![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
111 Cards in this Set
- Front
- Back
|
What percentage of SCIs are nontraumatic and what are possible causes? |
10%. most likely to occur in individuals with narrowing spinal canals 1. disc prolapse 2. vascular insult 3. neoplasm 4. RA 5. radiation 6. Spinal stenosis 7. surgery 8. cardiac arrest 9. aortic aneurysm 10. infection |
|
|
Where in the cervical spine are SCIs most likely and what is the MOI? |
C5 and C7 most often injured traumatically -flexion -vertical loading -extension with rotation or lateral flexion
|
|
|
Where in the Thoracic spine are SCIs most likely? And what is the MOI? |
-less likely to be injured from trauma due to rib cage and higher stability as compared to cervical region -T12-L1 most common site -flexion or vertical compression -> wedge compression or burst fractures of vertebral bodies damaging the SC
|
|
|
Where are lumbar spine SCIs most likely? and MOI? |
-most at L1 or L2 -below L1 and L2 the cauda equina is less likely to sustain a complete injury -neurological damage from trauma is usu incomplete due to large vertebral canal and relatively good vascular supply |
|
|
What, in general, is damage to the SC due to? |
1. physical impingement on the cord or 2. interruption of the cord's vascular supply -actual transection of the cord is rare |
|
|
What are the pathological changes with SCI? |
1. blunt trauma = primary destruction of neurons at the level of injury 2. most of damage from secondary sequelae of the initial trauma, which begins a process of progressive tissue destruction within the cord 3. tissue damage may travel up and down cord 1-3 segments 4. necrotic tissue is gradually reabsorbed and replaced by scar tissue |
|
|
what are the mechanisms of secondary tissue destruction in SCI? |
1. ischemia 2. edema 3. demyelination and destruction
|
|
|
How does ischemia cause secondary tissue destruction in SCI? |
-decr blood flow to traumatized are of SC due to 1. chemical in the body that cause vasoconstriction or thromboses 2. metabolic disturbances or 3. elevated pressure due to edema |
|
|
how does edema cause secondary tissue destruction in SCI? |
-disruption of cell membranes results in abnormal concentrations of sodium and potassium in the extracellular tissue -ion imbalance causes increased osmotic pressure in damaged area and creates excessive edema |
|
|
How does demyelination and destruction contribute to secondary tissue destruction in SCI? |
-when cells of Sc are traumatized, Ca+ ions accumulate in injured cells -abnormal [Ca+] disrupts functioning and causes demyelination and destruction of the cell membrane and axonal cytoskeleton -necrosis of axons progresses to scar tissue formation |
|
|
What is spinal shock? |
-temporary phenomenon that occurs after trauma to Sc in which SC ceases to function below the lesion -Spinal reflexes, voluntary motor control, sensory function, and autonomic control are absent below level of lesion -usually resolves within 24 hours of injury with the return of anal and bulbocavernosus reflexes -sparing of sensation or voluntary motor function below the lesion indicates that the lesion is incomplete |
|
|
How are SCI named? |
named according to the level of neurological injury and classified as complete or incomplete |
|
|
What is paraplegia? |
only lower extremities are involved, resulting in weakness (paraparesis) or paralysis
|
|
|
what is tetraplegia? |
all 4 extremities are involved =quadriplegia or quadriparesis (weakness) |
|
|
How is the spinal level designated for SCI? |
1. determine most caudal level with intact sensation for right and left side 2. determine most caudal level with motor level of 3+/5 3. determine the single neurological level - most cephalad of sensory and motor levels determined in steps 1 & 2 4. Determien whether injury is complete or incomplete and determine ASIA level |
|
|
How do you determine whether SCI is complete or incomplete? |
-incomplete: SC is not totally disrupted at the level of injury -preservation of some sensory or motor function more than 3 segments below the lesion -ascending and descending tracts are undamaged and resulting function is called sparing |
|
|
What is ASIA A? |
ASIA A = complete = no sensory or motor function is preserved in the sacral segments S4-S5 ( no voluntary anal contraction , no S4-S5 sensation and deep anal pressure = no) |
|
|
What is ASIA B? |
-sensory incomplete, motor complete -sensory but not motor function preserved below neurological level and includes LT at S4-S5 or deep anal pressure -no motor function preserved more than 3 levels below motor level on either side of body |
|
|
What is ASIA C? |
Sensory incomplete, motor incomplete -motor function preserved below the neurological level & >half of key mm functions below the single neurological level have a mm grade < 3 (MMT 0-2)
|
|
|
What is ASIA D? |
Motor incomplete, sensory incomplete -motor function preserved below neurological level & > or equal to half of key mm functions below neurological level of injury have a grade > or = to 3 |
|
|
What is ASIA E? |
normal -sensation and motor function graded as normal in all segments in pt who had prior deficits -if initial testing shows no deficits, the individual is neurologically intact and an ASIA score does not apply |
|
|
What is Brown-Sequard syndrome? |
hemisection of spinal cord (usu gunshot wounds or stab) -ipsilat side has 1. motor paralysis or weakness 2. loss of proprioception 3. loss of 2-point discrimination and vibration 4. decr reflexes 5. clonus 6. spasticity Contralat side: 1. loss of Pain and temp starting few levels below lesion |
|
|
What is Anterior Cord syndrome |
-results from trauma to anterior cord or damage of anterior spinal artery usually related to flexion injuries of cervical region -bilat loss of motor function and pain and temp below the level of the lesion |
|
|
What is Central Cord syndrome? |
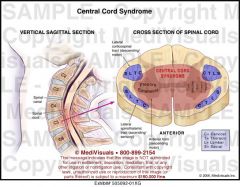
-MOI = hyperextension injuries with minor trauma to cervical region -results in damage to central aspect of SC affecting UE sensation and motor functioning with normal LE functioning |
|
|
What is posterior cord syndrome? |
-very rare -deficits of kinesthesia (e.g. stereognosis and 2-point discrimination) -deficits of proprioception -ataxic gait with wide BOS may result causes: trauma, extrinsic compression from posteriorly located tumors, MS -tabes dorsalis (teritary syphilis) preferentially affects posterior cord |
|
|
What is Cauda equina syndrome? |
injury below the L1 segment that results in damage to the lumbar and sacral nerve roots -sensory loss -paralysis -loss of Bladder/bowel control can occur -bc damage is to the peripheral nn roots, regeneration may be possible |
|
|
What is sacral sparing? |
-refers to incomplete lesion in which the most centrally located sacral tracts are spared 1. perianal sensation 2. rectal sphincter contraction 3. cutaneous innervation in the saddle area 4. active contraction of the sacrally innervated toe flexors are intact |
|
|
what does paralysis of voluntary motor control in SC injuries occur from? |
damage to descending motor tracts anterior horn cells spinal nerves |
|
|
How does SCI result in spasticity? |
-after spinal shock resolves, reflexes return and become progressively stronger resulting in spasticity -more prevalent with higher lesions and incomplete lesions -hypertonicity and hyperreflexia cause quick stretching of the mms to elicit exaggerated reflexive response |
|
|
what can loss of sensation following SCI result in? |
-discoordination of body movements -vulnerability to trauma -impaired body awareness |
|
|
How is respiration affected with SCI? |
-depends on level of lesion -C3, C4, C5 = diaphragm; if not active will affect pt's ability to breathe (inhalation) -an artificial ventilator or phrenic nn stimulater may be required to sustain life -disruption to intercostals and abdominal mms can impair respiration (primarily forced expiration and inhalation) -tidal volume and vital capacity are reduced and secondary respiration muscles are utilized more (e.g. scalenes) |
|
|
How is bowel and bladder function affected in SCI? |
1. voluntary control of urination and defecation is lost after injury to S2-S4 2. After spinal shock, 2 types of bladder conditions A. Reflex (UMN) bladders: empty in response to certain level of filling pressure (aka hyperreflexic or spastic bladder) -results in urge incontinence (urinary urgency) B. Autonomous or nonreflex (LMN) bladder: flaccid and can be emptied by increasing intra-abdominal pressure or by manually compressing the lower abdomen (results in overflow incontinence) |
|
|
How is genital function affected by SCI? |
-injury to thoracolumbar and sacral regions can alter functioning of genitals and disrupt sexual response -female fertility is unchanged -men more likely to become infertile -Parasympthetic = pointing= erection (S2-S4) -Sympathetic = shooting = ejaculation (T11-L1) |
|
|
How can SCI affect cardiovascular function? |
-lesions that interfere with communication between thoracolumbar cord and brainstem cause loss of sympathetic input to heart -parasympathetic input remains -->bradycardia, peripheral vasodilation and hypotension -orthostatic hypotension occurs = drop of at least 20 mm Hg in systolic BP or decr in DBP of at least 10 when changing position (supine to upright) -cardiovascular problems usually significant in ppl with lesions above T6 and often resolve within a few weeks of injury |
|
|
What is treatment for SCI orthostatic hypotensions? |
-thigh high TED hose + -abdominal binder -start with tilt in space w/c so can tilt back if need to |
|
|
How does SCI affect thermoregulation? |
-interruption of communication with hypothalamus can result in hypothermia due to peripheral vasodilation -reflexive tone returns in the peripheral vasculature, resolving this problem -later, hyperthermia occurs due to loss in sympathetic control of the sweat glands below the lesion -compensation for lack of sweating below lesion is diaphoresis above lesion |
|
|
What type of SCI patient is prone to pressure sores (decubitus ulcers)? |
-complete lesion and tetraplegia -impaired sensory function and lack of motor function to make frequent positional changes incr likelihood of pressure sores -relief over bony areas should take place 3-4 x per hour or every 15-20 min regardless of the material under the pt |
|
|
What is the most common cause of death following SCI? |
respiratory dysfunction
|
|
|
What are respiratory complications following SCI? |
-inability to cough effectively allows secretions to build in the lungs (decreased forced expiration) -inadequate inhalation and exhalation can reduce ventilation of lungs leading to atelectasis, pneumonia, and respiratory insufficiency |
|
|
How can contractures best be prevented following SCI> |
AROM periodically of joints through available ROM -PROM is 2nd best option |
|
|
What causes increased osteoporosis post SCI? |
-loss of calcium from bones below the level of lesion = incr risk of fractures -treatment = dietary management and early mobility activities to place stresses on the skeletal system (Wolff's law) |
|
|
What causes SCI patients to have incr risk of DVT and how can they be prevented? |
-occurs when thrombus forms within a blood vessel = medical emergency -loss of normal mm pumping action to move blood through veins contributes to thrombus formation -DVTs occur most frequently in first 3 months following SCI -prevent with regular turning program, PROM, elastic stockings, proper positioning of LEs (elevation) |
|
|
What are GI complications of SCI? |
-stress ulcers in stomach or duodenum in 5-22% during acute phase -bowel obstruction -fecal impaction -gastric dilation -bowel programs goal = regular evacuation with diet, stool softeners, fluid intake, digital stimulation, suppositories, manual stretch of sphincters with evacuation Reflex bowel = above conus medullaris (must use above techniques) Non reflex bowel = below conus medullaris and can strain using available muscles |
|
|
What is autonomic dysreflexia? |
medical emergency -mass sympathetic discharge caused by noxious stimuli -sudden increase in BP, bradycardia, pounding HA, flushing, profuse sweating, and anxiety -Occurs in lesions above T6 and more prevalent in first 3 years -most common cause = bladder distension -other causes: rectal distension, pressure sores, urinary stones, bladder infections, noxious cutaneous stimuli, kidney malfunction, and environmental temperature changes -bladder drainage system should be checked immediately and opened up if necessary -if lying flat, raise head (sit pt up) to lower BP |
|
|
What causes postural or orthostatic hypotension in SCI patients? |
lack of mm tone + loss of sympathetic vasoconstriction = venous pooling in the periphery -also due to immobilization for 6-8 weeks -symptoms: dizziness and faintness or impeding blackout -tx: slow progression to vertical position while vital signs are monitored and use of compressive stockings and an abdominal binder to minimize hypotensive effects |
|
|
What is heterotopic bone formation complication of SCI? |
-osteogenesis in soft tissue below the level of the lesion (formation of new bone between muscles and other connective tissue below the lesion) -unknown etiology -different from myositis ossificans which results from trauma to the mm tissue and bony deposits WITHIN mm tissue -occurs in 16-53% of all pts with SCIs -appears 1-4 mo after injury and can restrict ROM -treatment - combination of drug therapy and regular exercises during early stages of ectopic bone formation |
|
|
What is a patient with C1-C3 SCI capable of key muscles Assistive devices |
capable of talking, mastication, sipping, blowing key muscles: face and neck muscles -dependent self-care -requires portable ventilator or phrenic nn stimulator, power "tilt-in-space" w/c with mouth control and seat belt for trunk control -C3 lesion can attain indep with this equipment on smooth surfaces -Assistive technology devices (ATDs) and electronic aids to daily living (EADLs) make interaction with or mastery of environment feasible |
|
|
What is a patient with C4 SCI capable of key muscles Assistive devices |
CAPABLE OF: respiration, scapular elevation KEY MUSCLES: diaphragm, trapezius -ventilator usually not needed -glossopharyngeal breathing is used to cough -chin control to adjust w/c -limited feeding and ADLs may be possible with use of mobile arm supports, environmental controls, adapted eating equipment, head or mouth stick or other adaptive equipment |
|
|
what is a patient with a C5 SCI capable of key muscles Assistive devices |
CAPABLE OF: Elbow flexion and supination, shoulder ER, abd to 90 deg and limited shoulder flexion KEY MUSCLES: biceps, brachialis, brachioradialis, deltoid, infraspinatus, rhomboids, and supinator -mobile arm support assist UE ADL performance -mod to min for lower extremity dressing and rolling -dependent for transfers with aid of sliding board or swivel board -Power chair with hand controls (joy stick) for community integration and manual w/c with rim projectors 200-300 feet indoors -driving is possible with van lift -achieve ischial pressure relief with forward lean but is usu dependent -needs assistance for manual cough technique |
|
|
What is a patient with a C6 SCI capable of key muscles Assistive devices |
CAPABLE OF: shoulder flexion, ext, IR and adduction, scapular abd and UR, forearm pronation, wrist extension (tenodesis grip) KEY MUSCLES: ECRB, ECRL, infraspinatus, lats, pec major, SA, Teres minor -can become indep in self-care with equipment (e.g. sliding board using clavicular head of pec major to pull self over (triceps still not working at this level) -indep in rolling and unsupported sitting can be long-term goals -use of manual w/c with projections or friction hand rims for household mobility. May require power w/c for community integration -locks on casters positioned sideways provide increased stability in transfers -uses manual cough technique indep -can live without assistance if well motivated -can drive automobile with hand controls
|
|
|
What is C7 capable of ? |
-elbow ext -wrist flexion -finger extension |
|
|
WHAT are key muscles of C7? |
EPL EPB extrinsic finger extensors FCR triceps |
|
|
What is C7 capable of in terms of LE? |
indep in LE self-range of motion exercises -more indep in transfers due to triceps working |
|
|
What type of w/c is appropriate for C7 SCI? |
manual w/c with friction hand rims for community integration with some difficulty on rough terrain -able to get w/c in and out of car |
|
|
What is C7 able to do in terms of dressing? |
button hook may be required for indep dressing |
|
|
What is C8 SCI capable of ? |
full use of all UE muscles except intrinsics of the hand |
|
|
What are key muscles of C8 SCI? |
-extrinsic finger flexors -FCU -FPL -FPB |
|
|
What is C8 SCI capable of in terms of living? |
indep in living at home except for heavy work -may need tub seat, grab bars, etc, for full indep at home -able to work in a building free of architectural barriers |
|
|
What is C8 SCI capable of in terms of w/c mobility? |
may be able to indep go up/down curbs with manual w/c
|
|
|
What is T1-T5 capable of? |
-full use of UE -improved trunk control -increased respiratory reserve |
|
|
What are key muscles of T1-T5 SCI? |
top half of intercostals -long muscles of back -intrinsic finger flexors
|
|
|
What is T1-T5 capable of in terms of standing? |
standing table for physiologic standing
|
|
|
What is T1-T5 SCI able to achieve in terms of independence? |
-indep in all areas including car transfers -able to negotiate curbs using a wheelie technique -participates in w/c sports |
|
|
What is a T6-T8 SCI capable of? |
-improved trunk control -improved respiratory reserve |
|
|
What are key muscles for T6-T8? |
long muscles of the back including sacrospinalis and semispinalis |
|
|
What is T6-T8 SCI capable of in terms of gait and locomotion? |
-Independent in swing-to gait in parallel bars with bilateral knee-ankle-foot-orthoses (KAFOs) for short distances -Supervision with walker & KAFOs in home -w/c for community locaomotion |
|
|
What is T9-T12 capable of? |
Increased endurance |
|
|
Key muscles of T9-T12 SCI |
Lower abdominals |
|
|
T9-T12 SCI & gait |
-Independent swing-to or swing-through gait on level surfaces with bilateral KAFOs and a walker or forearm crutches -May be independent household ambulators -Will usually use a WC for outdoor locomotion & energy conservation |
|
|
T9-T12 SCI & transfers |
Independent floor to WC and tub transfers |
|
|
What is T12-L3 SCI is capable of? |
hip flexion & ADD knee ext |
|
|
Key muscles of T12-L3 SCI |
Gracilis Iliopsoas Quadratus Lumborum Rectus femoris Sartorius |
|
|
T12-L3 SCI & gait patterns |
Independent swing-to, swing-through, or four-point gait with bilateral KAFOs and forearm crutches on level surfaces and small elevations |
|
|
T12-L3 SCI and ambulation |
-indep for home ambulation -May use a WC for energy conservation or convenience |
|
|
L4-L5 SCI is capable of |
Strong hip flexion & knee extension |
|
|
What are the key muscles of L4-L5 SCI? |
Low back muscles |
|
|
L4-L5 SCI & ambulation |
indep home ambulators with Bilat AFOs and crutches or canes -Can be community ambulators |
|
|
WC - Patients with high cervical lesions (Cl-4): |
-Require electric WC with tilt-in space seating or reclining seat back |
|
|
WC prescription for - Patients with cervical lesions at (C5): |
-Can use a manual chair with propulsion aids (e.g., projections) |
|
|
WC prescription for - Patients with cervical lesions at (C6): |
Manual WC with friction surface hand rims (using wrist extensors) -May require power w/c for community |
|
|
WC - Patients with cervical lesions (C7): |
Same as for C6, but with increased propulsion due to triceps function -can use for community mobility with difficulty on rough terrain |
|
|
WC Prescription for (C8-Tl and below): |
Manual WC -Ambulation not functional until T12 or L1 and below -short distance amb not even possible until T6-T8 |
|
|
Head or Mouth Stick is used by patients with what SCI? |
Quadriplegia |
|
|
Head or Mouth Stick can be used to: |
12-18 inches long (wooden or metal rod) to hold utensils or devices such as pencils |
|
|
Mobile Arm Support's typical candidates would have what muscles? |

-device attached to WC -generally used by pts with weak proximal UE mms -Shoulder flexors |
|
|
Static Wrist-Hand Orthosis is used by patients with what level lesions? |
Cl-C5 lesions that have no wrist extensors |
|
|
Static Wrist-Hand Orthosis maintains what? |
-Functional hand position, which includes the thumb in ABD & support for the palm |
|
|
What is Wrist-Driven Orthosis (Tenodesis Splint)? |
A dynamic functional orthosis designed to assist with grasp -transfers mm force produced by wrist extensors to provide finger flexion and more functional prehension |
|
|
What level is Wrist-Driven Orthosis (Tenodesis Splint) used by? |
C6 or C7 lesion |
|
|
When is Wrist-Driven Orthosis (Tenodesis Splint) used? |
Sliding board transfers need to be performed with finger flexion or wrist in neutral to avoid stretching tight flexor tendons (tenodesis) of the hand and wrist |
|
|
T6-8 SCI & Ambulation: |
Limited Household: Supervision with walker and KAFOs short distances using swing-to gait |
|
|
T9-T12 ambulation |
Household amb: indep +swing to or swing through gait +bilat KAFOs + walker or forearm crutches Community: w/c due to energy conservation |
|
|
T12-L3 and ambulation |
Functional ambulation: indep household +swing-to, swing-through, or 4-point +B KAFOs +forearm crutches COMMUNITY: can be community ambulators -w/c for energy conservation/convenience |
|
|
L4-L5 SCI and ambulation |
Functional amb: indep household +B AFOs +forearm crutches or canes COMMUNITY: can be community amb -may use w/c for energy conservation/convenience |
|
|
What does VC depend on ? |
level of lesion and muscles innervated |
|
|
What is the primary muscle os inspiration and innervation? |
diaphragm C3, C4, C5 |
|
|
What is the innervation of the intercostals and their function? |
assis in inspiration innervated by T1-T12 |
|
|
What are the function of the abdominals and innervation? |
assist in forced expiration T5-T12 |
|
|
What are the secondary muscles of respiration and innervations and function? |
Trapezius (C1-C4) SCM (C1-C3) Scalenes (C3-C5) Levator Scapula (C3-C5) assist with inspiration |
|
|
what is the vital capacity of pts on ventilators? |
(C1-C3) <15% |
|
|
What is the VC for C3-C4 lesion? |
~15% |
|
|
What is VC of patients with lesions C4-C5 |
average VC of 58% of normal |
|
|
What is initial value of VC with C6-C8 lesion and VC at discharge |
initially: ~30% increases to 50-70% |
|
|
What is VC with high thoracic level lesion? |
average 73% of normal |
|
|
What is VC for T10-T12? |
initial values may be less than normal but can increase to 100% by discharge |
|
|
What are different types of cough ability? |
nonfunctional weak functional |
|
|
What levels have nonfunctional cough? |
C1-T3 |
|
|
What levels have a weak cough |
T4-T8 |
|
|
what levels have a functional cough |
T10 and below |
|
|
what is the manual cough? |
technique of abdominal compression used to assist with clearing secretions in patients with a weak or nonfunctional cough -can be done by a therapist or family member or by the patient alone if the lesion is at C6 or below |
|
|
What is Glosspharyngeal breathing? |
aka Frog breathing -used with pts who have a high level quadriplegia in which there is an aggressive use of the tongue, pharyngeal, and laryngeal structures as a respiratory pump to gulp air and increase VC |

