![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
46 Cards in this Set
- Front
- Back
|
name 3 effects of progesterone in pregnancy
|
1) endometrium - secretory changes
2) breasts - tender/sore 3) GIT - nausea/vomiting/constipation |
|
|
name symptoms of pregnancy. what are most of these due to?
|
nausea
constipation lethargy breast tenderness haemorrhoids varicose veins oedema backache flushes due to progesterone |
|
|
when is hCG detectable in pregnancy?
|
within 6-7 days after fertilisation
|
|
|
when does the placenta take over endocrine function from the corpus luteum?
|
after 1st trimester
|
|
|
Outline maternal cardiovascular changes in pregnancy
|
- maternal vascular-neogenesis, accommodated by changes in function of baro- & volume receptors
- increased blood flow to breasts, kidneys & GIT (increased metabolism) - plasma volume increases - TPR falls (vasodilation) - increased CO 40% by term due to increased stroke volume - mean BP remains the same, rises towards term - HR increases 15% |
|
|
explain what the increased stroke volume in pregnancy is due to (3)
|
- increase in ventricular wall muscle mass
- increased end-diastolic volume - heart physiologically dilated with increased contractility |
|
|
How is mean BP maintained during pregnancy?
|
increased SV increases systolic BP
but increased flow into additional tissue reduces the diastolic BP maintains mean BP |
|
|
What changes in a pregnant woman's heart might be apparent on examination?
|
upward displacement
mild hypertrophy flow murmers |
|
|
Describe supine hypotension in pregnancy & how can it be avoided?
|
aortocaval compression by gravid uterus
reduces venous return reduces CO reduces BP use a left lateral position or wedge/tilt |
|
|
What cardiovascular changes occur during labour?
|
- further increase in CO
- contractions lead to autotransfusion of blood back into the circulation - sympathetic response to pain increase HR & BP - CO increased during & between contractions |
|
|
What cardiovascular changes occur after delivery?
|
immediate rise in BP due to alleviation of IVC compression & contraction of uterus
CO increases 80% back to non-pregnant levels within an hour |
|
|
Describe BP changes in pregnancy
|
1st half: reduced diastolic, little change systolic - wider pulse pressure
2nd half: changes reverse BP falls from end of first trimester (fall in TPR) but rises in late pregnancy |
|
|
Summary of cardiac changes table
|
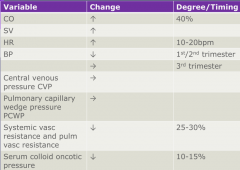
|
|
|
What would make you suspect pre-eclampsia?
|
high BP
proteinuria oedema can lead to eclampsia = seizures |
|
|
what is the threshold BP for hypertension in pregnancy?
|
140/90
|
|
|
What tests might indicate pre-eclampsia?
|
24 hour urine protein - proteins
platelets - low urinanalysis - urate indicates renal dysfunction liver function tests |
|
|
what should be done if pre-eclampsia is suspected?
|
IV hydralazine (vasodilator, reduces BP)
IV magnesium sulphate (reduces cerebral irritability, vasospasm & prevents fits) emergency C-section (only cure is to remove baby) |
|
|
name underlying conditions which may lead to pre-eclampsia?
|
essential hypertension
underlying renal diseases (associated with proteinuria) phaeochromocytoma (tumour of adrenal medulla) |
|
|
name & explain iron deficiency anaemia experienced in pregnancy
|
- foetus requires high nutrition flow in 2nd trimester
- discrepancy between plasma vol expansion & red cell mass expansion - maternal Hb levels fall = dilutional/physiological anaemia - 1g of iron is needed in pregnancy - eventually higher Hb flow is required by foetus & erythropoietin stimulation increases red cell mass |
|
|
Except increasing nutritional/O2 demand from the foetus, how else is iron turnover changed in pregnancy?
|
menstrual losses have stopped
|
|
|
How will smoking affect O2 flow to the foetus & by what mechanism
|
carbon monoxide in maternal blood flow
Hb-O2 curve shifts left = Bohr shift foetus suffers reduced pO2 in extracting its O2 requirement, which may not be fulfilled |
|
|
how may mean arterial BP change in pregnancy & what symptoms might the mother experience?
|
- rising progesterone levels causes peripheral vasodilation
- reduces TPR - compensated by increased CO symptoms: hot flushes, sweat, nasal congestion |
|
|
What 3 factors contribute to venous distension & engorgement in late pregnancy?
|
- smooth muscle relaxation due to progesterone
- raised circulating blood volume & low resistance to flow through the foetal-placental unit create high venous pressure - mechanical pressure from the uterus compresses the IVC, which may increase lower limb venous pressure, but only when mother is supine |
|
|
what are 2 long-term sequelae attributed to venous distension & engorgement in late pregnancy?
|
varicose veins
haemorrhoids |
|
|
what happens to resp rate, tidal volume & oxygen uptake in pregnancy?
|
RR - little change
tidal vol & O2 uptake increase |
|
|
why might dyspnoea be experienced in pregnancy?
|
- increased awareness of desire to breathe
- increase in tidal volume lowers the pCO2 - blood shunted away from functioning alveoli Increased resp effort & reduction in pCO2 induced by progesterone acting directly on the resp centre & sensitising chemoreceptors to CO2 changes |
|
|
what happens to the minute ventilation in pregnancy?
|
increases 40-50%, mainly due to increase in tidal vol as RR remains essentially unchanged
|
|
|
what anatomical/mechanical effect will the expanding uterus have on the resp system?
|
diaphragm rises & intercostal angle widens to due uterus exerting a mechanical limitation to inspiration
- reduced functional residual capacity - no change in vital capacity: FEV1 & peak flow are unchanged |
|
|
how much will the following change during pregnancy:
CO HR O2 consumption tidal volume |
CO - increases 40%
HR - increases to 80-90bpm O2 consumption - increases 15% tidal volume - increases 40% |
|
|
Describe maternal arterial blood gases in pregnancy
|
pO2 increases
pCO2 decreases 15-20% compensatory fall in serum HCO3- mildly compensation resp alkalosis - maternal pH 7.44 |
|
|
Summary of resp changes table
|
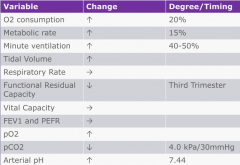
|
|
|
Describe the advantage of increased tidal volume in O2 transfer to the foetus (3)
|
Enhanced gas transfer:
- pCO2 reduced 15-20% while pO2 much the same - this is offset by increased 2.3 DPG in maternal RBCs: shifts dissociation curve to right so that maternal O2 saturation changes little - this enhances O2 transfer to foetal RBCs which have dissociation curve shifted to the left: foetal Hb much higher affinity for O2 & less sensitive to 2,3 DPG |
|
|
What happens to women with chronic respiratory diseases in pregnancy?
|
tend to deteriorate less - functional changes facilitate airflow along bronchial tree, & FEV1 & PEF don't change
in severe asthma, deterioration may be due to cessation of medicine |
|
|
Name 2 ways progesterone acts to change ventilation
|
- acts directly on respiratory centre
- increases carbonic anhydrase in maternal RBCs, so increases breakdown of CO2 & excretion of HCO3- through maternal kidneys |
|
|
What are the 2 main renal changes in pregnancy?
|
- increase in renal blood flow (GFR)
- fall in urea & uric acid in early pregnancy |
|
|
What effects might the gravid uterus have on the ureters?
|
- compresses them above the pelvic brim
- increased intraureteral tone - ureteral dilatation - hydroureter - hydronephrosis May also be caused by smooth muscle relaxation effect of progesterone. |
|
|
Explain why urinary incontinence could occur in pregnancy
|
- pressure on the bladder from enlarged uterus
- engagement of foetal head towards the end of pregnancy |
|
|
What complications are associated with multiple pregnancies?
|
- increased incidence of pregnancy-induced hypertension
- anaemia - polyhydraminos - perinatal mortality - antepartum haemorrhage |
|
|
What compensates for the increased expected sodium loss in pregnancy, due to a raised GFR?
|
increased secretion of renin, aldosterone & angiotensin II
|
|
|
what might progesterone-induced ureteric dilatation & slowed urine transport increase the risk of?
|
- UTI
- loin pain due to hydronephrosis & pyelonephritis(secondary to progesterone & mechanical obstruction of ureter by uterus) |
|
|
What are the effects of diabetes on pregnancy?
|
miscarriage
foetal malformations IUGR macrosomia unexplained IUD PET |
|
|
what are the effects of pregnancy on diabetes?
|
- poorer control
- deterioration of renal function - deterioration of ophthalmic disease - gestational diabetes mellitus |
|
|
Outline the effects of diabetes on the foetus & the increased risks (6)
|
- maternal diabetes --> hyperglycaemia
- foetal hyperinsulinaemia - increased foetal growth leads to: 1) foetal macrosomia (risks in birth) 2) polyuria -> polyhydraminos (preterm/cord prolapse) 3) increased O2 demand -> polycythaemia (stillbirth) 4) neonatal hypoglycaemia (cerebral palsy) |
|
|
Outline metabolism changes in mother in pregnancy (4)
|
- reduction in maternal blood glucose & aa concs
- maternal insulin resistance (2nd half of preg) - increase in FFAs, ketones & triglycerides (alternative metabolic fuel) - increased insulin release in response to normal meal |
|
|
How is maternal insulin resistance useful?
|
maternal glucose usage declines
gluconeogenesis increases maximal glucose availability to foetus mother metabolises peripheral fatty acids |
|
|
In early pregnancy, progesterone stimulates appetite & promotes maternal deposition of fat - how is this beneficial in late pregnancy/after birth?
|
- maternal preparation e.g breast growth
- reserve when foetus is metabolically demanding - fat (rather than glucose) is primary energy source for mother in later pregnancy |

