![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
177 Cards in this Set
- Front
- Back
|
adenosine & dosage
|
Med used for Conversion of paroxysmal supraventricular tachycardia (PSVT) to normal sinus rhythm when vagal maneuvers are unsuccessful.
Dosage: 6mg rapid IV push, 12 mg, 12 mg |
|
|
What does ST-depression usually signify?
|
Ischemia
|
|
|
What does ST-elevation usually signify?
|
nercrosis of cardiac muscle
|
|
|
Leads II, III, and AVF tell us which area of the heart is having an infarct?
|
inferior wall --> BAD
|
|
|
On monitor paper, how many seconds are a "little" box and a "big" box?
|
Little box = 0.04 seconds
Big box = 0.2 seconds |
|
|
What is the P wave?
|
* Indicates atrial depolarization, or contraction of the atrium.
* Normal duration is not longer than 0.11 seconds (less than 3 small squares) * Amplitude (height) is no more than 3 mm * No notching or peaking |
|
|
What is the QRS complex?
|
Indicates ventricular depolarization, or contraction of the ventricles.
Should less than 0.12 seconds. |
|
|
What could a QRS of > 0.12 mean?
|
Delay in ventricular contraction.
Usually a heart block in bundle branches. |
|
|
What is the T wave?
|
Indicates ventricular repolarization
Not more that 5 mm in amplitude in standard leads and 10 mm in precordial leads Rounded and asymmetrical |
|
|
What is the ST segment?
|
Indicates early ventricular repolarization
Normally not depressed more than 0.5 mm May be elevated slightly in some leads (no more than 1 mm) |
|
|
What is the PR interval?
|
Indicates AV conduction time
Duration time is 0.12 to 0.20 seconds Less than 0.20 seconds. |
|
|
What is the QT interval?
|
Measured from the Q to the end of the T.
Represents ventricular depolarization and repolarization (sodium influx and potassium efflux) V3, V4 or lead II optimize the T-wave. Less than 0.44 seconds |
|
|
What can cause elongated QT?
|
genetics, medications, electrolyte imbalance, MI, defective sodium or potassium channels.
|
|
|
What happens when a cell depolarizes?
|
Sodium rushes into cell, potassium rushes out causing an action potential.
|
|
|
Why is an inferior wall MI so bad?
|
This type of MI is not good. The patient will usually be vomiting and could die.
|
|
|
1mg/min of a solution of lidocaine (2g/500mL or 4 mg/mL) comes to what rate per hour?
How about for 2mg/min, 3mg/min, 4mg/min |
1 mg/min = 15 mL/hr
2 mg/min = 30 mL/hr 3 mg/min = 45 mL/hr 4 mg/min = 60 mL/hr |
|
|
What are PVCs?
When do they occur? Is the QRS wider or narrow or normal? |
Premature Ventricular Contractions.
Most common form of arrhythmia. Found in healthy and not healthy inviduals. QRS is wider because ventricle did not completely repolarize. |
|
|
When is treatment required for PVCs?
|
When they are:
associated with an acute MI, fall on or after the T wave, occur as couplets, are multifocal, or are frequent (>6/min). |
|
|
Describe these terms relating to PVCs: couplets, triplets, bigeminy, trigeminy, quadgeminy
|
Couplet = 2 PVCs in a row
Triplet = 3 PVCs in a row Bigeminy = every other beat is a PVC Trigeminy = every 2 beats is a PVC Quadgeminy = every 3 beats is a PVC |
|
|
How can you tell if PVCs are unifocal?
|
They all look the same.
|
|
|
What is amiodarone (Pacerone/Cordorone)? When is it used? What is the dosing?
|
*An anti-arrhythmic.
*Slows sinus rate, increases PR & QT, increases vasodilation. *Used for V-fib, pulseless V-tach *Give 300mg IV/IO once, then consider 150mg IV/IO once |
|
|
What is ventricular tachycardia? How do you treat VT w/ pulse and VT w/o pulse?
|
* No P waves, obscured if present.
* Rate between 100-250 bpm * Rhythm is three or more ventricular beats in a row; may be regular or irregular. TX (w/ pulse): synchronized cardioversion TX (w/o pulse): shock, epi or vaso, shock, amiodorone or lidocaine, shock Stable VT is treated with lidocaine, procainamide, amiodarone or may go directly to sedation and cardioversion. |
|
|
What is the dosing for amiodarone when treating VT or VF?
|
300mg IV/IO once, then consider 150mg once
|
|
|
What is the dosing for lidocaine when treating VT or VF?
|
1 to 1.5 mg/kg first dose then 0.5 to 0.75 mg/kg IV/IO, max 3 doses or 3 mg/kg
|
|
|
What is ventricular fibrillation? What is the treatment?
|
No organized contraction. No P waves or obscured if present. Results in the absence of cardiac output.
shock, epi or vaso, shock, amiodarone or lidocaine, shock |
|
|
What medication would you give for torsade de pointes?
|
magnesium 1 to 2 g IV/IO
|
|
|
What is atropine and when is it given?
|
Atropine is an anticholinergic. It blocks PNS signals & leads to increased HR @ intermediate doses.
0.5 mg used in sinus bradycardia. 1 mg used in asystole or slow PEA rate q 3-5 minutes. Use after epi and vasopressin |
|
|
What are symptoms of arrhythmias?
|
* Shortness of breath
* Chest pain * Decreased LOC * Low BP * Slow or fast HR varying greatly from baseline * Pulmonary edema * Congestive heart failure * Acute MI or shock |
|
|
What are the elements of Normal Sinus Rhythm?
|
* Regular Rhythm
* Rate 60-100 bpm * P waves uniform and before each QRS * PR < 0.20 * XRS < 0.12 |
|
|
What is cardiac tamponade?
|
Fluid accumulates in the pericardium (the sac in which the heart is enclosed). If the fluid significantly elevates the pressure on the heart it will prevent the heart's ventricles from filling properly. This in turn leads to a low stroke volume.
Will hear distant or muffled heart sounds. Will see decreased cardiac output. The end result is ineffective pumping of blood, shock, and often death. |
|
|
What is the treatment for asystole or PEA (pulseless electrical activity)?
|
CPR, epi or vasopressin, atropine, consider transcutaneous pacing
Try to treat the cause. (H's & T's) |
|
|
What are some possible causes for asystole or PEA? (Hs and Ts)
|
Hypovolemia, Hypoxia, Hydrogen ion (acidosis), Hypo/hyperkalemia, Hypoglycemia, Hypothermia
Toxins, Tamponade, Tension pneumothorax, Thrombosis (coronary or pulmonary), Trauma |
|
|
What is Torsades de Pointes?
|
A form of VT in which the QRS complexes appear to be constancy changing.
"Spindle" |
|
|
Why can PVCs be bad?
|
If it falls on a T wave, it can precipitate VT or VF.
|
|
|
How are PVCs treated?
|
In the setting of an acute MI --> MONA
Lidocaine is drug of choice but does little to the underlying pathology. |
|
|
What are the characteristics of atrial fibrillation?
|
No P wave
QRS normal Rhythm = irregularly irregular No contraction of the atria as a whole (lose 20% EF) |
|
|
What is the 7 step method to analyze a rhythm?
|
1. Determine the rate (atrial & ventricular)
2. Decide if the rhythm is regular or irregular 3. Analyze the P wave 4. Measure the PR interval 5. Is every P wave followed by a QRS? 6. Analyze the QRS complex 7. Measure the QT interval |
|
|
What is the treatment for A-fib?
|
1. Stop Procedure
2. Assess ABC's 3. If patient unstable --> synchronized cardioversion 4. If stable, control the rate with calcium channel blockers (diltiazem or verapamil), beta-blockers, or digoxin. 5. Maintain rhythm with amiodarone, procainamide, flecanide. |
|
|
How do you treat chronic A-fib (> 48 hours)?
|
- Chemical cardioversion, after a period of anti-coagulation
- Electrical cardioversion only after anti-coagulation |
|
|
What are the characteristics of atrial flutter?
|
- P waves become Flutter waves and have a "sawtooth appearance".
- QRS normal - 2:1 atrial to ventricular conduction most common - Ventricular rate varies depending on the number of impulses the AV node is blocking --> usually regular |
|
|
What is the relationship between the P waves and the QRS complexes?
|
If PR > 0.20 seconds, it may be some type of heart block.
|
|
|
How many kinds of heart blocks are there?
|
4 kinds.
1st Degree 2nd Degree Type I 2nd Degree Type II 3rd Degree |
|
|
What is the treatment for 3rd Degree Heart Block?
|
- Assess ABC's.
- If unstable, prepare for transcutaneous pacing. - Consider Atropine 0.5 mg while awaiting pacer. May repeat to max 3 mg. - Consider epi or dopamine infusion while awaiting pacer or if pacing ineffective. |
|
|
What is Romazicon (flumazenil)?
|
Benzodiazepine antidote
|
|
|
What is Narcan (nalaxone)?
|
opioid antidote
|
|
|
What is Digibind?
|
Digoxin antidote
|
|
|
What are some causes of slow rhythms?
|
Hypoxia, hyperkalemia, acute MI, Heart disease, incrased parasympathetic tone, drug effects from narcotics, benzodiazepines, digoxin, beta blockers, propanolol, or calcium channel blockers.
|
|
|
What is the treatment of unstable sinus bradycardia.
|
- Atropine 0.5 mg. May repeat to a total dose of 3 mg.
- If ineffective, begin pacing. - Consider epinephrine ( 2-10 mcg/min) or dopamine (2-10 mcg/kg per min) - Transvenous pacemaker |
|
|
What are some causes of fast rhythms?
|
Hypoxia, emotional and physical stress, caffeine, smoking, exercise, fatigue, alcohol, pain, infection, cardiomyopathy, fever
|
|
|
What is the tx for sinus tachy?
|
alleviate the underlying cause
|
|
|
What are characteristics of SupraVentricular Tachycardia?
|
- Rhythm is regular.
- Rate = 150-220 bpm - P waves may be buried in the T wave and may differ in morphology from sinus P waves - PR and QRS interval may be normal or prolonged. |
|
|
What is the treatment for SVT?
|
- Treat the cause
- Reduce HR by stimulating the vagus nerve by carotid massage or - Valsalva maneuver. - Medications to decrease rate = adenosine, calcium channel blockers, beta blockers. - If patient is unstable, cardioversion. |
|
|
What is paroxymal supraventricular tachycardia?
|
SVTs that have a sudden, almost immediate onset.
|
|
|
What does SVT mean?
|
Supraventricular tachycardia. Any tachycardia that is not ventricular in origin. Includes sinus tachycardia and junctional tachycardia.
|
|
|
What is junctional tachycardia?
|
Tachycardia originating from the AV node
|
|
|
What can cause JVD?
|
Damaged liver, right heart failure, venous HTN, tumors in chest, collapsed lung
|
|
|
What can a deviated trachea indicate?
|
tension pneumothorax
|
|
|
What is someone with neck surgery at high risk for?
|
Complications with airway that can lead to airway problems.
|
|
|
What is flail chest?
|
- A segment of the chest wall breaks & becomes detached from the rest of the chest wall.
- The flail segment moves in the opposite direction as the rest of the chest wall. |
|
|
What is tactile fremitus?
|
you feel more vibrations in the chest when the client speaks
|
|
|
Where is the PMI usually located? What can a deviated PMI indicate?
|
Mid-clavicle between the 4th and 5th rib. A deviated PMI can indicate pheumothroax.
|
|
|
What can enlarged spinous processes lead to?
|
Skin breakdown.
|
|
|
How many lobes does the right lung have?
|
3
|
|
|
How many lobes does the left lung have?
|
2
|
|
|
What makes up the S1 heart sound?
|
The AV valves (Bicuspid/mitral and Tricuspid) closing as the ventricles
|
|
|
What makes up the S2 sound?
|
Closure of the aortic and pulmonic valves.
|
|
|
What do pulsations in the abdomen tell us?
|
Not to touch
|
|
|
What is the patient:nurse ration in the ED?
|
4:1
|
|
|
Describe crisis intervention in the ED? What are some examples of crisis?
|
Everyone who comes to the ED is in some sort of crisis. We help them through these crisis. Examples are rape, car accidents, poisoning, heart attacks.
|
|
|
What is a trauma center?
|
a hospital equipped to provide comprehensive emergency medical services to patients suffering traumatic injuries.
|
|
|
What is trauma?
|
Trauma is any life-threatening occurrence, either accidental or intentional, that causes injuries. The leading causes of trauma are motor vehicle accidents, falls, and assaults.
|
|
|
What are the different levels of trauma centers?
|
Level 1 - involved in research & education; MD available 24 hours.
Level 2 - Surgeons on call Level 3 - They have a programmed service but surgeons not there all the time. |
|
|
What types of trauma are there?
|
- Blunt vs. penetrating
- Burns - Drowning |
|
|
What is the primary assessment for trauma?
|
A = Airway
B = Breathing C = Circulation D = Disability |
|
|
What are the secondary assessments for trauma?
|
E = Exposure / Environmental Control
F = Full Set of Vital Signs/ Give Interventions/ Facilitate Family Presence G = Give Comfort Measures H = History and Head to Toe Assessment |
|
|
What are some Common Problems of Critical Care Patients?
|
Nutrition
Anxiety Pain Impaired communication Sensory –perceptual problems Sleep problems |
|
|
What are some nursing diagnoses related to Home Health?
|
Knowledge deficit
Ineffective management of therapeutic regimen related to: -Medications -Diet and nutrition -Activity limitations -Tests and procedures -Disease process -Community resources |
|
|
What are other names for Hospice?
|
Palliative care
end-of-life care comfort care |
|
|
The valsalva manuever is used in which arrhythmia?
|
SVT
|
|
|
What does the Valsalva Maneuver ultimately do to the heart?
|
Lowers HR
|
|
|
What is Starling's Law?
|
The greater the stretch of cardiac muscle, the greater the force of contraction
|
|
|
What are the EKG intervals we need to memorize?
|
PR interval < 0.20
QRS interval < 0.12 QT interval < 0.44 |
|
|
List the cardiac enzymes used to assess if cardiac muscle injury has occurred.
|
Troponin
CK-MB Lactase Dehydrogenase Myoglobin Creatine Kinase-MB |
|
|
Troponin T and I? Levels?
|
These are contractile proteins of the myofibril. The cardiac isoforms are very specific for cardiac injury and are not present in serum from healthy people.
Rises 2 - 6 hours after injury Peaks in 12 - 16 hours I stays elevated for 5-10 days, T for 5-14 days |
|
|
Creatine Kinase (CK-MB)? Levels?
|
Rises and returns to normal sooner than total CK
Rises in 3-4 hours Returns to normal in 2 days MB2 is released from heart muscle and converted in blood to MB1. A level of MB2 equal or greater than 1.0 U/L and an MB2/MB1 ratio equal or greater than 1.5 indicates myocardial infarction. |
|
|
Myoglobin
|
Found in striated muscle. Damage to skeletal or cardiac muscle releases myoglobin into circulation.
Rises fast (2 hours) after myocardial infarction Peaks at 6 - 8 hours Returns to normal in 20 - 36 hours Have false positives with skeletal muscle injury and renal failure. |
|
|
Can you defibrillate over nitro paste?
|
No, so when you apply nitro paste, don't apply it on the chest where the defibrillator pads could go.
|
|
|
How many liters of O2 can you give with a non-way breather mask?
|
10-15 L
|
|
|
What does morphine do?
|
Decrease pain and dilates blood vessels therefore decreasing workload on heart
|
|
|
What does aspirin do?
|
Decrease platelet aggregation
|
|
|
What are risk factors for coronary artery disease (CAD)? Which are modifiable?
|
Age, gender, genetic makeup, ethnicity
Modifiable: smoking, HTN, high cholesterol, diet, exercise, obesity |
|
|
Why can a person appear pale, diaphoretic, and extremely anxious when they're in pain?
|
Pain can cause a release of catecholamines (epinephrine) which cause vasoconstriction.?????
|
|
|
What does a nursing diagnosis look at?
|
It looks at how the patient responds to the disease.
|
|
|
What is Angina?
|
Narrowing of blood vessels leading to ischemia and pain. Is transient. Decreased supply of blood supply to the heart. Cold weather can induce angina.
|
|
|
What is an MI?
|
Total occlusion of one of the coronary vessels
|
|
|
Who are at increased risk for silent MI's?
|
diabetics
|
|
|
What is transcutaneous pacing aka external pacing?
|
During transcutaneous pacing, pads are placed on the patient's chest, either in the anterior/lateral position or the anterior/posterior position.
May be uncomfortable for the patient. Sedation should therefore be considered. Prolonged pacing may cause burns on the skin. It is meant to stabilize the patient until a more permanent means of pacing is achieved. |
|
|
What is transvenous pacing aka endocardial pacing?
|
A pacing electrode is threaded through a vein into the right atrium, right ventricle, or both.
The greater use of atropine and epinephrine or external pacing may obviate the need for transvenous pacing by stabilizing patients early in the process of caring for the patient. Some debate exists over the efficacity and reliability of transvenous pacing, especially if the need for permanent pacing is anticipated. |
|
|
What is an internal pacemaker?
|
Permanent pacing with an implantable pacemaker involves transvenous placement of one or more pacing electrodes within a chamber, or chambers, of the heart. The procedure is performed by incision of a suitable vein into which the electrode lead is inserted and passed along the vein, through the valve of the heart, until positioned in the chamber. The procedure is facilitated by fluoroscopy which enables the physician or cardiologist to view the passage of the electrode lead. After satisfactory lodgement of the electrode is confirmed the opposite end of the electrode lead is connected to the pacemaker generator.
|
|
|
How do you know if a pacemaker is capturing/working?
|
You will see a pacer strike on the monitor followed by a QRS
|
|
|
What should you teach a patient about having an internal pacemaker?
|
- Patient should check his pulse if he feels palpitations or if he feels different because his pacer might not be working.
- Be careful around magnets - Don't let anyone touch your wound while its healing - Wear ID card or bracelet saying you have a pacemaker - Teach signs of bradycardia |
|
|
What are symptoms of bradycardia?
|
fatigue, weakness, dizziness, lightheadedness, fainting, chest discomfort, palpitations or shortness of breath
|
|
|
What position should a patient be in for a portable chest x-ray and why?
|
As high as possible because this helps identify if fluid or air is in the chest. Be careful because if the patient has decrease BP, he might lose perfusion to his brain. Air will be black on the xray, solid/fluid will be white.
|
|
|
What are presenting signs of an AMI?
|
Chest pain/discomfort, SOB, pale, diaphoretic, radiation to arm, neck or jaw, epigastric pain, dyspnea
|
|
|
What's the difference between Dilaudid and morphine?
|
dilaudid won't give you the euphoric effect
|
|
|
What is shock?
|
a serious, life-threatening medical condition where insufficient blood flow reaches the body tissues. As the blood carries oxygen and nutrients around the body, reduced flow hinders the delivery of these components to the tissues, and can stop the tissues from functioning properly
|
|
|
What kinds of shock are there?
|
Hypovolemic
Cardiogenic Septic Anaphylactic neurogenic obstructive endocrine |
|
|
What is dobutamine?
|
a sympathomimetic drug used in the treatment of heart failure and cardiogenic shock.
Increases BP but decreases afterload (work on the heart) |
|
|
What is afterload?
|
the pressure that the chamber of the heart has to generate in order to eject blood out of the chamber
|
|
|
What are specific considerations & concerns with a diabetic?
|
- Healing times longer
- Clarify meds b/c BG will increase due to stress - Close eye on I & O's - Renal function can be affected by dyes --> diabetics already have problems with this so watch carefully |
|
|
What are some S & S of hypoglycemia?
|
hunger, shakiness, nervousness, sweating, dizziness or light-headedness, sleepiness, confusion, difficulty speaking, anxiety, weakness
|
|
|
What does AACN stand for?
|
American Association of Critical Care Nurses
|
|
|
CI. What are the normal values.
|
Cardiac Index. It relates the cardiac output to the body surface area.
Normal = 2.6-4.2 L/min per square meter |
|
|
CO and normal values
|
Cardiac Output.
The amount of blood, in particular a ventricle, in one minute. Male = 5 L/min Female = 4.5 L/min |
|
|
CVP
|
Central venous pressure.
The pressure of blood in the thoracic vena cava, near the right atrium of the heart. Reflects the amount of blood returning to the heart and the ability of the heart to pump the blood into the arterial system. |
|
|
ETCO2
|
End-tidal carbon dioxide
|
|
|
FIO2
|
Fraction of Inspired oxygen
|
|
|
IABP
|
Intraaortic balloon pump
|
|
|
MAP
|
mean arterial pressure
|
|
|
PA
|
Pulmonary artery
|
|
|
PAS, PAD
|
pulmonary systolic (pressures)
pulmonary diastolic (pressures) |
|
|
PAWP
|
pulmonary artery wedge pressure
|
|
|
PVR
|
pulmonary vascular resistance
|
|
|
ScvO2
|
Percent oxygen saturation of hemoglobin in venous blood (e.g. in the superior vena cava)
|
|
|
SpO2
|
Percent oxygen saturation of hemoglobin measured by pulse oximetry
|
|
|
SvO2
|
Percent oxygen saturation of hemoglobin in mixed blood (e.g. in the pulmonary artery)
|
|
|
SV, SVI
|
Stroke volume - the volume of blood pumped by the right/left ventricle of the heart in one contraction.
stroke volume index - the stroke volume per body surface area |
|
|
SVR, SVRI
|
systemic vascular resistance - The resistance offered by the peripheral circulation that must be overcome to push blood through the circulatory system.
systemic vascular resistance index - Systemic vascular resistance normalized for body surface area |
|
|
VAD
|
ventricular assist device.
A ventricular assist device (VAD) is a mechanical pump that helps a heart that is too weak to pump blood through the body. It is sometimes referred to as “a bridge to transplant” since it can help a patient survive until a heart transplant can be performed. |
|
|
What are some reasons a patient might be admitted to the ICU?
|
physiologically unstable, at risk for serious complications, require frequent and invasive assessment, require intensive and complicative nursing support related to the use of intravenous polypharmacy
|
|
|
What does CMSTP stand for? When would you use it?
|
Color. Motor. Sensation. Temperature. Pulse. Use it when you're testing the extremities for for damage in the extremities.
|
|
|
What can low dose and high dose dopamine be used for?
|
Low dose dopamine is for renal perfusion. High dose dopamine is for vasoconstriction.
|
|
|
What is an intra-aortic balloon pump?
|
A balloon catheter that lies below the aortic arch and inflates/deflates with the heart. It increases coronary artery perfusion and decreases cardiac work.
|
|
|
What would you see if an intraaortic pump slid up or slid down?
|
Slides up = might affect head or arm
slides down = might affect kidneys. Check I & O |
|
|
How often should vital signs be checked immediate post-cardiac surgery.
|
q 15 min x4 then q 30 min x2 then q 1 hr x2
|
|
|
What are some immediate post-cardiac orders?
|
Bed rest, angioseal or pressure on artery site x20-30 min, VS, check CMSTP in extremities for clots, check I&O's for renal perfusion, check site for bleeding, pain management, LOC & respiratory for clots, cardiac monitor for arrhythmias, if stent placed the coronary artery could rupture leading to cardiac tamponade --> JVD, muffled heart sounds.
|
|
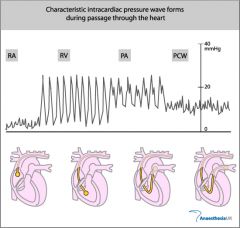
What type of pressure do we get in the right atrium?
|
CVP - Central Venous Pressure
|
|
|
What does the proximal port on a pulmonary artery catheter measure? What if the value is high or low?
|
CVP - central venous pressure - proximal port is found in the right atria. If the value is high, that could indicate right sided heart failure or fluid overload. If it is low, it could indicate dehydration.
|
|
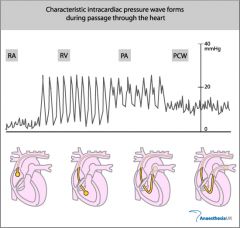
What kind of pressures do we get in the right ventricle?
|
Systolic and diastolic pressures
|
|
|
What is PCWP and what does it measure?
|
Pulmonary Capillary Wedge Pressure. It provides an indirect estimate of left arterial pressure (LAP).
|
|
|
What is the risk with inserting a PA catheter into the heart?
|
It can irritate the heart and cause VT or VF
|
|
|
What are the points of entry for a PA catheter?
|
- Internal or External Jugular
- Antecubital - Femoral vein - Subclavian |
|
|
What are the steps in the nursing process?
|
- Assessment (of patient's needs)
- Diagnosis (of human response needs that nurses can deal with) - Planning (of patient's care) - Implementation (of care) - Evaluation (of the success of the implemented care) |
|
|
List some of the cardiac anti-arrhythmics
|
adenosine, flecainide, lidocaine, verapamil, diltiazem, beta blockers, procainamide, digoxin, amiodarone
|
|
|
What is Acetylcholine?
|
A neurotransmitter used in the parasympathetic nervous system
|
|
|
What medications are used in A-fib or A-flutter?
|
diltiazem, beta blockers, procainamide
|
|
|
Which medication treats PSVT? Which medications are used for recurrences?
|
Adenosine.
Adenosine, diltiazem, beta blockers |
|
|
What medication would you give to treat stable VT?
|
amiodarone 150mg IV over 10 minutes. Repeat as needed to max dose of 2.2 g/ 24 hrs. Prepare for elective synchronized cardioversion.
|
|
|
What are some sympathetic nervous syste agonists?
|
Epinephrine
Norepinephrine Dopamine Dobutamine |
|
|
When is atropine used?
|
Bradycardia.
Asystole/PEA after epi/vaso given. |
|
|
What is atropine?
|
An anticholingergic. PNS blocker. Leads to increased HR. Used for sinus bradycardia.
|
|
|
What is lidocaine?
|
An anti-arrhythmic used for control of ventricular arrythmias.
1 to 1.5 mg/kg first dose then 0.5 to 0.75 mg/kg max 3 doses or 3 mg/kg |
|
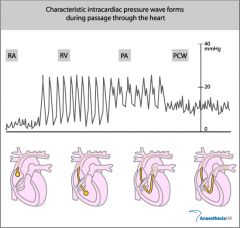
What does the pressure in the pulmonary artery reflect?
|
Pressure inside the lungs
|
|
|
What does CVP tell us?
|
Central venous pressure and preload
|
|
|
What is the normal pH for Arterial Blood?
|
7.35-7.45
|
|
|
What is the normal PCO2 for Arterial Blood?
|
35-45 mm Hg
|
|
|
What is the normal HCO3- for Arterial Blood?
|
22-27 mEq/L
|
|
|
What is the normal PO2 for Arterial Blood?
|
80-100 mm Hg
|
|
|
What are some causes of Respiratory Acidosis?
|
Asthma, atelectasis, brain trauma, bronchiectasis, bronchitis, CNS depressants, emphysema, hypoventilation, pulmonary, edema, pneumonia, pulmonary emboli
|
|
|
What are some causes of respiratory alkalosis?
|
Fever, hyperventilation, hypoxia, hysteria, overventilation by mechanical ventilators, pain
|
|
|
What are some causes of metabolic acidosis?
|
DM or DKA, excessive ingestion of aspirin, high-fat diet, insufficient metabolism of carbs, malnutrition, renal insufficiency or renal failure, severe diarrhea
|
|
|
What are some causes of metabolic alkalosis?
|
diuretics, excessive vomiting or GI suctioning, hyperaldosteronism, ingestion of and/or infusion of excess sodium bicarbonate, massive transfusion of whole blood
|
|
|
Respiratory Alkalosis leads to hypokalemia. True or False.
|
True
|
|
|
List the Cranial Nerves
|
I - Olfactory
II - Optic III - Oculomotor IV - Trigeminal V - Trochlear VI - Abducens VII - Facial VIII - Vestibulocochlear XI - Glossopharangeal X - Vagus XI - Accessory XII - Hypoglossal |
|
|
What is Cranial Nerve I. How would you test it?
|
Olfactory.
Is the patient able to smell if one nostril is plugged? |
|
|
What is Cranial Nerve II. How would you test it?
|
Optic.
Ask patient to cover one eye, look forward, and you check peripheral sight with one finger. |
|
|
What is Cranial Nerve III. How would you test it?
|
Oculomotor
Have patient stare at your pen or finger. Make sign of the cross and an X. Do their eyes move together |
|
|
What is Cranial Nerve IV. How would you test it?
|
Trochlear
Have patient stare at your pen or finger. Make sign of the cross and an X. Do their eyes move together |
|
|
What is Cranial Nerve V. How would you test it?
|
Trigeminal
Have patient close their eyes. Use a "fine tip" and poke along the side of their face. Can they feel it? |
|
|
What is Cranial Nerve VI? How can you test it?
|
Abducens
Have patient stare at your pen or finger. Make sign of the cross and an X. Do their eyes move together |
|
|
Which cranial nerves can you check using the same test.
|
III. Oculomotor
IV. Trochlear VI. Abducens AND IX. Glossopharangeal X. Vagal |
|
|
What is Cranial nerve VII? How can you test it?
|
Facial
Ask them to give you a big smile. Is it symmetrical? |
|
|
What is Cranial Nerve VIII. How can you test it?
|
Vestibulocochlear
Have patient close both eyes and make light sounds progressively closer to each ear. Can they hear it? |
|
|
What is Cranial Nerve XI. How can you test it?
|
Glossopharangeal
Test for patient's gag reflex by having the patient open the mouth and you use a tongue depressor to touch the soft palate or posterior pharynx at the back of the mouth. The palate should elevate, the tongue should retract, and the pharangeal muscles should constrict. |
|
|
What is Cranial Nerve X? How do you test it?
|
Vagal
Same as testing Cranial Nerve XI |
|
|
What is Cranial Nerve XI? How do you test it?
|
Accessory
Have patient shrug shoulders and move had left and right against resistance |
|
|
What is Cranial Nerve XII? How do you test it?
|
Hypoglossal
Have patient stick out tongue. |

