![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
416 Cards in this Set
- Front
- Back
|
pulmonary disease
|
asthma, COPD, bronchiectasis (shared etiology: inflammation, shared symptom: dyspnea)
|
|
|
airway obstruction
|
worse airway obstruction with exhalation
|
|
|
airway obstruction etiology
|
loss of structural support for small bronchi and bronchioles, constriction of bronchial smooth muscles, accumulation of mucus
|
|
|
asthma risk factors
|
genetics, fan hx, rsv, gender (female after adolescence), obesity, exposed to allergens/irritants, maternal smoking/smoking environment, low SES, LBW or premature
|
|
|
asthma variants
|
atopic, occupational, viral infections, asa/nsaid induced, exercise induced
|
|
|
atopic asthma
|
immune based, environmental allergens, IgE mediated
|
|
|
occupational asthma
|
wood, copper, platinum, plastic fumes
|
|
|
exercise induced bronchospasm
|
episodic bronchoconstriction that peaks after 10-15 minutes of exercise in some asthmatic individuals, resolves in about an hour, due to large volume of cool dry air
|
|
|
structural remodeling in asthma
|
increased exercise of bronchospasm results in hypertrophy, hyperplasia of smooth muscles; submucosal glands are increased in numbers and produce thick sticky mucus that strings; sub epithelial fibrosis is up regulation of collagen type 3/4 below basement membrane; as disease progresses patients develop significant fixed airway disease which is not responsive to beta 2 agonists
|
|
|
asthma clinical manifestations
|
recurrent chest tightness, SOB, wheezing, increased effort to breath because of increased resistance to airflow, cough (dry or producing thick, sticky mucus)
|
|
|
nocturnal worsening of asthma
|
common in untreated, best at 4pm worst at 4am
|
|
|
acute asthma cline man
|
unusual SOB, wheeze, and cough; tachypnea, tachycardia
|
|
|
asthma lab dx
|
elevated sedimentation rate, increased eosinophils, spetum eosinophilia, exhaled nitrogen oxide
|
|
|
asthma tests dx
|
pre and post bronchodilator spirometry (increase >15% after inhaling SABD); challenge test (breathing dilute amounts of methacholine or cold air or exercise on bicycle
|
|
|
structures of pulmonary system
|
upper airways, two lungs, lower airways, and blood vessels that serve them.
|
|
|
Division of lungs
|
three lobes in the right and two lobes in the left
|
|
|
Mediastinum
|
the space between the lungs which contains heart, great vessels, and esophagus
|
|
|
Bronchi
|
a set of conducting airways; delivers air into each section of the lung
|
|
|
Function of tissue surrounding airway
|
support; prevents distortion or collapse as gas moves in and out during vent
|
|
|
Conducting airways
|
passage for movement of air into and out of gas exchange portions of lungs; consist of upper and lower airways
|
|
|
Upper airway
|
nasopharynx and oropharynx; lined with ciliated mucousa with a rish blood supply
|
|
|
Upper airway mucosal lining function
|
warms and humidifies inspired air and removes foreign particles; during quit breathing gas usually flows through naso/oropharyx
|
|
|
Mouth breathing
|
happens when there is in increased demand for air; does not filter as well as oro/nasopharynx
|
|
|
Larynx structure and function
|
connects upper and lower airways; structures are endolarynx and bony cartilidge
|
|
|
Endolarynx structure and function
|
formed by two pairs of folds that form the false vocal cords and the true vocoal cords
|
|
|
Glottis
|
slit shaped space between true cords
|
|
|
Vestibule
|
space above false vocal cords
|
|
|
Laryngeal box
|
formed of three large cartilages (epiglottis, thyroid, cricord) and three small cartilages (arytenoid, corniculate, and cuneiform) that are connected by ligaments
|
|
|
Function of ligaments that support laryngeal box
|
prevents collapse during inspiration and swallowing
|
|
|
What doe the internal laryngeal muscles control
|
vocal cord lengtha and tension
|
|
|
What do the external laryngeal muscles do
|
move the larynx as a whole
|
|
|
What are the internal/external laryngeal muscles important for
|
swallowing, respiration, vocalization
|
|
|
Upper respiratory tract mucusoa mechanism of defense
|
Maintains constant temperature and humidification of gas entering the lungs; traps and removes foreign particles, some bacteria, and noxious gases from inspired air
|
|
|
Nasal hairs and turbinates mechanism of defeanse
|
trap and remove foreign particles
|
|
|
Mucous blanket mech of defense
|
protect trachea and bronchi from injury; trap foreign particles that reach lower airway
|
|
|
Cilia mech of defense
|
propel mucous blanket and entrapped particles toward the oropharynx to be swallowed or spat
|
|
|
Alveolar macrophages mech of defense
|
injest and remove foreign material from alveoli via phagocytosis
|
|
|
Irritant receptors in nares mech of defense
|
sneeze
|
|
|
Irritant receptors in trachea and large airways mech of defense
|
cough
|
|
|
Trachea connects
|
larynx to bronchi
|
|
|
Where does the trachea divdide
|
carina
|
|
|
Carina area of trachea
|
sensitive and when stimulated causes coughing and narrowing
|
|
|
Right main bronchus
|
extends from trachea more vertically than the left so its is more prone to aspiration of fluids or particles
|
|
|
Hilia
|
right and left main bronchi enter lungs here; also referred to as roots of lungs; from here bronchi branch into lobar bronchi and finally terminal bronchioles
|
|
|
Three layers of bronchial walls
|
epithelial lining, smooth muscle layer, connective tissue layer (contains cartilage)
|
|
|
Epithelial lining of bronchi
|
contains single celled exocrine glands (aka mucous secreting goblet cells) and ciliated cells
|
|
|
Ciliated epithelial lung cells function
|
rhythmically beat mucous blanket toward trachea and pharynx to be swallowed or spat
|
|
|
Gas exchange airway structures (3)
|
respiratory bronchioles, alveolar ducts, alveoli; all together called the acinus
|
|
|
Acinus function
|
gas exchange
|
|
|
Respiratory bronchioles structure
|
thin walls, cilia and goblet cells, little smooth muscle fiber, thin elastic connective tissue layer; end in alveolar ducts which lead to alveolar sacks
|
|
|
Alveoli structure and function
|
primary gas exchange unit of lung; 02 enters blood and c02 is removed from blood here; lung contains 25 millinon at birth and 300 million at adult
|
|
|
Alveolar septa structure and function
|
epithelial layer, thin elastic basement membrane, no muscle layer
|
|
|
Two types of epithelial cells in alveolus
|
type 1: provide structure; type 2 secrete surfactant
|
|
|
Surfactant
|
secreted by type 2 epithelial cells of alveoli; lipoprotein that coats inner surface of alveolus and facilitates expansion during inspiration, lowers alveolar surface tension at end expiration and thus prevents lung collapse
|
|
|
Alveolar macrophages
|
phagocytes of the lungs; ingest foreign material that reaches alveolus and move it to lymphatics
|
|
|
Mean pulmonary artery pressure
|
18mmHg; only 1/3 of vessels are full of blood at any given time therefore increase in blood to the lungs does not normally increase mean pulmonary artery pressure
|
|
|
Mean aortic pressure
|
90 mmHg
|
|
|
General pulmonary circulation functions
|
gas exchange, deliver nutrients to lung, reservoir for left ventricle, filtering system to remove clots and air from circulation
|
|
|
Pulmonary artery structure
|
divides and enters lungs at hilus with each main bronchus; branches with brochus at every division; divide at terminal bronchile to form network of pulmonary capillaries around acinus
|
|
|
Pulmonary capillaries structure
|
walls consist of endothelial layer and thin basement membrane; very little separation between blood in capillary and gas in alveolus
|
|
|
Alveolocapillary membrane
|
thing membrane made up of alveolar epithelium, alveolar basement membrane, interstitial space, capillary basement membrane, capillary endothelium; easily dadmaged and can leak plasma and blood into alveolar space
|
|
|
Where does gas exchange occur
|
alveolocapillary membrane
|
|
|
Pulmonary vein
|
drain pulmonary capillaries; dispersed randomly throughout the lung (compare this to pulmonary artery..remember?); have no valves
|
|
|
Lymphatic capillaries in lungs
|
deep and superficial; deep begin at level of terminal bronchioles; keeps lung free of fluid
|
|
|
Chest wall structure
|
skin, ribs, intercostal muscles
|
|
|
Chest wall general functions
|
protencts lungs from injuries; perform muscular work of breathing
|
|
|
Thorasic cavity structure and function
|
contained by chest wall, encases the lungs
|
|
|
Pleura structure and function
|
serous membrane adhered to the lungs; folds over itself and attaches to chest wall
|
|
|
Visceral pleura
|
membrane covering the lungs
|
|
|
Parietal pleura
|
membrane lining the thorasic cavity
|
|
|
Pleural space
|
area between visceral and parietal pleura
|
|
|
Pleural fluid
|
fluid secreted by pleura that fills the pleural space; lubricates surfaces allowing two layers to lside over each other without separating; pressure is -4 to -10 mmHg
|
|
|
3 main functions of pulmonary syste
|
ventilate alveoli; diffuse gases into and out of the blood; perfuse lungs so that organs and tissue of body receive blood
|
|
|
ventilation
|
mechanical movement of gas into and out of the lungs
|
|
|
minute volume
|
amount of effective ventilation; calculated by ventilation rate X volume of air per breath (tidal volume); expressed in liters per minute
|
|
|
normal PaC02
|
40mmHg
|
|
|
how can we accurately measure the adequacy of alveolar ventilation
|
ABG; cannot be determined by ventilatory rate, pattern, or effort
|
|
|
respiratory center in the brain
|
dorsal respiratory group, ventral respiratory group, pneumotaxic center, apneustic center
|
|
|
which piece of the brain sets the automatic rhythm of respiration
|
DRG; located in medulla; sends impulses to diaphragm and intercostal muscles
|
|
|
peripheral cehmoreceptors and respiration
|
located in carotid and aortic bodies; detect PaC02 and Pa02; send messages to DRG in medulla
|
|
|
how does the VRG area of brain affect respiration
|
not active during quiet respiration; becomes active when increased vent effort is required
|
|
|
how does the pneumotaxic center and apneustic center of brain affect breathing
|
don’t generate primary rhythm; act as modifierds of depth and rate established by medullary centers
|
|
|
three types of lung receptors that send impoulses from lungs to dorsal respiratory group
|
irritant, stretch, J
|
|
|
irritant receptors in the lungs
|
sensitive to noxious aerosols, gasses, and partiulate matter (dust); cause cough, constriction, increased vent rate; located in larger airways
|
|
|
stretch receptors in the lungs function
|
sensitive to increase in size or volume of lungs; when stimulated decrease vent rate and volume
|
|
|
j repceptors in the lungs function
|
sensitive to increased pulmonary capillary pressure; when stimulated initate rapid, shallow breathing, hypotension, bradycardia
|
|
|
parasympathetic nerve stimulation in the lungs
|
causes constriction
|
|
|
sympathetic nerve stimulation in the lung
|
causes dilation
|
|
|
chemoreceptors in the lungs
|
sensitive to changes in pH of CSF;
|
|
|
what happens to paco2/breathing when alveolar ventilation is inadequate
|
paco2 increases, co2 diffuses across BBB until pco2 in blood and CSF reaches equilibrium; and results in increased pH of CSF; increased pH stimulates respiratory center to increase depth and rate of ventilation; increased vent and rate decrease pcao2 below that of CSF and co2 diffuses back out of CSF and thus its pH returns to normal
|
|
|
how does long term hypventilation affect chemoreceptors in lungs
|
decreases their sensitivity to paco2; unable to regulate ventilation well; prolonged paco2 results in renal compensation through bicarbonate retention; bicarb diffuses into CSF to normalize the pH and negates ventilatory drive
|
|
|
mechanics of breathing involve (3)
|
major and accessory muscles of inspiration and expiration; elastic properties of the lung and chest wall: resistance to airflow through conducting airways. alterations in any of these will increase the workload of breathing
|
|
|
diaphragm
|
dome shaped; separates the abdomen and thorax; when it contracts it flattens downwards which increases the volume of the thorax six cavity and creates a negative pressure that draws gas into the lungs
|
|
|
What does contraction of the external intercostal muscles do
|
elevates the ribs; increases volume of thoracic cavity
|
|
|
What are the accessory muscles of inspiration
|
sternocleidomastoid and scalene
|
|
|
What are the accessory muscles of expiration
|
abdominal and intercostal muscles
|
|
|
Surface tension
|
tendency for liquid molecules exposed to air to adhere to one another
|
|
|
Laplace law
|
the (p) pressure required to inflate a sphere is equal to (2T) 2 times the surface tension divided by the (r) radius of the sphere; as the radius becomes smaller, more and more pressure is required to inflate it
|
|
|
Surfactant main function
|
lower surface tension
|
|
|
What cells produce surfactatnt
|
alveolar type II cells
|
|
|
How does surfactant effect laplace law
|
it reverses it; as radius gets small, the surface tension decreases and vice versa
|
|
|
What happens if not enough surfactant is available
|
surface tension increases, alveolar collapse, decreased lung expansion, increased work of breathing, severe gas exchange abnormalities, fluid accumulates in alveoli
|
|
|
Elastic recoil
|
tendency of lungs to return to resting state after inspiration
|
|
|
Compliance
|
measure of lung and chest wall distensibility; relative ease with which structures can be stretched; determined by alveolar surface tension and elastic recoil of lung/chest wall; formula tidal volume divided by pressure change (in airway or pleura)
|
|
|
Increased lung compliance
|
lung or chest wall is abnormally easy to inflate and has lost some elastic recoil
|
|
|
Decreased lung compliance
|
lung or chest wall is abnormally stiff; muscles have to work harder to breath
|
|
|
What can increase lung compliance
|
emphasyma
|
|
|
What can decrease lung compliance
|
ARDS, pneumonia, pulmonary edema, fibrosis
|
|
|
How to calculate airway resistance
|
divide change in pressure by rate of flow
|
|
|
What can increase airway resistnace
|
bronchoconstriction, bronchiole edema, airway obstruction; muscles have to work harder to breath
|
|
|
What can decrease airway resisntace
|
bronchodilation (beta 2 receptor stimulation)
|
|
|
4 steps of 02 transport in the body
|
1 ventilation of the lungs, 2 diffusion of 02 from alveoli into capillaries, 3 perfusion of systemic capillaries with 02 rich blood, 4 diffusion of 02 rich blood from systemic capillaries into cells
|
|
|
4 steps of c02 transport in body
|
diffuse of c02 from cells into systemic capillaries, 2 perfusion of pulmonary capillary bed by venous blood, 3 diffusion of c02 into alveoli, 4 removal of c02 from lungs via ventilation
|
|
|
How does a persons position change the ventilation and perfusion of the lungs
|
In a standing person, the blood via gravity falls to the lower lobs and thus perfusion is greatest here. The person lays down and the blood will no longer fall to the bottom of the lungs and thus they will not be the most perfused.
|
|
|
Zone 1 of the lungs
|
alveolar pressure exceeds pulmonary, areterial, and venous pressure. Cap beds collapse, normal blood flow ceases; small part of the lung at the apex.
|
|
|
Zone 2 of the lungs
|
alveolar pressure is >venous pressure but <than arterial pressure. Blood flows through this area but is impeded by alveolar pressure; locaed above the left atrium
|
|
|
Zone 3 of the lungs
|
arterial and venous pressure are greater than alveolar pressure; blood flow is not effected by alveolar pressure; located in base of lungs
|
|
|
What is the normal ventilation/perfusion ratio?
|
0.8; the amount by which perfusion exeeds ventilation under normal conditions
|
|
|
What do you need to calculate total arterial oxygen content
|
1, hmg concentration 2, oxygen saturation 3, Pa02
|
|
|
What is the maximum amount of oxygen blood can carry
|
1.34 mg/g
|
|
|
what happens to hemoglobin when someone has chronic pulmonary disease
|
it increases as a compensatory mechanism
|
|
|
what does a shift to the left in oxyhemoglobin dissociation curve depict
|
hemoglobins decreased affinity for 02 or ^ in ease which oxyhemoglobin dissociates and moves into cells; acidosis; hypercapnia; hyperthemia
|
|
|
what does a shift to the left in the oxyhemoglobin curve depict?
|
Hemoglobins increased affinity for oxygen which promotes Association and the lung and inhibts disassociation in tissue; alkalosis; hypocapnia; hypothermia
|
|
|
what is the bohr effect
|
the shift in the oxyhemoglobin curve related to changes in c02 levels
|
|
|
what is hypoxic pulmonary vasoconstriction
|
caused by alveolar/pulmonary venous hypoxia; can effect 1 piece or entire lung; if 1 piece effected the artioles in that segment will constrict, shunting blood to a better ventilated piece of the lung; if entire lung effected pulmonary hypertension results; if caused by low pa02 correct the pac02 and it will be ok
|
|
|
what does chronic alveolar hypoxia result in
|
chronic hypoxic pulmonary vasoconstriction; permanent pulmonary artery hypertension, cor pulmonale, heart failure
|
|
|
does acidosis or alkalosis cause pulmonary artery constristion?
|
Acidosis
|
|
|
spirometry
|
measures force of expiration; measures both volume and flow; able to detect disease in early stages
|
|
|
what are the most clinically important spirometric tests
|
FVC and FEV
|
|
|
diffusing capacity
|
measure of rate of gas diffusion across aveolarcapillary membrane
|
|
|
abg ranges
|
ph 7.35-.45; pc02 35-45; hc03 22-26; p02 80-100
|
|
|
what is the membrane surrounding alveoli contain
|
pulmonary capillaries
|
|
|
in which divsion of the lung does gas exchange occur?
|
16th
|
|
|
which part of the nervous system controls breathing most of the time
|
parasympathetic via bronchial constriction/relaxation and rate/depth of breath
|
|
|
not all 02 put into circulation is attached to hmG. what does the other 02 do?
|
exerts pressure and forces 02 to bind with hmG. this free 02 is called pa02
|
|
|
what pulmonary fucntion test can determine the cause of hypoxia
|
alveolar arterial oxygen gradient
|
|
|
how does aging effect pa02 and pac02
|
causes decrease in pa02 but doesnt effect pac02
|
|
|
s/s of pulmonary disease
|
*cough, *dyspnea, chest pain, abnormal sputum, hemotysis, altered breathing patterns, cyanosis, clubbing of digits, fever
|
|
|
true of false the distal bronchi and alveoli are rich with cough receptors
|
false. They have fewer and therefore significant material can accumulate without cough being initiated
|
|
|
which nerve transmits the cough reflex
|
vagus
|
|
|
which drug may cause patients to develop chronic cough?
|
ace inhibitors
|
|
|
Dyspnea
|
sensation of being unable to get enough air
|
|
|
What are the 3 theories of dyspnea
|
1, perceived work of breathing is greater than actual muscle effort 2, decrease in ph/hypercapnia/hypoxiemia 3, stimulation of stretch/irritant/J receptors 4, increased work of breathing r/t muscle fatigue/decreased reserve/emotions
|
|
|
Signs of dyspnea
|
flaring nostrils, accessory muscle use, retraction
|
|
|
Describe pleural pain
|
sharp or stabbing
|
|
|
Describe pleuritis
|
infection/inflammation of parietal pleura, causes pain when pleura is stretched during inspiration; pain is localized to a portion of chest; pleural friction rub heard over painful area
|
|
|
Hemoptsis
|
coughing up of blood; bright red alkaline ph and mixed with frothy sputum
|
|
|
Hematemesis
|
vomiting blood; dark red acidic ph mixed with food
|
|
|
Common causes of hemoptysis
|
bronchiecasis, lung CA, bronchitis, pneumonia, TB
|
|
|
Eupnea
|
normal breathing; 8-16 bpm; rhythmic and effortless
|
|
|
Kussmaul respiration
|
increased vent rate; large tital volume; no expiratory pause
|
|
|
Large airway obstruction
|
slow vent rate; increased effort; prolonged inspiration/expiration; stridor (high pitched during inspiration) or wheezing
|
|
|
Small airway obstruction
|
asthma/copd; rapid vent rate; small tidal volume; increased effort; prolonged expiration; wheezing
|
|
|
Restricted breathing
|
pulmonary fibrosis; small tidal volume; rapid vent rate
|
|
|
Cheyne stokes respirations
|
alternating patterns of deep and shallow breathing; apea lasting 15-60 seconds and then ventilation that increases in volume until it peaks then vent and volume decrease again until apnea; repeat
|
|
|
Hypoventilation
|
inadequate alveolar ventilation in relation to metabolic demands; caused by alterations in pulmonary mechanics/neurologic control of breathing;PaC02 increases and hypercapnia develops >44; respiratory acidosis
|
|
|
s/s of hypoventilation
|
somnolence, disorientation, acidosis, 2ndary hypercapnia, hypoxemia
|
|
|
hyperventilation
|
alveolar ventilation that exceeds metabolic demands; removes c02 faster than its produced; results in hypocapnia <36; respiratory alkalosis; anxiety, acute head injury, condiation that causes insufficnet 02 to be in blood
|
|
|
cyanosis
|
blue skin; caused by increased amounts of desaturated HmG or low HmG; occurs when 5g/dl of blood is desaturated no matter how much total HmG there is
|
|
|
peripheral cyansis
|
poor circulation; raynaud disease; cold places; severe stress
|
|
|
central cyanosis
|
low Pa02; pulmonary disease; pulmonary cardiac right to left shunts; indicator of sever problem in adults
|
|
|
which two conditions can cause inadequate 02 to be delivered to tissue without causing cyanosis?
|
severe anemia and carbon monoxide poisening
|
|
|
which disesase can cause cyanosis even though oxygen is being delivered to the tissue adequately?
|
polycythemia
|
|
|
clubbing
|
elargment of distal segment of a digit; severity graded 1-5 based on extent of nail bed hypertrophy; associated with bronchiectasis, CF, pulmonary fibrosis, lung abscess, congenital heart disease; reversible; lung ca
|
|
|
hypercapnia causes
|
depression of resp center r/t drugs; disease of medulla (trauma); spinal cord probs; myasthasia gravis; muscular dystrophy; thoracic cage abnormality; throat lung tumor; sleep apnea; emphysema
|
|
|
what can acidosis cause the heart to experience
|
dysrhythmias
|
|
|
hypoxemia causes
|
02 not being delivered to alveoli; inability to diffuse 02 from alveoli to blood; poor perfusion of pulmonary capillaries; low Fi02
|
|
|
Fi02
|
amount of 02 inspired; at sea level 0.21
|
|
|
Causes of decreased Fi02
|
high altitude
|
|
|
ARF clinical parameters
|
Pa03 < 50 or PaC02 >50 with a ph < 7.25
|
|
|
ARF causes
|
lung/airway/chest/brain injury and pulmonary diseases
|
|
|
ARF that is hypercapnic cause and tx
|
inadequate alveolar ventilation; need vent support
|
|
|
ARF that is hypoxemic causes and tx
|
inadequate exchange of 02 in alveoli and capillaries; give 02
|
|
|
Risk factors for ARF
|
sugery, smokers, lung disease, CRF, chronic hepatic disease, infection
|
|
|
Most common post operative pulmonary problems
|
atelectasis, pneumonia, pulmonary edema, pulmonary emboli
|
|
|
How to prevent ARF
|
turning, deep breathing, early ambulation, humidified inspired air, IS
|
|
|
How to diagnos chest wall restriction
|
reduced FVC
|
|
|
Flail chest clin man
|
results from fracture to ribs; during inspiration unstable chest moves inward and expiration moves out; dsypnea, chest pain, unequal chest expansion, hypoventilation, hypoxemia
|
|
|
Flail chest treatment
|
internal fixation by mech vent
|
|
|
Pneumothorax
|
air or gas in pleural space; caused by rupture in visceral/parietal pleura;
|
|
|
Primary/spontaneous pneumothorax
|
bleb rupture on pleura; unexpectedly; men 20-40; these people have emphysema like changes in lungs; + family history; folliculin gene
|
|
|
Tension pneumothorax
|
pleura rupture; site is one way valve permits air to enter but not to leave; air enters pleura and pneumothorax and pressure begins to = lung pressure; life threatening; pressurized pleura pushes against lung and cause atelectasis and displaces the heart
|
|
|
Clinical manifestations of primary pneumothorax
|
sudden pleural pain, tachypnea, mild dyspnea; absent breath sounds and hyperresonance
|
|
|
Clinical manifestations of tension pneumothorax
|
sudden pleural pain, tachypnea, mild dyspnea; absent breath sounds and hyperresonance; hypoxemia; tracheal deviation away from affected lung; hypotension
|
|
|
Dx primary pneumothorax
|
CXR; CT
|
|
|
Dx tension pneumothorax
|
physical examination alone; requires immediate chest tube
|
|
|
Pleural effusion
|
fluid in pleural space;
|
|
|
Transudative effusion
|
pleural effusion in which fluid is watery; fluid diffused out of capillaries r/t increased intravascular hydrostatic pressure or decreased capillary oncotic pressure; CHF, liver and kidney disorders that cause hypoproteniemia; htn
|
|
|
Exudative effusion
|
pleural effusion that contains WBC and plasma proteins; response to inflammation, infection, malignancy
|
|
|
Empyema
|
pus in pleural space; pulmonary infections; lung abscess
|
|
|
Hemothorax
|
blood in pleural space; trauma; surgery; rupture; malignancy
|
|
|
Chylothorax
|
chyle in pleural space; trauma; infection; lymphatic disorder
|
|
|
T/F both pleura effusions and pneumothorax cause atelectasis
|
false; only pneumothorax. Since pleura effusions do not introduce air into the pleura space, the lung is still able to remain open via pressure gradient.
|
|
|
Pleural effusion clin man
|
dyspnea; pleuritic chest pain; decreased breath sounds; dullness on percussion;
|
|
|
Aspiration RISK FACTORS
|
altered LOC, seizures, CVA, neuromuscular problems
|
|
|
Aspirate food with ph <2.5 consequences
|
bronchoscopy removal, develops into collapse of airway distally, recurrent bronchiectasis (permanent dilation of bronchus), surgical resection then required
|
|
|
Aspirate oral secretions
|
can cause aspiration pneumonia bc of bacterial content
|
|
|
s/s of aspiration
|
sudden onset of choking, irretractible cough, w/ or w/out vomit, fever, dyspnea, wheeze.
|
|
|
Subtle s/s of aspiration
|
recurrent lung infections, chronic cough, persistant wheeze ver months/years
|
|
|
Atelectasis
|
collapse of lung tissue
|
|
|
3 types of atelectasis
|
compression absorption, surfactant impairment
|
|
|
compression atelectasis
|
caused by external pressure on lung tissue; tumor, fluid, air, abdominal distention
|
|
|
absorption atelectasis
|
absorption of air from obstructed or hypventilated alveoli
|
|
|
Surfactant impairment atelectasisi
|
decreased production/inactivation of surfactant; prematurity, ARDS, anesthesia, mech vent
|
|
|
Clinical manifestations of atelectasis
|
dyspnea, cough, fever, leukocytosis
|
|
|
Bronchiectasis
|
persistant abnormal dilation of bronchi; causes are obstruction of airway w/ mucous plug, atelectasis, aspiration, CF, TB, congenital weakness of bronchi, impaired defense mechanisms
|
|
|
What kind of bronchiectasis is reversible?
|
cylindrical; from pneumonia
|
|
|
Bronchiectasis symptoms
|
productive cough; foul smelling sputum; hemoptysis; clubbing; decreased FVC
|
|
|
Bronchiectasis dx
|
CT
|
|
|
Bronchiectasis tx
|
atb, bronchodilators, chest physiology, supplemental 02
|
|
|
Bronchiolitis
|
inflammation of small airways (bronchioles); kids mainly; in adults its bronchitis
|
|
|
Bronchiolitis clin man
|
tachpnea, accessory muscles, low grade fever, dry non productive cough, hyperinflated chest
|
|
|
Bronchiolitis tx
|
atb, steroids, chest physiotherapy, humidified air, coughing, deep breathing, postural drainage
|
|
|
Bronchiolitis obliterans
|
fribrotic process that occludes the airways and permanently scars the lungs; most common after lung transplant
|
|
|
Dx bronchiolitis obliterans
|
spirometry and bronchoscopy w/ biopsy
|
|
|
Pulmonary fibrosis
|
excessive amounts of connective tissue in the lungs
|
|
|
Causes of pulmonary fibrosis
|
idiopathic, ARDS, TB, inhalation of harmful substance, autoimmune, rheumatologic disease
|
|
|
Idiopathic pulmonary fibrosis
|
men; 2-4 years survival; chronic inflammation and firbroproliferation around alveoli; decreased 02 diffusion and hypoxemia; dyspnea on exertion; tx with corticosteroids
|
|
|
Oxygen toxicity
|
prolonged exposure to high concentrations of supplemental oxygen; inflammatory response; damage to alveolocapillary membranes, disruption of surfactant, interstitial edema, alveolar edema, decreased compliance
|
|
|
Pneumoconiosis
|
any change in lung caused by inhaled dust particles
|
|
|
Silicosis
|
type of pneumoconiosis; inhaled dilica
|
|
|
Coal worker pneumoconiosis
|
coal dust deposits in lung; chronic bronchitis; pulmonary fibrosis; productive cough and wheezing
|
|
|
Asbestos exposure
|
pulmonary fibrosis; lung ca; mesothelioma (cancer of pleura)
|
|
|
Pulmonary edema causes
|
excess water in lung; caused by heart disease, left ventricular failure, anemia, decreasd plasma proteins, capillary injury, ards, obstruction of lymphatic system
|
|
|
Pulmonary edema s/s
|
dyspnea, orthopnea, hypoxemia, increased work of breathing
|
|
|
Pulmonary edema physical exam
|
inspiratory crackles, dullness over bases, evidence of ventricular dilation, pink frothy sputum, hypercapnia
|
|
|
ARDS
|
respiratory failure characterized by acute lung inflammation and diffuse alveolocapillary injury
|
|
|
ARDS pathophysiology
|
damage to the lungs, nutrophils, platelets and inflammatory substances called to the scene, capillary permeability increases, proteins fluid and blood leak into pulmonary interstitium and alveolar space, pulmonary htn occurs, alveolar ventilation is decreased. Surfactant is decreased, fibrosis occurs
|
|
|
ARDS clin man
|
progressive dyspnea
|
|
|
ARDS exam
|
dyspnea and hypoxemia→hyperventilation and respiratory alkalosis→decreased tissue perfusion, organ dysfunction, metabolic acidosis→decreased tidal volume and hypoventilation→respiratory acidosis and furher hypoxemia→decreased CO and hypotension→death
|
|
|
ARDS dx
|
refractory hypoxemia, cxr w/ bilat infiltrates, exclusion of cardio/pulm edema
|
|
|
ARDS tx
|
vent with peep and high 02 concentrations; supportive therapy; prevention of complications (pneumonia)
|
|
|
Obstructive pulmonary disease
|
airway obstruction that is worse with expiration; increased work of breathing; ventilation perfusion mismatch; decreased FEV1
|
|
|
Most common obstructive pulmonary diseases
|
asthma, chronic bronchitis, emphysema; collectively called COPD
|
|
|
Asthma
|
complex interation of airway obstruction, bronchiole hyperresponsiveness, inflammation
|
|
|
How does inflammation effect asthma
|
it is a intergral part of the dz; it causes recurrent episodes of coughing, wheezing, breathlessness, and chest tightness
|
|
|
When is coughing the worst for asthmatics
|
morning and night
|
|
|
Asthma patho
|
irritant enters lungs> immune response initiated> airway becomes obstructed> expiratory flow expecially obstructed> air becomes trapped and lungs hyperinflat> hyperventilation> hypoxemia without C02 retention> PaCO2 decreases and respiratory alkalosis developes>obstruction becomes more severe> lungs and thorax become hyperextended due to hyperinflation> C02 retention/respiratory acidosis> respiratory failure
|
|
|
Asthma clin man
|
chest tightness, expiratory wheeze, dyspnea, non productive cough, prolonged expiration, tachycardia, tachypnea
|
|
|
Pulsus paradoxus
|
decrease in systolic BP by 10pts during inspiration during asthma attack
|
|
|
Asthma attack eval
|
abg,expiratory flow rate, identify underlying trigger
|
|
|
Is alkalosis or acidosis expected early in an asthma attack?
|
alkalosis
|
|
|
Management of acute asthma attack
|
02, beta 2 agonists, oral corticosteroids; atb not indicated unless infection confirmed
|
|
|
Pulmonary function tests and asthmatics
|
decreased FEV1, FVC; increased FRC and TLC
|
|
|
Chronic bronchitis
|
hypersecretion of mucus and chronic productive cough for at leaste 3 months of the year and for 2 consequetive years
|
|
|
Chronic bronchitis patho
|
irritant> mucus production> ^ size/number of mucus glands. Mucus is thicker than normal and more likely to get backteria stuck in it. Ciliary function is impaired. Lungs defenses are down. Persistant inflammation/recurrent infection lead to bronchospasm and permanent narrowing of airways
|
|
|
Chronic bronchitis clin man
|
exercise intoleratnce, wheezing, SOB, productive cough, decreased FEV1, hypoxemia with exercise; later copious amounts of sputum, frequent pulmonary infections, FVC/FEV way low, FRC/RV increased
|
|
|
Chronic bronchitis dx
|
history of symptoms, physical exam, cxr, pulmonary function tests, blood gas analysis
|
|
|
Chronic bronchitis tx
|
prevention. Pathologic changes are irreversible; bronchodilators; expectorants; control cough and reduce dyspnea; deep breathing and postural drainage; nutritional counseling, resp hygiene, recognize early s/s of infection, techniques to relieve dyspnea; atb for all exacerbations; avoid chronic use of corticosteroids
|
|
|
Emphysema
|
permanent enlargement of gas exchanging airways (acini) with destruction of alveolar walls without fibrosis
|
|
|
Antitrypsin
|
gene indicated in primary emphysema. People who don’t have enough develop emphysema
|
|
|
Emphysema patho
|
most cases initiated by smoke, destruction of alveoli, breakdown of elastin, expiration becomes difficult, hyperinflation of alveoli, increased work of breathing
|
|
|
Emphysema clin man
|
dyspnea on exertion, develops into marked dyspnea even at rest; little coughing; little sputum; person is thin, tachypnic, prolonged expiration, uses accessory muscles to breath barrel chest, hyperresonant sound, leans forward with hands on knees, exhales through pursed lips
|
|
|
Emphysema dx
|
pulmonary function measures, cxr diaphragm flattened and lungs are too large, abg reveal hypoxia and or hypercapnia
|
|
|
Emphysema acute management
|
cxr, serum WBC, abg, sputum sample; give 02, may require positive airway pressure device or vent, bronchodilators, oral corticosteroids and atb immediately,
|
|
|
Emphysema chronic management
|
smoking cessation; ihaled antiocholinergics and beta agonists; avoid long term steroid; maybe long term 02
|
|
|
Pneumonia
|
infection of the lower respiratory tract of bacteria, virus, fungi, protozaoe, parasites
|
|
|
Pneumonia risk factors
|
age, immunocompromise, underlying lung disease (COPD), alcoholism, altered LOC, impaired swallowing, smoking, ET intubation, malnutrition, immobilization, cardiac/liver disease, nursing home residence.
|
|
|
What is the most common community aquired pneomnia caused from
|
S. Pneumoniae (pneumococcus)
|
|
|
What is a common bacteria that causes pneumonia in group home living (2)
|
m. pneumoniae and c. pneumoniae
|
|
|
Which bacteria that causes pneumonia hides in cooling systems
|
legionella
|
|
|
What are commong nosocomial bacteria that cuase pneumonia
|
p. aeruginosa, gram negatives, s. aureus
|
|
|
Which pneumonia bacteria are immunocompromised people suciptible to
|
p. jiroveci, fungus, virus, mycobacterial
|
|
|
Pneumonia patho
|
aspirate secretions, naso/oropharynx 1st line of defense, travels down to lung, epithelium next line of defense, alveolar macrophages recognize foreign and kick off the immunity, damage occurs and acini and bronchiles fill with exudate
|
|
|
Pneumonia clin man
|
preceded by upper airway infection usually viral, followed by onset of cough, dyspnea, fever. Cough is productive, chills, malaise, pleuritic chest pain
|
|
|
Pneumonia exam
|
signs of pulmonary consolidation, inspiratory crackles, tactile fremetis, egophony, whispered pectoriloquy,
|
|
|
Penumonia dx
|
exam, WBC (high), cxr (infiltrates), stains and cultures of blood, culture of resp secretions, blood cutlures
|
|
|
TB patho
|
transmitted via airborn droplet, organisms lodge in upper lobe, inflammation occurs, macrophages start to eat bacteria, tubercle forms, tuburcle dies and forms cheese like material
|
|
|
TB clin man
|
latent asymptomatic; fatigue, weight loss, lethargy, anorexia, low grade fever in afternoon, cough with purulent sputum, night sweats, general anxiety, dyspnea, chest pain, hemoptysis
|
|
|
TB dx
|
+ skin test, sputum culture, immunoassays, cxr
|
|
|
TB tx
|
antibiotics, isolation until culture is negative. Usually weeks to 2 months.
|
|
|
Acute bronchitis
|
acute inflammation of airways or bronchi; mostly caused by viruses
|
|
|
Viral bronchitis s/s
|
nonproductive cough aggrevated by cold, dry, or dusty air.
|
|
|
Viral bronchitis tx
|
rest, asa, humidity, cough suppressant
|
|
|
Bacterial bronchitis s/s
|
productive cough, fever, pain behind sternum aggrevated by coughing
|
|
|
Bacterial bronchitis tx
|
rest, asa, humidity, atb
|
|
|
PAH clin man
|
enlarged pulmonary art seen on cxr; fatigue, chest discomfort, tachypnea, dyspnea on exertion, palpitations, cough, perpheral edema, JVD, precordial heave, 2nd heart sound
|
|
|
PAH dx
|
right sided heart cathetrization; lab ABG, liver, hiv, ecg, cxr, ct scan, pulmonary function test, polysomnography, ventilation perfusion scanning, echo
|
|
|
PAH tx
|
02, diuretics, anticoagulants, avoid triggers, nitric oxide agonists, prostacyclin analogs, endothelin blockers, tx primary disorder
|
|
|
Cor pulmonale
|
2ndary to pulm art htn, consists of right ventricle enlargment
|
|
|
Cor pulm patho
|
develops in response to chronic pressure overload in right ventricle, hypertrophy occurs, right ventricle fails when pulm art pressure = systemic pressure
|
|
|
Cor pulm clin man
|
distress occurs only during exercise, heart appears normal at rest, with exercise CO falls; ecg shows right ven hypertrophy; chest pain; murmurs; peripheral edema, hepatic congestion, JVD
|
|
|
Cor pulm dx
|
physical exam, radiology findings, ecg/echo
|
|
|
Cor pulm tx
|
lower pulm art presure
|
|
|
Summery of digestion/absorption
|
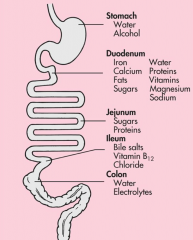
The process of intestinal digestion is initiated in the stomach by the actions of hydrochloric acid and pepsin, which break down food fibers and proteins. The chyme that passes into the duodenum is a liquid that contains small particles of undigested food. Digestion is continued in the proximal portion of the small intestine by the action of pancreatic enzymes, intestinal brush border enzymes, and bile salts (Box 38-1). Here carbohydrates are broken down to monosaccharides and disaccharides; proteins are degraded further to amino acids and peptides; and fats are emulsified and reduced to fatty acids and monoglycerides (Figure 38-11). These nutrients, along with water, vitamins, and electrolytes, are absorbed across the intestinal mucosa and into the blood by active transport, diffusion, or facilitated diffusion. Products of carbohydrate and protein breakdown move into villus capillaries and then to the liver through the portal vein. Digested fats move into the lacteals and eventually reach the liver through the systemic circulation. Intestinal motility exposes nutrients to a large mucosal surface area by mixing chyme and moving it through the lumen. Different segments of the gastrointestinal tract absorb different nutrients. Digestion and absorption of all major nutrients occur in the small
|
|
|
Three pairs of salivary gland
|
submandibular, sublingual, parotid glands
|
|
|
What makes up salaiva
|
mucus, bicarb, chloride, K+, amylase, IgA
|
|
|
Which nerve fibers stimulate salivary glands
|
parasympathetic cholinergic, beta adrenergic stimulation
|
|
|
What common drug inhibits salivation
|
atropine
|
|
|
When is peristalsis stimulated
|
affarent fibers along the esophagus sense change in wall tension caused by stretching as food passes
|
|
|
Which sphincter prevents entry of air into esophagus during respiration
|
upper esophageal sphincter aka cricopharyngeal
|
|
|
Which sphincter prevents regurgitation from the stomach
|
lower esophageal aka cardiac sphincter
|
|
|
Where is the swallowing center in the brain
|
reticular formation
|
|
|
Two phases of swalloing
|
1, oropharyngeal, voluntary and 2, esophageal, involuntary
|
|
|
What is primary peristalsis
|
peristalsis immediately following oropharyngeal phase of swallowing
|
|
|
What is 2ndary peristalsis
|
when a bolus of food gets stuck in esophageal; involuntary
|
|
|
What increases lower esophageal sphincter tone?
|
cholinergic vagal input and digestive hormone gastrin
|
|
|
What relaxes lower esophageal sphincter tone
|
nonadrenergic, noncholinergic, vagal impulses, progesterone, secretin, glucagon
|
|
|
Chyme
|
partially digested food
|
|
|
Which sphincter does food pass from the esophagus into the stomach?
|
cardiac
|
|
|
Which sphincter does food pass from the stomach into the duodenum
|
pylorus
|
|
|
What are thefunctional areas of the stomach
|
fundus (upper), body (middle), antrum (lower)
|
|
|
Which artery supplies blood to the stomach
|
celiac; blood supply is so abundant that nearly all vessels have to be occluded for there to be ischemia
|
|
|
Which nerve fibers innervate the stomach
|
sympatehitc and parasympathetic; there are extrinsic and intrinsic nerves
|
|
|
Which nerves that innervates the stomach are extrinsic
|
celiac plexus (sympathetic) and vagus (parasympathetic)
|
|
|
Which nerves that innervate the stomach are intrinsic
|
myenteric plexus
|
|
|
T/F the stomach can absorb water
|
false
|
|
|
Which 2 drugs can the stomach absorb
|
alcohol and asa
|
|
|
What increases the contraction of stomach peristalsis
|
gastrin, motilin, vagus nerve stimulation
|
|
|
What decreases the contraction of stomach peristalsis
|
secretin
|
|
|
What does the rate of gastric emptying depends on
|
volume, osmotic pressure, chemical content of gastric contents; larger volumes increase gastric pressure, peristalsis, and rate of emptying
|
|
|
Cholecytokinin secretion is stimulated by
|
products of fat digestion; bile from the liver and enzymes from the pancrease
|
|
|
Cholecytokinin action
|
inhibits gastric motility so that fat is not dumped into duodenum faster than bile/panc enzymes can be made
|
|
|
How does BGL effect peristalsis
|
low levels stimulate vagus nurse and gastric smooth muscles. There is an increase in peristalsis but not gastric emptying thus you get the sensation of hunger pains
|
|
|
Explain how osmoreceptors in the duodenum effect gastric emptying
|
tonicity of contents entering duodenum stimulate receptors this delays gastric emptying and facilitates an isoosmotic duodenal environment
|
|
|
What is the “intrinsic factor” necessary for?
|
vit b12 absorption
|
|
|
What is gastroferrin facilitate in the GI
|
iron absorption
|
|
|
What do parietal cells secrete
|
hydrochloric acid and intrinsic factor
|
|
|
What do the chief cells secrte
|
pepsinogen; converted to pepsin
|
|
|
If you are vomiting/have a NG suction, what ion are you loosing?
|
K+
|
|
|
What are the main functions of acid in the GI
|
dissolve food, bacteriocidal, convert pepinogen to pepsin
|
|
|
What substances stimulate acid secretion in the GI
|
acetylecholine, gastrin, histamine
|
|
|
Where does acetylcholine come from in the GI
|
vagus nerve
|
|
|
What inhibits acid secretion in GI
|
prostaglandins, gastric inhibitory peptide, somatostatin, secretin
|
|
|
What does pepsin do in the GI
|
breaks down protein in stomach; inactive in duodenum
|
|
|
What can cause a break in the stomachs mucosal lining
|
asa, NSAIDs, H pylori, ethanol, regurgitated bile, ischemia; breaks cause inflammation and ulceration
|
|
|
What are the phases of gastric secretion
|
cephalic, gastric, intestinal
|
|
|
Cephalic stage of gastric secretion
|
anticipatory part of eathing; acetylcholine, acid, pepsinogen
|
|
|
Gastric phase of gastric secretions
|
begins with arrival of food in stomach; distention stimulates nerve reaction;
|
|
|
TF calcium stimulates acid secretion
|
true; so does caffeine
|
|
|
Intestinal phase of gastric secretion
|
secretory process slows down; acid in the chyme in the duodenum inhibit gastric secretions and stimulate pepsinogen secretion to buffer the acid
|
|
|
What are the 3 sections of the small intestine
|
duodenum, jejunum, ilieum
|
|
|
What does the ileocecal valve control
|
passage of digested food from the ileium into the large intestine; prevents reflux
|
|
|
Essential role of duodenum
|
mix food with digestive juices from liver and pancreas
|
|
|
What are plica
|
mucosal folds in the small intestine that slow the passage of food and allow for more absorption
|
|
|
Villi
|
functional units of intestine; where absorption happens; secretes digestive enzymes;
|
|
|
Function of tight junctions at the villus
|
absorb water and electrolytes
|
|
|
Brush boarder
|
made of microvili
|
|
|
Crypts of lieberkuhn
|
between bases of vili; contain stem cells; produce alkaline fluid, mucus and electrolytes; turn into columnar cells
|
|
|
What suppresses vili proliferation
|
starvation, b12 deficiency, cytotoxic drugs, radiation; diarrhea and malnutrition
|
|
|
Salivary glands enzymes
|
amylase and lipase
|
|
|
Stomach enzymes
|
pepsin, gastric lipase
|
|
|
Pancrease enzymes
|
amylase, trypsin, chymotrypsin, carboxypeptidase, elastase, lipase-colipase, phospholipase, cholesterol estrase
|
|
|
Small intestine ezymes
|
enterokinase, disacharidases (maltase, sucrase, lactase), isomaltase, peptidases
|
|
|
How much water is absopbed in the small intestine
|
90%
|
|
|
How much water is absorbed in the colon
|
10%
|
|
|
TF insulin in required for CHO to absorb in intestine
|
false
|
|
|
4 phases of fat absorption
|
emulsification and lipolysis, micelle formation, fat absorption, resythesis of triglycerides/phospholipids
|
|
|
emulsification
|
agents in intestine cover small fat particles and prevent them from reforming into fat droplets
|
|
|
what are the emulsifying agents
|
fatty acids, monoglycerides, lechtin, cholesterol, protein, biles salts
|
|
|
lipolysis
|
hydrolysis of emulsified fats by pancreatic lipase, phospholipase, hydrolase
|
|
|
micelles
|
formed from bile salts, products of fat hydrolysis, and fat soluble vit, cholesterol
|
|
|
patho UC
|
no skip leasions in thin mucosa, rectal involvement, inflammation begins in large intestine
|
|
|
UC clin man
|
remission exacerbation; large volume watery diarrhea; bleeding, cramping, urge to poop; frequent diarrhea, small amounts of blood and purulent mucus
|
|
|
UC dx
|
low hmg, hypoalbuminemia, low K; r/u infection w/ culture
|
|
|
UC tx
|
mesalazine, steroids, salicyclates, immunosuppresives, broad atb, probiotics, colostomy
|
|
|
Chrones overall
|
inflammatory disorder affecting any part of GI tract from mouth to anus typically distal small/proximal large
|
|
|
Crohns risk factors
|
fam hx, tobacco, jews, urban ppl, CARD15 gene mutation
|
|
|
Crohns patho
|
inflam begins in submucosa, neutrophil infiltrate, abscess formation, common site ileocolon, skip leasions present,
|
|
|
Crohns clin man
|
non specific for years, abd pain, diarrhea, depends on where inflam is (ilieum = anemia, low folic, vit d, and ca, leading to bone disease, pain in right lower abdomen)
|
|
|
Crohns dx
|
history, endoscopy, r/u infection
|
|
|
Short bowel syndrome
|
happens after surgical resection of bowel r/t crohns, malabsorption, diarrhea, nutritional deficiencies
|
|
|
Diverticula
|
herniations of mucosa
|
|
|
Diverticulosis
|
asymptomatic diverticular dieases
|
|
|
Diverticulitis
|
inflammation of diverticula
|
|
|
Diverticulta patho
|
common site left colon, thick musclues around diverticula; may cause abscess, fistula, peritonitis, obstruction
|
|
|
Diverticula clin man
|
cramping lower abd, diarrhea, constipation, distention, flatulence
|
|
|
Diverticula dx
|
ultrasound, sigmoidoscopy, barium, CT
|
|
|
Diverticula tx
|
fiber, probiotics, salicylates, atb, sx
|
|
|
Appendicitis
|
inflam of the projection located at apex of cecum
|
|
|
Appendicitis patho
|
obstruction with stool, tumor, foreign bodies
|
|
|
Appendicitis clin man
|
epigastric or periumbilical pain; vague at first, increases with intensitiy over ¾ hours, rebound tenderness, RLQ pain, N/V anorexia, diarrhea, fever,
|
|
|
Appendicitis dx
|
wbc 10-16k, ^neutrophils, ^ c reactive protein, ct scan, ultrasound
|
|
|
IBS
|
functional GI disorder characterized by abd pain and altered bowel habits
|
|
|
IBS symptoms
|
diarrhea, constipation, pain
|
|
|
Causes of IBS
|
food allergy, overgrowth of intestinal flora, post infectious IBS, visceral hypersensitivity, abnormal GI motility/secretion, psychosocial factors
|
|
|
IBS clin man
|
lower abd pain, diarrhea/constipation predominant or alternating, gas, bloating, nausea, fecal urgency, incomplete evacuation
|
|
|
IBS dx
|
rome 3 criteria, 2 ore more of the following need to occurs for at least 3 months; abd pain or discomfort that 1, improves with defecation 2, onset associated with change in frequency 3, onset associated with change in form of stool
|
|
|
IBS tx
|
no cure, laxatives, fiber, antidiarrheas, antisposmotics, antidepressants, analgesics, serotonin agonists/antagonists
|
|
|
Acute occlusion of mesenteric artery
|
reduced mucosal blood flow to intestine; AAA, thrombi, emboli causes;
|
|
|
Chronic mesenteric insufficiency
|
non occlusive; atheroscleorsis, CHG, acute MI, dysrhythmias, hemorrhage, stenosis, thrombus, AAA, any condition that decreases arterial blood flow; cardinal symptom is colicky abd pain after eating
|
|
|
Abdominal angina
|
cramping pain due to mesenteric low flow after meals
|
|
|
Portal htn
|
a abnormally high blood pressure and portal venous system caused by her assistance to portal flow
|
|
|
Portal htn patho
|
caused by disorders that obstruct or MP bloodflow through any portion of the portal venous system or vena cava
|
|
|
Long term portal htn causes
|
varices, splenomegaly, ascites, hepatic encephalopathy,
|
|
|
Clin man portal htn
|
vomiting blood, bleeding from varicies
|
|
|
Portal htn dx
|
made at time of varices bleeding and edoscopy
|
|
|
Portal htn tx
|
beta blockers, emergency care for bleeding varices
|
|
|
Splenomegaly
|
enlarged spleen
|
|
|
Splenomegaly clin man
|
thrombocytopenia
|
|
|
Ascites
|
accumulation of fluid in peritoneal cavity
|
|
|
Ascites contributing factors
|
portal htn, hepatocyte failure, sodium rentention
|
|
|
Asciteds clin man
|
weight gain, abd distention, increased abd girth, tachypnea, semi fowler position to relieve,
|
|
|
Ascites dx
|
based on clin man and identification of liver disease, SAAG lab, paracentesis
|
|
|
Asciteds tx
|
goal is to relieve discomfort, restore liver function, restrict salt and use K sparring diruetics
|
|
|
Hepatic encephalopathy
|
impaired cognition, flapping, eeg changes due to hepitits
|
|
|
RF hepatic encephalopathy
|
advanced liver dz, ^ protein intake, electrolyte imbalance, hypoxia
|
|
|
Hepatic encepholapathy dx
|
hx of liver disease, clin man, eeg and blood chem., ammonia levels; no specific dx test
|
|
|
Heptatic encepholapthy tx
|
correct FE, withdrawl depressant drugs metabolized by liver, reduce ammonia levels by restricting protein and eliminate intestinal bacteria with neomycin; lactulose prevents ammonia absorption
|
|
|
Jaundice
|
caused by hyperbilirubinemia greater than 3mg/dl
|
|
|
Jaundice causes
|
gallstones, liver cirrosis, hepatitis, excessive bilirubin, hemolysis
|
|
|
Clin man jauncie
|
conjugated hyperbili makes urine dark, fever, jills, yellow skin
|
|
|
Unconjugated hyperbilirubinemia cause
|
hemolysis
|
|
|
Congjugated hyperbilirubinemia cause
|
plug in the bile duct, liver issue
|
|
|
Hep a
|
fecal oral and infected blood, incubation 6 weeks, shed up to 3 months after and is most contagious, antibodies 4 weeks after infection, immunization available; dx anti HAV
|
|
|
Hep b
|
blood, body fluids, contaminated needles, sti, materal fetal during 3rd trimester; 8 week incubation; ^ IgM levels; vaccination available; dx HBsAg
|
|
|
Hep c
|
shared needles; no vaccine
|
|
|
Hep d
|
occurs with ppl with hep b; shared needles; antiviral drug tx; dx anti-HDV
|
|
|
Hep e
|
oral fecal, contaminated water, animal resevoirs; no dx test
|
|
|
Gep g
|
sti, shared needles
|
|
|
Hepatitis clin man
|
abnormal liver function, ALT/AST
|
|
|
Prodromal phase of hepatitis
|
2 weeks after infection, jaundince, fatigue, anorexia, malaise, nv, headache, hyperalgia, cough, low grade fever
|
|
|
Icteric phase of hepatitise
|
2 weeks after prodromal phase; dark urine, clay colored stools, enlarged smooth tender liver, itching
|
|
|
Recovery phase
|
8 weeks after exposure
|
|
|
Cirrhosis
|
irreversible inflam that disrupts liver stucture and function
|
|
|
Cirrhosis clin man
|
enlarged liver, history of continuous alchol intake previous months or weeks, anorexia, nausea, jaundice, edema
|

