![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
69 Cards in this Set
- Front
- Back
|
CNS
|
-Controls and regulates all mental and physical functions -Dysfunction of the neurons in an area of the brain can disrupt the complex organization of firing, resulting in abnormal perception of the environment, uncoordinated movement, loss of force production, and decrease in cognition |
|
|
Cellular Dysfunction |
Cell death is common in nervous system disorders • Necrosis – death of a tissue -Cellular swelling, fragmentation and cell disintegration • Apoptosis – programmed cell death - Do not cellular swelling - Necessary to prevent overproduction of one type of cell o Damage to the CNS can cause excessive apoptosis |
|
|
Cellular Dysfunction |
Glial cells - Nerve cells - Neurotransmission - Amino acids - Amines - Neuropeptides - Gaseous neurotransmitters and others |
|
|
Cellular Dysfunction |
|
|
|
Glial Cells |
Provide support and structure for the CNS similar to connective tissue in other areas of the body - Do not signal information - Macroglia and microglia – two primary cell types located throughout the CNS - Macroglia - Astrocytes - Oligodendrocytes - Schwann cells - Macroglia support and maintain neuroplasticity in the CNS - Often effected by disease processes that affect brain tissue |
|
|
Macroglia |
Astrocytes remove neuronal debris - Astrocytes are seen early in a CNS injury – astrocyte swelling - Oligodendrocytes and Schwann cells – produce the myelin sheath - Demylinated disorders (MS) are often due to disruption in the function of oligodendrocytes |
|
|
Glial Cells |
Microglia – immune cells of the brain - Respond to an insult in the CNS by proliferating and infiltration of the CNS tissue - Act like macrophages for the benefit of CNS tissue |
|
|
Nerve Cells |
Communicators for biochemical events, regulate structure and function Nucleus of the cell contains genetic material and directs manufacturing of proteins to determine structure, function and regulation of neural circuits When mutation or a change in the structure of the DNA occurs, abnormal proteins can be produced and increase chance of neurological disease Cell body inclusions – growths that occur within the cell body due to age or because of disease Result in loss of function of the cell |
|
|
Nerve Cell Communication - Neurotransmission |
Communication occurs in response to electrical, mechanical and chemical signals Nerve cells generate the following signals Input signal, trigger signal, conducting signal, and output signal Dendrite receives incoming signals from other neurons Action potential is fired through the axon Axon also serves as entry route for pathogens and toxins |
|
|
Ion Channels Responding to the Changes in Voltage |
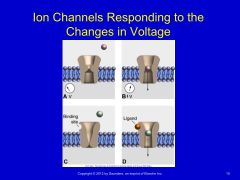
|
|
|
Neurotransmission |
Synapse – release of neurotransmitter from the presynaptic terminal and up take of that substance in the postsynaptic receptor Changes in the neurotransmitter substances is often the cause for neurological disease processes Figure 18-6 |
|
|
Neurotransmitters and Associated Responses |
Amines Acetylcholine – active in the peripheral nervous system (PNS), released at neuromuscular junctions and ANS, regulates general activity Catecholamines – working memory, decrease with age and especially with Alzheimer’s Dopamine – decreased in patients with Parkinson’s and attention disorders of the frontal lobe Norepinephrine – also associated with attending |
|
|
Neurotransmitters and Associated Responses |
Amino acids GABA – synthesized by glutamate, provides brief inhibitory responses, found in basal ganglia Glutamate – involved in cell metabolism, found in afferent nerve endings, cerebellum, dentate gyrus, important in basal ganglia function • Excess glutamate seen in stroke, TBI and SCI • May also lead to degenerative processes in ALS, Alzheimer’s, and Parkinson’s Glycine – overlaps with GABA but is found primarily in the spinal cord |
|
|
Neurotransmitters and Associated Responses (continued) |
Neuroactive peptides Enkephalins and β-endorphins: pain control achieved by use of drugs (opiates) that bind to endorphin and enkephalin receptors Substance P: involved in pain pathways |
|
|
Clinical Manifestations |
Sensory disturbances Brainstem dysfunction Movement disorders Disorders of coordinated movement Deficits of higher brain function Altered states of consciousness Memory problems Autonomic nervous system Aging and the central nervous system |
|
|
Sensory Disturbances |
Includes damage to afferent nerves, dorsal columns of the spinal cord and brainstem Symptoms – loss of cutaneous sensation, numbness, tingling, paresthesias or dysthesia Loss of proprioception – position in space, postural control |
|
|
Brainstem Dysfunction |
Controls the lower motor neurons for the muscles of the head Initial processing of afferent information involving the head Cranial nerve entry Serves as a conduit for ascending sensory and descending motor tracts of the spinal cord 3 parts – medulla, pons (including the vestibular nuclei), and the midbrain Also houses the reticular formation which influences movement |
|
|
Movement Disorders |
Movement is coordinated by many parts of the brain Parietal and premotor areas of the cerebral cortex identify targets in space, determine course of action, and create the motor program The cortex determines strategies for movement Brainstem and spinal cord execute the task |
|
|
Brain Functions |
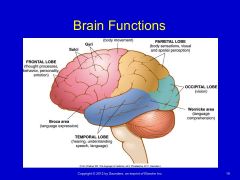
|
|
|
Disorders of Coordinated Movement |
Often involves the cerebellum Ataxia – lack of coordinated movement Usually seen in cerebellar dysfunction Hypotonicity – decreased muscle tone Usually seen in proximal muscle groups Asthenia – generalized weakness, can be seen in cerebellar lesions Dysmetria – over- or underestimation of movement toward a target, also seen in cerebellar lesions Intention tremor – over or undershooting during movement Dysdiadochokinesia – inability to perform rapidly alternating movements |
|
|
Disorders of Coordinated Movement |
Gaze-evoked nystagmus – nonvoluntary rhythmic oscillation of the eye Ocular dysmetria – similar to dysmetria of the extremities but involves the eyes’ ability to move from one target to another Gait disturbance Cerebellum has many other functions – motor learning, anticipatory/feedforward activity, cognitive and emotional processing |
|
|
Deficits of Higher Brain Function |
Cortex is responsible for language, abstract thinking, perception, movement, and adaptive response Frontal lobe – highest level of cognitive processing, control of emotion, behavior, personality Damage to frontal lobe – will see slow processing of incoming information, lack of judgement, withdrawal, irritability, lack of inhibition and apathy, lack of insight into deficits that are present Right hemisphere syndrome – inability to orient the body within external space (ie. Hemineglect |
|
|
Deficits of Higher Brain Function |
Dysarthria – disturbance in articulation (speech) Anarthria – inability to produce speech Aphasia – deficit of speech production or language output Apraxia – disorder of skilled purposeful movement and NOT a result of paresis, akinesia, ataxia, sensory loss, or comprehension Agnosia – inability to recognize an object |
|
|
Memory Problems |
Working memory – ability to hold information in short-term storage while permitting other cognitive operations to take place (depends of prefrontal cortex) Amnesia – loss of recent memory (common after TBI) Declarative memory – retention of facts and events of a prior experience or the memory of what has occurred |
|
|
Memory Problems |
|
|
|
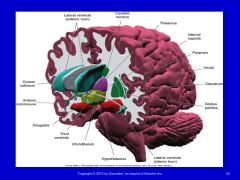
Autonomic Nervous System |
Controls unstriated tissue, cardiac muscle, and glandular tissue Efferent autonomic pathways – divided into sympathetic and parasympathetic Also includes the enteric nervous system of in the walls of the gut Neurons in the cerebral cortex, basal forebrain, hypothalamus, midbrain, pons and medulla contribute to autonomic control Hypothalamus – integrates ANS and endocrine responses for homeostasis Medulla – control of cardiovascular, respiratory and gastrointestinal function |
|
|
Aging and the CNS |
Each of the following changes are seen with aging: Loss of cells, atrophy, decreased nerve conduction velocity, wear and tear similar to that seen in musculoskeletal tissues, decreased blood supply Mood-related and depressive symptoms Loss of sensory inputs for balance, mobility, vision and somatosensation |
|
|
Diagnosis
|
Clinical localization Computed tomography Magnetic resonance imaging Functional magnetic resonance imaging Positron emission tomography Electroencephalography Brainstem auditory evoked potentials Transcranial Doppler ultraso |
|
|
Types of Central Nervous System Neoplasms |
Primary tumors: Develop in the brain, spinal cord, or surrounding structures Secondary (metastatic) tumors: May spread to the CNS from another site, such as a lung Paraneoplastic syndromes: May occur as a result of remote or indirect effects on the CNS from cancer elsewhere in the body Leptomeningeal carcinomatosis: Metastasized carcinoma throughout CNS with multiple lesions to the meninges and CSF pathways of the brain and/or spinal cord |
|
|
Types of Central Nervous System Neoplasms (Continued) |
Malignant Astrocytomas Benign–slow growth rate and relatively non-invasive Meningiomas Neurinomas Hemagioblastomas -Because of space-occupying properties in vital tissue with a resultant high threat of functional limitation, the use of the term benign is somewhat misleading. Some authors insist that because of location, even a very slow growing CNS tumor should be considered basically malignant. |
|
|
Signs and Symptoms of Brain Tumors |
Headache Visual changes (double vision, blurred vision) Nausea Vomiting Cognitive changes — impairment of memory, judgment, personality Lethargy Behavioral changes Seizures Syncope Weakness Hemiparesis, hemiplegia Apraxia Cortical sensory deficits (graphesthesia, stereognosis difficulties) Sensory impairments (tingling, spatial orientation changes) Cranial nerve palsies Aphasia Facial numbness Hearing disturbances Anosmia Swallowing difficulties Paralysis of outward gaze (sixth cranial nerve) Papilledema Incoordination Ataxia In children, diastases of cranial sutures and enlarging head size |
|
|
EPILEPSY
|
Overview and definition Epilepsy is defined as a chronic disorder characterized by recurrent seizures. Although a diagnosis of epilepsy requires the presence of seizures, not all seizures imply epilepsy. Epilepsy comes from the Greek word meaning attack and has been recognized since ancient Babylonian times when people believed seizures were caused by demons. Incidence The overall prevalence of epilepsy is approximately 5 to 8 per 1000 individuals. Incidence is highest among young children and the elderly, with men slightly more affected than women (1.5:1). Epilepsy is the third most common serious neurologic disease of old age after dementia and stroke. |
|
|
EPILEPSY (Continued) |
Etiologic and risk factors • Epilepsy may result as abnormalities in the “wiring” of the brain or imbalance of neurotransmitters, or a combination of both. • Forms that are more heritable than others are termed idiopathic or primary epilepsies. Adult-onset seizure disorder • Epilepsy can be caused by virtually any major category of serious disease or human disorder. It can result from congenital malformations, infections, tumors, vascular disease, degenerative diseases, or injury. Infantile seizure • The age-dependent appearance of spontaneous seizures in the primary epilepsies appears to depend on critical periods in cerebral maturation. • The other important cause of seizures arising in the early neonatal period is hypoglycemia. |
|
|
EPILEPSY (Continued) |
Etiologic and risk factors • Epilepsy may result as abnormalities in the “wiring” of the brain or imbalance of neurotransmitters, or a combination of both. • Forms that are more heritable than others are termed idiopathic or primary epilepsies. Adult-onset seizure disorder • Epilepsy can be caused by virtually any major category of serious disease or human disorder. It can result from congenital malformations, infections, tumors, vascular disease, degenerative diseases, or injury. Infantile seizure • The age-dependent appearance of spontaneous seizures in the primary epilepsies appears to depend on critical periods in cerebral maturation. • The other important cause of seizures arising in the early neonatal period is hypoglycemia. |
|
|
EPILEPSY (Continued) |
Pathogenesis All seizure activity is a result of chaotic, excessive electrical discharge in the central nervous system (CNS). Susceptibility to these seizures most likely results from inherited biochemical, membrane, or neurotransmitter defects that result in abnormal excitability within the involved circuits. Events that may trigger a seizure: • Stress • Poor nutrition • Missed medication • Skipping meals • Flickering lights • Illness • Fever and allergies • Lack of sleep • Emotions such as anger, worry, or fear • Heat and humidity |
|
|
EPILEPSY (Continued) |
Clinical manifestations Signs and symptoms • In most individuals, seizures occur unpredictably at any time and without any relationship to posture or ongoing activities. Tonic-clonic seizures • In the tonic phase of a tonic-clonic seizure, the body becomes rigid and the person is at risk of falling • The clonic phase begins with rhythmic, jerky contractions especially in the extremities and ends with relaxation of all body muscles |
|
|
EPILEPSY (Continued) |
Prognosis Persons with epilepsy have increased mortality rates compared with the general population. Much of this increased risk occurs in individuals with symptomatic epilepsy in whom mortality relates to the underlying condition. Death from asphyxia is the greatest concern in instances when the individual has a seizure during eating or when the airway is compromised during the seizure or in the postepileptic phase. |
|
|
EPILEPSY (Continued) |
Classification of seizures Partial seizures • Simple partial seizures • Complex partial seizures • Partial seizure evolving to secondarily generalized seizures Generalized seizures • Absence seizures • Myoclonic seizures • Atonic seizures Tonic-clonic seizures Status epilepticus |
|
|
EPILEPSY (Continued) |
Common misconceptions about epilepsy Myth: You can swallow your tongue during a seizure. Fact: It’s physically impossible to swallow your tongue. Myth: You should restrain someone during a seizure. Fact: Do not use restraint; the seizure will run its course and stop. Myth: People with epilepsy should not be in jobs of responsibility and stress. Fact: People with epilepsy hold many types of jobs; they often do not inform others of the disorder. Myth: You can’t tell what a person may do during a seizure. Fact: The characteristic form of seizure is consistent during each episode. Behavior may be inappropriate for the time and place but will most likely not cause harm. Myth: You can’t die from epilepsy. Fact: Status epilepticus can cause death. It should be treated as a medical emergency |
|
|
PRIMARY HEADACHES |
Migraine • “A familial disorder characterized by recurrent attacks of headache widely variable in intensity, frequency and duration.” Migraine without aura Migraine with aura Typical aura without headache Sporadic and familial hemiplegic migraine Basilar-type migraine Vestibular migraine Ophthalmoplegic migraine Retinal migraine Status migrainosus Chronic migraine |
|
|
PRIMARY HEADACHES |
Cluster headaches • Rare, but are the most painful of the primary headaches Episodal cluster headache • Defined by periods of susceptibility to headache, called cluster periods, alternating with periods of remission • The most common type, constituting 80% of all cases Chronic cluster headache • A term used when the headaches have gone on for at least 12 months and remissions last less than 14 days • Evolves from episodal CH Other classifications • Paroxysmal hemicrania • Short-lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing • Probable trigeminal autonomic cephalalgia |
|
|
SECONDARY HEADACHES |
Cervicogenic headaches Pain is localized to the neck and occipital regions and may project to the forehead, orbital region, temples, vertex, or ears Pain is precipitated or aggravated by special neck movements or sustained neck posture Posttraumatic headache syndromes Not a single pathology but a group of traumatically induced disorders with overlapping symptoms When the headache develops within 7 days of the trauma and resolves within 3 months, it is considered acute The headache can begin weeks or months after the trauma and can persist for years; this considered chronic |
|
|
SECONDARY HEADACHES |
Classifications of headache attributed to head or neck trauma Acute posttraumatic headache Chronic posttraumatic headache Acute headache attributed to whiplash injury Chronic headache attributed to whiplash injury Headache attributed to traumatic intracranial hematoma Headache attributed to other head and/or neck trauma Postcraniotomy headache |
|
|
SECONDARY HEADACHES |
Medication overuse headaches Frequent intake of medications used for headache can lead to chronic headache. It appears that all drugs used for the treatment of headache may lead to chronic headache. Migraineurs are most susceptible to headache related to excessive medication. Overuse of analgesic medications resulting in analgesic rebound phenomenon is common when the headache type has not been identified appropriately. |
|
|
SECONDARY HEADACHES |
Headaches in the elderly New-onset headaches in the elderly that are related to another disorder are more common than in the young. Such headaches can be caused by: • Increased use of nitrates for control of angina • Hypertension and atherosclerotic and hemorrhagic cerebrovascular disease • Diseases of the aged such as chronic obstructive lung disease • The hypercalcemia related to malignancy and chronic renal failure • Parkinson’s disease • Intracranial disease, tumors, and subdural hematomas • Cervical spondylosis and TMJ • Depression |
|
|
SECONDARY HEADACHE |
Temporal arteritis The headache of temporal arteritis classically is located over a branch of the superficial temporal artery and is described as a dull ache that persists throughout the day. Headache is the most common symptom in temporal arteritis, and this diagnosis should be considered in all adults older than 50 years who have headache or facial pain. Temporal arteritis may be related to widespread rheumatologic involvement such as polymyalgia rheumatica. Symptoms may include easy fatigability, weight loss, anorexia, and unexplained fevers, as well as proximal myalgias |
|
|
SECONDARY HEADACHE |
Sinus headaches The pain is usually localized to the frontal or maxillary area, and there is tenderness to tapping over the affected sinus. The pain is of low to moderate intensity and is present on a daily basis. Postdural puncture headaches Can occur after lumbar puncture or with epidural anesthesia The headache is due to leakage of cerebrospinal fluid and changes in the pressure within the skull. The headache is usually self-limiting but can last 3 to 5 days |
|
|
VESTIBULAR DISORDERS |
Because the vestibular system provides information about orientation in space, disorders of the vestibular system can cause a devastating abnormal sense of movement, visual instability, and loss of balance. Damage to the peripheral vestibular nerve can arise from a neurologic pathology, mechanical deformation from a nonneurologic pathologic condition, or trauma to the structures surrounding the nerve. |
|
|
COMMON CAUSES |
Benign positional vertigo Episodic, intense vertigo related to head position; is most often a benign disorder called benign paroxysmal positional vertigo Infection Viral infection is common and usually affects the vestibular nerve unilaterally The use of antibiotics in general has decreased the incidence of bacterial infections affecting the vestibular system; however, infections still do arise and can be introduced into the vestibular apparatus. |
|
|
COMMON CAUSES (continued) |
Endolymphatic hydrops and Meniere’s syndrome A disorder relating to the membranous inner ear as a consequence of the overaccumulation of endolymph compromising the perilymphatic space Perilymphatic fistula An abnormal communication of the inner and middle ear spaces, can cause vertigo |
|
|
COMMON CAUSES (continued) |
Ototoxicity Ototoxicity is usually seen in individuals who are given multiple doses of antibiotics over time or one large dose, usually aimed at managing a threatening infection. Damage to the hair cells in the inner ear can result in complete loss of vestibular function within 2 to 4 weeks after these drugs have been given. Mal de Debarquement A syndrome that is named essentially for the symptoms related to “getting off the boat.” It is usually triggered after a long time spent on a ship, such as during a cruise, or by an extended train ride. |
|
|
COMMON CAUSES (continued) |
√ Autoimmune ear disease Rapidly progressive bilateral sensorineural hearing loss, typically characterized by symptoms of pressure and tinnitus in the ears with or without dizziness. Neoplasia Primary carcinoma can directly involve the end organ, the middle ear, or the mastoid. Glomus tumors arethe most common tumor of the middle ear. |
|
|
COMMON CAUSES (continued) |
Traumatic brain injury Complaints of dizziness and imbalance are common after traumatic brain injury (TBI) and may affect as many as 50% of the individuals who experience TBI. Psychologic disorders and somatoform dizziness Forty percent of dizzy individuals have psychologic disorders and, in general, individuals with psychiatric disorders report more disability from dizziness than do individuals without psychiatric involvement. |
|
|
Cerebral Palsy (CP) |
CP • Permanent, nonprogressive neurologic disorder of motor function • Impairment in postural control and movement • Due to – Faulty development – Injury – Damage to motor cortex in the brain • Symptoms usually appear before the age of 2 |
|
|
Typical Signs of CP |
• Spas;city • Muscle weakness • Ataxia • Rigidity • Atypical movement patterns • Slow to reach developmental milestones • Musclesof speech, swallowing and breathing may be involved • Intellectual disabilities and seizures may also occur • Incidence: 500,000 in 2002: cost for care $8.2 billion |
|
|
Pathology |
• Permanent brain insult during pregnancy (prenatal), delivery (perinatal), or shortly after birth (postnatal). • Premature birth: increased risk of CP • Prior to 1980, thought result of birth trauma: only a small fraction due to birth trauma • 2 types 1. Congenital (present at birth) 2. Acquired (after birth within the first few years of life) |
|
|
Congenital CP
|
• Brain damage during pregnancy or around the time of birth • High risk: very low birth weight, premature, multiple pregnancy • Causes 1. Infection during pregnancy 2. Jaundice untreated: athetoid CP 3. Rh incompatibility: mother’s immune cells attack the fetus 4. Oxygen shortage: hypoxic-.‐ischemic encephalopathy 5. Stroke: coagula;on disorder 6. Toxicity: drug or alcohol use during pregnancy 7. Bleeding in the infant’s brain 8. Kidney and UTI |
|
|
Acquired CP |
• Brain damage in the first few months or years of life • Causes 1. Brain infection: encephalitis, meningitis 2. Head trauma or injury: falls, MVA, child abuse |
|
|
CP |
• No cure • Early diagnosis and treatment can improve the child’s chances of independence • Display a wide range of capabilities and level of involvement |
|
|
Classification of CP |
• Muscle tone: the amount of resistance to movement • Tone must be balanced to move smoothly • Types of tone 1. Spas;c: hypertonic 2. Hypotonic 3. Ataxic 4. Athetoid: dyskinetic
• Use Modified Ashworth Scale |
|
|
Spastic CP |
• Most common • Muscles stiff, tight • Increased resistance to passive movement • Abnormal reflexes:clonus: hyperactive • Hypersensitivity to sensory stimuli •Joint movement may be limited: joint deformities |
|
|
Hypotonic CP |
• Decreased tone throughout • Poorly defined muscles • Decreased responses to DTR • Hypermobile joints |
|
|
Athetoid CP |
• Fluctuating tone • Writhing movements |
|
|
Ataxic CP |
• Poor balance & coordination • Gait requires a wide base of support |
|
|
Classification of CP cont… |
• Patternern of motor development 1. Hemiparesis 2. Quadraparesis: tetraparesis 3. Diplegia: involvement primarily in legs 4. Triplegia • May be combined with first classifica;on: spastic quadraparesis |
|
|
Classification of CP cont…. |
• Gross Motor Functional Classification •Categorizes children by degree of severity or functional capacity •Qualita;ve, objective measure of prognosis for gross motor skills |
|
|
Level 1
|
• Infant 1. Can move in & out of sitting 2. Floor sit independently 3. Manipulate objects with their hands before 18 months • Child 1. Ambulate independently before 2.By4 can get up from floor into standing without assistance 3. By 6 can climb stairs • Adolescence 1. Able to ambulate on all surfaces without assistance 2. Can run & jump with reduced speed, balance |
|
|
Level II
|
• Infant 1. Able to maintain floor sitting but must use hands to maintain balance 2. Commando or belly crawling 3. Pulling to stand using furniture • Child 1. Beginning to cruise before age 2
2. By age 4, requires 1-2 hands to floor sit • Transition in & out of sit independently • Pull to stand on stable surface • Crawling reciprocal pattern • Ambulation with assistive device
3. At age 6, can sit on floor with both hands free • Ambulate short distances without assistive devices • Require assistive device when walking in community until age 12 • Climb stairs using rail • Cannot run or jump
• Adolescent 1.By age 12, uneven surfaces, inclines, crowds still difficult 2. Can ambulate without device for most conditions
|
|
|
Level III |
• Infants 1.Can maintain floor sitting when lower back is supported 2. Can roll & creep forward in prone
• Child 1. Between 2 & 4: “W” sit •Creep on stomach or crawl on hands & knees (often without reciprocal leg movement) • May pull to stand on stable surface • Cruise short distances •Walk short distance indoors using assistive device: need assistance for steering 2.Age 6: independent in chair, walk with assistive device, climb stairs with assistance • Adolescence 1.Age 12: can independently ambulate in community with assistive device, climb steps using rail, use wheelchair for longer distances |

