![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
89 Cards in this Set
- Front
- Back
|
Atheroma vs Xanthoma
|
Atheroma = plaques in BV walls
Xanthomas = Plaques or nodules of lipid-laden histiocytes in skin, esp. eyelids |
|
|
Arteriosclerosis vs Atherosclerosis
|
Arteriosclerosis: hyaline thickening of small aa. in essential HTN or DM; "onion skinning" in malignant HTN
Atherosclerosis: fibrous plaques and atheromas in intima of aa |
|
|
Describe the pathologic progression of atherosclerosis. Begin with endothelial cell dysfunction.
|
Endothelial cell dysfunction-->mac and LDL accumuln
-->foam cell formation -->Fatty streaks -->SM cell migration (PDGF and TGF-beta involved) -->fibrous plaque -->atheroma |
|
|
Most common site of atherosclerosis.
|
Abdominal aorta
Followed by coronary artery, followed by popliteal, followed by carotid artery |
|
|
Statins:
Drug Class Effect AEs |
HMG-CoA reductase inhibitors
Lower LDL; inhibit cholesterol precursor, mevalonate AE: Hepatotox (inc'd LFTs), rhabdomyolysis (muscle breakdown) |
|
|
Niacin:
MOA Effect AE |
MOA: inhibit lipolysis in adipose tissue; reduced hepatic VLDL secretion into circulation
Inc HDL (and dec LDL) AE: Flushing |
|
|
Bile acid resins:
Prefix MOA Effect |
Begin with cholest or coles
Dec'd LDL Malabsorption of fat (and fat-soluble vits) |
|
|
Ezetimibe:
MOA Effect |
Prevents cholesterol reabsorption at small intestine brush border
Lowers LDL, esp. when used with statin |
|
|
Fibrates:
Suffix Effect |
-fibrate or -fibrozil
Dec TGs |
|
|
Which lipid-lowering agent:
SE: facial flushing |
Niacin
|
|
|
Which lipid-lowering agent:
elevated LFTs, myositis |
Fibrates, statins
|
|
|
Which lipid-lowering agent:
SE: GI discomfort, bad taste |
Bile acid resins
|
|
|
Which lipid-lowering agent:
best effect on HDL |
Niacin
|
|
|
Which lipid-lowering agent:
best effect on TGs/VLDL |
Fibrates
|
|
|
Which lipid-lowering agent:
best effect on LDL/cholesterol |
Statins
|
|
|
Which lipid-lowering agent:
binds C. diff toxin |
Cholestyramine
|
|
|
A 50-year old man starts lipid-lowering medication.
On first dose, he develops a rash, pruritis, and diarrhea. What drug is he taking? |
Niacin--prevent flush with aspirin
|
|
|
What is the MOA of cardiac glycosides (digoxin)?
|
Inhibit Na/K ATPase-->dec'd extracell Na-->inc'd intracell Ca-->inc'd contractility
|
|
|
What is aortic dissection?
Presentation? Risk factors |
Longitudinal intraluminal tear forming false lumen
Assocd w/HTN or Marfan's Presents w/tearing chest pain radiating to back CXR w/mediastinal widening CAN RUPTURE AND RESULT IN DEATH :( |
|

|
aortic dissection
|
|

|
aortic dissection
|
|
|
Treatment of aortic dissection.
|
Beta-blocker--inc'd BP will cause greater tearing of aorta
|
|
|
When does angina become symptomatic?
Stable vs Unstable |
CAD narrowing >75%
Stable = predictable; know you'll get angina while walking upstairs Unstable: comes on unpredictably |
|
|
An abdominal aortic aneurysm is most likely a consequence of what process?
|
HTN
|
|
|
What are the 5 deadly causes of acute chest pain?
|
-Aortic dissection
-Unstable angina -MI -Tension pneumothorax -PE |
|
|
What is the likely cause of chest pain:
ST segment elevation only during brief episodes of chest pain |
Prinzmetal's angina
|
|
|
What is the likely cause of chest pain:
Patient is able to point to localize chest pain using one finger |
M/S chest pain (pulled muscle)
|
|
|
What is the likely cause of chest pain:
Chest wall tenderness on palpation |
M/S chest pain (pulled muscle)
|
|
|
What is the likely cause of chest pain:
Rapid onset sharp chest pain that radiates to scapula |
Aortic dissection
|
|
|
What is the likely cause of chest pain:
Rapid onset sharp pain in 20 year-old and associated with dyspnea |
Spontaneous pneumothorax (lung collapses)
|
|
|
What is the likely cause of chest pain:
Occurs after heavy meals, improved with antacids |
GERD or esophageal spasm
|
|
|
What is the likely cause of chest pain:
Acute onset dyspnea, tachycardia, confusion in hospitalized patient |
PE
|
|
|
What is the likely cause of chest pain:
Pain began day following an intensive new exercise program |
M/S Pain
|
|
|
What is the likely cause of chest pain:
Sharp pain lasting hours-days, somewhat relieved by sitting forward |
Pericarditis
|
|
|
What is the likely cause of chest pain:
Pain made worse by deep breathing and/or motion |
M/S Pain
|
|
|
What is the likely cause of chest pain:
Chest pain in dermatomal distribution |
Shingles (Zoster)
|
|
|
What is the likely cause of chest pain:
Most common cause of non-cardiac chest pain |
GERD
|
|
|
Drug classes used to treat angina.
Effects of each. |
Nitrates (dec'd preload): dec'd myocardial oxygen demand
beta-blockers (dec'd afterload): dec'd myocardial oxygen demand Nitrates and beta-blockers: Super dec'd myocardial oxygen demand |
|
|
Most commonly occluded coronary artery.
|
LAD--anterior wall MI
|
|
|
Describe evolution of MI (chronologically):
Gross vs Histo Risks associated |
First day:
Gross: dark mottling; pale with terazolium stain Histo: contraction bands after 12-24 hours (early coagulative necrosis); release of contents of necrotic cells, beginning of nphil emigration 2-4 days: Gross: hyperemia (dilated vessels) Histo: tissue surrounding infarct shows inflammn; dilated vessels (hyperemia), nphil emgration 5-10 days: Gross: Hyperemic border; YELLOW-BROWN softening--maximally yellow and soft by 10 days Histo: RISK FOR FREE WALL RUPTURE, tamponade, papillary muscle rupture, intraventricular septal septal rupture 7 weeks: Gross: recanalized artery, gray-white zone of previous infarct Histo: contracted scar complete; risk of ventricular aneurysms |
|
|
A patient with poorly managed HTN has acute, sharp substernal pain that radiates to the back and progresses over a few hours.
Death occurs shortly thereafter. Diagnosis? |
Aortic dissection
|
|
|
Describe EKG changes seen in evolution of MI.
|
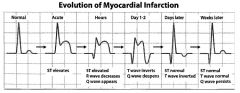
|
|
|
Describe diagnosis of MI.
|
ECG is gold standard.
Cardiac troponin I rises after 4 hours; elevated for 7-10 days CK-MB predominantly found in myocardium, but can also be released from skeletal muscle; useful in diagnosing reinfarction AST nonspecific and found in cardiac, liver, and skeletal muscle cells |
|
|
Transmural infarct vs Subendocardial infarct:
General EKG findings |
Transmural: due to inc'd necrosis; affects entire wall, ST elevation on EKG, Q waves
Subendocardial infarct: ischemic necrosis <50% of ventricle wall; due to fewer collaterals, higher pressure; ST DEPRESSION on EKG |
|
|
Severe mitral regurgitation days following MI
|
Papillary mm rupture
|
|
|
Infarct of LAD:
EKG leads? |
Q waves in leads V1-V4, V5
|
|
|
Infarct of Left Circumflex:
EKG leads? |
Q waves in leads aVL, V5, V6
|
|
|
Infarct of Right Coronary--Inferior wall:
EKG leads? |
II, III, aVF
|
|
|
Infarct of Right Coronary--Posterior wall:
EKG leads? |
R precordial EKG: V4
|
|
|
Thrombolytics:
Examples MOA Use Antidote |
Streptokinase, urokinase, tPA
Directly or indirectly aid conversion of plasminogen to plasmin, cleaves thrombin and fibrin clots (inc'd PT, inc'd PTT; no change in PLT count) Use: Early MI, early ischemic stroke Antidote: Aminocaproic acid |
|
|
Clopidogrel:
MOA Effects |
Both inhibit platelet aggregation by irreversibly blocking ADP receptors
|
|
|
Abciximab:
MOA |
MAB that bind GpIIb/IIIa on activated PLTs, prevent agg
|
|
|
Dilated cardiomyopathy:
Causes Concentric or Eccentric? Diastolic or systolic dysfunction? |
Alcohol abuse
wet BeriBeri-Thiamine deficiency (B1; 2 i's look like 1) Coxsackie B virus Chronic Cocaine, Chagas' Doxorubicin (ABCD) ECCENTRIC (sarcomeres added in series) SYSTOLIC dysfn NOTE: ECCENTRIC MEANS NO MUSCLE THICKENING, VENTRICLE IS DILATED |
|
|
Hypertrophic cardiomyopathy:
Causes Concentric or Eccentric? Diastolic or systolic dysfunction? |
Familial
Friedreich's Ataxia Cause of sudden death in young athletes Concentric hypertrophy (sarcomeres added in parallel)--proximity of hypertrophied IV septum to mitral leaflet obstructs outflow tract (systolic murmur) Diastolic dysfn NOTE: CONCENTRIC MEANS MUSCLE OF VENTRICLE IS THICKENED |
|
|
Restrictive cardiomyopathy:
Causes Diastolic or systolic dysfunction? |
Sarcoidosis
Amyloidosis Postradiation fibrosis Endocardial fibroelastosis Hemochromatosis Diastolic dysfn |
|
|
Dec'd LV contractility:
Causes Effects Treatment |
Causes: MI, chronic HTN
Effects: Low cardiac output-->Inc'd renin-->Inc'd systemic venous pressure-->peripheral edema -->inc'd symp activity-->inc'd contractility and cardiac output Tx: Digoxin |
|
|
Left-sided heart failure:
Symptoms |
Pulmonary congestion
Dyspnea on exertion Orthopnea (shortness of breath when supine) |
|
|
Right-sided heart failure:
Symptoms |
Hepatomegaly (nutmeg liver)
Ankle, sacral edema JVD |
|
|
Digoxin:
MOA AE Antidote |
Direct inihbition of Na/K ATPase activity leading to indirect inhibition of Na/Ca exchanger/antiport-->positive inotropy (stimulates vagus nerve)
AE: Cholinergic--n/v/d, blurry yellow vision***(think Van Gogh) Hypokalemia--worsened by renal failure Antidote: Slowly normalize K+, Lidocaine, pacemaker, anti-dig Fab fragments, Mg2+ |
|
|
During a high school football game, a young athlete collapses and dies immediately.
What type of cardiac disease did he have? |
Hypertrophic CM
|
|
|
Antidote:
Acetaminophen |
N-acetylcysteine
|
|
|
Antidote:
Salicylates |
NaHCO3 (trap with basic urine)
|
|
|
Antidote:
Amphetamine |
NH4Cl (acidify urine)
|
|
|
Antidote:
AChE-inhibitors Organophosphates |
Atropine, pralidoxime
|
|
|
Antidote:
Antimuscarinic, anticholinergic agnets |
-stigmine
|
|
|
Antidote:
Beta-blockers |
Glucagon
|
|
|
Antidote:
Digitalis |
Stop dig
Normalize K+ Lidocaine Anti-dig Fab frags Mg2+ |
|
|
Antidote:
Fe |
Deforxamine
|
|
|
Antidote:
Pb |
CaEDTA
|
|
|
Antidote:
Mercury, arsenic, cold |
Dimercaprol (BAL); Dime is a monetary unit, as is gold
|
|
|
Antidote:
Copper, arsenic, golc |
Penicillamine--Copper comes from PENnies
|
|
|
Antidote:
Cyanide |
Nitrite
Thiosulfate Hydroxocobalamin |
|
|
Antidote:
Methemoglobin |
METhylene blue
Vit C |
|
|
Antidote:
CO |
100% O2, hyperbaric O2
|
|
|
Antidote:
Methanol, ethylene glycol |
Ethanol
Dialysis Fomepizole*** (inhibits alcohol dehydrogenase) |
|
|
Antidote:
Opioids |
Naloxone/maltrexone
|
|
|
Antidote:
Benzodiazepenes |
Flumazenil
|
|
|
Antidote:
TCAs |
NaHCO3 (plasma alkalinization)
|
|
|
Antidote:
Heparin |
Protamine
|
|
|
Antidote:
tPA, streptokinase |
Aminocaproic acid
|
|
|
Antidote:
Theophylline |
beta-blocker
|
|
|
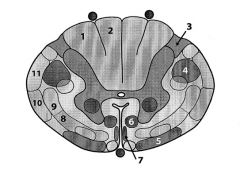
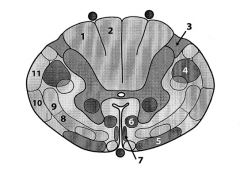
1. fasciculus cuneatus (Dorsal column)--from arms
2. fasciculus gracilis (Dorsal column)--from legs 3. Lissauer's tract--info from spinothalamic tract; pain and temp info ascends here and crosses at anterior commissure 4. Lateral corticospinal (voluntary motor info to body) 5. Vestibulospinal tract 6. Reticulospinal tract 7. Anterior/ventral spinal tract (voluntary motor command) 8. Anterior spinothalamic tract 9. Lateral spinothalamic tract (pain, temp sensation) 10. Anterior spinocerebellum tract 11. Posterior cerebellar tract (proprioception) |
|
|
Which spinal tract conveys:
Touch, vibration, and pressure sensation |
Dorsal column (affected by syphilis)
|
|
|
Which spinal tract conveys:
Voluntary motor command from motor cortex to body |
Corticospinal tracts
|
|
|
Which spinal tract conveys:
Voluntary motor command form motor cortex to head/neck |
Corticobulbar tract
|
|
|
Which spinal tract conveys:
Alternate routes for mediation of voluntary movement |
Reticulo- and rubrospinal tracts
|
|
|
Which spinal tract conveys:
Pain and temperature sensation |
Lateral spinothalamic tract
|
|
|
Which spinal tract conveys:
Important for postural adjustments and head movements |
Vestibulospinal tract
|
|
|
Which spinal tract conveys:
Proprioceptive information for cerebellum |
Dorsal and ventral spinocerebellar tracts
|

