![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
66 Cards in this Set
- Front
- Back
|
Causes of Arrhythmias |
-ion channel dysfunctions (electrolyte imbalance) -acute ischemia -myocardial infart -CHF -hyperthyroidism -sympathetic stimulation -myocardial scarring -Drugs (digoxin, anti-arrhythmics, caffeine) |
|
|
________ is the dominant pacemaker that sets the "sinus rhythm" for synchronized contraction of the atria & ventricle. The _________ slows down the impulse to allow enough time for the atria to contract & relax before the ventricle contracts |
SA node = pacemaker
AV delay= allows atria to empty into ventricle before ventricular contraction |
|
|
The heart rate reflects ___________________ |
sinus node automacity |
|
|
______ wave = atrial depolarization
______ wave = ventricular depolarization
______ wave = ventricular repolarization |
P wave = atrial depolarization
QRS wave = ventricular depolarization = conduction time in the ventricle
T wave = ventricular repolarization |
|
|
______ interval = how long AP takes to be conducted from atria to ventricle (via AV node & bundle of His)
______ interval = how long AP takes to go through ventricle & start repolarization (varies w/ HR, faster HR= shorter interval) |
PR interval = AV nodal conduction time (diff btwn P & R wave)
QT interval = ventricular AP duration (diff btwn T & QRS wave) |
|
|
Normal PR interval |
0.12 - 0.20 seconds |
|
|
what is occurring during the different phases of AP in the Ventricular, atrial, & purkinje myocytes? |

phase 0= rapid Na+ influx (depolarization) phase 1= transient outward K (partial repolarization) phase 2= slow Ca2+ influx (plateau) phase 3= K+ efflux (repolarization) phase 4= K+ current determines resting potential |
|
|
What is occurring during the different phases of the AP in SA & AV nodes? |
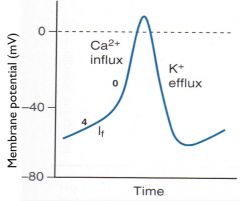
phase 4= slow influx of Na+ (funny current)(depolarization) phase 0= inward Ca2+ (AP upstroke) phase 3= K+ efflux (repolarization) |
|
|
slowing down phases 4 (blocking Na+ channels) or 0 (blocking Ca+ channels) and prolonging phase 3 (blocking K channels) can increase the ___________ |
AV delay (thus elongate the refractory period) |
|
|
When is the absolute refractive period (NO AP can be stimulated)? |
from phase 0--> phase 2 |
|
|
When is the relative refractive period (requires a higher stimuli to be initiated)? |
during the first 1/3 of phase 3
(during the rest of phase 3 = supranormal RP= smaller than normal stimuli can stimulate AP) |
|
|
Causes of tachyarrythmias |
-eptopic impulses: impulse NOT from SA node, messes up the regular sinus rhythm
-reentry phenomenon: wave of depolarization travels in endless circle (small or large loop) & causes excitation |
|
|
How can reentry phenomenon be interrupted? |
1. impair conduction (Na+ blocker) 2. prolong refractory period (K+ blocker) 3. decrease sympathetics (beta blockers) 4. inc AV node refractory if involved (beta blockers, Ca+ blocker, adenosine, digoxin) |
|
|
___________ is caused by reentry over a large circuit. -rapid regular atrial activity (180-350 bpm) -many of the impulses however are not conducted to ventricle due to AV delay (ventricular rate not as high)
Tx? |
atrial flutter
Tx: by slowing conduction through AV node |
|
|
________ is caused by multiple "wandering" reentrant circuits w/i atria. -chaotic rhythm w/ very fast atrial rate (350-600 bpm) -high ventricular rate (140-160 bpm) -disorganized contraction promotes pooling of blood in atrium--> possible thrombus & stroke
Tx? |
atrial fibrillation
Tx: slow AV conduction + anticoagulant (prevents thrombo-embolism) |
|
|
________ is caused by reentrant circuits that directly involve the AV node.
These patients should be rapidly treated w IV adenosine (impairs AV conduction) -also give IV Ca or beta blockers
|
AV nodal reentrant tachycardia (AVNRT) |
|
|
_______ is caused by an accessory pathway that allows impulses to go directly from the atrium to the ventricle, bypassing the AV node
Use caution in treating this patients -use sodium channel blockers to prolong the refractory period of accessory pathway |
Wolf- Parkinson White syndrome (AVRT) |
|
|
Some anti-arrhythmic drugs can cause "Torsades de Pointes" and increase the likelihood of an arrhythmia. How? |
*prolongation of the QT segment
-often due to cardiac K+ blockers
|
|
|
Vaughn-Williams classification of antiarrhythmics (based on the MAIN fxn) |
class I= sodium channel blockers class II= beta-blockers class III= potassium channel blockers (prolong AP) class IV= calcium channel blockers |
|
|
Effects of diff classes on PR, QRS, & QT |
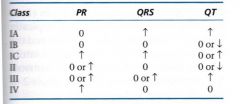
(incr in AV delay = inc PR= inc (prolong) refractory period & inc in QT= decr HR) |
|
|
class 1 (sodium channel blocker) subtypes |
IA= moderate block (dec phase 0 upstroke rate, prolong AP duration)
IB= mild block (slight dec phase 0, shorten Ap duration, detach from receptors fastest)
IC= marked block (greatly dec phase 0 upstroke, no change in AP duration) |
|
|
How do Class 1 drugs changes the AP in pacemaker cells (SA etc) |
decreased automacity
(via inc threshold & dec phase 4 slope) |
|
|
Class IA drugs
(prolong AP repolarization) |
Quinidine Procainamide disopyramide |
|
|
Which drug? -class IA -anticholinergic properties (usually combine w/ beta-blocker) -alpha-adrenergic blockade -reduces clearance of digoxin -oral |
Quinidine |
|
|
can cause; -nasuea, diarrhea -cinchonism (tinnitus, vertigo, and headaches) -thrombocytopenic purpura -dizziness & fainting -hypotension -QT interval prolongation (contraindicated in long QT sydrome |
Quinidine
(quindine syncope = dizziness & fainting due to prolonged QT interval & ventricular arrhthmias--> torsades) |
|
|
What drug? -class IA -does NOT prolong AP duration -IV & IM -renal excretion, adjust dosage in renal pts |
Procainamide |
|
|
can cause; -fever, rash arthralgias *(Antiarrhthmic with SLE side effects) -hypotension (less likely) -CNS effects (depression, hallucination, psychosis) |
Procainamide |
|
|
What drug? -class IA -used for ventricular arrhythmias (that are refractory to quindine or procanamide) -anti-muscarinic (can worsen heart block & sinus node activity) |
Disopyramide |
|
|
can cause; -dry mouth, blurred vision, constipation, urine retention (anti-muscarinic) -prolongs QT interval (contraindicated in long QT syndrome)--> Torsades |
Disopyramide |
|
|
How to tx class IA overdose |
-fix hyperkalemia -sodium lactate IV (inc Na current by inc ionic gradient & alkalinizing tissue to dec receptor binding) -sympathomimetics to reverse hypotension |
|
|
Class IB Drugs (shorten AP duration) |
Lidocaine Mexilitine
|
|
|
Class IB MOA |
-preferntially block Na+ channels in ischemic tissue -shortens phase 3 repolarization (& AP duration) -good for tx ectopic impulses -dissociate from channels quickly (less likely to interfere w/ normal impulses) |
|
|
What drug? -class IB (preference to ischemic tissues) -suppress ventricular arrhythmias in hospitalized pts (IV use only) -DOC to reverse/terminate digitalis induced arrhythmias (digoxin OD)
|
Lidocaine |
|
|
What drug? -class IB (targets ischemic sodium channels) -chronic tx of ventricular arrhythmias assoc w/ previous MI (give orally) -combined use w/ beta-blockers -some CNS side effects |
Mexilitine |
|
|
Class IC (sodium channel blocker) Drugs |
Flecainide |
|
|
Class IC MOA |
-slows phase 0 & conduction velocity in atria, ventricles, & purkinje -slows phase 4 in AV node (makes refractory) -blocks conduction through bypass/acessory tract (AVRT) |
|
|
What drug? -reserved for refractory ventricular tachycardias that tend to progress to ventricular failure (supraventricular arrhythmias) -VERY proarrhythmic (BAD) -CNS disturbances (dizziness, blurred vision, headache, nausea -Negative ionotropic effect, aggravates CHF (contraindication!) |
Felcainide
(class IC antiarrhythmic) |
|
|
Class II (beta-blockers) anti-arrhythmic drugs |
Esmolol Propanolol Acebutalol Metroprolol
(lols) |
|
|
Class II MOA |
-dec phase 4 slope= dec automacity -prolong repolarization of AV node= dec reentry -inc refractory of AV & impair conduction--> slow ventricular rate in atrial flutter & fibrillation
=BLOCK sympathetic overactivation--> suppress tachyarrhythmias
|
|
|
first line tx to suppress arrythmias in pts w previous MI |
class II beta blockers (lols)
*shown to reduce mortality & have protective effects after MI |
|
|
Which drug? -class II -DOC for acute arrhythmias (control ventricle in response to atrial fibrillation or flutter due to surgery) -very short acting -IV admin |
Esmolol |
|
|
class II/propanol (beta-blocker) side effects: |
-bradycardia -bronchospasm -depression -fatigue
*use w/ caution in asthma or diabetic pts (block hypoglycemic symptoms) |
|
|
Beta blockers (class II) should NEVER be used in someone w/ ____________________ |
2nd & 3rd degree AV block
*or in combo w calcium channel blockers |
|
|
Class III (K channel blocker) drugs |
-Amiodarone -sotolol
|
|
|
Class III K channel blocker MOA |
ventricular AP: -inc refractory period & dec conduction velocity --> dec reentry -dec rate of firing (phase 4 slope)--> dec automacity |
|
|
What drug? -class III (has weak class I, II, & IV actions) -1st DOC in emergency ventricular arrhymthmias during cardiac resuscitation -used for a wide spectrum of ventricular & supraventricular arrhythmias -highly lipophilic (can take month + to get out of system) -excreted via bilary, lacrimal, skin -usually given orally |
Amiodarone |
|
|
What drug? SE include; thyroid abnormalities, rashes, smurfism, pulmonary fibrosis (irreversible), GI, elevated LFTS
*do not combine w other drugs that prolong QT intervals (causes some prolongation) |
Amiodarone |
|
|
What drug? -class III (K channel blocker) -also non selective beta-blocker (via L-isomer) -may prolong QT--> Torsades (not common) -renal excretion, may adjust in renal pts -side effects: dyspnea & dizziness |
Sotalol |
|
|
Class IV (Ca channel blockers) Drugs: |
Verpamil Diltiazem |
|
|
Class IV MOA: |
-targets L-type Ca channels in pacemaker tissue (APs depend on Ca) -slows AV node conduction (prolongs phase 0) -slows depolarization (prolongs phase 4)--> *inc PR interval *dec contractility, slows HR *slows transmission of rapid atrial impulses to ventricles *dec AV nodal reentery |
|
|
Clinical use of class IV (ca blocker) |
-AV nodal reentry arrhythmias -atrial fibrillation -atrial flutter
|
|
|
Contraindications for class IV (Ca blockers) |
-do NOT use w/ beta blockers -dec contractility--> do NOT use during MI or in failing heartst--> cause AV block |
|
|
Misc. Drug
DOC for Acute Supraventricular tachycardia (AVNRT) Given IV bolus Acts in seconds (can give second dose w/o dangerous side effects)
side effects due to vasodilation--> facial flushing |
Adeonsine |
|
|
Adenosine: MOA |
-agonist at Ai adenosine receptors (on pacemaker cells) -activates receptor --> opens K+ channel--> hyperpolarization = decr automaticity & --> inhibits Adenylate cyclase--> dec pacemaker funny currents & Ca currents = decr automaticity & dec AV node conduction |
|
|
Misc. Drug
Used to treat; Rapid artial fibrillation, ventricular tachycardia SE; Green Yellow halos |
Digoxin |
|
|
Digoxin/ Digitalis: MOA |
inhibition of Na/K ATPase pump--> inc intracellular Na levels--> dec Ca efflux via Na/Ca exchanger--> inc Ca in the SR--> hypersensitivity to next AP--> inc force of contraction = inc CO, inc vagal tone (due to vagal brainstem stimulation), & decr sympathetic
|
|
|
Digoxin/Digitalis side effects |
-sets up for sponataneous depolarization--> ectopic beats ventricular tachycardia |
|
|
Commonly used drugs to treat Atrial Flutter? |
Propanolol (all beta-blockers) (II) Verapamil (IV)
(Digoxin less common alternative) |
|
|
Commonly used drugs to treat Atrial Fibrillation? |
Propanolol (all beta blockers) (II) *DOC Amiodarone (III) |
|
|
Commonly used drugs to treat AV Nodal Reentry?
|
Propanolol (beta-blockers) (II) Verapamil (IV)
(digoxin alternative) |
|
|
Commonly used drugs to treate Acute Supraventricular tachycardia? |
Adenosine * DOC
(verpamil (III) alternatively can be used) |
|
|
Commonly used drugs to treat Acute Ventricular Tachycardia? |
Lidocaine (I) Amiodarone (III) |
|
|
Commonly used drugs to treat ventricular fibrillation? |
Amiodarone Epinephrine
(lidocaine alternatively) |
|
|
What three drugs can increase plasma digoxin levels leading to toxicity?
|
Quinidine, Verapamil, Amiodarone |
|
|
Digoxin toxicity causes an arrhthmia? How do you treat? |
LIDOCAINE |
|
|
Digoxin toxicity causes an AV block, how do you treat? |
ATROPINE |

