving pain in the short term (up to 4 weeks), there is no evidence for long-term efficacy. There is not good evidence to support the use of glucosamine for treating osteoarthritis of the knee. One systematic review found it no more effective than placebo. |
|
|
An 83-year-old female presents with pain, swelling, and erythema of her left knee. She first noticed this problem last night before going to bed. She is generally healthy and takes no medications. She has not been sexually active since being widowed 15 years ago, and she currently lives with her sister. She states that she developed pain and swelling in her left ankle 2 years ago that lasted only a couple of days and resolved spontaneously. Blood testing shows a very elevated erythrocyte sedimentation rate but a normal rheumatoid factor and uric acid level. What is the most likely diagnosis?
|
Pseudogout (calcium pyrophosphate disease)
Acute monoarthritis in adults is most commonly caused by infection, trauma, or crystal deposition. Rheumatoid arthritis seldom presents as monoarthritis, and more often has a subacute course with multiple, symmetric joints involved. Although osteoporosis may result in a fracture of the knee joint without trauma at this age, there is no reason to believe that this patient has a torn anterior cruciate ligament. Gonococcal arthritis is one of the most common causes of septic arthritis, but is highly unlikely in this elderly, sexually inactive patient. Nongonococcal septic arthritis (especially due to staphylococcal and streptococcal bacteria) is still a consideration and should be ruled out by aspiration of fluid to be sent for culture. This patient's presentation is most consistent with pseudogout. Having a normal uric acid level suggests against gout, but does not rule it out. Also, gout is seven times more likely to be seen in males, whereas pseudogout is 1.5 times more frequent in females. Pseudogout most often affects the elderly, and usually affects the knee, wrist, and ankle. Gout presents most commonly in the first metatarsophalangeal joint and insteps of the feet, but also can occur in the knee, wrist, finger, and olecranon bursa. Differentiating between gout and pseudogout can be difficult and is best done by analysis of joint fluid. In patients with gout, this fluid contains highly negative birefringent, needle-shaped urate crystals, whereas in pseudogout the fluid contains rhomboid-shaped, weakly positive birefringent calcium pyrophosphate crystals. |
|
|
A 35-year-old white female comes to your office with a 3-month history of the gradual onset of pain and tenderness in the wrists and hands. She also complains of 1 hour of morning stiffness. She denies rash, fever, or skin changes. On physical examination she has symmetric swelling of the proximal interphalangeal joints and metacarpophalangeal joints. Motion of these joints is painful. She has no rash or mouth ulcers. Radiographs of the hands and wrists are negative, and a chest film is unremarkable. Her CBC is normal, but the erythrocyte sedimentation rate is elevated at 40 mm/hr. Latex fixation for rheumatoid factor is negative, and an antinuclear antibody (ANA) test is negative. The most likely diagnosis in this patient is:
|
Rheumatoid arthritis
This patient has rheumatoid arthritis (RA) by symptoms and physical findings. A positive latex fixation test for rheumatoid factor is not necessary for the diagnosis. A negative rheumatoid factor does not exclude RA, and a positive rheumatoid factor is not specific. Rheumatoid factor is found in the serum of approximately 85% of adult patients with RA; in subjects without RA, the incidence of positive rheumatoid factor is 1%–5% and increases with age. The ANA test is positive in at least 95% of patients with systemic lupus erythematosus (SLE), but in only about 35% of patients with RA. Elevation of the erythrocyte sedimentation rate is seen in many patients with RA, and the degree of elevation roughly parallels disease activity. A mean of 6 months after the onset of Lyme disease, 60% of patients in the U.S. have brief attacks of asymmetric, oligoarticular arthritis, primarily in the large joints and especially in the knee. |
|
|
A 40-year-old runner complains of gradually worsening pain on the lateral aspect of his foot. He runs on asphalt, and has increased his mileage from 2 miles/day to 5 miles/day over the last 2 weeks. Palpation causes pain over the lateral 5th metatarsal. The pain is also reproduced when he jumps on the affected leg. When you ask about his shoes he tells you he bought them several years ago. What is the most likely diagnosis?
|
Stress fracture
Running injuries are primarily caused by overuse due to training errors. Runners should be instructed to increase their mileage gradually, in increments of 10% or less each week. A stress fracture causes localized tenderness and swelling in superficial bones. Pain is reproduced by jumping on the affected leg. Plantar fasciitis causes burning pain in the heel and there is tenderness of the plantar fascia where it inserts onto the medial tubercle of the calcaneus. |
|
|
What clinical presentation is most consistent with vitamin D deficiency in the aged?
|
Development of chronic bone pain and weakness in association with bone loss
Vitamin D deficiency is being recognized more frequently among the elderly, especially in the nursing home or other settings where inactivity, nutritional deficiency, and lack of sunlight exposure combine to increase the propensity for deficiency. Vitamin D deficiency has been associated with abnormalities in bone metabolism, primarily osteomalacia. Clinically this can present as muscle weakness, limb pain, and impaired physical function. Bleeding gums and fatigue may be presenting symptoms of scurvy (vitamin C deficiency). High-output cardiac failure with vasodilation, dermatitis, and neuropathy is the clinical presentation of thiamine deficiency. The combination of diarrhea, scaly dermatitis, and dementia is one of the clinical presentations of niacin deficiency. |
|
|
An anxious and agitated 18-year-old white male presents to your office with a 2-hour history of severe muscle spasms in the neck and back. He was seen 2 days ago in a local emergency department with symptoms of gastroenteritis, treated with intravenous fluids, and sent home with a prescription for prochlorperazine (Compazine) suppositories. The best therapy for this problem is intravenous administration of:
|
Diphenhydramine (Benadryl)
While rarely life threatening, an acute dystonic reaction can be frightening and painful to the patient and confusing to the treating physician who may be unaware of what medications the patient is taking. Dystonia can be caused by any agent that blocks dopamine, including prochlorperazine, metoclopramide, and typical neuroleptic agents such as haloperidol. The acute treatment of choice is diphenhydramine or benztropine. |
|
|
For several years, a hypertensive 65-year-old female has been treated with hydrochlorothiazide (HydroDIURIL), 25 mg/day; atenolol (Tenormin), 100 mg/day; and hydralazine (Apresoline), 50 mg 4 times/day. Her blood pressure has been well controlled on this regimen. Over the past 2 months she has experienced malaise, along with diffuse joint pains that involve symmetric sites in the fingers, hands, elbows, and knees. A pleural friction rub is noted on examination. Laboratory testing shows that the patient has mild anemia and leukopenia, with a negative rheumatoid factor and a positive antinuclear antibody (ANA) titer of 1:640. What would be the most appropriate INITIAL treatment?
|
Discontinue the hydralazine
There are many drugs that can induce a syndrome resembling systemic lupus erythematosus, but the most common offender is procainamide, followed by hydralazine. There is a genetic predisposition for this drug-induced lupus, determined by drug acetylation rates. Polyarthritis and pleuropericarditis occur in half of patients, but fortunately, CNS and renal involvement are rare. While all patients with this condition have positive ANAs and most have antibodies to histones, antibodies to double-stranded DNA and decreased complement levels are rare, which distinguishes drug-induced lupus from idiopathic lupus. The best initial management is to withdraw the drug, and most patients improve in a few weeks. For those with severe symptoms, a short course of corticosteroids is indicated. Once the offending drug is discontinued, symptoms seldom last beyond 6 months |
|
|
A 37-year-old white female who has had silicone breast implants for 17 years is concerned about the risk of developing joint problems from the implants. You discuss studies concerning risks of connective tissue disease in women who have silicone breast implants and assure her that
|
Assure her that there is no increased risk of connective tissue disease in women with silicone implants
Despite widespread publicity and legal wrangling, a large meta-analysis of women who have had silicone breast implants has produced no evidence of any significant increase in the risk for connective tissue disease in women who have these implants. |
|
|
A high incidence of osteonecrosis of the femoral head occurs with:
A. Femoral neck fractures B. Intertrochanteric fractures C. Subtrochanteric fractures D. Femoral shaft fractures E. Supracondylar femoral fractures |
Femoral neck fractures
Femoral neck fractures disrupt the blood supply to the femoral head, which can lead to osteonecrosis. This does not occur with the other types of fractures. |
|
|
A 3-year-old white female is brought to your office because she is complaining of pain in her right arm. Her mother tells you the pain began after she pulled her daughter by the arm while the girl was fighting with her brother. You examine the child and diagnose “nursemaid’s elbow.” You recommend which intervention?
|
Manipulation of the forearm to reduce radial head subluxation
Subluxation of the radial head (nursemaid’s elbow) is a common childhood orthopedic problem. There is conflicting information in various textbooks on the proper technique to reduce the subluxed radial head. However, a study comparing hyperpronation to supination/flexion found that hyperpronation had a higher success rate. If a fracture is diagnosed, then a sling would be helpful. Neither a wrist splint nor a long arm cast is helpful in this situation. |
|
|
A 91-year-old white male presents with a 6-month history of a painless ulcer on the dorsum of the proximal interphalangeal joint of the second toe. Examination reveals a hallus valgus and a rigid hammer toe of the second digit. His foot has mild to moderate atrophic skin changes and the dorsal and posterior tibial pulses are absent. Appropriate treatment includes:
|
Custom-made shoes to protect the hammer toe
The treatment of foot problems in the elderly is difficult because of systemic and local infirmities, the most limiting being the poor vascular status of the foot. Conservative, supportive, and palliative therapy replaces definitive reconstructive surgical therapy. Surgical correction of a hammer toe and bunionectomy would be disastrous in an elderly patient with a small ulcer and peripheral vascular disease. The correct approach to this patient is to prescribe custom-made shoes and a protective shield with a central aperture of foam rubber placed over the hammer toe. Metatarsal pads are not useful in the treatment of hallux valgus and a rigid hammer toe |
|
|
A 67-year-old female is concerned about osteoporosis. The study of choice for determining whether or not she has osteoporosis is:
|
Dual-energy x-ray absorptiometry (DEXA) of the hip and spine
Dual-energy x-ray absorptiometry (DEXA) of the hip and spine is the method of choice for assessment of bone mineral density. Quantitative CT is the most sensitive method, but results in substantially greater radiation exposure. Plain radiographs are not sensitive enough to diagnose osteoporosis until total bone density has decreased by 50%. The predictive value of DEXA scans and ultrasound examinations of peripheral bones in assessing fracture risk at the hip or vertebrae is not clear. |
|
|
Which one of the following is consistent with spinal stenosis but not herniated vertebral disk?
A. Numbness B. Muscle weakness C. Pain relieved by sitting D. Pain relieved by standing |
Pain relieved by sitting
Causes of low back pain include vertebral disk herniation and spinal stenosis. Numbness and muscle weakness may be present in both. Pain in spinal stenosis is relieved by sitting and aggravated by standing. Pain from a herniated disk is aggravated by sitting and relieved by standing. |
|
|
A 32-year-old white female marathon runner presents with persistent pain and tenderness over the pubic symphysis. With exercise, pain is noted in the lower abdomen and medial thighs. There is no fever. A radiograph shows widening of the pubic symphysis. What is the most likely diagnosis?
|
Osteitis pubis
Osteitis pubis is characterized by the chronic occurrences of pain in the lower abdomen and medial thighs with exercise. It produces tenderness over the pubic symphysis, and widening of the symphysis is often seen on plain radiographs. Pain from osteomyelitis is similar, but usually presents with fever and systemic symptoms, and does not cause widening of the symphysis. A stress fracture of the pubic ramus may occur in distance athletes, but the pain and tenderness are lateral, located over the posterior ramus. Inguinal hernia should not present with symphysis pain. |
|
|
A 75-year-old female presents with a 1-month history of pain in her hips and shoulders bilaterally, accompanied by marked stiffness in the mornings. In addition, she reports a 4-lb weight loss and fatigue. She denies fever, chills, sweats, nausea, vomiting, swallowing disturbances, or changes in bowel habits. She specifically denies any visual symptoms or headache. Her physical examination is unremarkable, except for changes suggestive of osteoarthritis in the knees and hands. Laboratory testing reveals a hemoglobin level of 11.8 g/dL (N 13.0–16.0), a hematocrit of 36% (N 40–45), and an erythrocyte sedimentation rate of 84 mm/hr (N <20). What is the most appropriate management at this point?
|
Begin prednisone, 15 mg daily, with no plans for a temporal artery biopsy
It is generally not considered necessary to refer patients with classic polymyalgia rheumatica for a temporal artery biopsy in the absence of symptoms or signs of giant cell arteritis (e.g., headache, visual complaints, jaw claudication, fever, scalp tenderness, abnormal funduscopic exam). Corticosteroids should be started at relatively low doses (10–20 mg daily) and the patient followed for what should be a rapid clinical response. |
|
|
What is recommended regarding the use of alendronate (Fosamax) for the treatment of osteoporosis in men?
|
Its effectiveness is similar to that seen in women
In men with hypogonadism, testosterone therapy has limited efficacy, and the efficacy of other therapies for osteoporosis in men has not been evaluated. Bisphosphonates, including alendronate, are indicated for treatment of Paget’s disease. They decrease bone pain, decrease bone resorption, and increase new bone formation. The proportion of men whose height decreased by at least 10 mm over a 2-year period was 13% in the placebo group and 3% in the alendronate group. The frequency of adverse gastrointestinal effects in the two groups was similar despite the fact that 36% of the men in the placebo group and 41% of those in the alendronate group reported taking NSAIDs during the study. |
|
|
Which one of the following is associated with a reduced risk of postmenopausal osteoporosis?
A. Corticosteroid use B. Cigarette smoking C. Diuretic use D. Low BMI E. Asian ethnicity |
Diuretic use
Diuretic use is associated with a lower risk of osteoporosis, perhaps due to decreased urinary calcium excretion. Cigarette smoking, low BMI, corticosteroid use, and Asian ethnicity are among the factors associated with increased risk. |
|
|
The most common stress fracture in children involves which bone?
|
Tibia
Tibial fractures are the most common lower extremity stress fractures in both children and adults, accounting for about half of all stress fractures. |
|
|
A 70-year-old white female with osteoporosis sees you for follow-up a few days after an emergency department visit for an acute T12 vertebral compression fracture. The fracture was suspected clinically and on plain films; the diagnosis was confirmed with a bone scan. The emergency department physician prescribed oxycodone (OxyContin) and NSAIDs, but the patient is still experiencing considerable discomfort. In addition to increasing the dosage of oxycodone, which one of the following interventions would you suggest now to reduce the patient’s pain?
|
Calcitonin (Miacalcin)
Calcitonin, either intranasal or subcutaneous, provides pain relief within a few days in many patients with osteoporotic vertebral compression fractures. The remainder of the choices do not provide acute relief. Vertebroplasty/kyphoplasty procedures are generally reserved for cases in which medical management has failed. |
|
|
A 78-year-old white female presents with a 3-day history of lower thoracic back pain. She denies any antecedent fall or trauma, and first noted the pain upon arising. Her description of the pain indicates that it is severe, bilateral, and without radiation to the arms or legs. Her past medical history is positive for hypertension and controlled diabetes mellitus. Her medications include hydrochlorothiazide, enalapril (Vasotec), metformin (Glucophage), and a general multivitamin. She is a previous smoker but does not drink alcohol. She underwent menopause at age 50 and took estrogen for “a few months” for hot flashes. Physical examination reveals her to be in moderate pain with a somewhat stooped posture and mild tenderness over T12–L1. She has negative straight-leg raising and normal lower extremity sensation, strength, and reflexes. Which one of the following is true regarding this patient’s likely condition?
|
Subcutaneous or intranasal calcitonin (Calcimar, Miacalcin) may be very helpful for pain relief
The patient described has a classic presentation of an osteoporotic vertebral compression fracture. The diagnosis should be confirmed with a plain radiograph. Treatment is basically symptomatic, with a period of bed rest as short as possible (to avoid complications of immobility), pain medication, and bracing. Salmon calcitonin (injectable or intranasal) is often helpful in providing pain relief. Long-term management of underlying osteoporosis may help prevent future fractures. |
|
|
A 59-year-old female with type 2 diabetes develops a 2x1-cm ulcer on the plantar aspect of her right foot. The ulcer is very deep and there is surrounding cellulitis. A plain film is normal. Which one of the following would be the imaging study of choice to rule out osteomyelitis in this patient?
|
An MRI scan
Although leukocyte scans are sensitive for the diagnosis of foot ulcers, MRI is now considered the imaging study of choice when osteomyelitis is suspected; the sensitivity and specificity of MRI in diabetic patients are 90% or greater. |
|
|
A 38-year-old male is admitted to the hospital after being found lying on the floor unconscious from a drug overdose. The next morning, he is alert and complains of constant pain in the anterior aspect of his left leg. On examination, you note pain with passive stretching, pain with palpation anteriorly, and a slightly decreased dorsalis pedis pulse on the left. There is no edema or erythema. Radiographs of the lower extremity are normal. What should you do now?
|
Obtain immediate surgical consultation
The patient has a history and symptoms very suggestive of a compartment syndrome of the anterior compartment of the left leg. A common cause of this serious problem is limb compression during prolonged recumbency related to drug or alcohol overdose. Early diagnosis and treatment are essential in order to avoid permanent, severe disability. The five “P’s” of compartment syndrome are pain, pallor, paresthesias, pulselessness, and paralysis. If distal pulses are reduced, then muscle necrosis has occurred and immediate surgical consultation is necessary. Duplex doppler ultrasonography and impedance plethysmography are used to evaluate for deep venous thrombosis. Given the decreased pulses, however, this diagnosis is much less likely and such testing may needlessly delay urgent surgical treatment. Intravenous antibiotics would be appropriate for cellulitis. This diagnosis is unlikely in this scenario given the absence of fever, erythema, and edema, and the presence of a diminished pulse. Rest, ice, and elevation are inappropriate treatment modalities for compartment syndrome. |
|
|
A football player sustains a finger injury in a preseason scrimmage. He reports getting his finger caught in another team member’s jersey. His right ring finger is tender on the volar surface, and is swollen around the distal interphalangeal joint. He is unable to flex at the distal interphalangeal joint, but can flex at the proximal interphalangeal joint and at the metacarpophalangeal joint. Radiographs do not show any bony abnormality. You would now:
|
Splint his finger in a slightly flexed position and urgently refer him to a hand surgeon
This injury is commonly called jersey finger. It is a tendinous rupture, sometimes with a bony avulsion fracture of the flexor digitorum profundus tendon. The tendon usually retracts, which makes nonsurgical treatment unlikely to result in complete healing. Splinting in hyperextension will distract the two ends of the tendon and it will not heal. A cast or flexion splint is unlikely to lend itself to complete healing because the tendon ends are unlikely to reattach to each other. |
|
|
A 28-year-old white female complains of fatigue, stiffness, and a diffuse aching in her neck, shoulders, and back for several months. She is not sleeping well. A thorough physical examination is unremarkable except for tenderness over the upper trapezius, second costochondral junctions, lateral epicondyles, and medial knees. A CBC, erythrocyte sedimentation rate, and rheumatoid factor are unremarkable. What is the most appropriate management at this time?
|
Prescribe amitriptyline (Elavil), 10–25 mg every night at bedtime, along with exercise aimed at improving her overall level of fitness
This patient has a classic presentation of fibrositis-fibromyalgia syndrome. In addition to small bedtime doses of amitriptyline or cyclobenzaprine, symptoms are improved by an increase in physical fitness, stress reduction, regulation of sleep schedules, and reassurance. Opiate analgesics and sedative-hypnotics are not recommended for long-term treatment of this disorder. |
|
|
A 2-year-old white male is seen for a well care visit. His mother is concerned because he is not yet able to walk. The routine physical examination, including an orthopedic evaluation, is unremarkable. Speech and other developmental landmarks seem normal for his age. Which tests would be most appropriate?
|
A serum creatine kinase level
The diagnosis of Duchenne’s muscular dystrophy, the most common neuromuscular disorder of childhood, is usually not made until the affected individual presents with an established gait abnormality at age 4–5. By then, parents unaware of the X-linked inheritance may have had additional children who would also be at risk. The disease can be diagnosed earlier by testing for elevated creatine kinase in boys who are slow to walk. The mean age for walking in affected boys is 17.2 months, whereas over 75% of normal children in the United States walk by 13.5 months. Massive elevation of creatine kinase (CK) from 20 to 100 times normal occurs in every young infant with the disease. Early detection allows appropriate genetic counseling regarding future pregnancies. Hypothyroidism and phenylketonuria could present as delayed walking. However, these diseases cause significant mental retardation and would be associated with global developmental delay. Furthermore, these disorders are now diagnosed in the neonatal period by routine screening. Disorders of amino acid metabolism present in the newborn period with failure to thrive, poor feeding, and lethargy. Gross chromosomal abnormalities would usually be incompatible with a normal physical examination at 18 months. |
|
|
A 74-year-old African-American female has moderately severe pain due to osteoarthritis. However, she is also on medication for a seizure disorder. When choosing medications to manage her chronic pain, which one of the following should be used with caution because of her history of seizures?
|
Tramadol (Ultram)
According to the American Geriatrics Society 2002 clinical practice guidelines for management of persistent pain in older persons, tramadol has efficacy and safety similar to those of equianalgesic doses of codeine and hydrocodone. However, because of the threat of seizures (rare but potential), tramadol should be used with caution in patients with a history of seizure disorder or those taking other medications that lower seizure thresholds. |
|
|
A 79-year-old white male with a previous history of prostate cancer has a lumbar spine film suggesting osteopenia. Subsequent bone density studies show a T score of –2.7. What would be appropriate therapy?
|
Alendronate (Fosamax)
The only approved treatments for male osteoporosis are alendronate and recombinant parathyroid hormone. Several drugs have been tested in clinical trials, and more pharmacologic treatments should become available in the future as male osteoporosis is increasingly recognized. Testosterone should not be used in this patient because of his history of prostate cancer. |
|
|
A 28-year-old white male comes to your office complaining of pain in the right wrist since falling 2 weeks ago. On examination, he is tender in the anatomic snuffbox. A radiograph reveals a fracture of the proximal one-third of the carpal navicular bone (scaphoid).What is the most appropriate management at this time?
|
A thumb spica cast
Fracture of the scaphoid should be suspected in every “sprained wrist” where there is tenderness in the anatomic snuffbox. Radiographs may be negative initially. The scaphoid circulation enters the bone for the most part through the distal half. Fractures through the proximal third tend to cause loss of circulation and are slower to heal, and should be referred to an orthopedist because of the risk of nonunion and avascular necrosis. Fractures through the middle or distal one-third can be handled by the family physician in consultation with an orthopedist. The fracture is treated with a thumb spica cast for 10–12 weeks. A wrist splint does not provide adequate immobilization. A bone scan is unnecessary, and physical therapy is inappropriate. If there is still no evidence of union after 10 weeks of immobilization, the patient should be referred to an orthopedist for further care. |
|
|
A 22-year-old male has acute low back pain without paresthesias or other neurologic signs. There is no lower extremity weakness. Which treatment has been shown to be of most benefit initially?
|
Resumption of physical activity as tolerated
Recent studies have shown superior benefits to allowing patients with acute low back pain, without sciatic involvement, to return to normal activities as tolerated. This was better than either bed rest or a back exercise program. Injections would be considered only if conservative therapy fails. |
|
|
A 10-year-old male is brought to your office after sustaining a fall on an outstretched hand. Radiographs show a nondisplaced fracture of the middle third of the clavicle. Appropriate management would include:
|
A figure-of-8 splint or sling support
In treating the midshaft clavicular fracture, the goal is reduction of motion at the fracture site. This rarely requires operative intervention and can be managed by the family physician without orthopedic referral. The fracture site is best stabilized by restricting shoulder motion to less than 45 degree abduction. Either an arm sling or a figure-of-8 clavicular splint holding the shoulder back at the "position of attention" may be used. The figure-of-8 splint offers the advantage of leaving the elbow and hand free for activity. Ice and analgesics are used as needed during the acute stage of injury. Early use of heat may increase the inflammatory response. The patient may use the arm as pain permits, but should not abduct the arm more than 45 degrees for several weeks. The risk of adhesive capsulitis is negligible in children. Repeat radiographs at each follow-up office visit are not necessary, but a final radiograph should be ordered when clinical union has occurred to assess callus formation. |
|
|
A 20-year-old white male presents to your office after a fall on an outstretched hand while skateboarding. He has pain at the anatomic snuffbox with no abrasion. Radiographs are negative. What would be the most appropriate management?
|
A thumb spica splint and follow-up radiographs in 2 weeks
This is a classic presentation of a possible scaphoid fracture. This fracture is important to diagnose and treat appropriately because of a high rate of non-union. If radiographs are negative, the patient should be placed in a thumb spica splint and have repeat radiographs in 2 weeks, because initial studies may be negative. An Ace bandage or a sugar tong splint would be inappropriate because they do not immobilize the thumb. A long arm cast for 8 weeks would immobilize the thumb, but could lead to loss of function, and may overtreat the injury if it is not truly a scaphoid fracture. |
|
|
A 72-year-old white male with known coronary artery disease complains of pain in his back and legs which is increased by standing and walking and relieved by sitting. On examination, deep tendon reflexes in his legs are 0 to 1+ bilaterally. He has mild muscle weakness of his quadriceps and 1+ pedal pulses. He is taking ibuprofen, 800 mg three times a day, and using a back brace without much relief. What would be most likely to relieve his symptoms?
|
Posterior spinal decompression surgery
This patient’s symptoms are typical of spinal stenosis, as they are present when he is standing and relieved by sitting. He has already failed a trial of NSAIDs and bracing. Spinal decompression surgery is now indicated. Epidural corticosteroid injection might be helpful, but not trigger-point injections. Oral corticosteroids would be helpful if he had a herniated disc. Sympathectomy and bypass surgery are treatments for vascular occlusion. |
|
|
A 62-year-old white male comes to your office with pain and swelling of the left great toe at the metatarsophalangeal joint. Examination shows it is erythematous, warm, swollen, and tender to touch. The patient has a history of diabetes mellitus controlled by diet, and hypertension. His medications include hydrochlorothiazide, 25 mg/day. A CBC and blood chemistry profile are normal, except for a uric acid level of 9.2 mg/dL (N 3.6–8.5). Which one of the following is true in this situation?
|
Stopping the hydrochlorothiazide may control the hyperuricemia
This is a typical presentation for gout. Elevated uric acid levels are not necessary for the diagnosis, as there are some patients with normal uric acid levels who still have gout. Conversely, hyperuricemia does not establish the diagnosis of gout. Risk factors for the development of gout include several enzyme deficiencies, renal insufficiency, hypertension, obesity, moonshine ingestion (causing lead exposure), and alcohol abuse. There are several medications that elevate uric acid, including diuretics, low-dose salicylates, niacin, cyclosporine, ethambutol, and pyrazinamide. A typical gout attack such as the one described will resolve spontaneously within 2 weeks without treatment. In patients who have an acute monoarticular arthritis in addition to gout, other diagnoses such as osteoarthritis, pseudogout, and infection must be considered. The diagnosis of gout is established by aspiration of synovial fluid or tophi, with characteristic uric acid crystals detected by polarized light microscopy. Treatment can consist of NSAIDs in healthy individuals. Indomethacin is considered the drug of choice. Corticosteroids can also be used, and are particularly helpful when the patient has renal insufficiency. Intra-articular injections of a corticosteroid such as triamcinolone are useful, and intramuscular corticosteroids may be especially useful in patients with polyarticular gout. Colchicine may be used, but may cause diarrhea. Life style changes such as weight loss, discontinuing alcohol use, and changing antihypertensive therapy is often all that is needed to control the hyperuricemia and thus prevent further attacks. Colchicine can be used for prophylaxis as well, although it does not alter hyperuricemia or prevent tophi from forming. If a patient has more than two attacks per year, urate lowering therapy is indicated. A 24-hour urine collection to identify whether the patient is an under-excretor or an overproducer of uric acid would indicate the correct medication. Overproducers are treated with allopurinol, while under-excretors benefit from probenecid if renal function is normal and there is no history of kidney stones. |
|
|
A 21-year-old white female presents to the emergency department with a history consistent with a lateral ankle sprain that occurred 2 hours ago while she was playing softball. She complains of pain over the distal anterior talofibular ligament, but is able to bear weight. There is mild swelling, mild black and blue discoloration, and moderate tenderness to palpation over the insertion of the anterior talofibular ligament, but the malleoli are nontender to palpation. Which one of the following statements is true regarding the management of this case?
|
Early range-of-motion exercises should be initiated to maintain flexibility
This patient has an uncomplicated lateral ankle sprain and requires minimal intervention. The Ottawa ankle rules were developed to determine when radiographs are needed for ankle sprains. In summary, ankle radiographs should be done if the patient has pain at the medial or lateral malleolus and either bone tenderness at the back edge or tip of the lateral or medial malleolus, or an inability to bear weight immediately after the injury or in the emergency department, or both. If the patient complains of midfoot pain and/or bone tenderness at the base of the fifth metatarsal or navicular, or an inability to bear weight, radiographs should be ordered. Sprains can be differentiated from major partial or complete ligamentous tears by anteroposterior, lateral, and 30 degrees internal oblique (mortise view) radiographs. If the joint cleft between either malleolus and the talus is >4 mm, a major ligamentous tear is probable. Stress radiographs in forced inversion are sometimes helpful to demonstrate stability, but ankle instability can be present with a normal stress radiograph. Grade I and II ankle sprains are best treated with RICE (rest, ice, compression, elevation) and an air splint for ambulation. NSAIDs are used for control of pain and inflammation. Heat should not be applied. Early range-of-motion exercises should be initiated to maintain flexibility. Weight bearing is appropriate as tolerated and functional rehabilitation should be started when pain permits. Exercises on a balance board will help develop coordination. |
|
|
The most serious complication of a slipped capital femoral epiphysis is:
|
Avascular necrosis
Avascular necrosis is the most serious complication of a slipped capital femoral epiphysis, and leads to more rapid arthritic deterioration. It may require hip fusion and total hip replacement early in adulthood. |
|
|
A 39-year-old white male comes to your office with severe pain, fluctuance, erythema, and tenderness localized over the pad of the distal long finger. The most likely diagnosis is:
|
A felon (whitlow)
A felon, also called a whitlow, is an infection of the digital pulp of the terminal phalanx. The anatomic characteristics of this region compartmentalize infection, resulting in exquisite pressure and pain in the pulp spaces. As with all abscesses, incision and drainage is the single most important therapy. Paronychial and eponychial infections occur in the dorsal surface of the finger about the nail. Bacterial tenosynovitis is an extension of a deep space infection along the tendons. Digital cellulitis is a nonspecific term and does not adequately describe the infection depicted. The presence of fluctuance with this infection suggests abscess formation rather than a simple cellulitis. |
|
|
A 75-year-old Asian female comes to your office with a 6-week history of the gradual onset of localized low back pain. The pain is increased with walking or standing and relieved by sitting and lying. Pushing a shopping cart dramatically relieves the pain. Based on the history, which one of the following is the most likely diagnosis?
|
Spinal stenosis
Spinal stenosis pain is often referred to as pseudoclaudication because the pain is worsened by walking. Any movement that flexes the spine, such as pushing a shopping cart, relieves the pain. Pain from tumor or infection is persistent. Osteoporotic vertebral fractures have a sudden onset. Sciatica does not have the typical findings of spinal stenosis. |
|
|
A 3-year-old female is brought to your office for evaluation of mild intoeing. The child’s patellae face forward, and her feet point slightly inward. What would be most appropriate management?
|
Reassurance
Intoeing, as described, is usually caused by internal tibial torsion. This problem is believed to be caused by sleeping in the prone position, and sitting on the feet. In 90% of cases, internal tibial torsion gradually resolves without intervention by the age of 8. Avoiding prone sleeping enhances resolution of the problem. Night splints, orthotics, and shoe wedges are ineffective. Surgery (osteotomy) has been associated with a high complication rate, and is therefore not recommended in mild cases before the age of 8. |
|
|
A 9-month-old male is seen for a routine well-baby examination. There have been no health problems and developmental milestones are normal. Review of the growth chart shows that length, weight, and head circumference have continued to remain at the 75th percentile. The examination is normal with the exception of the anterior fontanelle being closed. Proper management at this time would include:
|
Serial measurement of head circumference
The anterior fontanelle in the newborn is normally 0.6–3.6 cm, with the mean size being 2.1 cm. It may actually enlarge the first few months, but the medial age of closure is 13.8 months. The anterior fontanelle closes at 3 months in 1% of cases, and by 1 year, 38% are closed. While early closure of the anterior fontanelle may be normal, the head circumference must be carefully monitored. The patient needs to be monitored for craniosynostosis (premature closure of one or more sutures) and for abnormal brain development. When craniosynostosis is suspected, a skull radiograph is useful for initial evaluation. If craniosynostosis is seen on the film, a CT scan should be obtained. |
|
|
A positive flexion abduction external rotation (FABER) test that elicits posterior pain indicates involvement of which joint?
|
Sacroiliac
When the flexion abduction external rotation (FABER) test elicits pain posteriorly, it indicates sacroiliac involvement. Anterior pain indicates hip involvement. |
|
|
Of the following, an 11-year-old who presents with knee pain is most likely to have:
A. Gout B. Tibial apophysitis C. A popliteal cyst D. Inflammatory arthropathy E. Pes anserine bursitis |
Tibial apophysitis
The three most common knee conditions in children and adolescents are patellar subluxation, tibial apophysitis, and patellar tendinitis. Gout, osteoarthritis, and popliteal cysts present in older adults. Inflammatory arthritis is more common in adults than in children. |
|
|
What would be an indication for a second dose of pneumococcal polysaccharide vaccine (Pneumovax 23) in children?
|
Sickle cell disease
Patients with chronic illness, diabetes mellitus, cerebrospinal fluid leaks, chronic bronchopulmonary dysplasia, cyanotic congenital heart disease, or cochlear implants should receive one dose of pneumococcal polysaccharide vaccine after 2 years of age, and at least 2 months after the last dose of pneumococcal conjugate vaccine (Prevnar 13). Revaccination with polysaccharide vaccine is not recommended for these patients. Individuals with sickle cell disease, those with anatomic or functional asplenia, immunocompromised persons with renal failure or leukemia, and HIV-infected persons should receive polysaccharide vaccine on this schedule and should be revaccinated at least 5 years after the first dose. |
|
|
The intranasal live, attenuated influenza vaccine would be appropriate for which patient populations?
|
A 5-year-old female who is otherwise healthy
The live, attenuated influenza vaccine is an option for vaccinating healthy, nonpregnant individuals age 5-49 years. The vaccine is administered intranasally. It is not indicated in patients with underlying medical conditions, such as chronic pulmonary or cardiovascular disease, or in patients with a history of Guillain-Barré syndrome, pregnant patients, or children and adolescents who receive long-term aspirin or salicylate therapy. Patients with a history of hypersensitivity to eggs should not receive this vaccine. |
|
|
Patients with obstructive sleep apnea have an increased risk for
|
hypertension
Obstructive sleep apnea-hypopnea syndrome is defined as the presence of at least five obstructive events per hour with associated daytime sleepiness. It is present in 2%-4% of the population. The prevalence in men is almost three times that seen in premenopausal women and twice that of postmenopausal women. Other factors associated with an increased prevalence are obesity, older age, and systemic hypertension. |
|
|
A 32-year-old white male teacher is seen for a paroxysmal cough of 5 days duration. He tells you that a student in his class was diagnosed with pertussis 3 weeks ago. What would be the best treatment?
|
Azithromycin (Zithromax)
Macrolides are considered first-line therapy for Bordetella pertussis infection. Trimethoprim/sulfamethoxazole is considered second-line therapy. |
|
|
A 60-year-old female is admitted to the hospital with pneumonia 1 week after her discharge following elective colorectal surgery. Her initial stay was 5 days and she had no complications. She had no signs of infection until 2 days ago when she developed a temperature of 39.1°C (102.4°F), a cough with yellow sputum, and hypoxia. She has no abdominal pain or diarrhea. Her pulse rate is slightly elevated to 96 beats/min, and her blood pressure is unchanged from baseline. A chest radiograph confirms a left lingular infiltrate. Methicillin-resistant Staphylococcus pneumonia is rare in this institution. What would be the best initial treatment for this patient?
|
Ceftazidime sodium (Fortaz) and gentamicin
This patient has a significant pneumonia that requires the initiation of empiric antibiotics. It is important to remember that because this patient was recently in the hospital, the usual coverage for community-acquired pneumonia is not adequate. Health care-associated pneumonia is more likely to involve severe pathogens such as Pseudomonas aeruginosa, Klebsiella pneumoniae, and Acinetobacter species. Methicillin-resistant Staphylococcus aureus also is a consideration, depending on local prevalence. Of the antibiotic regimens listed, ceftazidime and gentamicin is the only choice that covers these organisms. |
|
|
A 22-year-old competitive cross-country skier presents with a complaint of not being able to perform as well as she expects. She has been training hard, but says she seems to get short of breath more quickly than she should. She also coughs frequently while exercising. A review of systems is otherwise negative. Her family history is negative for cardiac or pulmonary diseases. Her physical examination is completely normal, and pulmonary function tests obtained before and after bronchodilator use are normal. After you discuss your findings with the patient, she acknowledges that her expectations may be too high, but can think of no other cause for her problem. What would be the next reasonable step?
|
A trial of inhaled albuterol (Proventil) for exercise-induced bronchospasm
Exercise-induced bronchoconstriction (EIB) is a very common and underdiagnosed condition in athletes. It is defined as a 10% lowering of FEV1 when challenged with exercise. The exercise required to cause bronchoconstriction is 5-8 minutes at 80% of maximal oxygen consumption. EIB is much more common in high-ventilation sports, such as track and cross-country skiing. It is also more common in winter sports, because of the inspiration of cold, dry air. In some studies the incidence among cross-country skiers is as high as 50%, and 40% of those who have positive tests for bronchospasm are unaware of the problem. A physical examination, as well as pulmonary function tests at rest and before and after bronchodilators, will be normal unless there is underlying asthma. Among athletes with EIB, 10% will not have asthma. Bronchoprovocative testing can be ordered, but if it is not available a trial with an albuterol inhaler is reasonable. |
|
|
A 25-year-old Hispanic male comes to the emergency department with the sudden onset of moderate to severe right-sided chest pain and mild dyspnea. Vital signs are normal. A chest film shows a loss of markings along the right lung margins, involving about 10%-15% of the lung space. The mediastinum has not shifted. The best INITIAL treatment would be
|
oxygen supplementation and close observation
A small spontaneous pneumothorax involving less than 15%-20% of lung volume can be managed by administering oxygen and observing the patient. The pneumothorax will usually resorb in about 10 days if no ongoing air leak is present. Oxygen lowers the pressure gradient for nitrogen and favors transfer of gas from the pleural space to the capillaries. Decompression with anterior placement of an intravenous catheter is usually reserved for tension pneumothorax. Chest tube placement is used if observation is not successful or for larger pneumothoraces. Strict bed rest is not indicated. |
|
|
A 30-year-old white male complains of several weeks of nasal stuffiness, purulent nasal discharge, and facial pain. He does not respond to a 3-day course of trimethoprim/sulfamethoxazole (Bactrim, Septra). Follow-up treatment with 2 weeks of amoxicillin/clavulanate (Augmentin) is similarly ineffective. Of the following diagnostic options, which one is most appropriate at this time?
|
Coronal CT of the sinuses
This patient has a clinical presentation consistent with acute sinusitis. Failure to respond to adequate antibiotic therapy suggests either a complication, progression to chronic sinusitis, or a different, confounding diagnosis. The diagnostic procedure of choice in this situation is coronal CT of the sinuses, due to its increased sensitivity and competitive cost when compared with standard radiographs. Cultures of the nasal discharge give unreliable results because of bacterial contamination from the resident flora of the nose. |
|
|
A 60-year-old male with a right-sided pleural effusion undergoes thoracentesis. Analysis of the pleural fluid reveals a protein level of 2.0 g/dL and an LDH level of 70 U/L. His serum protein level is 7.0 g/dL (N 6.0-8.3) and his serum LDH level is 200 U/L (N 100-105). Based on these findings, which one of the following is the most likely diagnosis?
|
Heart failure
Pleural effusions may be exudates or transudates. The distinction is important for an accurate diagnosis and to help determine what further evaluations may be necessary. Lights criteria use ratios of fluid/serum values for protein and LDH. Pleural fluid/serum ratios greater than 0.6 for LDH and 0.5 for protein are indicative of exudates. In the scenario presented, both ratios are approximately 0.3; therefore, the fluid is a transudate. The list of causes for transudates is much shorter than for exudates. The vast majority of transudates are due to heart failure, with cirrhosis being the next most common cause. Once there is reasonable certainty that the fluid is a transudate, additional studies usually are not necessary. The other conditions listed result in exudative pleural effusions. Ref: Porcel JM, Light RT: Diagnostic approach to pleural effusion in adults |
|
|
A 6-year-old female presents with a 24-hour history of dry cough, malaise, and a temperature of 39.8°C (103.6°F). She received an influenza vaccination shot 7 days ago. A rapid influenza test is positive for influenza A. Which one of the following would be the best treatment option for this patient?
|
Oseltamivir (Tamiflu)
Amantadine and rimantadine are not recommended for the treatment of influenza A because of the development of resistance to these drugs. Resistance is not a problem with neuramidase inhibitors such as oseltamivir in immunocompetent patients. Zanamivir is not recommended for treatment of children under the age of 7. Although this child has recently received influenza vaccine, this is not a contraindication to drug therapy. |
|
|
A 12-year-old female has a cough and slight shortness of breath on a daily basis. She is awakened by the cough at least 3 nights per week. What would be the most appropriate treatment for this patient?
|

Inhaled corticosteroids daily
This patient has moderate persistent asthma. The preferred and most effective treatment is daily inhaled corticosteroids. A leukotriene inhibitor would be less effective. Oral prednisone daily is not recommended because of the risk of inducing adrenal insufficiency. Short- and long-acting β-agonists are not recommended as daily therapy because either can cause tachyphylaxis. They are considered rescue medications rather than preventive treatments. |
|
|
Good evidence supports which one of the following measures for reducing the risk of postoperative pulmonary complications after major abdominal surgery?
|
Use of an incentive spirometer
Use of an incentive spirometer and similar lung expansion techniques such as chest physiotherapy have been shown to have significant benefit for reducing postoperative complications. A course of preoperative corticosteroids has been shown to be beneficial for patients with COPD. Prolonged antibiotic prophylaxis and postoperative total parenteral nutrition have not been shown to have any benefit. |
|
|
What is the schedule for administering rotavirus vaccine?
|
The first dose should be given prior to 12 weeks of age
The rotavirus vaccine is an oral vaccine recommended for infants in a 3-dose schedule at ages 2, 4, and 6 months. The first dose should be given between 6 and 12 weeks of age, with additional doses given at 4 to 10-week intervals. The vaccine cannot be initiated after 12 weeks of age and should not be administered after 32 weeks of age. The first rotavirus vaccine was taken off the market in 1999 after an increased risk of intussusception was noted in infants when the first dose of the vaccine was given after 12 weeks of age. Because of this, the two vaccines licensed in 2006 carry the recommendation that the vaccine not be initiated in infants over 12 weeks of age. There is no data regarding safety and efficacy after this age. |
|
|
What is recommended for the treatment of cough and cold symptoms in children younger than 2 years of age?
|
Nasal saline with bulb suction
No medication available in the United States has been shown to effectively treat cough or cold symptoms in children younger than 2 years of age. However, many agents are commonly prescribed despite reports of numerous minor, and some serious, adverse effects. For this reason, the American Academy of Pediatrics and the American Academy of Family Physicians recommend using only nasal saline, bulb suction, humidified air, and good hydration in children younger than 2 years of age. |
|
|
A 66-year-old male smoker is being evaluated for a persistent cough and difficulty breathing. Spirometry confirms a fixed obstructive pathology with an FEV1 of about 50% of predicted for habitus and age. His oxygen saturation is 89%-90% on room air. Which one of the following would be most effective to prevent worsening of this patient's condition?
A. A combined inhaled corticosteroid and long-acting β-agonist B. A long-acting anticholinergic agent C. Long-term oral corticosteroids D. Oxygen therapy E. Smoking cessation |
|
|
|
A 66-year-old male smoker is being evaluated for a persistent cough and difficulty breathing. Spirometry confirms a fixed obstructive pathology with an FEV1 of about 50% of predicted for habitus and age. His oxygen saturation is 89%-90% on room air. Which one of the following would be most effective to prevent worsening of this patient's condition?
A. A combined inhaled corticosteroid and long-acting β-agonist B. A long-acting anticholinergic agent C. Long-term oral corticosteroids D. Oxygen therapy E. Smoking cessation |

This patient has moderate to severe COPD. Smoking cessation is the single most important therapeutic intervention in patients with this condition and should be the priority of care. No existing medications have been shown to modify the long-term decline in lung function that is typical of COPD, but smoking cessation does prevent this decline. Long-term use of oxygen in COPD patients who also have chronic, severe hypoxia (<88% saturation) can improve quality of life and prolong survival; however, oxygen cannot prevent further decline in lung function. Long-term use of oral corticosteroids is discouraged because of an unfavorable risk-to-benefit ratio. Ref: Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease.
|
|
|
A 67-year-old smoker with a history of pulmonary tuberculosis at 22 years of age presents with a 6-month history of increasing shortness of breath. On office spirometry his FVC is 60% of predicted, his FEV1 is 80% of predicted, and his FEV1/FVC ratio is 0.8. Which one of the following would be the most appropriate next step in his evaluation?
|
Refer to a pulmonary laboratory for static lung volume measurement and diffusion studies
Pulmonary function tests are usually classified as normal, compatible with a restrictive defect, or consistent with obstructive airway disease. In restrictive ventilatory processes, the FVC is decreased, the FEV1 is decreased or normal, and the absolute FEV1/FVC is >0.7. In obstructive airway problems, findings include a normal or decreased FVC, a decreased FEV1, and an absolute FEV1/FVC <0.7. When simple spirometry suggests a restrictive ventilatory problem, the patient should undergo full pulmonary function testing for static lung volume measurements and diffusing capacity of the lung for carbon monoxide. If spirometry suggests an obstructive problem, it should be repeated after administering an inhaled bronchodilator. Because this patient has a history of pulmonary tuberculosis, a TB skin test is inappropriate and would not provide any useful information. |
|
|
What is a significant side effect of varenicline (Chantix)?
|
Suicidal ideation
Education, support, and medications are all valuable tools in assisting patients with a smoking habit. Varenicline, a clinically effective smoking-cessation product, has been associated with patient mood changes following the initiation of therapy, including suicidal thoughts and aggressive and erratic behavior. The other problems listed have not been associated with varenicline use. |
|
|
A 40-year-old male respiratory therapist presents for a health examination prior to hospital employment. His history indicates that as a child he lived on a farm in Iowa, and his examination is unremarkable, but a chest radiograph shows that both lung fields have BB-sized calcifications in a miliary pattern. No other findings are noted. A PPD skin test is negative. The findings in this patient are most likely a result of
|
histoplasmosis
Asymptomatic patients in excellent health often present with this characteristic chest radiograph pattern, which is usually due to histoplasmosis infection, especially if the patient has been in the midwestern United States. Exposure to bird or bat excrement is a common cause, and treatment is usually not needed. This pattern is not characteristic of the other infections listed, although miliary tuberculosis is a remote possibility in spite of the negative PPD skin test. |
|
|
A 60-year-old male presents to the urgent care center with a fever and a productive cough. He has a 40 pack/year history of cigarette smoking. In addition to lobar pneumonia on a chest radiograph, there is an incidental finding of bilateral pleural plaques. Which one of the following is the most likely cause of this finding?
|
Asbestos
Development of pleural plaques is the most common pathologic pulmonary response to asbestos inhalation. Over time, collagen is deposited in the pleura and may calcify. Most plaques are asymptomatic, and there is no evidence that plaques transform into malignant lesions. Plaques occur in approximately 50% of persons with heavy and prolonged exposure to asbestos and, therefore, are a marker of asbestos exposure. This should alert the physician to follow the patient for development of more serious asbestos-related diseases (e.g., lung cancer and mesothelioma). Although the other substances listed are associated with pulmonary diseases (coal dust and silicon dust with pneumoconiosis, and vinyl chloride and radon with lung cancer), none is associated with pleural plaques as found in this patient. |
|
|
A 72-year-old male slipped on a rug in his kitchen and struck his right side against a counter. He presents several days after the fall with a complaint of ongoing pain in his flank. He has a history of chronic atrial fibrillation, which is treated with warfarin (Coumadin). His vital signs are normal. A physical examination reveals tenderness to palpation along the posterior-lateral chest wall and decreased breath sounds in the right base. Radiographs reveal two fractured ribs on the right side and a moderately large pleural effusion in the right hemithorax. Laboratory test results include a hemoglobin of 10.5 mg/dL (baseline 11.0-12.0 mg/dL) and a prothrombin time of 33.5 seconds with an INR of 3.5. Which one of the following would be the most appropriate management at this time?
|
Evacuation of the pleural space
This patient has been clinically stable despite losing what appears to be a fair amount of blood into his pleural space after fracturing two ribs, a condition referred to as hemothorax. The treatment of choice in this condition is to remove the bloody fluid and re-expand the associated lung. This therapy is felt to decrease any ongoing blood loss by having the lung pleura put a direct barrier over the site that is bleeding. It also prevents the development of empyema or fibrosis, which could occur if the blood were to remain. |
|
|
A 70-year-old male sees you because of slowly increasing problems with COPD. He has had frequent exacerbations requiring emergency department visits. He currently uses a tiotropium (Spiriva) inhaler once a day, as well as an albuterol (Proventil) inhaler, 2 puffs 4 times a day as needed. An examination shows decreased breath sounds throughout, and an oxygen saturation of 92%. Spirometry shows he has severe COPD (stage III); his FEV1/FVC ratio is 65% of predicted and his FEV1 is 45% of predicted. The most reasonable change in treatment would be to add
|

inhaled fluticasone (Flovent), 2 puffs twice daily
This patient is suffering from severe COPD (stage III) and has a history of frequent exacerbations. The addition of a corticosteroid inhaler for patients with severe disease has been found to significantly decrease the number of exacerbations, but has no effect on overall mortality. Side effects of oral candidiasis and easy bruising of the skin are increased. Continuous oxygen has been shown to improve overall mortality and endurance in patients with an oxygen saturation of 88% or less, but has not been shown to improve quality of life in those with mild hypoxemia or if used only at night. Oral prednisone has been shown to be effective when used to treat acute exacerbations, but when used on a chronic basis it is no more effective than corticosteroid inhalers. Chronic oral prednisone is also associated with significant side effects, and therefore is not generally recommended. Oral theophylline has not been shown to be of benefit in either preventing exacerbations or improving quality of life, and has significant side effects of gastrointestinal toxicity, seizures, and arrhythmias. It should be reserved for carefully selected patients only. |
|
|
A previously healthy 20-month-old female is brought to the urgent-care clinic during the evening with a barking cough. On examination her rectal temperature is 37.9°C (100.2°F), respiratory rate 18/min, heart rate 120 beats/min, and O2 saturation 94%. She has stridor, with mild substernal retractions only when her temperature was taken. Which one of the following would be most appropriate at this point?
|
Dexamethasone, 0.6 mg/kg orally or intramuscularly as a single dose
Croup is a syndrome most often caused by viruses, but can occasionally be of bacterial origin as in laryngotracheitis, laryngotracheobronchitis (LTB), laryngotracheobroncheopneumonia (LTBP), or laryngeal diphtheria. Mild croup is manifested by an occasional barking cough with no stridor at rest, and mild or absent intercostal retractions. Moderate croup presents with a more frequent barking cough, stridor with suprasternal and sternal retractions at rest, but no agitation. Severe croup includes more prominent inspiratory and expiratory stridor with agitation and distress. There is good evidence that corticosteroids produce significant improvement. The regimens studied most frequently have consisted of single-dose dexamethasone (0.6 mg/kg orally or intramuscularly), with some studies including up to four more doses over a 2-day period. Longer courses of corticosteroids have not proven to be more effective and may be harmful, leading to secondary infections. Racemic epinephrine by nebulization is indicated in severe croup. Antitussives and decongestants have not been studied and are not recommended. Antibiotics are indicated in LTB and LTBP, which can be diagnosed on the basis of crackles and wheezing on examination, or by an abnormal chest radiograph. Laryngotracheitis can sometimes be associated with a bacterial infection, but should be suspected only after a patient does not improve with corticosteroids and epinephrine. |
|
|
A 42-year-old female presents with a 2-day history of chest pain. She describes the pain as sharp, located in the right upper chest, and worsened by deep breathing or coughing. She also complains of shortness of breath. She was previously healthy and has no recent history of travel. Her vital signs are normal. A pleural friction rub is noted on auscultation of the lungs. The remainder of the examination is normal. An EKG, cardiac enzymes, oxygen saturation, and a D-dimer level are all normal. What would be most appropriate at this point?
|
A chest radiograph
This patient has pleurisy. Patients presenting with pleuritic chest pain may have life-threatening disorders, and pulmonary embolism, acute myocardial infarction, and pneumothorax should be excluded. While 5%-20% of patients with pulmonary embolism present with pleuritic chest pain, this patient has no risks for pulmonary embolism and the normal D-dimer level obviates the need for further evaluation. Moderate- to high-risk patients may need a helical CT scan or other diagnostic testing. An EKG and chest radiograph are recommended in the evaluation of acute/subacute pleuritic chest pain. The chest radiograph will exclude pneumothorax, pleural effusion, or pneumonia. An echocardiogram would not be indicated if the cardiac examination and EKG are normal. An antinuclear antibody level could be considered in recurrent pleurisy or if other symptoms or signs of lupus were present, but it would not be indicated in this patient. Most cases of acute pleurisy are viral and should be treated with NSAIDs unless the workup indicates another problem. |
|
|
A 24-year-old female with a past history of asthma presents to the emergency department with an asthma exacerbation. Treatment with an inhaled bronchodilator and ipratropium (Atrovent) does not lead to significant improvement, and she is admitted to the hospital for ongoing management. On examination she is afebrile, her respiratory rate is 24/min, her pulse rate is 92 beats/min, and oxygen saturation is 92% on room air. She has diffuse bilateral inspiratory and expiratory wheezes with mild intercostal retractions. Which one of the following should be considered in the acute management of this patient?
A. Chest physical therapy B. Inhaled fluticasone/salmeterol (Advair) C. Oral azithromycin (Zithromax) D. Oral prednisone E. Oral theophylline |
Oral prednisone
Hospital management of acute exacerbations of asthma should include inhaled short-acting bronchodilators in all patients. Systemic corticosteroids are recommended for all patients admitted to the hospital. The efficacy of oral prednisone has been shown to be equivalent to that of intravenous methylprednisolone (SOR A). Oxygen should also be considered in most patients. Antibiotics are not recommended in the treatment of asthma exacerbations unless there is a comorbid infection. Inhaled ipratropium bromide is recommended for treatment in the emergency department, but not in the hospital (SOR A). Chest physical therapy and methylxanthines are not recommended in the treatment of acute asthma exacerbations. |
|
|
A male infant is delivered at 41 weeks gestation by spontaneous vaginal delivery. The amniotic fluid is meconium stained. Apgar scores are 7 at 1 minute and 7 at 5 minutes. The baby is noted to have respiratory distress from birth and is hypoxic by pulse oximetry. Respiration improves with supplemental oxygen, as does the hypoxia, but does not return to normal. What would most likely be seen on a chest radiograph?
|
Patchy atelectasis
The chest radiograph of a child with meconium aspiration syndrome will show patchy atelectasis or consolidation. If the child has a normal chest film and respiratory distress, a noncardiopulmonary source should be considered (i.e., a neurologic or metabolic etiology). The chest film of a child with transient tachypnea of the newborn will show a wet silhouette around the heart, diffuse parenchymal infiltrates, or intralobar fluid accumulation. Homogeneous opaque infiltrates with air bronchograms on a chest radiograph are seen with hyaline membrane disease. |
|
|
A male infant is delivered by cesarean section because of dystocia due to macrosomia. Apgar scores are 8 at 1 minute and 10 at 5 minutes. However, at about 1 hour of age he begins to have tachypnea without hypoxemia. A chest radiograph shows diffuse parenchymal infiltrates and fluid in the pulmonary fissures. The symptoms resolve without treatment within 24 hours. The most likely diagnosis is
|
transient tachypnea of the newborn
This child had transient tachypnea of the newborn, the most common cause of neonatal respiratory distress. It is a benign condition due to residual pulmonary fluid remaining in the lungs after delivery. Risk factors include cesarean delivery, macrosomia, male gender, and maternal asthma and/or diabetes mellitus. The other conditions listed cause neonatal respiratory distress, but do not resolve spontaneously. They also cause additional significant abnormal findings on physical examination and/or ancillary studies such as imaging and laboratory studies. |
|
|
You see a 9-month-old male with a 1-day history of cough and wheezing. He has previously been healthy and was born after an uncomplicated term pregnancy. He is up to date on his immunizations. On examination his temperature is 38.6°C (101.5°F) and his respiratory rate is 30/min. He has diffuse wheezing and his oxygen saturation on room air is 94%. Because it is midwinter, you obtain a swab for influenza, which is negative. A chest radiograph shows peribronchiolar edema. Appropriate management would include which one of the following?
|
Supportive care only
This child has a respiratory syncytial virus (RSV) infection. Supportive care is the mainstay of therapy. If the child can take in fluids by mouth and tolerate room air, outpatient management with close physician contact as needed is reasonable, especially in the absence of significant underlying risk factors. Routine use of corticosteroids is not recommended (SOR B). Although up to 60% of infants hospitalized for bronchiolitis receive corticosteroid therapy, studies have not provided sufficient evidence to support their use. Inhaled corticosteroids have not been shown to be beneficial, and the safety of high doses in infants is unclear. Supplemental oxygen should be administered if functional oxygen saturation (SpO2) persistently falls below 90% and can be discontinued when an adequate level returns (SOR C). Antiviral therapy for RSV bronchiolitis is controversial because of its marginal benefit, cumbersome delivery, potential risk to caregivers, and high cost (SOR B). Studies of ribavirin in patients with bronchiolitis have produced inconsistent findings. Palivizumab is a preventive measure, and is not used for treatment of the active disease. It may be considered in select infants and children with prematurity, chronic lung disease of prematurity, or congenital heart disease (SOR A). If used, it should be administered intramuscularly in five monthly doses of 15 mg/kg, usually beginning in November or December (SOR C). |
|
|
A 27-year-old male presents with what he thinks is a sinus infection. He has a 2-day history of right maxillary pain associated with nasal congestion and clear rhinorrhea. The only significant findings on examination are a low-grade fever and subjective tenderness with palpation over the right maxillary sinus. Which one of the following treatments is most supported by current evidence?
A. Antihistamines B. Oral decongestants C. Topical vasoconstrictor sprays D. Oral analgesics E. Nasal lavage |
Oral analgesics
Although oral antibiotics are overwhelmingly prescribed as initial treatment in acute sinusitis, it has been shown that the majority of acute illnesses are viral in origin and that 98% of cases will resolve spontaneously. Analgesics are considered the mainstay of therapy for acute sinusitis, according to evidence-based recommendations (SOR A). Other treatments should be considered if symptoms are prolonged (>7 days) or severe (two or more localizing symptoms or signs of serious bacterial complications). There is little evidence of effectiveness for antihistamines, oral decongestants, or vasoconstrictor sprays. There is also little evidence of effectiveness for nasal lavage in acute sinusitis, although it has an emerging role in chronic sinusitis. |
|
|
A 32-year-old African-American female presents with a 3-day history of fever, cough, and shortness of breath. She has been healthy otherwise, except for a sinus infection 2 months ago treated with amoxicillin. She does not appear toxic. A chest radiograph reveals an infiltrate in the right lower lobe, consistent with pneumonia. What would be the best choice for antibiotic treatment?
|
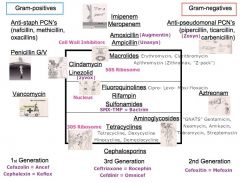
Levofloxacin (Levaquin)
For previously healthy patients with community-acquired pneumonia and no risk factors for drug resistance, a macrolide such as azithromycin is the preferred treatment (SOR A). Doxycycline is also acceptable (SOR C). Patients who have been treated with antibiotics within the previous 3 months should be treated with a respiratory fluoroquinolone (moxifloxacin, gemifloxacin, or levofloxacin) (SOR A). A β-lactam plus a macrolide is also an alternative (SOR A). The antibiotic chosen should be from a different class than the one used for the previous infection. These alternative treatments are also recommended for those with comorbidities such as chronic heart, lung, liver, or renal disease; diabetes mellitus; alcoholism; malignancies; asplenia; immunosuppressing conditions or use of immunosuppressing drugs; or other risk factors for drug-resistant Streptococcus pneumoniae infection (SOR A). |
|
|
A 5-month-old infant has had several episodes of wheezing, not clearly related to colds. The pregnancy and delivery were normal; the infant received phototherapy for 1 day for hyperbilirubinemia. He had an episode of otitis media 1 month ago. There is no chronic runny nose or strong family history of asthma. He spits up small amounts of formula several times a day, but otherwise appears well. His growth curve is normal. An examination is unremarkable except for mild wheezing. Which one of the following is the most likely diagnosis?
|
Gastroesophageal reflux
Gastroesophageal reflux is a common cause of wheezing in infants. At 5 months of age, most infants no longer spit up several times a day, and this is a major clue that the wheezing may be from the reflux. Also, there is no family history of asthma and the wheezing is not related to infections. Cystic fibrosis is more likely to present with recurrent infections and failure to thrive than with intermittent wheezing. |
|
|
A 40-year-old African-American female presents to your office complaining of a persistent dry cough for the last 3 months. This seemed to start with a “bad chest cold.” She went to an urgent-care facility 6 weeks ago and the physician prescribed albuterol (Proventil, Ventolin) by metered-dose inhaler empirically for presumed reactive airways disease. This did not help. Now she also reports dyspnea on exertion that is noticeable when walking uphill. She has been taking nitrofurantoin (Macrodantin) for chronic urinary tract infections, but has an otherwise negative history. She works as a legal secretary. On examination, she is tachypneic. There is no cyanosis or clubbing. Her lungs are clear. Her height is 160 cm (63 in) and her weight is 60 kg (132 lb). Office pulmonary function tests reveal a forced vital capacity (FVC) of 1.4 L (average 3.3) and a 1-second forced expiratory volume (FEV1) of 1.6 L (average 2.8). An inhaled bronchodilator produces no improvement in these numbers. Which one of the following is the most likely cause of her problem?
|
Interstitial lung disease
This patient has a markedly reduced FVC with an FEV1/FVC ratio of 1.14%. This is consistent with moderately severe pulmonary restriction. Most likely the patient has chronic interstitial restrictive lung disease. Nitrofurantoin can cause this picture, usually after continuous treatment for 6 or more months, and pulmonary function may be impaired permanently. A wide variety of additional causes have been described including noxious gases, pulmonary hypersensitivities, neoplasia, and systemic diseases (e.g., sarcoidosis). Management includes avoidance of the offending agent or treatment of the underlying condition. |
|
|
A 25-year-old white male who has a poorly controlled major seizure disorder and a 6-week history of recurrent fever, anorexia, and persistent, productive coughing visits your office. On physical examination he is noted to have a temperature of 38.3 degrees C (101.0 degrees F), a respiratory rate of 16/min, gingival hyperplasia, and a fetid odor to his breath. Auscultation of the lungs reveals rales in the mid-portion of the right lung posteriorly. What is most likely to be found on a chest radiograph?
|
A lung abscess
Anaerobic lung abscesses are most often found in a person predisposed to aspiration who complains of a productive cough associated with fever, anorexia, and weakness. Physical examination usually reveals poor dental hygiene, a fetid odor to the breath and sputum, rales, and pulmonary findings consistent with consolidation. Patients who have sarcoidosis usually do not have a productive cough and have bilateral physical findings. A persistent productive cough is not a striking finding in disseminated tuberculosis, which would be suggested by miliary calcifications on a chest film. The clinical presentation and physical findings are not consistent with a simple mass in the right hilum nor with a right pleural effusion. |
|
|
A healthy 24-year-old male presents with a sore throat of 2 days’ duration. He reports mild congestion and a dry cough. On examination, his temperature is 37.2 degrees C (99.0 degrees F). His pharynx is red without exudates, and there are no anterior cervical nodes. His tympanic membranes are normal, and his chest is clear. What's the next appropriate step?
|
Treat with analgesics and supportive care
The Centers for Disease Control and Prevention (CDC) assembled a panel of national health experts to develop evidence-based guidelines for evaluating and treating adults with acute respiratory disease. In clinical screening, the most reliable predictors of streptococcal pharyngitis are the Centor criteria. These include tonsillar exudates, tender anterior cervical lymphadenopathy, absence of cough, and history of fever. The presence of three or four of these criteria has a positive predictive value of 40%–60%, and the absence of three or four of these criteria has a negative predictive value of 80%. Patients with four positive criteria should be treated with antibiotics, those with three positive criteria should be tested and treated if positive, and those with 0–1 positive criteria should be treated with analgesics and supportive care only. This patient has only one of the Centor criteria, and according to the panel should not be tested or treated with antibiotics. |
|
|
A 12-year-old white male asthmatic has an acute episode of wheezing. You diagnose an acute asthma attack and prescribe an inhaled beta2-adrenergic agonist, but despite 1–2 hours of treatment he continues to experience wheezing and shortness of breath. Which one of the following is the most appropriate addition to acute outpatient management?
|

Oral corticosteroids
The treatment of choice for occasional acute symptoms of asthma is an inhaled beta2-adrenergic agonist such as albuterol, terbutaline, or pirbuterol. However, acute symptoms that do not respond to beta-agonists should be treated with a short course of systemic corticosteroids. Theophylline has limited usefulness for treatment of acute symptoms in patients with intermittent asthma; it is a less potent bronchodilator than subcutaneous or inhaled adrenergic drugs, and therapeutic serum concentrations can cause transient adverse effects such as nausea and central nervous system stimulation in patients who have not been taking the drug continuously. Cromolyn can decrease airway hyperreactivity, but has no bronchodilating activity and is useful only for prophylaxis. Inhaled corticosteroids should be used for suppressing the symptoms of chronic persistent asthma. Oral beta2-selective agonists are less effective and have a slower onset of action than the same drugs given by inhalation. |
|
|
A 3-year-old child is brought to the emergency department with a barking cough, a hoarse voice, and mild stridor. You diagnose acute laryngotracheitis. Which treatment in the emergency department will reduce this child’s chance of subsequent hospitalization during this acute illness?
|
Dexamethasone (Decadron)
In laryngotracheitis (croup), intramuscular or oral dexamethasone (0.6 mg/kg) has been shown to reduce the rate of subsequent admission after acute treatment. Nebulized budesonide is also useful, but is not yet available in the United States. This disease is usually viral, and antibiotics are not helpful. Humidified air is of unproven benefit, and mist tents separate children from caregivers and hinder observation and evaluation. |
|
|
A healthy 68-year-old white male comes to your office for a health maintenance visit. He tells you he last saw a physician 6 years ago, and he recalls receiving a “flu shot” and a “pneumonia shot” at that time. According to current Centers for Disease Control (CDC) recommendations for giving pneumococcal vaccine (Pneumovax) in the elderly, this patient should be revaccinated:
|
Once
According to the most recent guidelines from the Centers for Disease Control, pneumococcal vaccine should be given to ALL persons 65 or over, including both previously unvaccinated persons and those who received the vaccine before age 65 but were vaccinated over 5 years ago. This patient was age 62 when he received the vaccine, indicating he should be revaccinated at the time of the health maintenance visit. Data from a single epidemiologic study suggest that the vaccine may provide protection for at least 9 years after receipt of the initial dose; however, data to support the need for subsequent doses of pneumococcal vaccine are not available, and because there is insufficient data concerning the safety of pneumococcal vaccine when administered three or more times, revaccination following a second dose is not routinely recommended. |
|
|
In a 1-year-old, pneumococcal 7-valent conjugate vaccine (Prevnar) is preferred rather than polyvalent pneumococcal vaccine (Pneumovax) because of which advantage?
|
It is more immunogenic
Pneumococcal 7-valent vaccine produces a satisfactory immune response in a 1-year-old, while polyvalent vaccine does not cause a good antibody response in children under the age of 2. Neither vaccine is available orally, and cost is not a factor. The 7-valent vaccine requires multiple doses. Neither vaccine can be combined with MMR. |
|
|
Pneumococcal 7-valent vaccine produces a satisfactory immune response in a 1-year-old, while polyvalent vaccine does not cause a good antibody response in children under the age of 2. Neither vaccine is available orally, and cost is not a factor. The 7-valent vaccine requires multiple doses. Neither vaccine can be combined with MMR.
|
A repeat PPD in 2 weeks
In 2000, the American Thoracic Society and the Centers for Disease Control and Prevention (CDC) advocated a shift in focus from screening the general population to testing only patients at increased risk for developing tuberculosis. In some persons PPD reactivity wanes with time but can be recalled by a second skin test administered 1 week or more after the first (i.e., two-step testing). For persons undergoing PPD skin testing, such as health-care workers, initial two-step testing may preclude misclassification of persons with boosted reactions as PPD converters. In those at low risk, such as this patient, a tuberculin skin test is now considered positive only if induration is at least 15 mm. Thus, this hospital volunteer would pose little risk to the hospital population since her 10-mm reaction falls within the guidelines of a negative test. She does not require diagnostic evaluation at this time, and isoniazid therapy is not indicated. |
|
|
What physical exam finding is an indicator of low risk for streptococcal infection in a patient with acute pharyngitis?
|
Cough
Indicators of a low risk of streptococcal infection include the absence of fever in patients not using antipyretic agents, the absence of pharyngeal erythema, and the presence of obvious manifestations of the common cold. Uncharacteristic symptoms include coryza, hoarseness, cough, and diarrhea. |
|
|
The most common illness related to occupational exposure is:
|
Asthma
While occupational exposure to large and small particles and gases is common and can lead to long-term pulmonary difficulties, asthma remains the most common illness related to on-the-job exposures. Bronchitis, obstructive pulmonary disease, and pulmonary fibrosis can all be associated with occupational exposure to various toxins, but the incidence is less than that of asthma. Ref: Beckett WS: Occupational respiratory diseases. N Engl J Med 2000 |
|
|
A 10-year-old white male is brought to your office with a chief complaint of “head congestion” associated with moderate malaise and a low-grade fever for 7 days. He has had a thick, discolored nasal discharge for the last 2 days. What's the appropriate next step?
|
No antibiotics should be used at this time
Clinical diagnosis of bacterial sinusitis requires the following: prolonged nonspecific upper respiratory signs and symptoms (i.e., rhinosinusitis and cough without improvement for >10–14 days), or more severe upper respiratory tract signs and symptoms (i.e., fever of 39 degrees C or higher, facial swelling, and facial pain). This individual does not meet these criteria, so antibiotics should not be used at this time. Although some believe that mucopurulent rhinitis (thick, opaque, or discolored nasal discharge) indicates the presence of bacterial sinusitis, this sign should be recognized as part of the natural course of a nonspecific, uncomplicated viral upper respiratory infection (URI). Sinus radiographs can demonstrate thickened mucosa, infundibular occlusion, and occasional air-fluid levels in uncomplicated viral URI. |
|
|
You are treating an 18-year-old white male college freshman for allergic rhinitis. It is September and he tells you that he has severe symptoms every autumn which impair his academic performance. He has a strongly positive family history of atopic dermatitis. Which medication is considered optimal treatment for this condition?
|
Intranasal glucocorticoids
Topical intranasal glucocorticoids are currently believed to be the most efficacious medications for the treatment of allergic rhinitis. They are far superior to oral preparations in terms of safety. Cromolyn sodium is also an effective topical agent for allergic rhinitis; however, it is more effective if started prior to the season of peak symptoms. Because of the high risk of rhinitis medicamentosa with chronic use of topical decongestants, these agents have limited usefulness in the treatment of allergic rhinitis. Some of the newer oral antihistamines have been found to be comparable in efficacy to intranasal steroids, but their use slightly increases the incidence of adverse effects and drug interactions. They are not as useful for congestion as for sneezing, pruritus, and rhinorrhea. Newer agents are relatively free of sedation. Overall, they are not as effective as topical glucocorticoids. Azelastine, an intranasal antihistamine, is effective in controlling symptoms but can cause somnolence and a bitter taste. |
|
|
You are caring for a 70-year-old male with widespread metastatic prostate cancer. Surgery, radiation, and hormonal therapy have failed to stop the cancer, and the goal of his care is now symptom relief. He is being cared for through a local hospice. Over the past few days he has been experiencing respiratory distress. His oxygen saturation is 94% on room air and his lungs are clear to auscultation. His respiratory rate is 16/min. Which medication would be best at this point?
|
Morphine
Dyspnea is a frequent and distressing symptom in terminally ill patients. In the absence of hypoxia, oxygen is not likely to be helpful. Opiates are the mainstay of symptomatic treatment. |
|
|
You diagnose sinusitis in a 7-year-old Hispanic male. He has been in good health otherwise, and has not been seen by a physician since his well care visit at age 6. What is recommended as initial antibiotic treatment?
|
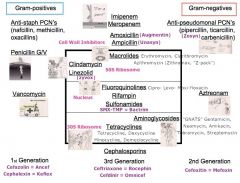
Amoxicillin
In the absence of any risk factors, approximately 80% of children with acute bacterial sinusitis will respond to treatment with amoxicillin. Risk factors for the presence of bacterial species that are likely to be resistant to amoxicillin include attendance at day care, antimicrobial treatment within the past 90 days, and age <2 years. The desire to continue to use amoxicillin as first-line therapy in patients suspected of having acute bacterial sinusitis relates to its general effectiveness, safety, tolerability, low cost, and narrow spectrum. |
|
|
At a routine annual visit, a healthy 65-year-old male is given pneumococcal vaccine. When should he receive a booster dose of this vaccine?
|
Never
If an otherwise healthy patient receives pneumococcal vaccine at age 65 or later, a second dose is not needed. If a healthy patient receives the vaccine before age 65, a second dose should be given after age 65 if at least 5 years have elapsed since the first dose. |
|
|
Residential and occupational exposure to radon is most closely linked with the development of:
|
Lung cancer
Radon is a naturally occurring, inert, radioactive gas which is a decay product of uranium. It can seep from soil beneath homes and reach concentrations in excess of the EPA standard of 4 picocuries. The EPA and the Surgeon General have recommended that all homes be tested for radon levels. Radon abatement measures can reduce radon concentration below EPA thresholds. Epidemiologic studies implicate radon as the second leading cause of lung cancer in the U.S., responsible for up to 30,000 of the 150,000 annual cases of bronchogenic cancer. Risk is heightened by concomitant exposure to tobacco smoke. |
|
|
What is the reason for the marked decline in the incidence of epiglottitis in the pediatric population?
|
Immunization with Haemophilus influenzae type b vaccine
The dramatic decrease in the incidence of epiglottitis is the result of routine vaccination with Haemophilus influenzae type b vaccine. This decreased incidence has also dramatically reduced morbidity and mortality. |
|
|
The mother of a 16-year-old male calls to report that her son has a severe sore throat and has been running a fever of 102 degrees F. What physical exam finding would be most specific for peritonsillar abscess?
|
Difficulty opening his mouth
Trismus is almost universally present with peritonsillar abscess. Voice change, otalgia, and odynophagia may or may not be present with peritonsillar abscess. Pharyngotonsillitis and peritonsillar cellulitis may also be associated with these complaints. Otalgia is common with peritonsillar abscess, otitis media, temporomandibular joint disorders, and a variety of other conditions. Peritonsillar abscess is rarely present without at least a 3-day history of progressive sore throat. |
|
|
A 7-year-old male presents with a 3-day history of sore throat, hoarseness, fever to 100 degrees (38 degrees C), and cough. Examination reveals injection of his tonsils, no exudates, and no abnormal breath sounds. What's the appropriate next step?
|
Recommend symptomatic treatment (don't have to do rapid strep test)
Pharyngitis is a common complaint, and usually has a viral cause. The key factors in diagnosing streptococcal pharyngitis are a fever over 100.4 degrees F, tonsillar exudates, anterior cervical lymphadenopathy, and absence of cough. Age plays a role also, with those <15 years of age more likely to have streptococcal infection, and those 10–25 years of age more likely to have mononucleosis. The scenario described is consistent with a viral infection, with no risk factors to make streptococcal infection likely; therefore, this patient should be offered symptomatic treatment for likely viral infection. Testing for other infections is not indicated unless the patient worsens or does not improve. |
|
|
A 7-year-old male with recurrent sinusitis has difficulty breathing through his nose. He has had chronic diarrhea and his weight is at the 5th percentile. Nasal polyps are noted on examination, in the form of grayish pale masses in both nares. No nasal purulence or odor is present. Which test should you order?
|
A sweat chloride test
This child has chronic diarrhea, recurrent sinusitis, and nasal polyps, and is underweight. Nasal polyps tend to occur more often in adult males, with the prevalence increasing in both sexes after age 50. Any child 12 years or younger who presents with nasal polyps should be suspected of having cystic fibrosis until proven otherwise. A sweat chloride test, along with a history and clinical examination, is necessary to evaluate this possibility. Nasal polyps are found in 1% of the normal population, but a full 18% of those with cystic fibrosis are afflicted. There is no association of polyps with Wilson’s disease, sarcoidosis, or emphysema, so serum ceruloplasmin, angiotensin-converting enzyme, and alpha1-antitrypsin levels would not be useful. An erythrocyte sedimentation rate likewise would yield limited information. |
|
|
An 84-year-old white female presents to your office with symptoms of an upper respiratory infection and a hacking cough. She admits to smoking one pack of cigarettes daily since she was 21 years of age. Which one of the following is true with regard to her tobacco use?
|
Sustained-release bupropion (Wellbutrin SR) has been shown to reduce the relapse rate for up to 12 months
Sustained-release bupropion has been shown to reduce the relapse rate for smoking cessation and blunt weight gain for 12 months. Beneficial effects of smoking cessation are seen even among older smokers. Evidence has now shown that smokers who switch to low-tar or low-nicotine cigarettes do not significantly decrease their health risks. The approved Food and Drug Administration medications for smoking cessation (sustained-release bupropion, nicotine patch, nicotine gum, nicotine inhaler, and nicotine nasal spray) have been shown to be safe and should be recommended for all patients without contraindications who are trying to quit smoking. The nicotine patch in particular is safe, and has been shown not to cause adverse cardiovascular effects. Ref: Fiore MC, Hatsukami DK, Baker TB: Effective tobacco dependence treatment. JAMA 2002 |
|
|
Which one of the following is true concerning control of mild persistent asthma in the pediatric population?
|

Inhaled anti-inflammatory agents, such as glucocorticoids or cromolyn sodium, should be used initially to maintain chronic control of asthma
Initial medications for the control of moderately severe asthma in children should include an anti-inflammatory agent, such as glucocorticoids or cromolyn. Cromolyn may be used safely in any pediatric age group, including infants. Ipratropium bromide is useful in the treatment of COPD but has very limited use for asthma. Inhaled beta-adrenergic agents should be used every 4 hours if needed. Overuse of these agents has been associated with an increased mortality rate. |
|
|
The local school district has found that there is asbestos in many of the classrooms. The asbestos is contained in ceiling material used as acoustical insulation. Which one of the following statements is true regarding this situation?
|
Workers removing the ceiling material without respiratory protection would have an increased risk of mesothelioma
Asbestos removal from public buildings is not mandated by the Environmental Protection Agency unless there is severe and extensive damage and there are no other options such as special repairs or encapsulation that will control fiber release. Asbestos exposure has been associated with a variety of cancers, including lung cancer, mesothelioma, cancer of the oropharynx, cancer of the larynx, and gastrointestinal cancer. Cigarette smoking amplifies the effects of asbestos exposure. Smoking, drug and alcohol abuse, improper diet, and inadequate exercise are all greater public health hazards than asbestos. Asthmatics, especially when exercising, can be influenced by a variety of inhaled irritants, including sulfur dioxide and acidic aerosols in concentrations present in many cities, but not including asbestos. |
|
|
Sleep apnea is known to be associated with:
|
Hypertension
Sleep apnea is associated with hypertension, and may in fact be a cause of hypertension. Improvement of sleep apnea can be associated with improved blood pressure. |
|
|
A 35-year-old male consults you about a vague chest pain he developed while sitting at his desk earlier in the day. The pain is right-sided and was sharp for a brief time when it began, but it rapidly subsided. There was no hemoptysis and the pain does not seem pleuritic. His physical examination, EKG, and oxygen saturation are unremarkable. A chest film shows a 10% right pneumothorax. Which one of the following is true in this situation?
|
Outpatient observation with a repeat chest radiograph in 24 hours is indicated
The majority of patients presenting with spontaneous pneumothorax are tall, thin individuals under 40 years of age. Most do not have clinically apparent lung disease, and the chest pain is sometimes minimal at onset and may resolve within 24 hours even if untreated. Patients with small pneumothoraces involving less than 15% of the hemithorax may have a normal physical examination, although tachycardia is occasionally noted. The diagnosis is confirmed by chest radiographs. Studies of recurrence have found that an average of 30% of patients will have a recurrence within 6 months to 2 years. The treatment of an initial pneumothorax of less than 20% may be monitored if a patient has few symptoms. Follow-up should include a chest radiograph to assess stability at 24–48 hours. Indications for treatment include progression, delayed expansion, or the development of symptoms. The majority of patients with spontaneous pneumothoraces, and perhaps almost all of them, will have subcutaneous bullae on a CT scan. |
|
|
A health-care worker has a negative tuberculin skin test (Mantoux method). A second test 10 days later is positive. This result indicates:
|
Long-standing, latent infection
A positive result on the second, but the not the first, step of a two-step Mantoux tuberculin skin test indicates long-standing, latent infection. |
|
|
In adults, what is the most likely cause of chronic, unilateral nasal obstruction?
|
Nasal septal deviation
The most common cause of nasal obstruction in all age groups is the common cold, which is classified as mucosal disease. Anatomic abnormalities, however, are the most frequent cause of constant unilateral obstruction. Of these, septal deviation is the most common. Foreign body impaction is an important, but infrequent, cause of unilateral obstruction and purulent rhinorrhea. Mucosal disease is usually bilateral and intermittent. Adenoidal hypertrophy is the most common tumor or growth to cause nasal obstruction, followed by nasal polyps, but both are less frequent than true anatomic causes of constant obstruction. |
|
|
A 6-year-old male is brought in for evaluation by his mother, who is concerned that he may have asthma. She reports that he coughs about 3 days out of the week and has a nighttime cough approximately 1 night per week. There is a family history of eczema and allergic rhinitis. Which one of the following would be the preferred initial treatment for this patient?
|

A low-dose inhaled corticosteroid such as budesonide (Pulmicort Turbuhaler)
The National Asthma Education and Prevention Program (NAEPP) updated its recommendations for the treatment of asthma in 2002. Treatment is based on asthma classification. This child meets the criteria for mild persistent asthma: symptoms more than 2 times per week but less than once a day, symptoms less than 2 nights per month, peak expiratory flow (PEF) or FEV1 >80% of predicted, and a PEF variability of 20%–30%. Asthma controller medications are recommended for all patients with persistent asthma, and the preferred long-term controller treatment in mild persistent asthma is a low-dose inhaled corticosteroid. Cromolyn, leukotriene modifiers, nedocromil, and sustained-release theophylline are alternatives, but are not preferred initial agents. Quick-acting, quick-relief agents such as short-acting beta-agonists are appropriate for prompt reversal of acute airflow obstruction. |
|
|
The treatment of choice for a 4-month-old infant with suspected pertussis is:
|
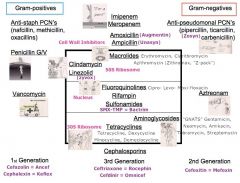
Erythromycin
In spite of widespread vaccination of infants, pertussis occurs endemically in 3- to 5-year cycles in the U.S. It appears to be more common within populations not routinely immunized, such as Mennonite communities, but can occur widely. Infants younger than 6 months are affected most severely, although pertussis occurs in all age groups. The diagnosis is made by nasopharyngeal culture, but because the disease is uncommon and the organism is fastidious, laboratory personnel should be advised of the physician’s suspicion of pertussis. Treatment includes respiratory and nutritional supportive care, particularly for infants younger than 6 months. Antibiotic therapy is most effective in shortening the illness when given early, during the upper respiratory phase, but is indicated at any stage to reduce the spread of disease to others. The drug of choice is erythromycin, 40–50 mg/kg/day divided into four doses, for 14 days. Also effective are azithromycin and clarithromycin, which may be better tolerated with improved compliance. Resistance to these agents is rare. Penicillins and cephalosporins are ineffective. Gentamicin is potentially very toxic, and is not indicated. |
|
|
An 83-year-old male has a long history of COPD. His resting oxygen saturation is 86% on room air. Treatment includes oral bronchodilators, inhaled corticosteroids, inhaled beta-agonists, inhaled cholinergics, and home oxygen. Which one of his treatments has been shown to prolong survival in cases such as this?
|

Home oxygen
Treatment of hypoxemia is critical in the management of COPD and trials have shown a reduction in mortality with the use of oxygen for 15 or more hours daily. Inhaled beta-adrenergic agonists and cholinergic agents, either alone or in combination, provide symptomatic relief but do not prolong survival. Theophylline can be used for symptoms inadequately relieved by bronchodilators. Inhaled corticosteroids do not appear to alter the rate of decline in lung function in COPD. However, some evidence shows that these agents alleviate symptoms and reduce disease exacerbation. Pulmonary rehabilitation improves quality of life and reduces hospitalizations. |
|
|
What would be the most appropriate empiric therapy for nursing home–acquired pneumonia in a patient with no other underlying disease?
|
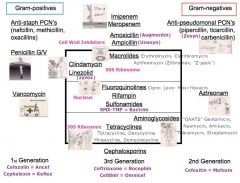
Levofloxacin (Levaquin)
The major concern with regard to pneumonia in the nursing-home setting is the increased frequency of oropharyngeal colonization by gram-negative organisms. In the absence of collectible or diagnostic sputum Gram’s stains or cultures, empiric therapy must cover Streptococcus pneumoniae, Staphylococcus aureus, Haemophilus influenzae, and gram-negative bacteria. Levofloxacin is the best single agent for providing against this spectrum of organisms. |
|
|
Which one of the following unimmunized patients should receive two doses of influenza vaccine?
|
A 5-year-old with asthma
Two doses of influenza vaccine are recommended for children under the age of 9 years unless they have been vaccinated previously. Children 3–8 years of age should receive one or two 0.5-mL doses of split-virus vaccine intramuscularly. |
|
|
A 50-year-old male who is a heavy smoker asks you about vitamin supplementation to prevent cancer and cardiovascular disease. The patient is unwilling to stop smoking. According to the 2003 recommendations of the U.S. Preventive Services Task Force, which one of the following is true regarding vitamin supplementation in adults who are middle-age or older?
|
Large supplemental doses of ~17beta-carotene may increase the risk of lung cancer in heavy smokers
The U.S. Preventive Services Task Force found that beta-carotene supplementation provides no benefit in the prevention of cancer in middle-aged and older adults. In two trials limited to heavy smokers, supplementation with beta-carotene was associated with a higher incidence of lung cancer and all-cause mortality. In general, little evidence was found to determine whether supplementation of any of the mentioned vitamins reduces the risk of cardiovascular disease or cancer. |
|
|
In the elderly, which measures of pulmonary function is characteristically increased?
|
Functional residual capacity
Although vital capacity declines with age, total lung capacity remains constant. The reduction in vital capacity results from an increase in residual volume. This increase in residual volume and functional residual capacity results from the collapse of small airways that occurs at higher lung volumes as age increases. Residual volume increases nearly 50% between early adulthood and age 70. In addition, standard spirometric measurements of lung function (i.e., forced expiratory volume in 1 second, peak expiratory flow rate, and maximal expiratory flow volume) have been shown to decline with age. Arterial oxygen tension also slowly declines with age. |
|
|
Which one of the following is true regarding PPD testing for tuberculosis?
|
Patients who have converted within the past year should be treated, regardless of age
Because the risk of developing active disease is highest in patients within 2 years after conversion, recent converters should generally be treated regardless of age. BCG vaccination has a limited effect on PPD reactivity; tests should not be interpreted any differently in patients who have previously received BCG. The use of a two-step approach (i.e., retesting 1–4 weeks later in patients who initially test negative) is designed to decrease the false-negative rate of PPD testing. The significance of a positive result on either phase of the test is the same. Patients who are HIV positive are at higher risk for false-negative PPDs and active disease, but PPD testing is not contraindicated. |
|
|
A 4-year-old child returns to your clinic after 3 days of treatment for acute otitis media. She had been taking amoxicillin, 40 mg/kg/day, and using acetaminophen and ibuprofen for pain and fever. On examination, the child still has a bulging red tympanic membrane on the left, with a flat tympanogram. She has continued to have a fever. Which antibiotic would be contraindicated?
A. Amoxicillin/clavulanate (Augmentin) orally B. Ceftriaxone (Rocephin) intramuscularly C. Cefuroxime (Ceftin) orally D. Ciprofloxacin (Cipro) orally E. Clindamycin (Cleocin) orally |
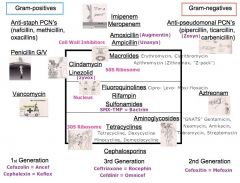
Ciprofloxacin (Cipro) orally
All of these medications listed are indicated for second-line treatment of acute otitis media. Ciprofloxacin, however, is not approved for patients under age 18. |
|
|
You see a 90-year-old male with a 5-year history of progressive hearing loss. The most common type of hearing loss at this age affects:
|
Predominantly high frequencies
In the geriatric population, presbycusis is the most common cause of hearing loss. Patients typically have the most difficulty hearing higher frequencies such as consonants. Lower-frequency sounds such as vowels are preserved. |
|
|
A 4-year-old Hispanic female has been discovered to have a congenital hearing loss. Her mother is an 18-year-old migrant farm worker who is currently at 8 weeks' gestation with her second pregnancy. The mother has been found to have cervical dysplasia on her current Papanicolaou (Pap) smear and has also tested positive for Chlamydia. The most likely cause of this child’s hearing loss is:
|
Cytomegalovirus
Cytomegalovirus (CMV) is the most common congenital infection and occurs in up to 2.2% of newborns. It is the leading cause of congenital hearing loss. The virus is transmitted by contact with infected blood, urine, or saliva, or by sexual contact. Risk factors for CMV include low socioeconomic status, birth outside North America, first pregnancy prior to age 15, a history of cervical dysplasia, and a history of sexually transmitted diseases. Infection can be primary or a reactivation of a previous infection. While the greatest risk of infection is during the third trimester, those occurring in the first trimester are the most dangerous to the fetus. |
|
|
Within a 2-week period you see an unusually large number of patients of all ages who complain of painless loss of central vision. You refer them appropriately to an ophthalmologist. The feedback you get is that most of these persons have bilateral central scotomas caused by an ophthalmoscopically visible macular defect. Which one of the following events would most likely explain this problem?
|
A solar eclipse
Direct observation of the sun without an adequate filter, which often occurs during a solar eclipse, results in a specific type of radiation injury termed solar (eclipse) retinopathy. The lens system of the eye focuses the sun’s light onto a small spot on the macula, usually in one eye only, producing a thermal burn. The resulting retinal edema may clear spontaneously with minor functional loss, or it may cause significant tissue atrophy, leaving a defect seen with an ophthalmoscope as a macular hole. This macular injury produces a permanent central scotoma. Visual blurring and difficulty with light perception are reversible manifestations of the tissue hypoxia associated with carbon monoxide poisoning. Dust and other particulate matter can produce injury to the cornea and conjunctiva. These lesions are painful, usually prompting medical attention and appropriate treatment. While severe contusions to the globe and periorbital structures can produce retinal detachment, the clinical vignette does not support a boxing-type injury. Although potatoes have eyes, there is no other significant relationship between potato salad and ophthalmologic disease. |
|
|
A 73-year-old white male who is otherwise in good health noted a sudden shower of flashing lights before his left eye a few hours ago. He has never had this symptom before. The most likely diagnosis is:
|
Retinal detachment
While all of the conditions listed are associated with flashing light before the eyes, a sudden shower of flashing lights is highly suggestive of retinal detachment. Migraine syndrome rarely begins in the eighth decade, vitreous floaters are more likely to be perceived as spots rather than lights, and central retinal vein thrombosis would likely cause more loss of vision. Emergency referral to an ophthalmologist is mandatory in cases of probable retinal detachment. |
|
|
Which one of the following is the most common risk factor for retinal detachment?
|
Posterior detachment of the vitreous
Vitreous detachment is very common after age 60 and occurs frequently in younger persons with myopia. The separation of the posterior aspect of the vitreous from the retina exerts traction on the retina, with the attendant risks of a retinal tear and detachment. Symptoms of retinal detachment may include light flashes (photopsia), a sudden appearance or increase in “floaters,” or peripheral visual field loss, any of which should prompt an ophthalmology referral. Cataract surgery can result in premature shrinkage of the vitreous and thereby poses an increased risk, but vitreous detachment resulting from other processes is more common. Hyphema, glaucoma, and diabetic retinopathy are not specific risk factors for retinal detachment. |
|
|
What is the most common cause of visual loss in children?
|
Amblyopia
Evaluation of visual symptoms in children can be challenging, but is important for identifying correctable conditions. Amblyopia, or “lazy eye,” is the most common cause of visual loss, with a prevalence of 2% in childhood. It is often related to strabismus, in which the image from one eye is suppressed in order to eliminate diplopia. Iritis is unusual and may have minimal symptoms; it is frequently associated with juvenile rheumatoid arthritis. Glaucoma does occur in children, often after cataract surgery. Eye trauma is relatively common, especially in boys. They may sustain abrasions, foreign bodies and penetrating injuries. Conjunctivitis will usually resolve without visual loss except when complicated by keratitis, such as in herpetic infections. |
|

A 16-year-old white female experiences the sudden onset of tender, bleeding gums, malodorous breath, and a bad taste in her mouth. On examination she is febrile and has cervical lymphadenopathy and tachycardia. Her mouth has marginal punched-out, crater-like depressions of the interdental gingival papillae and gingival margins that are covered with a gray pseudomembranous slough. The drug of choice for treating this condition is:
|
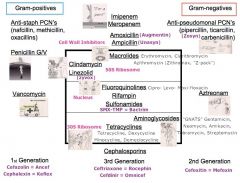
Penicillin
This patient has acute necrotizing ulcerative gingivitis. The onset is sudden and findings include tender, bleeding gums, malodorous breath, and a bad taste in the mouth. The disease is frequently associated with systemic findings such as fever, anorexia, malaise, tachycardia, cervical lymphadenopathy, and leukocytosis. Characteristic gingival lesions are seen, appearing as marginal punched-out, crater-like depressions of the interdental gingival papillae and gingival margin. They are covered with a gray pseudomembranous slough that is demarcated from the remainder of the gingiva and bleeds when removed. These lesions may be related to a single tooth, a group of teeth, or the gingiva throughout the mouth. Management includes removing predisposing factors such as stress, fatigue, heavy smoking, and poor nutrition that can cause tissue breakdown. Mouth rinses with warm half-strength hydrogen peroxide are useful. When fever and lymphadenopathy occur, antibiotic treatment is warranted and penicillin is the drug of choice. Tetracycline and erythromycin are good alternatives. |
|
|
A 25-year-old male has a dental infection associated with facial swelling and lymphadenopathy. Which one of the following is the most appropriate antibiotic?
|
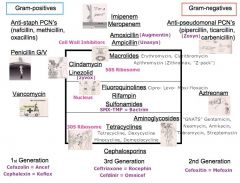
Penicillin
Dental infections complicated by the development of cellulitis should be treated with oral antibiotic therapy. The antibiotic of choice is penicillin. Clindamycin should be used if a patient is allergic to penicillin. |
|
|
A 42-year-old African-American male recently traveled to the Caribbean for a scuba diving trip. Since his return he has noted brief intermittent episodes of vertigo not associated with nausea or vomiting. He is concerned, however, because these episodes occurred after sneezing or coughing and then a couple of times after straining while lifting something. He has had no hearing loss, and no vertigo with positional changes such as bending over or turning over in bed. The most likely cause of this patients vertigo is
|
a perilymphatic fistula
A perilymphatic fistula between the middle and inner ear may be caused by barotrauma from scuba diving, as well as by direct blows, heavy weight bearing, and excessive straining (e.g., with sneezing or bowel movements.) This patients recent trip involved two of these potential factors. Vestibular neuronitis is a more sudden, unremitting syndrome. Menieres disease is manifested by episodes of vertigo, associated with hearing loss and often with nausea and vomiting. Benign paroxysmal positional vertigo is more likely in older individuals, and is associated with postural change. Multiple sclerosis requires symptoms in multiple areas and is not thought to be provoked by climate change. |
|
|
What insulin regimens most closely mimics the normal pattern of pancreatic insulin release in a nondiabetic person?
|
Insulin detemir (Levamir) daily plus rapid-acting insulin with meals
Basal insulin provides a relatively constant level of insulin for 24 hours, with an onset of action in 1 hour and no peak. NPH gives approximately 12 hours of coverage with a peak around 6–8 hours. Regular insulin has an onset of action of about 30 minutes and lasts about 5–8 hours, with a peak at about 2–4 hours. New rapid-acting analogue insulins have an onset of action within 5–15 minutes, peak within 30–75 minutes, and last only about 2–3 hours after administration. Thus, a 70/30 insulin mix (typically 70% NPH and 30% regular) provides coverage for 12 hours, but the peaks of insulin release do not closely mimic natural patterns. NPH given twice daily along with an insulin sliding-scale protocol using regular insulin is only slightly closer than a 70/30 twice-daily regimen. Rapid insulin alone does not provide any basal insulin, and the patient would therefore not have insulin available during the night. |
|
|
In a patient with a severe anaphylactic reaction to peanuts, the most appropriate route for epinephrine is:
|
intramuscular
Intramuscular epinephrine is the recommended drug for anaphylactic reactions (SOR A). Epinephrine is absorbed more rapidly intramuscularly than subcutaneously. |
|
|
A 19-year-old college student comes to your office with significant pain in his right great toe that is making it difficult for him to walk. He has never had this problem before.
When you examine him you find increased swelling with marked erythema and seropurulent drainage and ulceration of the medial nail fold. The toe is very tender to touch, particularly when pressure is applied to the tip of the toe. The most appropriate initial management would be: |
partial avulsion of the medial nail plate and phenolization of the matrix at this visit
This ingrown nail meets the criteria for moderate severity: increased swelling, seropurulent drainage, infection, and ulceration of the nail fold. In these cases, antibiotics before or after phenolization of the matrix do not decrease healing time, postoperative morbidity, or recurrence rates (SOR B). A conservative approach, elevating the nail edge with a wisp of cotton or a gutter splint, is reasonable in patients with a mild to moderate ingrown toenail who do not have significant pain, substantial erythema, or purulent drainage. Either immediate partial nail avulsion followed by phenolization, or direct surgical excision of the nail matrix is effective for the treatment of ingrown nails (SOR B). Pretreatment with soaking and antibiotics has not been demonstrated to add therapeutic benefit or to speed resolution. Several studies demonstrate that once the ingrown portion of the nail is removed and matricectomy is performed, the localized infection will resolve without the need for antibiotic therapy. Bilateral partial matricectomy maintains the functional role of the nail plate (although it narrows the nail plate) and should be considered in patients with a severe ingrown toenail or to manage recurrences. |
|
|
A 59-year-old male who is morbidly obese suffers a cardiac arrest. Intravenous access cannot be obtained. Which one of the following is true regarding intraosseous drug administration in this patient?
|
There are no contraindications to intraosseous administration in this patient
The current American Heart Association ACLS guidelines state that intraosseous access can be obtained in almost all age groups rapidly, and is preferred over the endotracheal route. Any drug that can be administered intravenously can be administered intraosseously. Many drugs administered via an endotracheal tube are poorly absorbed, and drug levels vary widely. |
|
|
Ultrasonography shows a complete placenta previa in a 23-year-old primigravida at 20 weeks gestation. She has not experienced any vaginal bleeding. Which one of the following would be the most appropriate management for this patient?
|
Repeat the ultrasonography at 28 weeks gestation
Placenta previa is a relatively common incidental finding on second trimester ultrasonography. Approximately 4% of ultrasound studies at 20–24 weeks gestation show a placenta previa, but it occurs in only 0.4% of pregnancies at term, because of migration of the placenta away from the lower uterine segment. Therefore, in the absence of bleeding, the most appropriate management is to repeat the ultrasonography in the third trimester (SOR A). Because many placenta previas resolve close to term, a decision regarding mode of delivery should not be made until after ultrasonography is performed at 36 weeks gestation. Digital cervical examinations should not be performed in patients with known placenta previa because of the risk of precipitating bleeding. Corticosteroids are indicated at 24–34 weeks gestation if the patient has bleeding, given the higher risk of premature birth. In patients with a history of previous cesarean delivery who have a placenta previa at the site of the previous incision, a color-flow Doppler study should be performed to evaluate for a potential placenta accreta. In such cases, MRI may be helpful to confirm the diagnosis. |
|
|
What class of diabetes medications acts primarily by stimulating pancreatic insulin secretion?
|
Sulfonylureas, such as glipizide (Glucotrol)
Biguanides and thiazolidinediones are insulin sensitizers that decrease hepatic glucose production and increase insulin sensitivity. Sulfonylureas and meglitinides stimulate pancreatic insulin secretion, while DPP-4 inhibitors prevent GLP-1 breakdown and slow the breakdown of some sugars. GLP-1 mimetics stimulate insulin secretion, suppress glucagon secretion, and promote β-cell production. Amylin analogs act with insulin to delay gastric emptying and they also inhibit glucagon release. |
|
|
A 30-year-old male presents with a 3-week history of severe, burning pain in his right shoulder. He recalls no mechanism of injury. An examination reveals weakness to resistance of the biceps and triceps, and with external rotation of the shoulder. Full range of motion of the neck and shoulder does not worsen the pain.
Which one of the following would be most likely to identify the cause of this patient’s problem? |
Electromyography and nerve conduction studies
This patient has brachial neuritis, which can be difficult to differentiate from cervical radiculopathy, shoulder pathology, and cerebrovascular accident. The pain preceded the weakness, no trauma was involved, and the weakness is in a nondermatomal distribution, making brachial neuritis the most likely diagnosis. Electromyography is most likely to show this lesion, but only after 3 weeks of symptoms. MRI of the neck may show abnormalities, but not the cause of the current problem. Symptoms are not consistent with shoulder pathology, deep-vein thrombosis of the upper extremity, or cerebrovascular accident. |
|
|
A 30-year-old African-American female is being evaluated because of absent menses for the last 6 months. Menarche was at age 12. Her menstrual periods have frequently been irregular, and are accompanied only occasionally by dysmenorrhea. She had her first child 4 years ago, but has not been able to become pregnant since. A physical examination and pelvic examination are unremarkable. A serum pregnancy test is negative, prolactin levels are normal, and LH and FSH levels are both three times normal on two occasions.
These findings are consistent with: |
ovarian failure
The history and physical findings in this patient are consistent with all of the conditions listed. However, the elevated FSH and LH indicate an ovarian problem, and this case is consistent with ovarian failure or premature menopause. Most pituitary tumors associated with amenorrhea produce hyperprolactinemia. Polycystic ovary syndrome usually results in normal to slightly elevated LH levels and tonically low FSH levels. Hypothalamic amenorrhea is a diagnosis of exclusion, and can be induced by weight loss, excessive physical exercise (running, ballet), or systemic illness. It is associated with tonically low levels of LH and FSH. |
|
|
A 30-year-old female presents to your office for an initial visit. She reports a long history of asthma that currently awakens her three times per month, necessitating the use of an albuterol inhaler (Proventil, Ventolin).
According to current guidelines, which one of the following would be optimal treatment? |

Adding a low-dose inhaled corticosteroid
Inhaled corticosteroids improve asthma control more effectively in children and adults than any other single long-term controller medication (SOR A). This patient has mild persistent asthma and should be treated with a low-dose inhaled corticosteroid. |
|
|
A 26-month-old child presents with a 2-day history of 6–8 loose stools per day and a low-grade fever. When evaluating the child to determine whether he is dehydrated, which one of the following would NOT be useful?
A. Skin turgor B. Capillary refill time C. Respiratory rate and pattern D. The BUN/creatinine ratio E. The serum bicarbonate level |
The BUN/creatinine ratio
The most useful findings for identifying dehydration are prolonged capillary refill time, abnormal skin turgor, and abnormal respiratory pattern (SOR C). Capillary refill time is not affected by fever and should be less than 2 seconds. Skin recoil is normally instantaneous, but recoil time increases linearly with the degree of dehydration. The respiratory pattern should be compared with age-specific normal values, but will be increased and sometimes labored, depending on the degree of dehydration. Unlike in adults, calculation of the BUN/creatinine ratio is not useful in children. Although the normal BUN level is the same for children and adults, the normal serum creatinine level changes with age in children. In combination with other clinical indicators, a low serum bicarbonate level (<17 mmol/L) is helpful in identifying children who are dehydrated, and a level <13 mmol/L is associated with an increased risk of failure of outpatient rehydration efforts. |
|
|
A 70-year-old Asian male presents with hematochezia. He has stable vital signs. Lower endoscopy is performed, but is unsuccessful due to active bleeding.
What's the appropriate next step at this point? |
A technetium-99m blood pool scan
In most patients with heavy gastrointestinal bleeding, localizing the bleeding site, rather than diagnosing the cause of the bleeding, is the most important task. A lower GI series is usually nondiagnostic during heavy, active bleeding. A small-bowel radiograph may be helpful after the active bleeding has stopped, but not during the acute phase of the bleeding. A blood pool scan allows repeated scanning over a prolonged period of time, with the goal of permitting enough accumulation of the isotope to direct the arteriographer to the most likely source of the bleeding. If the scan is negative, arteriography would be unlikely to reveal the active source of bleeding, and is also a more invasive procedure. Exploratory laparotomy may be indicated if a blood pool scan or an arteriogram is nondiagnostic and the patient continues to bleed heavily. |
|
|
A patient presenting with severe carbon monoxide poisoning should be treated with:
|
oxygen
Patients with carbon monoxide poisoning should be treated immediately with normobaric oxygen, which speeds up the excretion of carbon monoxide. |
|
|
A patient who underwent coronary bypass grafting several months ago has been intolerant of all medications for cholesterol lowering. However, on the recommendation of a friend, he began taking red yeast rice that he purchased at a natural healing store. His cholesterol level has improved with this product and he has tolerated it so far.
You should consider monitoring which laboratory test in this patient, based on the active ingredient in red yeast rice? |
Liver enzymes
Red yeast rice (Monascus purpureus) is a widely available dietary supplement that has been used as an herbal medication in China for centuries. In recent years it has been used for alternative management of hyperlipidemia in the U.S. Extracts of red yeast rice contain several active ingredients, including monacolin K and other monacolins, that have HMG-CoA reductase inhibitory activity and are considered to be naturally occurring forms of lovastatin. Red yeast rice extract lowers total cholesterol, LDL-cholesterol, and triglycerides. It may be useful for patients unable to tolerate statins due to myalgias, but requires periodic monitoring of liver enzymes because its metabolic effects and potential for consequences are similar to those of statins. |
|
|
A 40-year-old nurse presents with a 1-year history of rhinitis, and a more recent onset of episodic wheezing and dyspnea. Her symptoms seem to improve when she is on vacation. She does not smoke, although she says that her husband does. Her FEV1 improves 20% with inhaled β-agonists.
Which one of the following is the most likely diagnosis? |
Occupational asthma
Occupational asthma merits special consideration in all cases of new adult asthma or recurrence of childhood asthma after a significant asymptomatic period (SOR C). Occupational asthma is often preceded by the development of rhinitis in the workplace and should be considered in patients whose symptoms improve away from work. Reversibility with β-agonist use makes COPD less likely, in addition to the fact that the patient is a nonsmoker. Cystic fibrosis is not a likely diagnosis in a patient this age with a long history of being asymptomatic. Sarcoidosis would be less likely to cause reversible airway obstruction and intermittent symptoms. Vocal cord dysfunction would not be expected to respond to bronchodilators. |
|
|
A previously healthy 60-year-old male is diagnosed with multiple myeloma after a workup for an incidental finding on routine laboratory work. He has no identified organ or tissue damage and is asymptomatic.
What would be appropriate treatment of this patient’s condition? |
No treatment
This patient has smoldering (asymptomatic) multiple myeloma. He does not have any organ or tissue damage related to this disease and has no symptoms. Early treatment of these patients does not improve mortality (SOR A) and may increase the likelihood of developing acute leukemia. The standard treatment for symptomatic patients under age 65 is autologous stem cell transplantation. Patients over 65 who are healthy enough to undergo transplantation would also be appropriate candidates. Patients who are not candidates for autologous stem cell transplantation generally receive melphalan and prednisolone with or without thalidomide. Radiotherapy can be used to relieve metastatic bone pain or spinal cord compression. |
|
|
A 35-year-old male presents with a 4-month history of pain in the lower lumbar region without radiation. He works in retail sales, and the pain and stiffness prevent him from working. He estimates the pain to be 7 on a 10-point scale. He has been under the care of a chiropractor and has experienced some relief with spinal manipulation. His history is negative for red flags indicating a serious cause for his pain.
The only positive findings on a physical examination are diffuse mild tenderness over the lumbar region and mild limitation of lumbar mobility on forward and lateral flexion/extension maneuvers. Appropriate laboratory tests and imaging studies are all within normal limits. In addition to appropriate analgesics, which one of the following modalities has the best evidence of long-term benefit in this situation? |
Multidisciplinary rehabilitation
This patient has nonspecific chronic back pain, most likely a lumbar strain or sprain. In addition to analgesics (e.g., acetaminophen or NSAIDs) (SOR A) and spinal manipulation (SOR B), a multidisciplinary rehabilitation program is the best choice for management (SOR A). This program includes a physician and at least one additional intervention (psychological, social, or vocational). Such programs alleviate subjective disability, reduce pain, return the person to work earlier, and reduce the amount of sick time taken in the first year by 7 days. Benefits persist for up to 5 years. Back school, TENS, and SSRIs have been found to have negative or conflicting evidence of effectiveness (SOR C). There is no evidence to support the use of epidural corticosteroid injections in patients without radicular signs or symptoms (SOR C). |
|
|
A 55-year-old male presents to your office for evaluation of increasing dyspnea with exertion over the past 2 weeks. He has smoked 2 packs of cigarettes per day since the age of 20. He has had a chronic cough for years, along with daily sputum production. He was given an albuterol inhaler for wheezing in the past, which he uses intermittently. On examination he has a severe decrease in breath sounds, no evidence of jugular venous distention, no cardiac murmur, and no peripheral edema. A chest film shows hyperinflation, but no infiltrates or pleural effusion. Office spirometry shows that his FEV1 is only 55% of the predicted value.
You consider using inhaled corticosteroids as part of the treatment regimen for this patient. This has been shown to: |

increase the risk of pneumonia
COPD has several symptoms, including poor exercise tolerance, chronic cough, sputum production, dyspnea, and signs of right-sided heart failure. The most common etiology is cigarette smoking. A patient with any combination of two of these findings, such as a 70-pack-year history of smoking, decreased breath sounds, or a history of COPD, likely has airflow obstruction, defined as an FEV1 ≤60% of the predicted value. In stable COPD, treatment is reserved for patients who have symptoms and airflow obstruction. Treatment options for monotherapy are all similar in effectiveness and include long-acting inhaled anticholinergics, long-acting β-agonists, and inhaled corticosteroids. Inhaled corticosteroids will not reduce mortality or affect long-term progression of COPD. However, they do reduce the number of exacerbations and the rate of decline in the quality of life. There appears to be no increase in cataract formation or rate of fracture. These agents do have side effects, including candidal infection of the oropharynx, hoarseness, and an increased risk of developing pneumonia. |
|
|
Which one of the following patients is unlikely to benefit from vaccination against hepatitis A?
A. A missionary traveling to Mexico B. A man who has sex with men C. A methamphetamine addict D. A patient with chronic hepatitis E. A 40-year old recent immigrant from India |
A 40-year old recent immigrant from India
Each of the individuals listed is at increased risk for hepatitis A infection or its complications, except for the Indian immigrant. Hepatitis A is so prevalent in developing countries such as India that virtually everyone is infected by the end of childhood, and therefore immune. Infection with hepatitis A confers lifelong immunity, so an adult from a highly endemic area such as India has little to gain from vaccination. |
|
|
For a healthy 1-month-old, daily vitamin D intake should be:
|
400 IU
It is now recommended that all infants and children, including adolescents, have a minimum daily intake of 400 IU of vitamin D, beginning soon after birth. The current recommendation replaces the previous recommendation of a minimum daily intake of 200 IU/day of vitamin D supplementation beginning in the first 2 months after birth and continuing through adolescence. These revised guidelines for vitamin D intake for healthy infants, children, and adolescents are based on evidence from new clinical trials and the historical precedent of safely giving 400 IU of vitamin D per day in the pediatric and adolescent population. New evidence supports a potential role for vitamin D in maintaining innate immunity and preventing diseases such as diabetes mellitus and cancer. |
|
|
A 68-year-old male was seen in a local urgent-care clinic 6 days ago for upper respiratory symptoms and was started on cefuroxime (Ceftin). He presents to your office with a 2-day history of 4–5 watery stools per day with no blood or mucus. He is afebrile and has a normal abdominal and rectal examination. A stool guaiac test is negative, and a stool sample is sent for further testing.
What is the best initial management for this patient? |
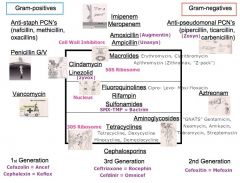
Stop the cefuroxime
This patient is at high risk for Clostridium difficile–associated diarrhea, based on his age and his recent broad-spectrum antibiotic use. The initial management is to stop the antibiotics. Treatment should not be initiated unless the stool is positive for toxins A and B. The recommended initial treatment for C. difficileenteritis is oral metronidazole. Probiotics may be useful for prevention, but their use is controversial. Loperamide should be avoided, as it can slow down transit times and worsen toxin-mediated diarrhea. |
|
|
A 74-year-old female presents with a several-month history of gradually increasing dyspnea on exertion, swelling in her feet and lower legs, and having to sleep sitting up due to increased shortness of breath while lying flat. She has been healthy otherwise, with no known heart disease or hypertension, and she has no significant family history of heart disease. An echocardiogram shows an ejection fraction of 20% and a thin-walled, diffusely enlarged left ventricle.
Which one of the following is the most likely diagnosis? |
Dilated cardiomyopathy
This patient’s symptoms and echocardiographic findings indicate a dilated cardiomyopathy. In patients with hypertrophic cardiomyopathy the echocardiogram shows left ventricular hypertrophy and a reduction in chamber size. In restrictive cardiomyopathy, findings include reduced ventricular volume, normal left ventricular wall thickness, and normal systolic function with impaired ventricular filling. Arrhythmogenic right ventricular cardiomyopathy usually presents with syncope and without symptoms of heart failure, and segmental wall abnormalities would be seen on the echocardiogram. Highly trained athletes may develop echocardiographic evidence of eccentric cardiac hypertrophy, but no symptoms of heart failure would be present. |
|
|
Which one of the following is true regarding treatment of pressure ulcers?
|
Topical antibiotics should not be used for more than 2 weeks at a time
Trials have not definitively shown that nutritional supplements speed ulcer healing. The head of the bed should be elevated only as necessary, and should be kept to less than 30° to reduce shearing forces.Systemic antibiotics should only be used for cellulitis, osteomyelitis, and bacteremia. Topical antibiotics may be used for periods of up to 2 weeks (SOR C). |
|
|
The “Get Up and Go Test” evaluates for what?
|
Risk of falling
The “Get Up and Go Test” is the most frequently recommended screening test for mobility. It takes less than a minute to perform and involves asking the patient to rise from a chair, walk 10 feet, turn, return to the chair, and sit down. Any unsafe or ineffective movement with this test suggests balance or gait impairment and an increased risk of falling. If the test is abnormal, referral to physical therapy for complete evaluation and assessment should be considered. Other interventions should also be considered, such as a medication review for factors related to the risk of falling. |
|
|
A 20-year-old male presents with a complaint of pain in his right testis. The onset of pain has been gradual and has been associated with dysuria and urinary frequency. The patient has no medical problems and is sexually active. On examination he has some swelling and mild tenderness of the testis. The area posterior to the testis is swollen and very tender. He has a normal cremasteric reflex, and the pain improves with elevation of the testicle.
Which one of the following would be the most appropriate management of this patient? |
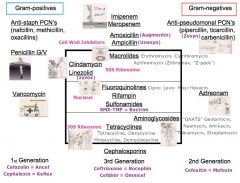
Ceftriaxone (Rocephin) and doxycycline
This patient has epididymitis. In males 14–35 years of age, the most common causes are Neisseria gonorrhoeae and Chlamydia trachomatis. The recommended treatment in this age group is ceftriaxone, 250 mg intramuscularly, and doxycycline, 100 mg twice daily for 10 days (SOR C). A single 1-g dose of azithromycin may be substituted for doxycycline. In those under age 14 or over age 35, the infection is usually caused by one of the common urinary tract pathogens, and levofloxacin, 500 mg once daily for 10 days, would be the appropriate treatment (SOR C). If there is concern about testicular torsion, urgent surgical evaluation and ultrasonography are appropriate. Testicular torsion is most common between 12 and 18 years of age but can occur at any age. It usually presents with an acute onset of severe pain and typically does not have associated urinary symptoms. On examination there may be a high-riding transversely oriented testis with an abnormal cremasteric reflex and pain with testicular evaluation. Color Doppler ultrasonography will show a normal-appearing testis with decreased blood flow. |
|
|
An elevation of serum alkaline phosphatase combined with an elevation of 5'-nucleotidase is most suggestive of conditions affecting which organ?
|
the liver
Alkaline phosphatase is elevated in conditions affecting the bones, liver, small intestine, and placenta. The addition of elevated 5'-nucleotidase suggests the liver as the focus of the problem. Measuring 5'-nucleotidase to determine whether the alkaline phosphatase elevation is due to a hepatic problem is well substantiated, practical, and cost effective (SOR C). |
|
|
A 60-year-old right-handed white male arrives in the emergency department with symptoms and signs consistent with a stroke. His past medical history is significant for tobacco abuse and chronic treated hypertension. He is alert and afebrile. His pulse rate is 100 beats/min, respirations 20/min, and blood pressure 190/95 mm Hg. He has a moderate right-sided hemiparesis and is aphasic. There are no other significant physical findings.
While appropriate tests are being ordered, immediate management in the emergency department should include which one of the following? |
Monitoring oxygenation status with pulse oximetry
Maintaining adequate tissue oxygenation is an important component of the emergency management of stroke. Hypoxia leads to anaerobic metabolism and depletion of energy stores, increasing brain injury. While there is no reason to routinely administer supplemental oxygen, the potential need for oxygen should be assessed using pulse oximetry or blood gas measurement. Overzealous use of antihypertensive drugs is contraindicated, since this can further reduce cerebral perfusion. In general, these drugs should not be used unless mean blood pressure is >130 mm Hg or systolic blood pressure is >220 mm Hg. Antithrombotic drugs such as heparin must be used with caution, and only after intracerebral hemorrhage has been ruled out by baseline CT followed by repeat CT within 48–72 hours. Hypovolemia can exacerbate cerebral hypoperfusion, so there is no need to restrict fluid intake. Optimization of cardiac output is a high priority in the immediate hours after a stroke. Based on data from randomized clinical trials, corticosteroids are not recommended for the management of cerebral edema and increased intracranial pressure after a stroke |
|
|
Which one of the following is the most common secondary cause of nephrotic syndrome in adults?
|
Diabetes mellitus
Although most cases of nephrotic syndrome are caused by primary kidney disease, the most common secondary cause of nephrotic syndrome in adults is diabetes mellitus. Other secondary causes include systemic lupus erythematosus, hepatitis B, hepatitis C, NSAIDs, amyloidosis, multiple myeloma, HIV, and preeclampsia. Primary causes include membranous nephropathy and focal segmental glomerulosclerosis, each accounting for approximately one third of cases. |
|
|
A 19-year-old college student comes to your office with her mother. The mother reports that her daughter has frequently been observed engaging in binge eating followed by induced vomiting. She has also admitted to using laxatives to prevent weight gain.
What electrolyte abnormality is most likely to be found in this patient? |
Hypokalemia
The patient described is likely suffering from bulimia. These patients use vomiting, laxatives, or diuretics to prevent weight gain after binge eating. This often causes a loss of potassium, leading to weakness, cardiac arrhythmias, and respiratory difficulty. The levels of other electrolytes are not as dramatically affected. |

