![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
278 Cards in this Set
- Front
- Back
|
Agnosia: |
inability to recognize familiar objects with one form of sensation (for example – visual agnosia) |
|
|
Akinesia: |
Inability to initiate movement |
|
|
Aphasia: |
Disturbance to language that results in errors in word choice, comprehension, or syntax |
|
|
What is expressive aphasia and what area of the brain is affected with this? |
Severe difficulty in verbal expression with impairment in object naming and writing abilities. This is found in Broccas area; mostly found in those with R hemiplegia |
|
|
What is the global aphasia? |
The most common and severe form of aphasia: characterized by reduced speech and comprehension. Reading and writing are impaired as well |
|
|
What is receptive aphasia and what area of the brain is affected with this? |
Severe disturbance and auditory comprehension. Reading, writing, and word recognition are also impaired. This is found in Wernecke's area |
|
|
apraxia: |
Inability to perform movements previously learned even though there is no loss of strength, coordination, sensation, or comprehension |
|
|
Ideational apraxia: |
Person no longer gets the idea of how to do a routine task; for example washing hands or brushing teeth |
|
|
Ideomotor apraxia: |
Person cannot do a task on command but can do it spontaneously |
|
|
Astereognosis: |
Inability to recognize objects by touch alone |
|
|
Asynergia: |
Inability to move muscles together in a coordinated manner |
|
|
Ataxia: |
Uncoordinated movement, especially gait |
|
|
Athetoid: |
Slow, involuntary, worm like, twisting motions. Usually seen in forms of cerebral palsy |
|
|
causalgia: |
Burning sensations, which are painful. |
|
|
What impairment or disorder is causalgia often associated with? |
Complex regional pain syndrome Type I (formerly reflex sympathetic dystrophy) |
|
|
Cheyenne-Stokes respiration: |
A common and bizarre breathing pattern characterized by periods of apnea lasting 10 to 60 seconds followed by gradually increasing, then decreasing depth and frequency of respirations. |
|
|
What does Cheyne-Stokes respirations accompany? What may it be a result of? |
it is postulated to be a result of an abnormality in the neurologic respiration center; can occur with severe cases of TBI or CHF |
|
|
Chorea: |
Rapid, involuntary jerking movements; seen especially in Huntington's disease |
|
|
Clonus: |
rhythmic oscillation of the muscle in response to sustained stretch in patients with upper motor neuron disease |
|
|
Decerebrate rigidity: |
Contraction of the extensor muscles of the upper and lower extremities because of an injury at the level of the brainstem |
|
|
Decorticate rigidity: |
Contraction of the flexor muscles of the upper extremities with contraction of the extensor muscles of the lower extremities |
|
|
Delirium: |
Temporary confusion and loss of mental function |
|
|
What is delirium often a result of? |
1) Illness 2) drug toxicity 3) lack of oxygen Often reversible |
|
|
Dementia: |
Loss of memory or intellectual functioning |
|
|
In what cases may dementia be reversible? |
When caused by toxins, drugs, metabolic, or psychiatric disorders. |
|
|
In what cases is dementia often not reversible and slowly progressing? |
When it is a result of alcoholism, Alzheimer's disease, infarction, Parkinson's disease, etc. |
|
|
Dysmetria: |
Inability to judge distances |
|
|
What part of the brain is generally associated with dysmetria? |
Cerebellar dysfunction |
|
|
Electromyography (EMG): |
The study of a graphic record of the contraction of a muscle as a result of electrical stimulation. Used to evaluate the voluntary electrical activity of the muscle |
|
|
Glove and stocking anesthesia: |
Can occur in generalized peripheral neuropathy's in which the distal portions of the nerves degenerate resulting in anesthesia of the distal extremities in a pattern as if the patient were wearing long gloves and stockings |
|
|
What impairment is glove and stocking anesthesia occasionally scene with? |
Guillain-Barré |
|
|
Herpes zoster (shingles): |
A painful inflammation of the posterior root ganglion |
|
|
What causes herpes zoster? |
A virus |
|
|
What is the result (regarding presentation) of herpes zoster? |
The formation of vesicles (fluid filled sac) along the course of the nerds (dermatomal pattern) |
|
|
Horner's syndrome: |
Ptosis of the eyelid, construction of the pupil, and sweating of the ipsilateral face |
|
|
What does Horner's syndrome often accompany? |
stroke involving the anterior inferior or posterior inferior cerebellar arteries |
|
|
morton's neuroma: |
Often an excessive pronation during stance produces compression between the third and fourth metatarsals; The nerve can enlarge forming a neuroma on the inter-digital nerve resulting in metatarsalgia |
|
|
Nerve conduction velocity test (NCV) |
determines the speed of propagation of an action potential along a nerve or muscle fiber |
|
|
If the nerve is compressed or damaged, what happens to the velocity of action potential and latency? |
The velocity of the action potential will be slowed and the latency, or time the potential takes to travel between two points, will be increased. |
|
|
What is a nerve conduction velocity test utilized to determine?
|
the severity of nerve compression (Ie: from a herniated disc) prior to surgery. |
|
|
Nystagmus: |
rapid, usually back and forth, movement of the eyeballs |
|
|
Reciprocal inhibition:
|
inhibition of muscles antagonistic to those being facilitated |
|
|
What is reciprocal inhibition essential for?
|
Coordinated movement |
|
|
Romberg's sign: |
loss of balance in standing when the eyes are closed |
|
|
Somatagnosia: |
A lack of awareness of the relationship of one's own body part or the body parts of others |
|
|
Vegetative state: |
a deep coma with abnormal posturing; the patient may not have rehabilitation potential if this state persists |
|
|
Visual acuity:
|
sharpness of vision; generally decreases with age or certain disabilities such as diabetes |
|
|
What might people with visual acuity impairment require? |
Reading glasses to focus on or read things nearby |
|
|
What strategies may assist people with visual acuity impairments?
|
Due to the decreased ability to adapt to very dark or light environments these people may need more or higher intensity lighting at home or use color contrast on the walls, floors, and stairs to increase safety during ambulation. |
|
|
Name the three common visual field deficit.
|
1) Homonymous hemianopsia, 2) Bitemporal hemianopsia, 3) blindness in one eye a.k.a. monocular blindness |
|
|
Homonymous hemianopsia:
|
a visual deficit of either the right or left halves of both eyes |
|
|
What causes a Homonymous hemianopsia? |
Damage to the contralateral optic tract
|
|
|
Bitemporal hemianopsia:
|
a visual deficit of the outside halves of both eyes
|
|
|
What causes bitemporal hemianopsia? |
Injury at the optic chasm
|
|
|
What is another term for bitemporal hemianopsia? |
Tunnel vision |
|
|
What is monocular blindness or blind in one eye a result of? |
Damage to the optic nerve |
|
|
Cerebral vascular accident:
|
arterial occlusion or hemorrhage in the brain
|
|
|
Stroke produces focal signs specific to what?
|
The artery involved |
|
|
What are the most common sites for lesions to occur ( with regard to stroke)?
|
1) The origin of the common carotid artery me, 2) at the main bifurcation of the middle cerebral artery, 3) at the junction of the vertebral arteries with the basilar artery |
|
|
What artery is most commonly involved in a stroke? |
MCA a.k.a. middle cerebral artery |
|
|
A stroke that presents with contralateral hemiplegia, mostly upper extremity involvement, and loss of sensation primarily in the arm and face is likely to stem from a lesion where? |
MCA |
|
|
A stroke that presents with Homonymous hemianopsia is commonly due to a lesion where? |
MCA a.k.a. middle cerebral artery
|
|
|
An infarction in a dominant left hemisphere may produce what type of presentation? |
Aphasia and apraxia |
|
|
Occlusion of the main stem of the MCA can cause what? |
Global aphasia |
|
|
This artery is rarely involved, however when it is involved in a stroke the lower extremity is more frequently affected; what artery is this?
|
Anterior cerebral artery |
|
|
A lesion in this area will often result in contralateral hemiplegia and sensory loss |
Anterior cerebral artery |
|
|
A lesion in what area can result in mental confusion, aphasia, and contralateral neglect if involvement is extensive on the dominant side? |
Anterior cerebral artery |
|
|
A lesion in what area presents as persistent pain syndrome or contralateral pain and temperature sensory loss? |
Posterior cerebral artery |
|
|
Homonymous hemianopsia, aphasia, and thalamic pain syndrome can result from the occlusion of this artery |
posterior cerebral artery |
|
|
A lesion in what area often results in death from the edema associated with the infarct? |
Vertebral basilar
|
|
|
If a patient survived a vertebral basilar lesion affecting the pons what could be the result? |
Quadriparesis and bulbar palsy or a "locked in state" whereby the patient can only communicate by eye blinking |
|
|
What are other the vertebral artery symptoms? |
1) vertigo, 2) coma, 3) diplopia, 4) nausea, 5) dysphasia (difficulty swallowing), and 6)ataxia |
|
|
Stages of recovery following a stroke: what is present early, often with no voluntary movement? |
Flaccidity |
|
|
Stages of recovery following a stroke: what might the flaccid stage be followed by?
|
1) spasticity, 2) hyperreflexia, 3) synergies (mass patterns of movement) |
|
|
Stages of recovery following a stroke: late in recovery, what type of movement patterns become possible?
|
Isolated and advanced movement patterns |
|
|
Stages of recovery following a stroke: describe stage 1 |
flaccid, no limb movement |
|
|
Stages of recovery following a stroke: describe stage 2 |
1) synergies may appear, 2) Spasticity begins to develop, 3) minimal voluntary control
|
|
|
Stages of recovery following a stroke: describe stage 3 |
1) spasticity increases and may become severe, 2) voluntary control of movement synergies appear |
|
|
Stages of recovery following a stroke: describe stage 4
|
1) some movement independent of synergies, 2) spasticity begins to decline |
|
|
Stages of recovery following a stroke: describe stage 5 |
if patient progresses, synergies no longer dominate and movement becomes more complex |
|
|
Stages of recovery following a stroke: describe stage 6 |
1) spasticity is gone, 2) coordination and movement approach normal |
|
|
Synergies: |
primitive and stereotyped movement patterns associated with spasticity |
|
|
How may synergies be elicited? |
Reflexively, as associated reactions or as voluntary movement patterns |
|
|
What are the two basic synergies of each extremity? |
Flexion synergy and extensor synergy |
|
|
What does flexion synergy of the upper extremity present as? |
1) scapular elevation and retraction, 2) shoulder abduction and external rotation, 3) elbow flexion (generally the strongest component), 4) forearm supination and 5) wrist/finger flexion |
|
|
What does flexion synergy of the lower extremity present as? |
1) hip flexion (generally the strongest component), abduction, external rotation; 2) knee flexion; 3) ankle dorsiflexion and inversion, 4) toe dorsiflexion |
|
|
Extensor synergies are exactly the opposite of flexor synergies except for what?
|
Except for wrist/finger flexion and ankle inversion, which are common to both |
|
|
When do tonal changes occur in patients?
|
In patients following a stroke as well as with other neurological conditions |
|
|
Name one positive and one negative effect of tone? |
It can interfere with function or can be used to develop movement patterns (synergies) |
|
|
Hypotonicity:
|
floppy, low tone, flaccid, risk of dislocation of atlantoaxial joint (spinal cord injury potential), hip, knee, elbow, shoulder, etc. |
|
|
What two things are associated with hypotonicity?
|
1) Hypoactive reflexes and 2) shallow breathing patterns |
|
|
What are treatments for hypotonicity?
|
1) avoid hyperextension, 2) work for joint compression and facilitation to help normalize tone, 3) use resistance of functioning muscles and isometric holding to increase activation of inactive muscles, 4) facilitation techniques |
|
|
Name some facilitation techniques for treating hypotonicity:
|
1) quick stretch, 2) tapping of muscle belly or tendon, 3) high frequency vibration, 4) light touch, 5) quick icing, 6) fast spinning or rolling. |
|
|
In a patient with hypotonicity, what does joint approximation facilitate? |
cocontraction |
|
|
Hypertonicity: |
spastic, high tone with hyperactive reflexes, and decreased thoracic mobility |
|
|
Individuals with hypertonicity are at risk for what? |
Contractures and deformity
|
|
|
With hypertonicity can changes in body position affect tone? |
Yes |
|
|
What are treatments for hypertonicity?
|
1) work to inhibit reflex activity, 2) inhibition techniques, 3) reciprocal inhibition
|
|
|
How can a PT assist to inhibit reflex activity in a patient with hypertonicity?
|
through the following: 1) postures, 2) positions, 3) techniques of relaxation training |
|
|
What are some inhibition techniques that are used as treatments for hypertonicity? |
1) prolonged static muscle stretch, 2) inhibitory casting, 3) slow repetitive rocking or rolling, 4) very low frequency vibration, 5) reflex inhibiting postures, 6) limb movements emphasizing rotation, 7) slow stroking, 8) neutral warmth, 9) prolonged icing, 10) deep pressure to tendons |
|
|
Reciprocal inhibition: |
using facilitation techniques to the non-spastic muscles will cause inhibition of the spastic muscles
|
|
|
Why do gait problems occur following a stroke? |
1) due to sensation impairments, 2) due to perception impairments, 3) due to motor control impairments |
|
|
What are some common gait problems at the TRUNK-PELVIS following a stroke when the patient is in stance phase?
|
1) unawareness of affected side due to poor proprioception, 2) forward trunk from weak hip flexion or extension contracture |
|
|
What are some common gait problems at the HIP following a stroke when the patient is in stance phase?
|
1) poor hip position (typically adduction or flexion) as a result of poor proprioception, 2) Trendelenburg gait due to weak abductors on contralateral side, 3) scissoring as a result of spastic adductors. |
|
|
What are some common gait problems at the KNEE following a stroke when the patient is in stance phase?
|
1) flexion during forward progression from a flexion contracture combined with weak knee extensors and/or poor proprioception, 2) hyper extension during forward progression do the plantarflexion contracture past 90° or severe spasticity in quadriceps or weak knee extensors (compensatory locking of the knee) |
|
|
What are some common gait problems at the ANKLE-FOOT following a stroke when the patient is in stance phase? |
1) Equinus gait (heel does not touch the ground) from spasticity or contractures of gastroc-soleus, 2) unequal step length due to hammertoes caused by spastic toe flexors |
|
|
What are some common gait problems at the TRUNK-PELVIS following a stroke when the patient is in swing phase? |
1)insufficient forward pelvic rotation from weak abdominal muscles, 2) inclination to sound side for foot clearance because of weakness of hip flexor muscles |
|
|
What are some common gait problems at the HIP following a stroke when the patient is in swing phase? |
1)inadequate flexion from weak hip flexors, 2) poor proprioception, 3) spastic quadriceps, 4) hip abductor weakness of opposite side, 5) exaggerated hip flexion due to strong flexor synergy |
|
|
What are some common gait problems at the KNEE following a stroke when the patient is in swing phase? |
1)inadequate knee flexion from spastic quadriceps or reduced hip flexion, 2) exaggerated but delayed knee flexion because of strong flexor synergy, 3) inadequate knee extension at weight acceptance due to spastic hamstrings or sustained total flexor pattern |
|
|
What are some common gait problems at the ANKLE-FOOT following a stroke when the patient is in swing phase?
|
1)persistent equinovarus from plantarflexor contracture or spasticity, weak dorsiflexors, delayed contraction of dorsiflexors (toe drag during midswing), 2) Varus position of foot from spastic anterior tibialis, weak peroneals, and toe extensors, 3) exaggerated dorsiflexion due to strong flexor synergy pattern |
|
|
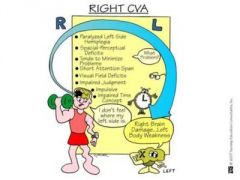
Perceptual problems associated with right hemisphere stroke or damage to the brain: |
left hemiparesis, 1) problems with spatial relationships and hand eye coordination, 2) irritability, short attention span, 3) cannot retain information, difficulty learning individual steps, 4) poor judgment affecting personal safety, 5) diminished body image with left-sided neglect, 6) quick and impulsive |
|
|
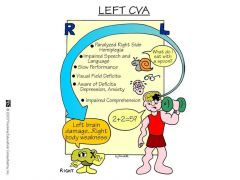
Perceptual problems associated with left hemisphere stroke or damage to the brain:
|
right hemiparesis, 1) apraxia, 2) difficulty starting and sequencing tasks, 3) perseveration, 4) easily frustrated with high levels of anxiety, 5) inability to communicate verbally, 6) cautious and slow |
|
|
Functional considerations regarding MOBILITY ACTIVITIES following a stroke:
|
1) initially, focus on using both sides of the body (compensatory training approach), 2) provide guided or active assistive movement (augmented feedback) early in the rehabilitation process, 3) focus on rolling, sitting up, bridging, sitting, standing, and transfers, 4) upright activities should focus on control in both sitting and standing. |
|
|
Upright activities per individual following a stroke should follow what progression? |
1) holding a posture (stability), 2) moving in a posture (controllability), and 3) dynamic challenges to balance (example in sitting, initially maintain proper pelvic alignment) |
|
|
How should transfers be taught to patients following a stroke? |
To both sides to promote reeducation and reintegration of the two sides of the body |
|
|
What are some respiratory activities for a patient following a stroke? |
1) improve chest expansion, 2) stress diaphragmatic breathing and combine respiratory activities with movement patterns, 3) avoid Valsalva maneuver |
|
|
How can one improve chest expansion following a stroke? |
With the use of manual contacts, resistance, and stretch to chest wall segments |
|
|
How can one combine respiratory activities with movement patterns in a patient (following a stroke)? |
Inspiration with PNF reverse chop and expiration with chop |
|
|
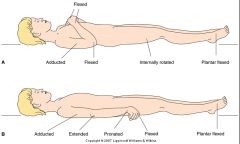
Visualize Decerebrate vs Decorticate Posturing/Synergies and then look at the picture in the answer to see if you were right |
|
|
|
On the other side of this card is a visual to help you remember how a patient with a R sided stroke may present |
|
|
|
On the other side of this card is a visual to help you remember how a patient with a L sided stroke may present |
|
|
|
Oromotor activities following a stroke: describe appropriate posture for a patient following CVA.
|
Establish a right sitting posture with hips well back, symmetrical weight-bearing, and feet flat on the floor
|
|
|
Oromotor activities following a stroke:describe appropriate head position for a patient following CVA. |
Head in normal position, not extended or tipped back, to avoid aspiration or choking, and promote normal swallowing. |
|
|
Oromotor activities following a stroke: initially following a CVA how should food be prepared for a patient? |
initially semi moist then progressing to foods rich in taste, smell, and texture to aid in swallowing
|
|
|
Oromotor activities following a stroke: how can patients be assisted using facilitation techniques?
|
With jaw closure, lip closure, or tongue control using facilitation techniques (examples: quick ice, quick stretch, or resistance)
|
|
|
Oromotor activities following a stroke: what can stimulate the posterior elevation of the tongue for swallowing?
|
Firm pressure applied to the anterior third of the tongue
|
|
|
Oromotor activities following a stroke: what can stimulate sucking?
|
Deep pressure to the neck above the thyroid notch
|
|
|
What is the best way to communicate with a patient with receptive aphasia?
|
Use word repetition and manual cues
|
|
|
What is the best way to communicate with a patient with expressive aphasia? |
Phrase questions for simple yes or no responses to avoid confusion and frustration
|
|
|
What is the best way to communicate to a patient with global aphasia?
|
Uses symbolic gestures to reduce the chance of overestimating the patient's ability to understand speech
|
|
|
Rancho Los Amigos levels of cognitive functioning:
|
A descriptive scale of response to stimuli that is useful for communicating or documenting general cognitive and/or behavioral status of a patient with a TBI |
|
|
Typical presentation of a patient at Ranchos Los Amigos Level 1:
|
no response; completely unresponsive to any stimuli |
|
|
Typical presentation of a patient at Ranchos Los Amigos Level 2:
|
Generalized response: patient reacts inconsistently and non-specifically to stimuli |
|
|
Typical presentation of a patient at Ranchos Los Amigos Level 3:
|
Localized response; patient reacts inconsistently but specifically to stimuli
|
|
|
Typical presentation of a patient at Ranchos Los Amigos Level 4:
|
confused-agitated; patient is in a heightened state of activity; behavior is bazaar and non-purposeful relative to the immediate environment; recall an attention span are poor |
|
|
Typical presentation of a patient at Ranchos Los Amigos Level 5:
|
confused -inappropriate; patient is able to respond to simple commands but not do complex tasks; memory is impaired; verbalization is inappropriate
|
|
|
Typical presentation of a patient at Ranchos Los Amigos Level 6:
|
confused-appropriate; patient is dependent upon external input but can perform consistently; memory improved
|
|
|
Typical presentation of a patient at Ranchos Los Amigos Level 7:
|
automatic – appropriate; can perform automatically and appropriately in structured environments; judgment remains impaired |
|
|
Typical presentation of a patient at Ranchos Los Amigos Level 8:
|
purposeful – appropriate; patient ask appropriately though not perfect; may have some problems in stressful or unusual circumstances |
|
|
Glasgow Coma scale:
|
Objective way to describe the patient's level of consciousness
|
|
|
What are the subcategories within each category of the Glasgow coma scale quantified with? |
1) eye-opening – spontaneous to none, 2) best motor response – follows commands to abnormal responses to no response, 3) verbal response – oriented to inappropriate to no response |
|
|
What score on the Glasgow Coma scale is indicative of severe brain injury? |
8 or less
|
|
|
Arousal: |
the overall level of alertness or reaction to stimulus |
|
|
What is low arousal associated with? |
coma
|
|
|
High arousal may occur during which state following a TBI?
|
The agitated state
|
|
|
What may help patients in a high state of arousal (with regard to daily routine)?
|
A quiet environment and consistency in management
|
|
|
What behavioral difficulties may interfere with therapy and persist over time in a patient with a TBI? What are the characteristics of these behaviors? |
1) depression: crying, apathetic, poor self-care, 2) dependent: childlike, follows therapist around, 3) denial: blames others for problems or lack of progress; may not go to treatment, 4) aggressive; physically abusive or verbal obscenities, 5) sexually appropriate: verbally or physically, 6) agitated: the frustration tolerance, combative, impatient, 7) poor judgment: regarding actions and behaviors |
|
|
Treatment strategies for behavioral problems when working with the patient status post TBI:
|
1) use a calm voice, perhaps a reassuring touch, 2) if patient becomes disruptive, redirect patient away from frustrating experiences, 3) set limits on behavior and give positive feedback, 4) offer treatment choices to patient and to give greater patient responsibilities to increase self-esteem, 5) remove patient from treatment environment ("timeout") only in the patient becomes overstimulated and strikes out at the therapist, 6) avoid surprises; keep therapist and schedule consistent,7) keep verbal instructions and descriptions to a minimum, 8) practice should follow right after demonstration of the activity, 9) use a memory log with key information (address, phone number, apartment floor, etc.) if the patient demonstrates memory loss; patient can carry it or attach it to clothing when leaving the home, 10) it may take up to a year or more before a patient with a TBI achieves maximal functional return |
|
|
Name a strategy to use of the patient becomes disruptive
|
redirect patient away from frustrating experiences
|
|
|
What does offering treatment choices to patients and giving them greater responsibilities produce?
|
increased self-esteem
|
|
|
When should you remove the patient from the treatment environment (timeout)?
|
Only the patient becomes overstimulated and strikes out of the therapist
|
|
|
How can you avoid surprises when working with the patient status post TBI?
|
Keep therapist and schedule consistent
|
|
|
What is the best way to communicate with the patient experiencing behavioral problems status post TBI?
|
Keep verbal instructions and descriptions to minimum
|
|
|
What should follow right after the demonstration of an activity?
|
Practice
|
|
|
What can help with the patient demonstrates memory loss?
|
Using a memory log with key information
|
|
|
Amyotrophic lateral sclerosis a.k.a. Lou Gehrig's disease:
|
a degenerative disease that involves both upper and lower motor neuron; cranial nerves may be affected as well
|
|
|
What are signs and symptoms of ALS? |
1) muscle weakness is progressive and can affect muscles of respiration, 2) weakness may appear in hands first 3) dysarthria and dysphasia (difficulty swallowing), 4) muscle atrophy, cramping, and fasciculations (LMN signs), 5) spasticity and hyperreflexia (UMN signs), 6) often no sensory changes |
|
|
What type of motor neuron sign includes muscle atrophy, cramping, and fasciculations?
|
Lower motor neuron (LMN)
|
|
|
What type of motor neurons fine includes spasticity and hyperreflexia?
|
Upper motor neuron (UMN) |
|
|
What are some treatments that are used with patients who have ALS?
|
1) maintain respiratory function and activity level, 2) PROM exercises, 3) positioning and skincare, 4) prevent further deconditioning and disuse atrophy and, 5) avoid overworking muscles and teach energy conservation, 6) symptomatic treatment of pain, spasm, and spasticity, 7) provide psychological support and reassurance |
|
|
Bells palsy:
|
An inflammatory response resulting in paralysis of the muscles of facial expression |
|
|
What nerve is affected in Bells palsy?
|
Facial nerve (CN 7); the branch of CN 7 affected will dictate symptoms
|
|
|
How will a patient with bells palsy present? |
The patient may have difficulty in wrinkling forehead, closing the eye tightly, and smiling; Signs and symptoms may vary depending on the branch of the nerve involved but may include loss of control of salvation, one sided facial muscle weakness or paralysis, or normal sensation; the mouth may droop and the patient may have decreased taste sensation with the anterior two thirds of the tongue |
|
|
What are possible treatments for bells palsy? |
1) artificial tears or temporary patch and protects the cornea, 2) Electrical stimulation to maintain tone and support function of facial muscles, 3) teach facial muscle exercises, 4) provide functional retraining (chewing on the opposite side) |
|
|
Guillain-Barré syndrome – GBS: |
polyneuropathy of probable immune-mediated viral origin, resulting in the metric motor paralysis and progressive muscular weakness that develops quickly |
|
|
What are signs and symptoms of Guillain-Barré syndrome? |
1) LMN disease affecting the cranial and peripheral nerves, 2) some sensory loss in stocking glove pattern and parenthesis including tingling and burning, 3) muscle weakness and atrophy progressing from lower extremities to upper and from distal to proximal, 4) may produce full tetraplegia with respiratory failure, 5) tachycardia, and abnormalities in cardiac rhythm, and blood pressure changes, 6) recovery is slow (up to one year) with some mild weakness persisting and a 3% mortality |
|
|
What type of motor neuron disease is Guillain-Barré syndrome? |
Lower motor neuron disease affecting the cranial and peripheral nerves |
|
|
In Guillain-Barré syndrome, what pattern does sensory loss occur?
|
In a glove and stocking pattern
|
|
|
When a patient experiences Guillain-Barré syndrome which muscles we can and atrophy first?
|
Lower extremities first then upper; distal to proximal
|
|
|
What vital sign changes may occur in a patient with Guillain-Barré syndrome? |
1) tachycardia, 2) abnormalities in cardiac rhythm, 3) blood pressure changes
|
|
|
How is treatment administered to the patient with Guillain-Barré syndrome? |
It is based on the phase of the syndrome
|
|
|
During the ascending phase (disease progressing) of Guillain-Barré syndrome, what treatment is provided? |
1) Respiratory function (pulmonary PT), 2) PROM within tolerance, 3) positioning to reduce contractures, 4) skin care to prevent breakdown |
|
|
During the stabilization phase of Guillain-Barré syndrome, what treatment is provided to the patient?
|
1) Prevention of injury to denervated muscles, 2) avoiding overused and fatigue, 3) beginning gentle stretching and initiating movement in a controlled environment
|
|
|
During the descending phase (paralysis slowly recedes) of Guillain-Barré syndrome what treatment is provided? |
1) muscle re-education with a moderate exercise program, 2) improve cardiovascular fitness, 3) teach energy conservation |
|
|
What type of disease is multiple sclerosis – MS?
|
a demyelinating disease |
|
|
In what climate is multiple sclerosis more prevalent? |
colder climates |
|
|
How does multiple sclerosis progress? |
The disease may be relatively mild, have bouts of remission and exacerbation, or get progressively worse
|
|
|
What are signs and symptoms of multiple sclerosis? |
1) sensory disturbances including tingling, numbness, and pain, 2) coordination problems and spasticity, 3) fatigue (especially in the afternoon), 4) diplopia, 5) bowel and bladder problems, 6) communication disorders, 7) psychosocial problems including euphoria and or depression, 8) adverse reactions to heat (caution with heating modalities and hot environment) |
|
|
What type of sensory disturbances might an individual with multiple sclerosis experience? |
1) tingling, 2) numbness, 3) pain
|
|
|
In a patient with multiple sclerosis what might over vigorous exercise or activity cause? |
Fatigue that may worsen symptoms
|
|
|
What time of day our sessions preferred for a patient with multiple sclerosis? |
Morning treatment sessions
|
|
|
What type of disease is Parkinson's disease and what is affected? |
It's a progressive disease affecting the basal ganglia
|
|
|
What neurotransmitter or receptor is decreased in a patient with Parkinson's these?
|
Dopamine production and or dopamine receptors in the brain or decreased
|
|
|
What are signs and symptoms of Parkinson's disease?
|
1) tremor, rigidity, and fatigue, 2) difficulty initiating or slowness of movement (bradykinesia), 3) abnormal gait (festinating or slow shuffling), 4) flexed posture, 5) mask-like face, 6) decreased postural reflexes, 7) behavioral changes including memory loss or apathy that can lead to secondary problem including decubitus ulcer's, muscle atrophy, contractures, decreased vital capacity, and falls |
|
|
What type of movements and gait do patients with Parkinson's typically present with? |
difficulty initiating movement, bradykinesia, and a festinating or slow shuffling gait
|
|
|
What type of posture do patients with Parkinson's disease tend to present with? |
Flexed posture
|
|
|
What are PT treatments for patients with Parkinson's disease? |
Gait training to increased stride width and length, 2) breathing exercises, 3) relaxation techniques (examples: gentle rhythmic rocking, vestibular stimulation, and prone on a large ball), 4) mobility exercises, 5) PNF diagonals with rhythmic initiation to overcome bradykinesia, 6) range of motion activities including PNF contract – relax, inhibitory casting, or orthoses, 7) avoid excessive exercise or stretching; pain or lack of endurance could lead to fatigue |
|
|
What type of relaxation techniques might be used for a patient with Parkinson's disease? |
1) gentle rhythmic rocking, 2) vestibular stimulation, 3) prone on a large ball |
|
|
What activity may overcome bradykinesia in a patient with Parkinson's disease? |
PNF diagonals with rhythmic initiation
|
|
|
What type of range of motion activities might be implemented for a patient that has Parkinson's disease? |
1) PNF contract – relax, 2) inhibitory casting, 3) orthoses
|
|
|
Why would you want to avoid excessive exercise or stretching with the patient that has Parkinson's disease?
|
Pain or lack of endurance could lead to fatigue |
|
|
What artery would a lesion affect if the patient presented with unilateral deafness, loss of pain and temperature on the contralateral side, paresis of lateral gaze, unilateral Horner's syndrome (ptosis, constricted pupils, and loss of sweating), plus ataxia, vertigo, and nystagmus?
|
anterior inferior cerebral artery AICA
|
|
|
What artery would a lesion affect if the patient presented with severe ataxia, dysarthria (loss of muscle articulation control), dysmetria (finger to nose test), and contralateral loss of pain and temperature? |
Superior cerebellar artery
|
|
|
What does the patient with Wallenberg's syndrome present with? |
Vertigo, nausea, hoarseness, dysphasia, ptosis, and decreased impairment of sensation and ipsilateral face and contralateral torso and limbs. |
|
|
What artery would a lesion affect if the patient presented with Wallenberg's syndrome and possibly Horner's syndrome? |
Posterior inferior cerebellar artery PICA |
|
|
Dopamine agonist medications may be used for what?
|
Tremor and Brady can Ezio in patients with Parkinson's disease.
|
|
|
Dopamine agonist medications I do what overtime?
|
Lose their effectiveness
|
|
|
What time of day is it best to treat patients following dopamine agonist administration?
|
In the a.m. after they have had their medication
|
|
|
Post polio syndrome:
|
a new form of muscular dystrophy that may occur decades after the initial episode of polio
|
|
|
With post polio syndrome how does new denervation occur?
|
With asymmetrical muscular weakness
|
|
|
What are signs and symptoms of post polio syndrome?
|
1) myalgia, 2) joint pain, 3) variable asymmetrical muscle atrophy with decreased strength, 4) excessive fatigue and decreased endurance which contribute to loss of function
|
|
|
What are possible treatments for post polio syndrome?
|
1) low intensity exercise never to the point of fatigue (stop exercise with pain or weakness), 2) use orthotic device as needed to improve function, 3) work on endurance and energy conservation techniques
|
|
|
What are some presentations of Charcot Marie tooth disease?
|
1) stored like deformity, 2) footdrop, 3)distal lower extremity muscle weakness |
|
|
Pain syndromes: neuropathic –
|
pain as a result of lesions in some part of the nervous system
|
|
|
What is neuropathic pain usually accompanied by?
|
Some degree of sensory deficit
|
|
|
What type of pain is Thalamic pain?
|
Neuropathic
|
|
|
How does someone with Thalamic pain present?
|
With continuous, intense pain occurring on the contralateral hemiplegic side
|
|
|
What is Thalamic pain the result of?
|
Stroke involving the posterior cerebral artery – PCA
|
|
|
What type of pain is complex regional pain syndrome?
|
Neuropathic
|
|
|
What is complex regional pain syndrome formally referred to as?
|
Reflex sympathetic dystrophy
|
|
|
What is nervous system is complex regional pain syndrome maintained by?
|
the sympathetic nervous system
|
|
|
How would a patient with complex regional pain syndrome present?
|
1) burning pain (causalgia), 2) hypersensitivity to light touch, 3) coldness, 4) sweating
|
|
|
What is complex regional pain syndrome usually associated with?
|
Traumatic injury |
|
|
What are selected neuropathic techniques?
|
Treatment strategies for patients with neurological dysfunction which include neuromuscular facilitation, sensory stimulation, and exercises designed to reduce impairments and improve function of involved body segments
|
|
|
Proprioceptive neuromuscular facilitation – PNF:
|
uses total patterns of movement and posture to promote motor learning in synergistic muscle patterns and prepare the body for advanced and I'll skills (for example – date)
|
|
|
PNF diagonal D1 Flexion upper extremity:
|
Starts with glenohumeral medial rotation, abduction and extension then goes to lateral rotation, adduction and flexion
|
|
|
PNF diagonal D1 Flexion lower extremity:
|
Starts with his medial rotation, abduction and extension then goes to lateral rotation, adduction and flexion
|
|
|
PNF diagonal D2 Flexion upper extremity:
|
starts with glenohumeral medial rotation, adduction and extension then goes to lateral rotation, abduction and flexion
|
|
|
PNF diagonal D2 Flexion lower extremity:
|
starts with hip lateral rotation adduction and extension then goes to medial rotation, abduction and flexion |
|
|
What might diagonal patterns of the head and trunk be used for? |
To enhance breathing and movement patterns
|
|
|
What PNF activity the silicate rolling to prone position?
|
supine or sitting chopping
|
|
|
How is supine or sitting chopping performed?
|
Upper trunk flexion with rotation and upper extremity D1 extension (facilitates rolling to prone position)
|
|
|
What is another supine PNF pattern that can be used to enhance breathing and moving?
|
Supine lower trunk flexion with rotation to right or left; needs flexing |
|
|
What does lower extremity D1 flexion help with?
|
Rolling in any direction
|
|
|
Approximation:
|
joint compression
|
|
|
What is approximation used for (think PNF)?
|
to stimulate afferent nerve endings and facilitate postural extensors promoting stability
|
|
|
Agonist reversals (AR):
|
Slow isotonic shortening contractions through the range followed by eccentric lengthening contractions with the same muscle group
|
|
|
What are agonist reversals used for? |
Weak postural muscles, inability to eccentrically control body weight during movement transitions (example – sitting down) |
|
|
Contract – relax (CR):
|
isotonic movement in rotation followed by an isometric hold of the range limiting muscles in the antagonistic pattern against slowly increasing resistance, then passive motion and active contraction of the agonistic pattern
|
|
|
When is contract– relax indicated?
|
with limited range of motion caused by muscle tightness or spasticity
|
|
|
Hold – relax (HR):
|
isometric contraction of the antagonistic happen against slowly increasing resistance, followed by voluntary relaxation and passive movement into the newly gained range of the agonist pattern.
|
|
|
Hold – relax active contraction (HRAC):
|
Active contraction of the agonist performed which relaxes the antagonist through receptacle inhibition
|
|
|
When is hold – relax and hold – relax active contraction indicated?
|
With limitations in range of motion due to muscle tightness, spasm, or pain
|
|
|
Repeated contractions (RC):
|
repeated isotonic contractions induced by quick stretches and enhanced by resistance performed through the range or part of range at a point of weakness
|
|
|
When should it repeated contractions be used?
|
With 1) weakness, 2) incoordination, 3) muscle imbalances, and 4) lack of endurance
|
|
|
Rhythmic initiation (RI):
|
voluntary relaxation followed by passive movement through increasing our ROM, followed by active – assisted contractions progressing to resisted isotonic contractions
|
|
|
When is rhythmic initiation indicated?
|
With 1) spasticity, 2) rigidity, 3) hypertonicity and the inability to initiate motion (apraxia), 4) Motor learning deficits, 5) communication deficits (aphasia)
|
|
|
Rhythmic stabilization (RS):
|
simultaneous isometric contractions of both agonistic and and agonistic patterns performed without relaxation using careful grading of resistance |
|
|
Co-contraction of opposing muscle groups is part of what type of PNF?
|
rhythmic stabilization
|
|
|
When is rhythmic stabilization indicated?
|
1) Instability in weight-bearing and holding, 2) poor antigravity control, 3) weakness, 4) ataxia, 5) limited range of motion caused by muscle tightness, 6) painful muscle splinting
|
|
|
Slow reversal (SR) and slow reversal hold (SRH):
|
Alternating isotonic contractions of agonist and antagonist patterns using careful grading of resistance and optimal facilitation.
|
|
|
What is the difference between slow reversal hold and slow reversal?
|
In SRH, an isometric hold is added at the end of the range at a point of weakness
|
|
|
When is slow reversal and slow reversal hold indicated?
|
1) Inability to reverse directions, 2) muscle weakness or imbalance, 3) incoordination, 4) lack of endurance
|
|
|
Traction:
|
separation of joint surfaces
|
|
|
When is traction indicated?
|
1) facilitates flexor muscles and 2) mobilizing patterns
|
|
|
Exteroceptive stimulation:
|
facilitation techniques applied to the antagonist to inhibit the agonist via reciprocal inhibition |
|
|
Name some Exteroceptive stimulation FACILITATION techniques and what they are used for
|
1) repetitive brushing– Facilitates tactile receptors and movement responses, 2) Quick icing – for muscles, 3) quick stretch or tapping – agonist tendon or muscle belly is stimulated, 4) high-frequency vibration – 50 to 300 Hz to agonist
|
|
|
Name some Exteroceptive stimulation INHIBITION techniques and what they are used for
|
1) prolonged icing – inhibits muscle, 2) neutral want – relaxation by wrapping patient in towels or blankets to decreased postural tone, 3) prolonged stretch – muscle tone decrease, 4) low frequency vibration – 5 to 50 Hz inhibition of agonist, 5) pressure on tendons – firm, constant pressure may decrease tone
|
|
|
What are some examples of the vestibular stimulation and what are the effects?
|
1) Slow rocking, rolling on ball– Inhibits postural tone and has a calming effect, 2) fast spinning – the silicates postural tone and promote head writing, 3) head down position, prone over large ball– can activate postural extensors of neck, trunk, and proximal joint – has a soothing effect especially for sympathetic responses
|
|
|
Neurodevelopmental treatment – NDT, Bobath:
|
The idea that motor learning (or relearning) can be facilitated by repetition and experience in the environment |
|
|
What does NDT inhibit?
|
Unwanted activity precedes practice of normal motor patterns (for example abnormal tone or reflex patterns) |
|
|
Guided movement falls under what type or category of treatment?
|
NDT
|
|
|
Guided movement:
|
active movements that are guided or assisted only when needed
|
|
|
When (at what point) is guided movement used in the rehabilitation process?
|
Early in the rehabilitation process
|
|
|
Normalization of postural tone includes what?
|
1) efforts are made to increased tone if hypotonic or decrease tone if hypertonic, 2) abnormal patterns of movement and reflexes are inhibited or prevented
|
|
|
Normalization of sensory or perceptual experiences falls under what type or category of treatment?
|
NDT
|
|
|
What is normalization of sensory or perceptual experiences?
|
Resumption of normal functioning activities that are meaningful, goal oriented (for example rolling, sitting up, standing, walking)
|
|
|
Asymmetrical tonic neck reflex- describe the following for this reflex: 1) stimulus, 2) response, 3) strongest influence, 4) prolonged influence result, 5) results if the reflexes severe, 6) onset, 7) typical time of integration
|
1) rotation of the head to one side, 2) flexion of the skull limbs, extension of the jaw limbs, "fencing posture", 3) strongest influence in the supine are sitting position, 4) along to influence can result in scoliosis or even hit subluxation or dislocation if there is marked hypotonia, 5) if the reflex is severe, grasping of objects with the extended arm is only possible if the patient looks away from the object to lessen the reflex influence, 6) onset birth, 7) integrated at 4–6 months |
|
|
Crossed extension reflex –describe the following for this reflex: 1) stimulus, 2) test position 3) response, 4) effect when coupled with another reaction, 5) onset, 6) typical time of integration
|
1) noxious stimulus to the ball of foot of extremity fixed and extension, 2) tested in supine position, 3) opposite lower extremity flexes, then adducts and extends; inpatient with hemiplegia, lifting the uninvolved leg off the ground during ambulation results in increased extensor tone in the involved leg, 4) this reflex, when coupled with the "positive supporting reaction", can result in hyper extension of the knee, 5) onset 28 weeks gestation, 6) integrated 1 to 2 months
|
|
|
Equilibrium reactions – describe the following for this reaction: numeral one) stimulus, 2) response, 3 onset, 4) typical time of integration
|
1) displace the center of gravity by tilting or moving the support surface (for example with an equilibrium board or ball), 2) curvature of the trunk tour the afford side along with extension and abduction of the extremities on that side, protective extension on the opposite (downward) side, and the equilibrium reaction will be absent if there is marked spasticity, 3) onset approximately 6 months of age and develop sequentially in prone (six months), then into pine (7 to 8 months) and then and sitting (7 to 8 months), kneeling in front of the 9 to 12 months) and a standing (12 to 21 months), 4) it is not integrated, but rather persists.
|
|
|
Grasp reflex – describe the following for this reflex: 1) stimulus, 2) response, 3) onset, 4) typical time of integration
|
1) maintain pressure to palm of hand (Palmer) or ball of foot under toes (plantar), 2) maintain flexion of fingers or toes, 3) onset – Palmer at birth; plantar at 28 weeks gestation, 4) integrated – Palmer 4 to 6 months; plantar 9 months |
|
|
Name two disorders of peripheral roots and nerves?
|
1) neuralgia – pain along a nerve, 2) radiculalgia - neuralgia of nerve roots
|
|
|
What type of pain syndrome is herpes zoster?
|
Neuropathic
|
|
|
What type of pain syndrome is phantom limb?
|
Neuropathic
|
|
|
Phantom limb pain:
|
Pain in the residual limb following amputation
|
|
|
What type of pain syndrome is fibromyalgia?
|
Musculoskeletal
|
|
|
How would a patient with fibromyalgia present?
|
With widespread pain accompanied by tenderness of muscles and adjacent soft tissue
|
|
|
What is the origin of fibromyalgia?
|
Non-articular rheumatic disease of unknown origin
|
|
|
What type of pain syndrome is myofascial pain syndrome – MPS?
|
Musculoskeletal
|
|
|
How would a patient with myofascial pain syndrome present?
|
persistent, deep aching pains in muscle
|
|
|
What is myofascial pain syndrome characterized by?
|
Well-defined, highly sensitive tender spots (triggerpoints)
|
|
|
Referred pain:
|
starts in the deep visceral tissues and is felt in a body region remote from the site of pathology, resulting in tenderness and pain in superficial locations
|
|
|
Referred pain presenting in the medial left arm and jaw pain may be associated with what?
|
Heart attack
|
|
|
Referred pain presenting in the right subscapular area may be associated with what?
|
A Gallbladder attack
|
|
|
Referred pain presenting in the thoracic area or flank pain maybe associate with what?
|
Kidney problems
|
|
|
Referred pain presenting in the left upper quadrant and shoulder pain may be associated with what?
|
Spleen damage
|
|
|
Referred pain presenting in the right upper quadrant may be associated with what?
|
Liver problems
|
|
|
What are some goals and interventions when working with a patient with neuropathic, musculoskeletal, or referred pain? |
1) Assist the patient and identifying pain behaviors, 2) teach coping skills, 3) provide relaxation training, 4) provide direct pain – symptom control (time-limited), 5) establish a realistic daily exercise program |

