![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
70 Cards in this Set
- Front
- Back
|
What is polycythemia?
What do we see in the CBC? What types of polycythemia exist? |
↑RBC in the blood vol. (not nO/platelets like in HM)
↑PCV/↑HCT (above RI) Relative & absolute. |
|
|
Relative polycythemia can be due to...
|
Dehydration (H20 loss)
Fluid shifts (edema) Excitement (↑cortisol → ↓margination = ↑PCV) Exercise (spleen contracts → ↑PCV) |
|
|
Absolute polycythemia can be due to...
|
・↑EPO
Appropriate (chronic hypoxia) Inappropriate (Renal cysts/tumors (suffocate renal cells) → ↑EPO ・Primary polycythemia/polycythemia vera (BM makes too many RBCs (myeloproliferative disorder)) |
|
|
What are 3 causes of hypoxia that will stimulate ↑EPO (appropriate)?
|
High altitude
Pulmonary disease Congenital heart defects (eg. PDA) H (heart) y (sky) p (pulmonary) |
|
|
What do we suspect in puppies with an ↑PCV/↑HCT?
|
Patent Ductus Arteriosus (PDA)
|
|
|
If PCV & TP is increased, what do we suspect?
|
Relative polycythemia
・Dehydration (H20 loss) |
|
|
How can we distinguish acute renal failure from chronic renal failure?
|
In acute renal failure we will see an ↑PCV while in chronic renal failure we expect to see an anemia (↓EPO).
|
|
|
Why do we see hypocalcemia in ethylene glycol poisoning?
|
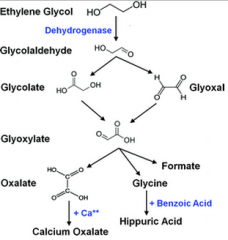
Ca combines with oxalate to form calcium oxalate (monohydrate) crystals.
|
|
|
PCV (%): 69 (RI: (37-55))
TP: Normal Arterial O2: Normal EPO: Increased Appropriate/inappropriate ↑EPO? Why? |
Inappropriate because Arterial O2 is normal
|
|
|
PCV (%): 71 (RI: (37-55))
TP: Normal Arterial O2: Normal EPO: Normal At rest Dx? |
Not dehydrated
EPO not being produced Only option left is Polycythemia vera |
|
|
PCV (%): 62 (RI: (37-55))
TP: Normal Arterial O2: Decreased EPO: Increased Appropriate/inappropriate ↑EPO? Why? What exams should we do next? |
Appropriate because animal is hypoxic.
Heart & lung exams should be performed. |
|
|
Define leukemia:
|
Presence of neoplastic cells in PERIPHERAL BLOOD (not always) &/ BM or spleen.
“Leuk” means white and “emia” means blood |
|
|
Why would we like to identify cell type in lymphoproliferative disorders/myeloid neoplasms?
|
Chemotherapy & prognosis differs.
|
|
|
What type of leukemias cause:
Anemia NeutroPENIA ThrombocytoPENIA |
Acute Lymphoblastic leukemia
Acute Myeloid leukemia |
|
|
Types of leukemia (all originate from the BM):
1. Aleukemic leukemia: 2. Subleukemic leukemia: 3. Leukemic leukemia: |
1. No cancer cells in circulation
2. Small amounts of cancer cells in circulation 3. Many cancer cells in circulation |
|
|
Maturity of leukemia:
1. Acute leukemia: 2. Chronic leukemia: |
1. Proliferation of blasts (tends to be more severe)
2. Proliferation of more mature blood cells (tends to be less severe) |
|
|
What are the 2 major types of proliferative disorders (leukemias)?
|
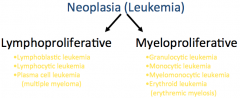
|
|
|
What are the different types of lymphoproliferative disorders?
|
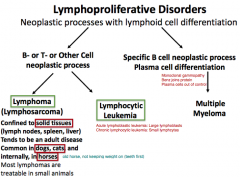
Lymphoma (confined to solid tissues)
Lymphocytic Leukemia ・Acute lymphoblastic leukemia (Lg lymphoblasts) ・Chronic lymphocytic leukemia (small lymphocytes) Multiple Myeloma |
|
|
On a CBC, what is important for Dxing a leukemia?
What are the normals for lymphocytosis in: Excitement response (Cats) Antigenic stimulation (Dogs ehrlichia +) With ehrlichia Agic stimul, what else will be evident? Dogs ehrlichia -, maximum lymphocytosis? |
Lymphocytosis magnitude & morphology
Excitement response: **20,000** = max Ag response: **35,000** = max (rare in SA otherwise) Lg Granular Lymphocytes & Polyclonal Gammopathy Ehrlichia -: **15,000** = max |
|
|
1. [Lymphocyte] = 34,000/µl & ehrlicia +, Dx?
2. [Lymphocyte] = 38,000/µl & ehrlicia -, Dx? 3. [Lymphocyte] = 19,000/µl & ehrlicia -, Dx? |
1. Dx: Ag response to ehrlicia
2. Dx: Leukemia 3. Dx: Leukemia |
|
|
How else can we Dx neoplastic lymphoproliferative diseases (lymphocytic/blastic leukemias, multiple myeloma, lymphomas)?
|
Morphology
Immunophenotyping (determines B/T cell neoplasia) PCR for lymphoma |
|
|
Which cells' morphology do we compare to identify the type of leukemia?
|
nO & Lymphocytes (LO size > nO size, then worry)
|
|
|
We must differentiate Acute Lymphoblastic Leukemia (ALL) from ____. How?
|

Stage V Lymphoma
(→ lymphadenopathy (enlarged LNs)) = cancerous lymphocytes spill into the bloodstream. |
|
|
With ALLs, what is often evident in a CBC if untretd?
What clinical signs are associated with ALL? |
Multiple cytopenia (lack of norm hematopoietic cells)
Clinical signs: Pale MM, Spleno/Hepatomegaly, Lethargy, Wt. loss |
|
|
CBC shows:
Anemia NeutroPENIA ThrombocytoPENIA Lymphocytosis Lymphoblasts in blood (not always) If lymphoproliferative disorder, then Dx? |
Acute Lymphoblastic Leukemia
|
|
|
How can we identify lymphblasts?
|
Morphology
Immunophenotyping Cytochemistry (Neg. for most cytochemical stains except **nonspecific esterase**) |
|
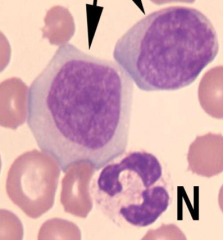
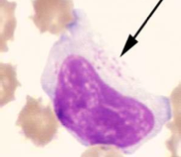
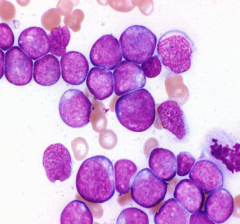
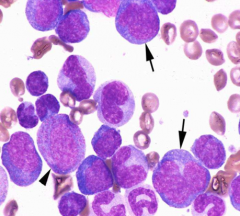
Identify the cells indicated by the arrows.
What are some characteristics that distinguish them? |
Lymphoblasts
Visible nucleolus & larger than the nO |
|
|
Young cats with ALL are usu. FeLV ___.
Prognosis for ALL is usu. ___. |
Positive
Poor (rapid, progressive, poorly responsive to therapy) |
|
|
Acute Lymphocytic Leukemia (ALL) is often characterized by ___.
Chronic Lymphocytic leukemia (CLL) is often characterized by ___. |
Lymphoblasts
Small & well differentiated lymphocytes. |
|
|
CLL is most common in ___.
What must we differentiate CLL from? |
Dogs
Differentiate from other causes of lymphocytosis: Dogs ・>15,000 ・Chronic Ehrliciosis Agic stimulation (<35,000) Cats ・Excitement stimulation (< 20,000) ・Bartonella henselae ("Cat Scratch Fever") |
|
Identify the cell:
What is this indicative of? Why is this significant? |
Large Granular Lymphocytes
Indicative of Chronic ehrliciosis If Lymphocytosis present, it is due to chronic ehrlicia |
|
|
CBC shows:
Anemia ThrombocytoPENIA Lymphocytosis ↑small LO in BM If lymphoproliferative disorder, then Dx? |
Chronic Lymphocytic Leukemia
|
|
|
Young cats with CLL are usu. FeLV ___.
Prognosis? |
Negative
Untreated animals may live for years. |
|
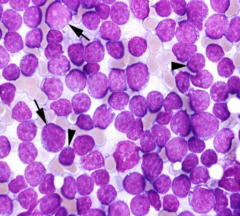
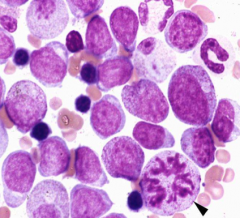
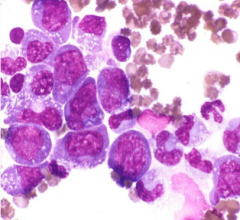
BM aspirate.
Dx? |
Chronic Lymphocytic Leukemia
Occasional blast but more small lymphocytes crowding out other hematopoeitic precursors. |
|
|
Phenotypic classification of Chronic Lymphocytic Leukemia is done by ___.
___ (often LGLs) are more common in dogs & cats than is ___. ___ tends to proliferate in spleen. |
Flow cytometry
T-Cell CLL/B-Cell CLL T-Cell |
|
|
What does PCR do in respect to leukemias?
|
Detect Ag receptor rearrangements:
Identify & differentiate neoplastic population of cells and neoplastic disorders from non-neoplastic lymphoproliferative disorders |
|
|
What is multiple myeloma?
Will we see an ↑plasma cells in the peripheral blood? |
Proliferation of PLASMA cells at various sites in d BM
Occasionally but rarely. |
|
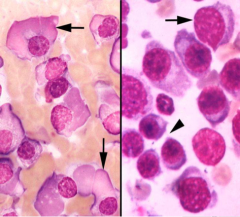
Bone marrow aspirate:
Identify the cells on the left. Identify the cells on the right. Dx of either patient? |
Left: Flame cells with Ig in cytoplasm
Right: Abnormal plasma cells Dx: Multiple myeloma |
|
|
How does the [Hi] of Ig affect the blood?
|
↑viscosity (hyperviscosity → affect circulation (CNS, Retinal & Cardiac problems.
|
|
|
1. What % of plasma cells must be found within BM to confirm multiple myeloma?
2. What must multiple myeloma be differentiated from? |
1. 20% of plasma cells in BM & in aggregates.
2. Chronic Ag stimulation |
|
|
1. How can we differ multiple myeloma from chronic Ag stimulation?
2. What would we expect as the results? 3. What are the proteins made by the abnormal plasma cells referred to? 4. What will we discover in the urine? |
1. Running a protein electrophoresis
2. Monoclonal gammopathy (sometimes biclonal) 3. Referred to PARAPROTEINS 4. Bence-Jones proteins (separated light chains) |
|
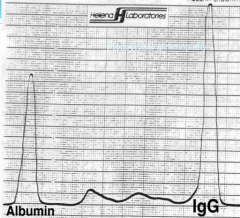
What are we seeing here?
Dx? What is the general rule? |
Monoclonal Gammopathy
Multiple Myeloma Rule: If peak is 4x taller than the width then it is multiple myeloma. |
|
|
What pathologic effects are associated with multiple myeloma?
|
・Hyperviscosity syndrome (↑Ig)
・Osteolysis (PCs → osteoclastic activating factor) ・Cytopenia (Pancytopenia) ・Non-regenerative anemia ・Hypercalcemia (→ Renal dz. (from OAF → Ca)) ・Renal dz (PU/PD (paraprotein-induced)) ・Hemorrhaging: epistaxis, intraocular (paraprotein-induced thrombocytopathy) CR3HON |
|
|
What are some special consideration for cats with multiple myeloma?
|
・Anemia (non-regenerative)
・Bone lesions (PCs → osteoclastic activating factor) ・Organ involvement (v. common in cats) ・ATYPICAL PLASMA cell morphology (vs. differentiated in dogs) |
|
|
Azotemia
Severe anemia Neutropenia Thrombocytopenia Prognosis? Hypercalcemia Bence-Jones proteinuria Plasma Cell leukemia Extensive bone lesion Survival time? |
Prognosis: Bad with those signs
Survival time: Short with those signs |
|
|
What is indicated with a Hi [protein]?
What should a NON-REGENERATIVE ANEMIA & THROMBOCYTOPENIA trigger? |
Protein electrophoresis
Trigger: BM aspirate |
|
|
What are 4 indications of multiple myeloma?
|
・Monoclonal gammopathy
・↑plasma cells in BM (20% or more) ・Lytic lesions in bones (+/-) ・Bence-Jones proteinuria (light chains of Ig) |
|
|
How do myeloid neoplasms manifest?
|
・Either by LACK of NORMAL CELLS in the blood/presence of neoplastic cells.
|
|
|
1. What MYELOID cancer is associated with RAPID disease progression?
2. What 2 MYELOID cancers are associated with GRADUAL disease progression? |
1. Acute MyeloID Leukemia (AML)
2. MyeloDYSplastic Syndromes (Preleukemic) & MyeloPROliferative Neoplasms |
|
|
1. How do we distinguish acute (RAPID) from chronic (GRADUAL)?
2. To be considered Acute MyeloID leukemia by definition, ___% or greater BLAST cells must be present in the BM. |
1. % of blast cells in MARROW
2. 20% or greater (% of blasts in BLOOD is variable) |
|
|
What are some features of MyeloDYSplastic Syndromes (MDS; preleukemic)?
|
✓Morphologic abnormalities
・Erythrocytes & RBC precursors abnormally LARGE ・Platelets & nO may also be abnormally LARGE ・Dysynchrony of nuclear & cytoplasmic maturation ✓Cytopenia ・Non-regenerative anemia ・Neutropenia (but Lg) ・Thrombocytopenia (but Lg) ✓BM Hypo/Normal/Hypercellular |
|
|
What will we expect to see as a MCV & histogram?
|
High MCV = Macrocytosis
Histogram: Anisocytosis (widening of histogram) |
|
|
Cat comes into clinic
MCV: HIGH Non-regenerative anemia What do we test for? |
FeLV
|
|
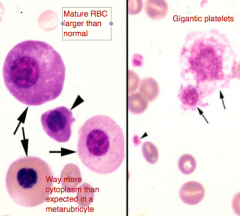
1. Dysplastic erythroid cells (1) & dysplastic giant platelets (2) suggest what Dx.?
2. If this was a cats BM film, what induced it? |
1. MyeloDYSplastic Syndrome (MDS; preleukemic)
2. FeLV (usu.) |
|
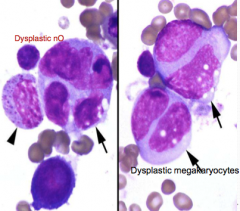
1. Dysplastic neutrophils & dysplastic megakaryocytes (2) suggest what Dx.?
2. If this was a cats BM film, what induced it? |
1. MyeloDYSplastic Syndrome (MDS; preleukemic)
2. FeLV (usu.) |
|
|
What are some Ddx for myeloDYSplasia when HYPERcellular marrow & cytopenia?
|
・Recovering stage of marrow damage (Parvo)
・Imun-medi dz w/ destruction of mature precursors ・Consump of nO due to OVERWHELMING inflam dz |
|
|
1. What do we assume is the pathogenesis of Acute Myeloid Leukemia (AML)?
2. What are the 3 classifications of Acute Myeloid Leukemia (AML) for people? |
1. Genetic abnormality that affects cellular proliferation & maturation.
2. ・AML w/ Myelodysplasia-related changes ・Therapy-related AML (sequela of therapeut agents) ・AML not categorized |
|
|
1. What are the different morphological classifications of Acute Myeloid Leukemias?
2. How can we differentiate cell lines? |
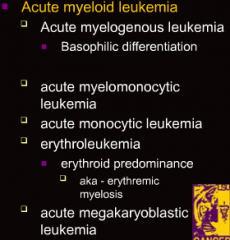
1.
・*Acute Granulocytic Leukemia* (Myeloblastic leukemia w/ differentiation OR Myeloblastic leukemia with neutrophilic differentiation)) ・*Acute Myelomonocytic Leukemia* (Combination of myeloblasts and monoblasts) ・*Acute Monocytic Leukemia* (Monocytic leukemia without differentiation OR Monocytic leukemia with differentiation) ・*Acute Erythroid Leukemia* (Combination of myeloblasts and rubriblasts) ・*Acute Megakaryoblastic Leukemia* 2. By immunophenotyping |
|
Classify leukemia (BM has 20%/> blasts):
・Cannot be classified based on morphology/cytochemistry ・Has features of both erythroid & myeloid leukemias |
Undifferentiated leukemia
|
|
Classify leukemia (BM has 20%/> blasts):
・Very poorly differentiated myelomonocytic leukemia. ・Cannot be differentiated based on morphology from lymphoid leukemia |
Undifferentiated leukemia
|
|
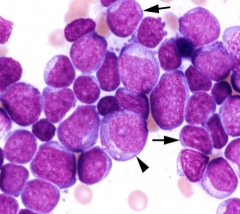
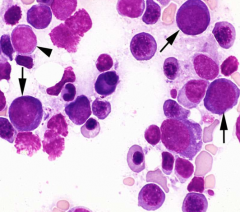
Classify leukemia (BM has 20%/> blasts):
>90% Blasts in BM <10% more differentiated granulocyte precursors Type I Myeloblasts (Arrows) Type II Myeloblasts (Arrowhead) |
Acute Granulocytic Leukemia
(Myeloblastic leukemia with differentiation) |
|
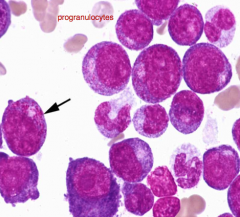
Classify leukemia (BM has 20%/> blasts):
<90% Blasts in BM >10% more differentiated granulocytes Many promyelocytes |
Acute Granulocytic Leukemia
(Myeloblastic leukemia with neutrophilic differentiation) |
|
Classify leukemia (BM has 20%/> blasts):
Cells in mitosis (arrowhead) |
If we see granules, then granulocytic leukemia
|
|
|
What can appear similar to granulocytic leukemia?
|
Immune-mediated neutropenia (mature precursors destroyed)
|
|
CBC: WRI (Not anemic)
WBC: 43% NCC: 3,000 Neut: 1,000 Lymphs: 2,000 Platelets: 53,000 |
Remember Leukemia crowds out all normal cells → anemia
This is immune-mediated neutropenia Interpretation: Granulocytic hyperplasia with disorderly maturation |
|
Classify leukemia (BM has 20%/> blasts):
>20% myeloblasts & monoblasts in BM >20% monocytes & granulocytes Monoblasts (arrows) Progranulocytes (arrowhead) |
Acute Myelomonocytic Leukemia
(Combination of myeloblasts and monoblasts) |
|
|
Classify leukemia (BM has 20%/> blasts):
>80% Promonocytes & monoblasts -------------------------------------------------------------------- 20%-80% Promonocytes & monoblasts |
Monocytic leukemia
(Monocytic leukemia without differentiation) (Monocytic leukemia with differentiation) |
|
Classify leukemia (BM has 20%/> blasts):
>50% Erythroid OR if most blasts are erythroid <20% Myeloblasts & monoblasts |
Erythroleukemia
(Combination of myeloblasts and rubriblasts) |
|
|
Erythroleukemia is most commonly seen in cats with ___.
|
FeLV (combination of RBC & nO leukemia)
|
|
|
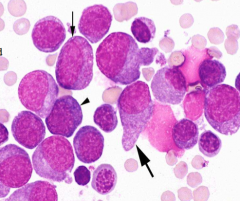
Classify leukemia (BM has 20%/> blasts):
>20% megakaryoblasts and also in blood |
Megakaryoblastic leukemia
|

