![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
72 Cards in this Set
- Front
- Back
|
Pre-eclamptic woman, BP 170/110, headache, proteinuria 1.2g. Which of the following NOT to use for control of her hypertension:
A. Magnesium B. SNP C. GTN D. Hydralazine E. Metoprolol |
A
ANCZA SIG – “Safe agents include methyldopa, labetalol, nifedipine and some β-adrenoceptor blockers (METOPROLOL, pindolol, propranolol). Atenolol is not recommended due to fetal growth restriction. Angiotensin converting enzyme inhibitors (ACE-I) and angiotensin type II receptor blockers are contraindicated (Abalos et al 2006, Level I; Podymow & August 2008, Level IV; Rowe 2008, Level IV)” SNP and GTN not ideal, but can be used for acute hypertension control |
|
|
Male with a Haemoglobin of 8G% and reticulocyte count 10%. Possible diagnosis:
A. Untreated pernicious anaemia B. Aplastic anaemia C. Acute leukaemia D. Anaemia of chronic disease E. Hereditary spherocytosis |
E
Wiki - Spherocytosis: “A cause hemolytic anemia characterized by the production of red blood cells (RBCs), or erythrocytes, that are sphere-shaped, rather than bi-concave disk shaped. Spherocytes are found in hereditary spherocytosis and autoimmune hemolytic anemia” |
|
|
Commonest organism causing meningitis post spinal:
A. Staph epidermidis B. Staph salivarius C. Staph aureus D. Strep pneumoniae |
B
Baer E. Post-dural puncture bacterial meningitis. Anesthesiology 2006;105: 381--93 “Potential sources of bacterial introduction into the intrathecal space during spinal procedures include intrinsic or extrinsic contamination of needles, syringes, or injected medications; inadequately decontaminated patient skin; inadequately cleaned health-care provider hands; a contaminated sterile field; and droplet transmission from the health-care provider's upper airway. S. salivarius and other viridans group streptococci, which are normal mouth flora, are the most commonly identified etiologies of meningitis after spinal procedures, accounting for 49% and 60% of cases in two literature reviews (2,6). Droplet transmission of oral flora has been suggested as the most likely route of transmission in reports of clusters associated with a single health-care provider” |
|
|
Exponential decline / definition of time constant (with various options)
A. time for exponential process to reach log(e) of its initial value B. Time until exponential process reaches zero C. Time to reach 37% of initial value D. Time to reach half if its initial value E. 69% of half life |
C
Time constant is the time taken for the amount of something to fall to 1/e of the initial amount The number "e" equals 2.718281828. 1/e = 0.368. Therefore the time constant is the time it takes for the concentration/amount to fall to 36.8% of the initial value (approx 37%) |
|
|
Relative humidity – air fully saturated at 20 %. What is the relative humidity at 37 degrees ?
A. 20 B. 30 C. 40 D. 50 E. 60% |
C
"1m3 of air at 20˚C, 100% saturated, contains about 17g of water. If it is warmed to 37˚C, the mass of water vapour or absolute humidity is still the same but the relative humidity is only 39%, as at 37˚C, 1m3 of air contains 44g of water vapour when fully saturated and the ratio of 17 to 44 gives a value of 39%." |
|
|
A 50 year old man with multiple fractures. The BEST parameter to monitor volume resuscitation is:
A. Heart rate B. LVEDV C. PCWP D. RVEDV E. Changes in R atrial pressure during inspiration |
E
LVEDV is the closest correlate to preload However, this artcile Echocardiographically Derived Parameters of Fluid Responsiveness suggests that dynamic measures are superior (like RAP change in inspiration)” "We are learning that static parameters of cardiac preload, such as right atrial pressure (RAP), PAOP, RVEDV, and LVED area (LVEDA) are inferior to dynamic parameters. The dynamic parameters [eg, inspiratory decrease in RAP(DRAP), expiratory decrease in arterial systolic pressure (Ddown), respiratory changes in pulse pressure (DPP), respiratory changes in aortic blood velocity (Dpeak)] have been shown to predict fluid responsiveness better than the static parameters. The aortic flow variation6 and superior vena cava (SVC) collapsibility are 2 echocardiographically derived parameters that have been found to be excellent predictors of volume responsiveness." |
|
|
Anaphylaxis to rocuronium. Which is most likely to cause coss-reactivity ?
A. Vecuronium B. Pancuronium C. Atracurium D. Cisatracurium E. None of the above -cross reactivity too variable to predict |
E
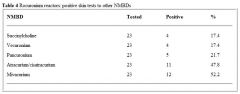
From Allergy 2007; 62: 471-487 Review Article: Anaphylaxis during anaesthesia:diagnostic approach "Cross Reactivity between NMBA is said to be common because of ubiquitous ammonium groups in these drugs. The estimated prevalence of cross-reactivity between NMBA is about 65% by skin tests and 80% by radioimmuno assay inhibition tests. While some pairings are common, the patterns of cross-reactivity vary considerably between patients." However another article on the wiki has this table, suggesting both atrac and cisatrac have the highest of these options |
|
|
Hypotension post propofol induction in elderly patient. More pronounced / profound than in younger patient. Reason ?
A. Concentric LVH associated with ageing and therefore preload dependent B. Because of increased lean body mass C. Decreased cardiac output with ageing D. Increased sensiticity to all anaesthetic agents, thus relative overdose is common E. Decreased liver blood flow with ageing, decrease drug clearance and increased drug concentration |
A
A = ? True. The reduction in preload is the main contributor to hypotension according to Fundamentals of Anaesthesia, p576 B = False. Reduced C = False. The statement is true, but this is not the main mechanism of hypotension D = ? False. A true statement in terms of loss of consciousness, but not necesscarily the cause of hypotension E = ? False. For the same reasons as D |
|
|
Predictive factors for mortality in elderly patient (except):
A. Aortic stenosis B. Diabetes mellitus C. Elevated Creatinine D. Cognitive dysfunction E. Type of surgery |
D
Cognitive dysfunction is the only one not mentioned in this article: Jin F. Chung F. Minimizing perioperative adverse events in the elderly. Br. J. Anaesth. 2001;87(4):608-624 |
|
|
The best clinical indicator of SEVERE AS
A. Presence of thrill B. Mean Gradient 30mmHg C. Area 1.2 cm2 D. Slow rising pulse and ESM radiating to carotids E. Shortness of breath |
A
International Anaesthesiology Clinics 2005; 43(4); 21-31 According to Talley & O’conner thrill is a sign of severity “Symptoms of AS include syncope, angina, and dyspnea (SAD). Presence of any of these symptoms leads to a life expectancy of less than 5 years and 20% chance of sudden death. Of the 35% of patients with AS presenting with angina, half will die within 5 years unless the aortic valve is replaced. Fifteen percent of patients with AS present with syncope, half of which will die within 3 years. Fifty percent of patients with AS will present with dyspnea, and half will die within 2 years unless the valve is replaced” |
|
|
Elderly patient. Indications for pre Femoro-Popliteal Bypass angiogram include all EXCEPT:
A. Severe heart failure B. Suspicion of L main disease C. Symptomatic tachyarrhythmia D. Unstable angina E. Stable angina with positive thallium |
C
A is an Active Cardiac Conditions for Which the Patient Should Undergo Evaluation and Treatment Before Noncardiac Surgery B, C and E all seem appropriate reasons to do an angiogram and seem to be covered by AHA guidelines on indications for pre-op revascularisation: 7.1. Preoperative Coronary Revascularization With CABG or Percutaneous Coronary Intervention CLASS I 1. Coronary revascularization before noncardiac surgery is useful in patients with stable angina who have significant left main coro- nary artery stenosis. (Level of Evidence: A) 2. Coronary revascularization before noncardiac surgery is useful in patients with stable angina who have 3-vessel disease. (Survival benefit is greater when LVEF is less than 0.50.) (Level of Evidence: A) 3. Coronary revascularization before noncardiac surgery is useful in patients with stable angina who have 2-vessel disease with signifi- cant proximal LAD stenosis and either EF less than 0.50 or demon- strable ischemia on noninvasive testing. (Level of Evidence: A) 4. Coronary revascularization before noncardiac surgery is recom- mended for patients with high-risk unstable angina or non–ST- segment elevation MI.§ (Level of Evidence: A) 5. Coronary revascularization before noncardiac surgery is recom- mended in patients with acute ST-elevation MI. (Level of Evidence: A) CLASS IIa 1. In patients in whom coronary revascularization with PCI is appro- priate for mitigation of cardiac symptoms and who need elective noncardiac surgery in the subsequent 12 months, a strategy of balloon angioplasty or bare-metal stent placement followed by 4 to 6 weeks of dual-antiplatelet therapy is probably indicated. (Level of Evidence: B) In patients who have received drug-eluting coronary stents and who must undergo urgent surgical procedures that mandate the discontinuation of thienopyridine therapy, it is reasonable to continue aspirin if at all possible and restart the thienopyridine as soon as possible. (Level of Evidence: C) |
|
|
How do you minimise risk of intravenous cannulation with epidural insertion ?
A. Injection saline through epidural needle before catheter insertion B. Lie patient lateral C. Do CSE D. Thread catheter slowly E. |
A
|
|
|
Timing of peak respiratory depression post intrathecal 300 mcg morphine:
A. < 3.5 hours (think it was one hour) B. 3.5 – 7.5 hours (then three hours) C. 7 - 12.5 hours (then 7.5 - 12.5 hrs) D. 12.5 -18 hours E. > 18 hours |
B
"Respiratory depression occurs in up to 1.2% to 7.6% of patients (Meylan et al, 2009 Level I) given intrathecal morphine. When measured in opioid-naive volunteers, respiratory depression peaked at 3.5 to 7.5 hours following intrathecal morphine at 200 to 600 mcg doses (Bailey et al, 1993 Level IV). Volunteers given 600 mcg had significant depression of the ventilatory response to carbon dioxide up to 19.5 hours later” |
|
|
Patient with aortic dissection. Blood pressure 150/90. Best drug to control BP:
A. Captopril B. Esmolol C. GTN D. Hydralazine E. SNP |
B
eMedicine: • Aggressive management of heart rate and blood pressure should be initiated. • Beta-blockers should be given initially to reduce the rate of change of blood pressure (dP/dt) and the shear forces on the aortic wall. • The target heart rate should be 60-80 beats per minute. • The target systolic blood pressure should be 100-120 mm Hg. |
|
|
Type of dissection – which is classically for NON-operative management:
A. DeBakey Type I B. DeBakey Type II C. Stanford A D. Stanford B E. Stanford C |
D
The Stanford classification divides dissections into 2 types, type A and type B. • Type A involves the ascending aorta (DeBakey types I and II); type B does not (DeBakey type III). • This system also helps delineate treatment. Usually, type A dissections require surgery, while type B dissections may be managed medically under most conditions. The DeBakey classification divides dissections into 3 types. • Type I involves the ascending aorta, aortic arch, and descending aorta. • Type II is confined to the ascending aorta. • Type III is confined to the descending aorta distal to the left subclavian artery. o Type III dissections are further divided into IIIa and IIIb. o Type IIIa refers to dissections that originate distal to the left subclavian artery but extend both proximally and distally, mostly above the diaphragm. o Type IIIb refers to dissections that originate distal to the left subclavian artery, extend only distally and may extend below the diaphragm. |
|
|
TURP – patient under spinal. Confused. ABG: Na+ 117 / normal gas exchange. Treatment ?
A. 10 ml 20% Saline as fast push IV B. 3% NS 100 ml/h C. Normal saline 200 ml/h D. Frusemide 40 mg IV E. Fluid restrict 500 ml/day |
B
|
|
|
Male undergoing trans-sphenoidal surgery. Now Na+ 155mmol/l and thirsty with polydypsia. Treatment:
A. Desmopressin (DDAVP) B. Fluid restrict C. Aldosterone D. E. |
A
|
|
|
The STRONGEST stimulus for ADH secretion:
A. High serum osmolality B. Low serum osmolality C. Hypovolaemia D. High serum Na E. |
C
Osmoreceptor control is very sensitive, responding to 1-2% changes in plasma osmolality. If hypovolaemia is present, this will 'over-ride' osmoreceptor control. Thus it is commonly said that volume is maintained at the expense of osmolality, or equivalently, that hypovolaemia will result in an increase in ADH level despite the inhibitory effect of hypo-osmolality |
|
|
Stellate ganglion block. Needle entry next to SCM muscle at C6. Which direction to advance needle ?
A. C3 B. C4 C. C5 D. C6 E. C7 |
D
|
|
|
Thermoneutral zone in 1 month old infant ?
A. 26 – 28 degrees Celcius B. 28 – 30 degrees Celcius C. 30 – 32 degrees Celcius D. 32 – 34 degrees Celcius E. 34-46 degrees celcius |
D
|
|
|
A 60 year old man describes orthopnoea. On examination: pansystolic murmur (at LSE)/ displaced apex beat. Likely diagnosis ?
A. Mitral regurgitation B. ? C. D. E. |
A
|
|
|
A 4 year old child with VSD (repaired when 2 years old) for dental surgery. What antibiotic prophylaxis do the guidelines recommend?
A. Amoxycillyn orally B. Amoxycillin IV C. Cephazolin IV D. Amoxycillin / gentamicin E. No antibiotics required |
E
|
|
|
A 4 year old child with Arthrogrophysis multiplex congenita for dental surgery. Jaw rigidity post induction. Likely cause ?
A. Temporomandibular joint involvement/ TMJ rigidity B. Inadequate depth of anaesthesia C. Inadequate muscle relaxation/ inadequate sux D. Masseter spasm E. ? |
A
Unclear from these options ?A given it involves are joints Sounds like they are difficult arirways secondary to micrognathia Arthrogryposis multiplex congenita refers to a variety of conditions that involve congenital limitation of joint movement. Intelligence is relatively normal except when the arthrogryposis is caused by a disorder or syndrome that also affects intelligence. There are two major types of arthrogryposis multiplex congenita (AMC): • Amyoplasia (classic arthrogryposis): Multiple symmetric contractures occur in the limbs. • Distal arthrogryposis: The hands and feet are involved, but the large joints are spared. Etiology Any condition that impairs in utero movement for > 3 wk can result in AMC. Causes may involve • Physical limitation of movement (eg, due to uterine malformations, multiple gestations, oligohydramnios) • Maternal disorders (eg, multiple sclerosis, impaired uterine vascularity) • Fetal disorders (eg, neuropathies; myopathies, including muscular dystrophies; connective tissue abnormalities; impaired fetal vascularity; anterior horn cell disease) More than 35 specific genetic disorders (eg, spinal muscular atrophy type I, trisomy 18) have been linked to AMC. Symptoms and Signs Deformities are prominent at birth. AMC is not progressive; however, the condition that causes it (eg, muscular dystrophy) may be. Affected joints are contracted in flexion or extension. In classic AMC, shoulders are sloped, adducted, and internally rotated; the elbows are extended; and the wrists and digits are flexed. Hips may be dislocated and are usually slightly flexed. Knees are extended; feet are often in the equinovarus position. Leg muscles are usually hypoplastic, and limbs tend to be tubular and featureless. Soft-tissue webbing sometimes occurs over ventral aspects of the flexed joints. The spine may be scoliotic. Except for slenderness of the long bones, the skeleton appears normal on x-rays. Physical disabilities may be severe. As noted, some children may have primary CNS dysfunction, but intelligence is usually unimpaired. Endotracheal intubation during surgery may be difficult because children have small immobile jaws. Other abnormalities that rarely accompany arthrogryposis include microcephaly, cleft palate, cryptorchidism, and cardiac and urinary tract abnormalities. |
|
|
A 78 year old man with past difficult intubation for arm surgery. Supraclavicular block with 25 mls 0.5% bupivacaine. Shortly after begins convulsing. INITIAL management?
A. Midazolam 5mg B. Intralipid 20% 1.5 ml/kg C. Thiopentone 150mg D. Suxamethonium 50mg E. Propofol 50mg |
A
Local Anesthetic Systemic Toxicity 2010 Regional Anesthesia and Pain Medicine: March/April 2010 - 35(2):152-193 "If seizures occur, they should be rapidly controlled to prevent injury to the patient and acidosis. The Panel recommends that benzodiazepines are the ideal drugs to treat seizures because they have limited potential for cardiac depression. In the absence of readily available benzodiazepine, propofol or thiopental are acceptable alternatives; however, their potential for worsening existing hypotension or cardiac depression requires using the lowest effective dose.” |
|
|
Advantages of bronchial blockers over double lumen tubes:
A. Able to achieve lobar isolation B. Lower cuff pressure C. Quicker deflation of isolated lung D. Pneumonectomy E. Lower incidence of malposition |
A
Bronchial Blockers • ADVANTAGES o Easy recognition of anatomy if the tip of a single lumen tube is above carina o Best device for pt with difficult airway o No cuff damage during intubation o No need to replace ETT if post-op ventilation required o Selective lobar isolation is possible (mentioned at end of article, not in table) • DISADVANTAGES o Small channel for suctioning o Conversion from 1- to 2- then to 1-lung ventilation (problematic for novice) o High maintenance device (dislodgement or seal loss during surgery) Double-Lumen ETT's • ADVANTAGES o Large lumen facilitates suctioning o Best device for absolute lung separation o Conversion from 2 to 1-lung ventilation easy and reliable • DISADVANTAGES o Difficulty selecting proper size o Difficult to place during laryngoscopy o Damage to tracheal cuff o Major tracheo-bronchial injuries |
|
|
Patient for pneumonectomy. Pre op FEV1 2.4. (Predicted 4.5L) FVC given as well. For R lower lobectomy. Postoperative predicted FEV1 ?
A. 1.3 B. 1.5 C. 1.7 D. 1.9 E. 2.2 |
C
19 lung segments in total - 10 on the right (RUL=3, RML=2, RLL=5), and 9 on the left (LUL=3, Lingula=2, LLL=4). Therefore for a right lower lobectomy we will be removing 5 segments, and therefore be left with 14 segments. The ppoFEV1 will be 14/19 x 2.4L = 0.7368 x 2.4L = 1.77L Or, based on the numbers used in Miller there are 42 segments in total: 22 segments (or subsegments) in the right lung (RUL=6, RML=4, RLL=12), and 20 in the left lung (LUL=10, LLL=10). The calculation is the same, but with different numbers: A right lower lobectomy will remove 12 segments, and we will be left with 30. Therefore ppoFEV1 will be 30/42 x 2.4L = 0.7143 x 2.4L = 1.71L |
|
|
Post accidental dural puncture with epidural needle. Headache. Which does NOT fit ?
A. Epidural blood patch 30-50% effective B. Unlikely to be related to epidural if purely occipital headache C. Caffeine mildly effective in reducing headache D. Subdural haematoma can rarely occur with PDPH E. (?something about photophobia) |
A
• A - Epidural blood patch is about 60-70% effective (long-term, higher initially) according to most articles, so I say A=false. • B - Post-dural puncture headache can be frontal, fronto-temporal, or occipital. The BJA CEACCP article from 2001 states that "The headache does not occur in any specific distribution within the cranium". Therefore B=false. • C - Caffeine does have some initial benefit in reducing headache, but this does not seem to be prolonged (see article by Ghaleb). C=True. • D - Subdural haematoma is a rare complication of accidental dural puncture following epidural (see articles from Int J Obstet Anesth and Anaesthesia & Intensive Care). D=True . |
|
|
Cell saver. Which does NOT get filtered ?
A. Foetal cells B. Free Hb C. Platelets D. Clotting factors E. Microaggregates of leukocytes |
A
Cell salvage filters the following substances: • Free haemoglobin • White blood cells • Plasma • Platelets • Heparin • Clotting factors • Complement Foetal cells (particularly fetal RBC's) are NOT filtered/removed, and are spun down with maternal RBC's (ie the process does not differentiate between maternal and fetal RBCs) and then reinfused into the mother. However, the risk of alloimmunisation is thought to be no greater than that occurring during a normal vaginal delivery. The risk of amniotic fluid embolism is also thought to be very low - so much so that cell salvage in obstetrics has been endorsed by the Obstetric Anaesthetists Association, AAGBI, NICE and CEMACH in the UK, as well as the ASA in America. |
|
|
You are on a humanitarian aid mission in the developing world. Drawover vaporiser apparatus described being used. Given 400 mm tubing, OMV or diamedica vaporiser, 200mm tubing attached to self-inflating bag. Which other ONE piece of equipment is ESSENTIAL to make this system functional?
A. Halothane B. In-line Waters' Cannister [1] C. Non-rebreathing valve D. Oxygen source E. Ventilator |
C
The keyword here is "functional". You don't need volatile agent for the circuit to be functional and there are other ways of providing anaesthesia even in 3rd world countries. I was going to go with oxygen, however it also says "self-inflating bag" which means fresh gas flow is not required and flow of gas in the circuit would be promoted by the self inflation of the bag provided there is a unidirectional flow valve on it. The Waters' Canister is a CO2 absorbing canister and is not required for functionality, nor is a ventilator if the anaesthetist has arms and legs to squeeze the bag with. The answer must be C - non-rebreathing valve |
|
|
Regarding post craniotomy pain:
A. Local infiltration proven to reduce long-term pain B. Local more painful than discrete nerve blocks C. Local infiltration more efficacious than discrete nerve blocks D. Local infiltration more efficacious than opioid analgesia E. Local infiltration more efficacious with clonidine included |
A & B
From APMSE book: • "Local infiltration "...reduces incidence of subsequent chronic pain." (Level 2) - so option A is correct. • Nerve blocks are less painful than discrete blocks so option B is correct. • Local infiltration not more efficacious, so incorrect • No difference in anlagesia between scalp infiltration and morphine or fentanyl • There is also a comment in that section in the book that: "Clonidine did not improve analgesia after supratentorial craniotomy", so option E is wrong |
|
|
A 60 year old female is undergoing hysterectomy. Gabapentin reduces postoperative:
A. Nausea B. Vomiting C. Sedation D. Pruritus E. Constipation |
A
Vomiting and pruritis also, but nausea specifically with hysterectomy From APMSE: • Peri-op gabpentinoids reduce the incidence of vomiting, pruritis and urinary retention, but increase the risk of sedation • After hysterectomy and spinal surgery specifically, gabapentin improved pain relief and was opioid sparing, nausea was less in patient with hysterectomy, and there was no difference in sedation |
|
|
Burns dressings. The following is proven to be of analgesic benefit:
A. Morphine gel B. Biosynthetic dressings (the answer per pain book) C. Dexmedetomidine IV D. Lignocaine IV E. Cognitive/Distraction technique |
B & E
Though only B is level 1 evidence According to APMSE: • The use of biosynthetic dressings is associated with a decrease in time to healing and a reduction in pain during burn dressings changes (N) (Level I [Cochrane Review]). • Opioids, particularly via PCA, are effective in burn pain, including procedural pain (S) (Level II). • Augmented reality techniques (N) (Level II), virtual reality or distraction techniques (N) (Level III-3) reduce pain during burn dressings. • Gabapentin reduces pain and opioid consumption following acute burn injury (N) (Level III-3) • PCA with ketamine and midazolam mixture provides effective analgesia and sedation for burn dressings (N) (Level IV). |
|
|
Subtenon’s block. What is the worst position to insert block?
A. Inferonasal B. Inferotemporal C. Superonasal D. Supertemporal E. Medial / canthal |
C
A sub-Tenon's block can be done in any of the 4 quadrants (options A-D above). However: Continuing Education in Anaesthesia, Critical Care & Pain | Volume 5 Number 3 2005 "There is individual variation in the disposition of blood vessels, but they congregate in the apex of the orbit. There is a view that the inferotemporal and medial parts of the orbit are relatively poorly supplied with blood vessels, whereas the superonasal region is relatively vascular." |
|
|
Liposuction. Infiltration of lignocaine with 1:200,000 adrenaline. Peak plasma concentration of lignocaine occurs at:
A. 1 hour B. 3 hours C. 18 hours D. 24 hours E. 30 mins |
C
Different values quoted:: • 5-17 hours postoperatively – sPlasma lidocaine levels and risks after liposuction with tumescent anaesthesia. Acta Anaesthesiol Scand. 2005 Nov;49(10):1487-90 • 11-15 hours postoperatively – eMedicine |
|
|
Child-Pugh score. Components ?
A. Bilirubin / albumen / INR (yes INR, not PT), ascites, encephalopathy B. Various other options including AST/ALT, GGT, PT C. ? D. ? E. ? |
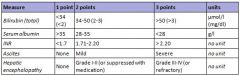
A
The score employs five clinical measures of liver disease. Each measure is scored 1-3, with 3 indicating most severe derangement |
|
|
Which is NOT a disadvantage of drawover vaporiser versus plenum vaporiser:
A. Temperature compensation B. Cannot use sevoflurane C. Small volume reservoir D. Flow compensation E. |
B
All are disadvantages, presuming A is talking about its lack of compensation. Though seems it function ok if temp >1 to <50 degrees Drawover vaporisers are • "simple to assemble and use, and can operate without fresh gas supplies. They are lightweight and portable" • Not well compensated for temperature (ok between 1-50 degrees) • very difficult to use with sevoflurane - "Sevoflurane (Sevorane) has been used in draw-over, but its use is hampered by a need to deliver high percentages which are at the upper limits of simple vaporiser performance capabilities...using additional wicks to maximise output can be helpful, but latent heat of vaporisation rapidly cools the system and lowers performance...two OMV vaporisers are required to provide adequate concentrations for induction” • equipped with a small volume reservoir • variable with regards to flow compensation Advantages: • Simplicity of concept and assembly • No need for pressurised gas supply regulators and flow meters • Minimum FiO2 is 18-21% • Robust reliable and easily serviced • Low cost • Portable Disadvantages: • Decreasing familiarity with technique/equipment • Vaporiser limitations • Filling systems not agent specific (can be an advantage) • Basic temperature compensation affecting performance at extremes (>1 to <50 degrees they maintain their accuracy) • Less easy to observe spontaneous ventilation with self inflating bag • Cumbersome in paediatric use |
|
|
Acute renal failure. Which is not an indication for dialysis ?
A. Hyperkalaemia B. Metabolic alkalosis C. Hypernatraemia D. Uraemic pericarditis E. APO |
B
CEACCP article: Indications for continuous renal replacement therapy Classical: Volume overload Metabolic acidosis (pH < 7.1) Hyperkalaemia (>6.5 mmol litre�1) Symptomatic uraemia (Pericarditis, encephalopathy, bleeding dyscrasia) Dialysable intoxications (e.g. lithium, ethylene glycol, methanol, aspirin, theophylline, vancomycin, procainamide) Hyperthermia (cooling) Alternative: Endotoxic shock Hypothermia (rewarming) SIRS (pancreatitis, ARDS) Nutritional support Hepatic failure Deliberate hypothermia Severe dysnatraemia (<115 mmol litre-1, >165 mmol litre-1) Traumatic rhabdomyolysis Plasmapheresis (Guillain–Barre syndrome, myasthenia gravis, thrombotic thrombocytopaenic purpura) |
|
|
Chronic alcohol use. Which is not an associated complication?
A. AF B. hypertriglyceridemia C. Macrocytosis D. Nephrotic syndrome E. Pancreatic Ca |
D
CEACCP Article - Alcohol and Anaesthesia Volume 9 Number 1 2009 CNS: Wernicke–Korsakoff syndrome, Peripheral neuropathy, Autonomic dysfunction Metabolic: Hyperlipidaemia, Obesity, Hypoglycaemia, Hypokalaemia, Hypomagnesaemia, Hyperuricaemia, Osteoporosis CVS: Cardiomyopathy, Heart failure, Hypertension, Arrhythmias (e.g. AF, SVT, VT) Haematological: Macrocytosis Thrombocytopenia, Leucopoenia GI: Alcoholic liver disease, Pancreatitis, Gastritis, Oesophageal and bowel carcinoma Musculoskeletal: Myopathy,Osteomalacia |
|
|
Chest xray shown of patient post Left pneumonectomy with heart swung to left side. Management:
A. Increase PEEP B. Roll onto right side C. Turn on suction to left pleural catheter D. Lung biopsy E. |
B
Cardiac herniation following completion pneumonectomy for bronchiectasis. Annals of Cardiac Anesthesia. Sep 2010 “(in cardiac herniation)...Three conservative measures to improve the cardio-respiratory function before patient transfer to the operation suite include repositioning the patient with nonsurgical side down, avoiding hyperinflation of the remaining lung and injecting 1-2 liters of air into the surgical hemithorax. [10] Definitive treatment and prevention of recurrence require open surgery to reduce the hernia and repair the pericardial defect by prosthetic patch or autologous graft like fascia lata.” |
|
|
Salicylate poisoning:
A. Respiratory acidosis B. Metabolic acidosis (/ don’t think this was an option - ak )(yep i think it was- mm) C. Increased CO2 (production) D. High output renal failure E. Hyperthermia (/ pretty sure this option was HYPOthermia - too late) |
B
The toxic effects of salicylates are complex. • Respiratory centers are directly stimulated, causing a primary respiratory alkalosis. • Salicylates also cause an inhibition of the citric acid cycle and an uncoupling of oxidative phosphorylation and may produce renal insufficiency that causes accumulation of phosphoric and sulfuric acids. • The metabolism of fatty acids is likewise increased in patients with salicylate toxicity, generating ketone body formation. These processes all contribute to the development of an elevated anion-gap metabolic acidosis in patients with salicylate poisoning. This combination of a primary respiratory alkalosis and a primary metabolic acidosis is characteristic of salicylate poisoning, especially in adults, and should make the clinician suspect the diagnosis when it is present. Catabolism occurs secondary to the inhibition of adenosine triphosphate (ATP) ̶ dependent reactions with the following results: • Increased oxygen consumption • Increased carbon dioxide production • Accelerated activity of the glycolytic and lipolytic pathways • Depletion of hepatic glycogen • Hyperpyrexia Adult patients with acute poisoning usually present with a mixed respiratory alkalosis and metabolic acidosis |
|
|
New onset atrial fibrillation in a 10 week pregnant lady. BP 150/90, HR 160, SaO2 92%. Moderate mitral stenosis on TTE, no thrombus seen. Emergency doctor gave her anticoagulant (not specified what). Most appropriate management:
A. Verapamil B. Labetalol 20mg iv to 300mg C. Amiodarone 300mg IV D. Synchronised biphasic cardioversion with 70-100 Joule E. Oral digoxin -1000mcg then 500mcg 6 hrs later |
D
|
|
|
Patient post anterior cervical fusion. Patient in recovery. Confused and combative. Nurse concerned about haematoma Taken to theatre: Most appropriate way of securing airway:
A. Gas induction / laryngoscopy / intubate B. Awake tracheostomy C. Awake fibreoptic intubation using minimal sedation D. Thiopentone, suxamethonium, direct laryngoscopy and intubation E. retrograde intubation |
A
Awake fibreoptic would be safe, but probably impossible in an awake patient Awake tracheostomy seems extreme, and would presumably also be difficult I think A is a safer option than D, though could potentially be difficult in the combative patient |
|
|
Young asthmatic male in emergency department. RR 26, pCO2 27, SAO2 92%, struggling talking in sentences. Given nebulised salbutamol, and ipratropium, 200mg IV hydrocortisone. After 30 minutes - no improvement. Further management:
A. IV salbutamol B. IV aminophylline C. IV magnesium D. Intubate and ventilate E. ? |
C
From discussion on wiki: • Seems IV salbutamol reserved for when nebs no longer tolerated • Aminophyline can be used, although according to the Global initiative for Asthma, pocket guide updated 2010, isn’t recommended in addition to high dose beta-agonits • Magnesium 2g over 20min appears to be quoted in multiple sources including OHA and positive results in a cochrane review • I imagine you want to avoid intubating the asthmatic patient until absolutely necessary |
|
|
Called to emergency department to review a 20 y/o male punched in throat at a party. Some haemoptysis / hoarse / soft voice. Next step in management:
A. CT to rule out thyroid cartilage fracture B. XR to rule out fractured hyoid C. Rapid sequence induction / laryngoscopy / intubation D. Awake fibreoptic intubation E. Nasendoscopy by ENT in emergency department |
A
Bronchoscopy appears to be the gold standard in diagnosing neck trauma (can probably include nasendoscopy as a form of upper airway bronchoscopy). However the below article includes CT prior to bronchsocopy in its algorithm for stable blunt neck trauma Perioperative management of laryngotracheobronchial injury: our experience in a level 1 trauma centre. European Journal of Trauma and Emergency Surgery Sep2012 “Bronchoscopy is the most reliable method to diagnose, locate and determine the severity of Tracheobronchial injury” Evaluation and Management of Neck Trauma. Emerg Med Clin N Am 25 (2007) 679–694 “Stable patients who have suspected airway injury should be evaluated with a combination of careful physical examination, plain films, CT, and bronchoscopy, depending on the institutional approach. Although threedimensional (3D) reconstructive CT is extremely good at identifying and locating tracheal injuries, bronchoscopy must still be considered the gold standard test” However, “CT scanning is the initial imaging modality of choice in the hemodynamically stable patient and is used to guide selective operative management” |
|
|
How quickly does the CO2 rise in the apnoeic patient?
A. 1 mmHg per min B. 2 mmHg per min C. 3 mmHg per min D. 4 mmHg per min E. 5 or ?8 mmHg per min |
C
From Miller, 1st minute Co2 increases by 6 mm Hg all subsequent minutes 3 -4 mm Hg |
|
|
Long-standing T6 paraplegia. All present EXCEPT ?
A. Flaccid paralysis B. Poikilothermia C. Autonomic hypereflexia D. Labile BP E. Hyperkalaemia with suxamethonium |
A
|
|
|
Young female patient for tonsillectomy with history of bleeding tendency. Which is the most likely cause?
A. Factor V Leiden B. Protein C deficiency C. Haemophilia B (Christmas disease) D. Antithrombin III deficiency E. Lupus anticoagulant |
C
• Factor V Leiden confers resistance to breakdown by protein C & S system. It results in hypercoagulability, and is therefore the wrong answer. • Protein C deficiency results in reduced FV & VIII breakdown and hypercoagulability, and is therefore the wrong answer. • Haemophilia B, is X-linked but the phenotype in females is variable. It does cause increased bleeding. And is the answer to choose. • ATIII deficiency is associated with a hypercoagulable state, and is the wrong answer. • Lupus anticoagulant, causes in vitro prolongation of the APTT but in vivo, results in hypercoagulability, and is the wrong answer |
|
|
Amniotic fluid embolism. Cause of death in first half hour ?
A. Pulmonary hypertension B. Malignant arrhythmia C. Pulmonary oedema D. Hypovolaemic shock E. |
A
|
|
|
Hypocalcaemia – earliest sign:
A. Tingling of face and hands B. Chvostek’s sign C. Carpopedal spasm D. E. |
A
Wikipedia page on hypocalcaemia says this is the earliest sign |
|
|
Elderly COAD patient. On home oxygen. 24 hours of worsening condition. Various blood gases given:
A. paO2 > 50, paCO2 70 HCO3 30 etc… B. C. D. E. |
A
|
|
|
Visual loss with pupillary reflexes retained. Likely cause ?
A. Retinal detachment B. Occipital mass C. Frontal mass D. Chiasmal mass E. Optic neuritis |
B
Cortical blindess = visual loss but with retained pupillary reflexes and normal fundoscopy. Caused by pathology in the occipital lobes |
|
|
Nerve block for anaesthesia over anterior 2/3 of ear?
A. C2 B. Mandibular nerve C. Maxillary nerve D. Ophthalmic nerve E. Vagus |

B
Not sure exactly what part of the ear this is referring to, however… Four sensory nerves supply the external ear: 1. greater auricular nerve (C2 branch) 2. lesser occipital nerve, (C2 branch) 3. auricular branch of the vagus nerve, and 4. auriculotemporal nerve (branch of mandibular nerve) |
|
|
Complex regional pain syndrome. What proportion of patients have motor involvement ?
A. 0 % B. 25 % C. 50 % D. 75 % E. 95 % |
D
From Blue Book 2005 (Australasian Anaesthesia) - Complex Regional Pain Syndrome: Motor / trophic changes - motor dysfunction 57-98% - weakness 75-95% - limited range of movement 80-88% - incoordination 47% - tremor 48% - spasm 13% - dystonia 14% - myoclonus 4-20% |
|
|
Malignant hyperthermia. The number of people in the community at any given time with a predisposition is called the:
A. Prevalence B. Incidence C. D. E. |
A
Incidence measures the rate of occurrence of new cases of a disease or condition. Prevalence measures how much of some disease or condition there is in a population at a particular point in time |
|
|
Patient with Hx COAD and suspected pneumonia – clinical findings supporting R pneumonia on examination:
A. R Dull percussion note & increased vocal resonance B. R Dull percussion note & decreased vocal resonance C. R Decreased air entry D. Tracheal deviation to left E. Tracheal deviation to right |
A
|
|
|
Thallium scan:
A. High negative predictive value B. High positive predictive value C. Not as good as a dobutamine stress echocardiography D. E. |
A
From the 2007 AHA guidelines, 'because of a very high sensitivity of abnormal stress nuclear imaging studies for detecting patients at risk for perioperative cardiac events, the negative predictive value of a normal scan has remained uniformly high at approximately 99% for MI or cardiac death' |
|
|
A 50 y/o male diabetic admitted to intensive care with pneumonia. Intubated and ventilated. Extensive results given. BP 80/-, HR 120, CVP 4, PCWP 6, SvO2 69% PaO2 80, BE -4 pH 7.2. Management:
A. Blood transfusion B. Bicarbonate infusion C. Fluid resuscitation D. Adrenaline infusion E. Insulin infusion |
C
Haemodynamic variables suggest hypovolaemia |
|
|
Young female having cholecystectomy. Venous air embolus:
A. Mechanical ventilation and PEEP is part of treatment strategy B. Most likley to occur at initial gas insufflation, but can occur at any time C. Inert gas (argon, xenon) is safer D. E. |
B
Miller 7th ed. p. 2188 "This complication develops principally during the induction of pneumoperitoneum, particularly in patients with previous abdominal surgery." |
|
|
LUSCS for failure to progress. Spinal is inserted uneventfully. Next day the patient has foot drop. The most likely cause is?
A. epidural haematoma B. lumbosacral palsy C. sciatic nerve palsy D. common peroneal palsy E. |
B
|
|
|
Severe pre-eclampsia. WORST treatment option:
A. Magnesium B. Nifedipine C. Metoprolol D. SNP E. |
D
|
|
|
In pregnancy the dural sac ends at:
A. T12 B. L2 C. L4 D. S2 E. S4 |
D
BJA 1995 75: 6-8 Anatomical configuration of the spinal column in the supine position. Confirms in both pregnant and non pregnant it ends at S2 |
|
|
Septic elderly man. Given lots of obs but essentially mixed venous oxygen sat 65%, lactate 4, MAP low. Mx.
A transfuse B fluid bolus C Noradrenaline |
B
|
|
|
Another pregnant woman with ?MS. Develops SVT. Try vagal manouveres without success.
A. Adenosine B. ? C. ? |
A
|
|
|
Pregnant woman presents with narrow complex tachycardia HR 190, stable BP 100/60. No response to vagal manoevures. Management?
A. Adenosine 6mg B. DCR C. Amiodarone D. Atenolol E. ? |
A
|
|
|
Which gives the BEST seal?
A LMA classic B Proseal C Intubating LMA D. ? E. ? |
B
From the LMA website / product information: • LMA Classic - Seal pressure up to 20cm H20 • LMA Supreme™ - measured oropharyngeal leak pressures up to 37 cm H2O • LMA Flexible™ - oropharyngeal seal pressures up to 20 cm H2O • LMA Fastrach - Seal pressures up to 20 cm H2O • LMA ProSeal™ - leak pressures up to 32 cm H2O |
|
|
The MAIN indication for biventricular pacing is
A. complete heart block B. congestive cardiac failure C. VF D. E. |
B
|
|
|
What's the area burnt in the following man? Half of left upper arm, all of left leg and anterior abdomen.
A. 27% B. 32% C. 42% D. |
A
|
|
|
The intercostobrachial nerve:
A. Arises from T2 trunk B. Is usually blocked in brachial plexus block C. Supplies antecubital fossa D. can be damaged by torniquet E. Arises from inferior trunk |
D
|
|
|
IV paracetamol:
A. late plasma levels around the same as oral B. highly protein bound C. ?30%? renally excreted D. VD 10L/kg E. |
A
True. “plasma concentrations of intravenous propacetamol were significantly higher and obtained earlier, compared to oral administration, however after the first hour and up to 24 hours the plasma concentrations remained similar” MIMS False. It is not extensively protein bound. False. 90% excreted in 24 hours. False. VD 1L/kg |
|
|
Patient with diastolic dysfunction. Is it caused by:
A. Restrictive cardiomyopathy B. Dilated cardiomyopathy C. D. E. |
A
|
|
|
Management of rhabdomyolysis – best option?
A. Haemodialysis B. Bicarbonate C. Frusemide D. IV fluids E. |
D
|
|
|
The average expected depth of insertion of an oral endotracheal tube, from the lip, in a normal newborn infant is
A. 7.5 cm B. 8.5 cm C. 9.5 cm D. 10.5 cm E. 11.5 cm |
C
Paediatric advanced life support: Australian Resuscitation Council Guidelines 2006) in a newborn is 9.5 cm, 11.5 cm for a 6 months old infant 12 cm for a 1 year old. Thereafter, the approximate depth of oral insertion is given by the formula: age (years)/2 + 12cm. Neonates: Weight in Kg + 6. So 3.5Kg = 9.5cm at lips |

