![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
75 Cards in this Set
- Front
- Back
|
1.1-Monteggia’s fracture vs. Galeazzi fracture |
1-GRIMUS RADIUS OUT
distal ("inferior") or proximal ("superior") part of the bone is involved. G - Galeazzi; R - radius; I - inferior; M - Monteggia; U - Ulna; S - Superior 2-Disorder of worsening neurologic dysfunction characterized by progressive muscle weakness w/ Muscle biopsy Duchenne Muscular Dystrophy (DMD) : Doesn't Make Dystrophin. vs Becker Muscular Dystrophy (BMD): Badly Made Dystrophin (a truncated protein). affects young males only=X-linked recessive 3-Friedreich's TooK 9 CCANDY T-Toes (Hammer Toes) & Trinucleotide repeat expansion of GAA :frataxin gene K-Kyphoskoliosis(abnormal curvature of the spine kyphosis and scoliosis) 9 (chromosome) C-Cavavarus a rigid hindfoot will not correct into neutral C-Cardiomyopathy, Hypertrophic A-Areflexia & Ataxia N-Nystagmus D-Dysarthria Y-spanish AND treat-cavovarus(2)-ambulatory patient=plantar release, transfers, +/- metatarsal and calcaneal osteotomy Y-nonambulatory patients=triple arthrodesis Y(&) Kyphoskoliosis curve > 60 deg, rapid progression with positive predictors of progression (see above) usually does not need to be extended to pelvis 4-“Hurlers ran around in a daze, they couldn’t see or breathe”. “When you run hard hard you hurl, you’re bent over and can’t breathe, and you take off your lid to see.” Hurler’s Syndrome – Results in developmental delay, gargolyism (bent over), airway obstruction (can’t breathe), corneal clouding (can’t see) and hepatosplenomegaly. Results to a deficiency in a-L-iduronase, accumulating heparan and dermatan sulfate. “They are aggressive hunters who see clearly and hit the x with their arrows.” Hunter’s Disease manifests with aggressive behavior, no corneal clouding, and is X-linked Recessive inherited. It’s due to a lack of iduronate sulfase, and an accumulation of heparan and dermatan sulfate. 5-Hari chiari=Chiari or shelve which are salvage procedure) 6-fem::Prox =3mm/yr & Distal =9mm/yr knee=15mm/yr tibia:::Prox =6mm/yr &Dis =5mm/yr. total=23 16 yrs= B & 14 yrs = G, 7-“that FELLER’s-DAAMN-LOOSE!” & Three-lers Danlos Syndrome (Type III collagen most frequently affected) characterized by=joint hypermobility, Skin hyperelasticity, Pathologic defect of collagen Poor wound healing, generalized ligamentous laxity, pes planus, vascular defects, high palates, gastroparesis, and mitral valve prolapse 11 types AD and AR, COL5A1 or COL5A2 mutation in 40-50% gene for type V collagen->important in proper assembly of skin matrix collagen fibrils and basement membrane, Echocardiogram cardiac evaluation with echo is mandatory in the workup, |
|
|
2.1-Marfans=
2.2-PosterioMedial bowing of tibia, mnemonic 2.3-What are the 4 Forms of myelodysplasia Horse race 2.4-Stills disease 2.5-LateraL eLbow mnemonic 2.6-mnemonic for club foot 2.7-mnemonic for CP |
2.1-MARFANS PP is Dural Ecstasy
M=Mitral valve prolapse/regurgiatation, ,megalocornea A=Arachnodactyl R=Retinal detachment, (60%), F=Fibrillin-1 (FBN1) gene A=Aortic valve disease (aortic dissection) N=Nystagmaus, Normal IQ S=Subluxation Superior lens dislocations , Scoliosis=ASF +/- PSF with instrumentation, Spider finger=arachnodactyly, PP=Protrusio acetabuli (15-25%), Pes planovalgus, Pectus excavatum, sPontaneous P neumonthoraces Patella, hyPerlaxity Dural Ecstasy=dural ectasia (>60%), meningocele, dolichostenomelia (arm span greater than height (>1.05 ratio), 2.2-PosteroMedial PM= PMP PPP Aka PBT PeriMaterial Positioning in Pregnancy that Permentaley Passes Away aka Physiologic bowing of tibia thought to be a result of intrauterine positioning usually involves middle and distal third of tibia no known genetic association 2.3--SPO/spinal bifida oculta=defect in vertebral arch w/ confined cord and meninges; 2-MENO/ meningocele= protruding sac w/out neural elements; 3-M &M/myelomeningocele= protruding sac with neural elements; 4-KISS KISIEI/rachischisis=neural elements exposed w/no covering 2.4-RHEUMATISM R Rheumatoid factor (RF) +ve in 80%/Radial deviation of wrist H HLA-DR4 associated with polyarticular; DR8, DR5, DR2.1 assoc/w pauciarticular E ESR/Extra-articular features (restrictive lung disease, subcutaneous nodules) U Ulnar deviation of fingers M Morning stiffness/MCP+PIP joint swelling A Ankylosis/Atlanto–axial joint subluxation/Autoimmune/ANA +ve in 30% 2.5-LLLLL's for Lat. eLbow fx 1L-Lateral condyle fx 2L-miLich type 1, Lateral to trochlear grove SH4 3L-Late vaLgus deformity from maLunion 4L-Late uLnar nerve tardy 5L-radiaL head & captiLLum is Lateral 6L-best xray view interaL obLique and contraLateral for comparison 7L-critoL-11 & 11 I is 17 2.6-"CinnInADDE CAVE-E.in. varus" INversion, ADduction & Equinus of the foot=congenital talipes equinovarus corrected via the Ponseti method:CAVE midfoot Cavus (tight intrinsics, FHL, FDL =>weak dorsiflexors) forefoot Adductus (tight tibialis posterior =>weak ) hindfoot Varus (tight tendoachilles, tibialis posterior=>weak peroneal brevis ) then hindfoot Equinus (tight tendoachilles=>weak peroneus brevis & longus) 2.7-SADAM PALSY POSTER : S-Spastic – increased tone, MC A-Athetoid / D-Dyskinetic – involuntary and uncontrolled movements A-Ataxic – cerebellar damage difficulty with fine motor skills and balance, similar to Diplegic Legs more than arms but usually still ambulatory. IQ may be normal (injury in brain is midline) Quadriplegic=Total body involvement and nonambulatory with a low IQ and a high mortality M-Mixed, Hemiplegic Arms and legs on one side of the body, usually with spasticity; all will eventually be able to walk, regardless of treatment PALSY: P-Paresis A-Ataxia L-Lagging motor development S-Spasticity Y-Young POSTER P - abnormal Posture: adducted thumbs-fisting with hyperextension & (scissoring) of LE, and hyperextension of trunk (arching). O - poor Oral-sucking-swallow S - Strabismus: commonly associated with CP. T - abnormal muscle Tone: increased resistance to passive movement of the extremities and decreased axial tone. E - Evolution of automatic responses: persistent palmar grasp, Moro, asymmetric tonic neck reflexes. Poor equilibrium, delayed protective response.delayed integration of primitive reflexes, delayed R - deep tendon Reflexes: brisk, with clonus. Infants with 4 or more of these findings are likely to receive the diagnosis of CP later in childhood. |
|
|
3-1The Kocher criteria for septic arthritis include fever degrees centigrade, ? bear weight,
3-2ESR> ?and 3-3WBC count>? 3-4an aspiration of < ? leukocytes per mL virtually r/o sepsis of the joint. 3-5Genu varum is abn? 3-6necrotic bone aka mnemonic 3-7outer layer of new bone is formed by the periosteum aka mnemonic |
3-1The Kocher criteria for septic arthritis include fever>38.5 degrees centigrade, inability to bear weight, 2/4 of the criteria are positive (inability to bear weight & ESR>40mm/h), which indicates approximately a 40% likelihood of septic arthritis.
3-2=ESR>40 mm/h, and 3-3=WBC count>12,000/ul. 3-4=an aspiration of < 50,000 leukocytes per mL virtually rules out sepsis of the joint. 3-5=>16 ° = abn 95% chance of progression <10 ° =95% chance of natural resolution of the bowing 3-6=(Satanic sequestrum) is necrotic bone 3-7=involucrum form an envelope of new bone is formed by the periosteum |
|
|
4-1= in-toeing? nl and abn, what age?
4-2 what age spontaneously resolve by? 4-3=what level in spinabifida WC, household ambulate, community ambulator? 4-4 how long after the onset of symptoms Legg-Calve-Perthes Dz are xray changes necessary for accurate classification 4-5=salvage procedure for pts presenting late in Legg-Calve-Perthes Dzwhat age ? 4-6=when perform Hari chiari 4-7 4=pedi elbow fx that always get surgery mnemonic |
4-1 in-toeing nl =IR= (-5 degrees);
abn= -10 deg =tibial torsion in toddlers (1-3 years) 4-2=by age 6=resolves spontaneously 4-3WC=L1; H Amb=L3; C Amb= L5 4-4=6 months 4-5= > 8 yr, especially lateral pillar B and B/C=femoral and/or pelvic osteotomy (Salter, triple innominate, Dega or Pemberton osteotomy, pelvic osteotomy-Shelf arthroplasty 4-6=Hari chiari=Chiari or shelve which are salvage procedure) 4-7 (1)Suprachondyler fs type 3; (2)Lateral Condyle Fx - 2 2 2 = ALWAYS DO surgery (milch 2 salter harris 2 > 2mm; (3)Incarcerated med epicondyl fx (4)a distal humeral physeal separation |
|
|
5-1=claw-hand deformity what nerve out, define?
Froment sign, define?, Wartneberg sign, define?, Jeanne's Sign, define? 5-2=Larsen's Syndrome,1-definition 2-clinical findings, genetics, PE 5-3=Titanium flexible nails should be avoided in patients 5-4=when do you see tear drop in pelvis 5-5 ossific nucleus of the proximal femur is visable on xrays by? 5-6: nl=early adolescence the average thigh foot axis is ? 5-7=nl=average foot progression angle is ? |
5-1=tardy ulnar nerve palsy:
-claw-hand deformity=MCP joints of the 4th and 5th fingers are extended and the Interphalangeal joints of the same fingers are flexed. -Froment sign (compensatory thump IPJ flexion due to weak adductor pollicis) -Wartneberg sign (persistent abduction and extension of the small digit during active adduction due to weak interosseous and lumbrical musculature). PICT #1 -Simultaneous hyperextension of the thumb MCP joint is indicative of ulnar nerve compromise. 5-2=hyperlaxity, abnormal facial features, and multiple joint dislocations; AR linked to carbohydrate sulfotransferase 3 deficiency; extremity weakness secondary to myelopathy, hand deformities=long cylindrical fingers that do not taper & wide distal phalanx at the thumb, scoliosis, bilateral knee dislocations, bilateral radial head dislocations, clubfeet cervical kyphosis 5-3=unstable fx and in those w/ > 11 yrs of age and > 108 lbs. As the patient is 10 years old and has open physes, there are concerns with intramedullary nailing (greater troch or piriformis entry) 5-4=In nl hips, all children have a teardrop figure=18 mths of age 5-5ossific nucleus of the proximal femur is visable=6 mths 5-6=early adolescence the average thigh foot axis is 10 degrees external (range -5 to +30), 5-7average foot progression angle=5 deg external for late childhood/early adolescence |
|
|
6-1:Beighton-Horan scale is used to evaluate patients with? what condition?
6-2;Beighton-Horan scale is scored on ?; a score of indicates generalized joint hypermobility? 6-3=Elements that are included in the physical exam include ? 6-4=Polyethylene wear rates have shown association with osteolysis and subsequent component loosening. Wear rates >?? mm per year are at significant risk of osteolysis. 6-5=ESR >??? was 93% sensitive and 83% specific for an infection while a CRP >????was 91% sensitive and 86% specific. aspirates w/ a WBC count > ???? and ???PMNs are highly suggestive of infection 6-6 composition of cartilage OA vs aging water???/proteoglycans???/collagen???/subchondral bone???/chondrocytes activity???/proliferation of chondrocytes???? 6-7"Fatel" anemia, aka, test for it, tx? |
6-1 Beighton-Horan scale is used to evaluate patients with joint laxity &
condition= Ehlers-Danlos syndrome. 6-2= a 9 items are scored on a scale from 0-> 9, A score of > 3 indicates generalized joint hypermobility. Elements that are included in PE= hyperextension of the fifth MCP joint 1 R & 1 L, apposition of the thumb 1 R & 1 L, hyperextension of the elbow and knee, 1 R & 1 L forward flexion of the trunk.1 6-4= Wear rates > 0.1 mm per year are at significant risk of osteolysis. 6-5=(NUN)ESR >22.5mm/hr; (DUMMY)(CRP >13.5mg/L aspirate w/(TATTO)WBC >1100 and PMN > 64% 6-6=(softer)increased water (as a result of the disruption in architecture of the matrix molecules)// decreased proteoglycans(same loss of filler)// decreased collagen w decreases in cross-linking and stiffness associated w/ degradation///, increased thickness of subchondral bone/// increased chondrocyte activity and proliferation of chondrocytes. =natural aging process which include: (dry) decreased water content, (less filler)decreased proteoglycan content and size (decreased length of protein core and GAG chains), nl quantity of collagen, ((stiff) increased collagen stiffness and cross-linking, unchanged thickness of subchondral bone, unchanged chondrocyte;unchanged chondrocyte; activity/proliferation 6-7Fanconi anemia, an AR condition resulting in aplastic anemia and eventual death; CBC, peripheral blood smear and chromosomal breakage analysis, None marrow transplant |
|
|
7-1=The bending rigidity of an intramedullary nail is related to the ???? power of the nail’s radius.
7-2=rigidity of a fracture plate is proportional to the plate thickness to the???? power. 7-3=likelihood of complete functional recovery to preoperative strength levels is???% 7-4=independent risk factors for dislocation after total hip arthroplasty EXCEPT vs. All of the following are associated with a post-operative nerve palsy EXCEPT vs risk factors for heterotopic ossification EXCEPT?? 7-5=acetabulum retroversion nl is ??? & ???degrees of abduction 7-6Acetabular Screw Placement and 4 Zones? 7-7Intersection Syndrome |
7-1=The bending rigidity of an intramedullary nail is related to the 4 power of the nail’s radius.
7-2=rigidity of a fracture plate is proportional to the plate thickness to the 3 power. 7-3=likelihood of complete functional recovery to preoperative strength levels is 35% to 40% 7-4= post traumatic OA should NOT have an increased risk of dislocation vs avn & RA NOT have increased risk post-op nerve palsy vs valgus knee deformity? 7-5=RTV=15-20 deg & Abd=45-55 7-6=3 DDD (Death, Danger & Disability Zones) and target zone "target zone"=posterior-superior quadrant BEST place for supplemental component screws. -elevating the hip center in revisions can place sciatic n @ risk in this quadrant "dEAth zone"=Anterior-superior quadrant (facing me) ExternAl iliAc vEssEls at risk "danger zone/ jEOpArdy"=ant-inf =Obturator n, artery, and vein at risk "Disability zone"=posterior-Inferior quadrant if screw > 20mm the following structures are at risk Sciatic n; Inferior gluteal n & vessles; Internal pudendal n& vessels 7-7=inflammation at 2nd dorsal compartment (ECRL, ECRB) |
|
|
8-1=Apert's syndrome is caused by a mutation in what gene?2: Achondroplasia?, SED congenita?; SED tarda ?Marfan syndrome?
8-2quadrigia effect = 8-3=Treatment - Proximal Phalanx Fx; Nonop=extraarticular w/< ???angul or < ???mm shortening & ???rotational deformity 8-4 why replace nail to ??? MC complication phalanx fx 8-5 if untreated a swan neck deformity will result from? pseudoboutonniere? failure to treat will lead to boutonneire deformity??? 8-6=volar lip fractures >???%-ORIF of phalanx fx 8-7which injuries tx buddy tape vs block splinting? |
8-1= apert's=(FGFR2) 2: Achondroplasia =FGFR3, (three foot dwarf) SED congenita = COL2A1; X-linked form of SED tarda = SEDL (SED late); Marfan syndrome = fibrillin
8-2quadrigia effect =overtensioning of the FDP tendon during surgical repair. 8-3NoP buddy taping x 3 wks of immobilization THEN aggressive motion=extraarticular with < 10° angulation or < 2mm short; 0 rotational deformity 8-4= replace nail-> maintain epi fold; Loss of motion 8-5=dorsal PIP dislocation injury secondary to a volar plate injury and at least on collateral ligament -PIP flexion contracture p/ PIP dorsal disloc - injury to the central slip and at least one collateral ligament, in Volar PIP Dislocation & Fracture-dislocations=boutinneirre 8-6> 40% joint involved and unstable fx 8-7 Bud tape=Dorsal PIP Dislocations dorsal extension block splinting =Dorsal PIP Fracture-Dislocations, Volar PIP Dislocation & Fracture-dislocations x 6-8 wks, Dorsal DIP Dislocations & Fracture-Dislocations x 2wks |
|
|
9-1=optimum tx for type 1 jersey finger,
9-2=MC congenital malformation of the limbs 9-3 flexor tendon repairs are weakest between postop day ???& ??? 9-4# of suture strands that cross the repair site is more important than ??? 9-5most common complication following flexor tendon repair 9-6 what % of tendon should re repaired?, when should tendon be repaired? 9-7Vickers ligament, MC hand mass |
1-FDP tendon retracted to palm. Leads to disruption of the vascular supply Prompt surgical treatment within 7 to 10 days
9-2=Syndactyly 9-3=tendon repairs are weakest = day 6 & 12 9-4# of suture strands that cross the repair site is more important than = # of grasping loops 9-5 adhesions 9-6 >60%, < 3 wks ideal 2 wks 9-7thickening ligament from the distal radius to the lunate seen in Madelung's Deformity, ganglion cyst |
|
|
10-1 MC location ganglion cyst?
10-2 ??? % elongation will disrupt axons, ???mm Hg can cause paresthesias, ??? mm Hg can cause complete block of conduction 10-3 what is abn value with CTS re: latencies of NCV sensory & motor; conduction velocities; motor action potential (MAP) & (SNAP) 10-4 when nerve graft used to treat? does the type of nerve autograft efect functional outcome 10-5 which nerves has the worse recovery than most other repairs?(3) which has the best? 10-6 Merkel's receptor chrteristics 10-7 Commonly missed injury on xray (~25%) on initial presentation? name the 8 carpal bones. |
10-1 dorsal carpal (70%) originate from SL ligament
volar carpal (20%) originate from radiocarpal or STT joint 10-2 15% elongation will disrupt axons; 30 increase latency, 60 mm block conduction 10-3=>CTS->increase sensory distal latency of > 3.2 & motor latencies > 4.3 ms conduction velocities decreased< 52 m/sec less specific that latencies motor action potential (MAP) & sensory nerve action potential (SNAP)->decreases in amplitude 10-4 NG=x>2.5-5.0 cm (25-50 mm) loss or collagen conduit; type of nerve graft (sural, saphenous, etc) used has NOT shown to be statistically significant in terms of functional recovery after nerve repair. 10-5=the worst recovery=>deep peroneal nerve, ulnar nerve, brachial plexus lesions. Best-radial 10-6=slowly adapting skin receptors that detect pressure, texture, and low frequency vibration and are best evaluated by static two-point discrimination 10-7 Lunate Dislocation (Perilunate dissociation); prox row=scaphoid, lunate, triquetrium, pisiform distal row=trapezium, trapezoid, capitate, hamate |
|
|
11-1 break in Gilula's arc, piece-of-pie sign
11-2=Lumbrical Plus Finger, What is a potential complication of an amputation at the level of the distal interphalangeal joint? 11-3-Intrinsic Minus Hand 11-4 Extensor Tendon Compartments mnemonic name the tendons & pathologies 11-5 Bennett Fracture, Rolando fx= 11-6 Heberden's nodules, Bouchard nodes 11-7 AIN is terminal motor branch of??? nerve, mnem for AIN mus innervation? Froment sign define? Jeanne sign? Wartenberg sign? |
three radiographic arcs was first proposed by Gilula in 1979. The carpal bones all have rounded edges to varying degrees, and as such the arcs have small indentations at the joint lines. However, there should be no stepoffs in the contour of the arcs. Such a "broken arc" implies a ligament tear or fracture at the site of the broken arc.
-abnormal triangular appearance of the lunate on an AP image of the wrist indicating lunate dislocation or perilunate dislocation 1-2. A lateral image will help differentiate whether there is lunate or perilunate dislocation with lunate dislocation demonstrating a spilled teacup sign. 11-2=paradoxical extension of the PIP joints while attempting to flex the fingers, lumbricals originate from FDP, with FDP laceration, FDP contraction leads to pull on lumbricals, lumbricals pull on lateral bands leading to PIP and DIP extension of involved digit, Lumbrical plus finger. 11-3 (Claw Hand)-Caused by imbalance between strong extrinsics and deficient intrinsics, Characterized by MCP hyperextension & PIP & DIP flexion 11-4=2-2-1-2-1-long short long short long 1 Extensor pollicis brevis (EPB) Abductor pollicis longus (APL) De Quervain's tenosynovitis 2 Extensor carpi radialis longus (ECRL) Extensor carpi radialis brevis (ECRB) Intersection syndrome 3 Extensor pollicis longus (EPL) Drummer's wrist, traumatic rupture with distal radius fx 4 Extensor indicis proprius (EIP) Extensor digitorum communis (EDC) Posterior interosseous nerve Extensor tenosynovitis 5 Extensor digiti minimi (EDM) Vaughn-Jackson Syndrome 6 Extensor carpi ulnaris (ECU) Snapping ECU 5-Bennett Fracture=Intra-articular fracture/dislocation of base of 1st metacarpal R fx=Comminuted, intra-articular fracture of the metacarpal base 6-B comes before H, so Bouchard's is in proximal IP joint ( "B" is proximal to "H" in the alphabet chain) Heberden's nodules=When you hold a Hair (H for Heberden's) you use more of your distal IPJ Bouchard nodes=When you hold a Bat, you use more of your proximal IPJ i.e. B for Bat and Bouchard's. 7=AIN is terminal motor branch of median nerve, AQUA PRO: FDP (index and middle finger); FPL; pronator quadratus, compensatory thumb IP flexion by FPL (AIN) during key pinch -Jeanne sign=compensatory thumb MCP hyperextension and thumb adduction by EPL (radial n.) with key pinch =WS=persistent small finger abduction and extension during attempted adduction secondary to weak 3rd palmar interosseous and small finger lumbrical |
|
|
12-1=proximal to carpus, warm ischemia time ??hours & cold ischemia time ??? hours; distal to carpus (digit), warm ischemia time ???hours & cold ischemia time ??? hours
12-2boxer's knuckle= 12-3 4 PE signs =ULNAR neurapathy & define 12-4-in a normal neutral wrist approximately ??? of the load goes to the ulna &??? to the radius 12-5=free tissue transfer within ???hours for severe trauma in the UE has been shown to decrease complication rates? 12-6Which of the following flexor tendon annular pulleys originate from palmar plates overlying joints? 12-7 radial nerve innervation, mn |
1-proximal to carpus, warm ischemia time < 6 hours & cold ischemia time < 12 hrs
distal to carpus (digit), warm ischemia time < 12 hrs & cold ischemia time < 24 rs 2=Sagittal band (SB) rupture leads to dislocation of the extensor tendon 3=Froment sign=compensatory thumb IP flexion by FPL (AIN) during key pinch Wartenberg sign persistent small finger abduction and extension during attempted adduction secondary to weak 3rd palmar interosseous and small finger lumbrical Jeanne sign=compensatory thumb MCP hyperextension and thumb adduction by EPL (radial n.) with key pinch 4-ulna 20 & radius 80 Masse sign=palmar arch flattening and loss of ulnar hand elevation secondary to weak opponens digiti quinti and decreased small finger MCP flexion 5=free tissue transfer within 72 hours for severe trauma in the upper extremity has been shown to decrease complication rates 6-A1,A3,A5 7-Radial nerve, proximal to distal "Try A Big Brazilian Chocolate PECAN Chip Sundae, Double Dip Cherries And PeanutButter Please Included" T-Triceps, A-Anconeus, B-Brachioradialis, B-Brachials Lateral 1/2, C-ext. Carpi radialis longus(ECRL), PECAN-PIN C-ext. Carpi radialis brevis (ECRB), S-Supinator, D-ext. Digitorum comminunus (EDC), D-ext.Digiti minimi, ext.(EDM) C-extensor Carpi ulnaris (ECU), A- Abductor poll. longus (APL), P-ext. Poll. brevis (EPB), P- ext. Poll. longus (EPL), I- ext. Indicis proprius (EIP) |
|
|
1-MC solid tumor of childhood,MC benign bone tumor in childhood ? **MC primary bone malignancy? ****MC benign bone tumor
2-mn=Round cell tumors of bone adult and child 3-mn=multiple myeloma? what causes the lytic destruction seen on xrat in Multiple myeloma? 4-Mazabraud's syndrome, MC site in axial skeleton for GCT? 2^ MC form of soft tissue sarcomas in adults? hallmark of liposarcomas? 5-MC soft-tissue sarcoma in adults 55 to 80 years of age 6-mnc-Differential Diagnosis of Solitary Lucent Bone Lesions, mnc-Differential Diagnosis of Multiple Lucent Bone Lesions 7-why get MRI for ST Sarcoma? |
1-MC S.T.oC.H-Neuroblastoma = sympathetic neural tissue
-MC Ben bone tumor in children=Non-ossifying Fibroma NOF -MC 1^ bone malignancy=Multiple Myeloma -MC ben bone tumor=Osteochondroma 2-??MR. LEMONS'', might refer to a similar thing; M-Metastatic neuroblastoma R-Rhabdomyosarcoma, embryl, round cell liposarcoma L-Lymphoma Non hodgkins E-Ewing's sarcoma, eosinophilic granuloma Meduloblastoma- Wilms’ tumor blastemic, myeloma O-Osteosacroma N-Neuroblastoma/pNET=primitive neuroectodermal tumors S-Small cell (oat cell)?? Round cell tumors of bone child NEWeR & adult ROME R: reticulum cell sarcoma O: osteosarcoma M: - E: Ewing's sarcoma N: Non-Hodgkin's lymphoma E: Ewing's sarcoma/PNET W: Wilms’ tumor blastemic component of R: rhabdomyosarcoma 3-multiple myeloma is "CRAB infections": C-Calcium (i.e. hypercalcaemia) R-Renal failure (acute or chronic) A-Anaemia (multifactorial) B-Bone pain (from lytic lesions or pathological fractures) Infections (they're heavily predisposed, mostly from their immune paresis) -show multiple "punched-out" lytic lesions lytic lesions caused -> osteoclastic activation via tumor cell secretion of RANKL, IL-6 and MIP-1alpha 4-MazaBrauD's syndrome=Multiple intraMuscular Myxomas associated with Monostotic or polyostotic fiBrous Dysplasia, MC loc for GCT in axial skel=sacrum, -2nd MC sarcoma=liposarcoma -lipoblast which signet ring-type cell 5-MC ST Sarc=MFH Malignant Fibrous Histiocytoma (Pleomorphic Sarcoma) 6FOGMACHINES F-Fibrous dysplasia, Fibrous cortical defect O-Osteoblastoma G-Giant Cell Tumor M-Myeloma (plasmacytoma), Metastases from kidney, thyroid, breast A-Aneurysmal bone cyst / Angioma C-Chondromyxoid fibroma, Chondroblastoma H-Hyperparathyroid brown tumor, Hemangioma, Hemophilia, Histiocytosis X I-Infection (Brodie abscess, Echinococcus, coccidioidomycosis) N-Non-ossifying Fibroma E-Eosinophilic granuloma, Enchondroma, Epithelial inclusion cyst S-Solitary Bone Cyst 3-FE2M2-H2I F-Fibrous Dysplasia E-Eosinophilic Granuloma / Enchondroma M-Metastasis / Myeloma H-Hyperparathyroidism (brown tumors) / Hemangioma I-Infection 7-evaluate size, depth, and surrounding anatomy |
|
|
14-1 what is Harington's criteria used for? what are the 7 criteria?
2-what is Mirels criteria used for, based on? what value of Mirels criteria suggests prophylactic fixation? 3-In terms of life expectency, which cancers (2) have the worst median survival (<6 months) and 5 year survival (<5%) when bone metastases are present. 4-MC long bone associated with metastatic dz? MC site for pathologic fx 2^ to metastatic carcinoma is? What is the MC site of all bone metastasis? 5- MC side effect of Doxorubicin, a cytotoxic antibiotic (commonly referred to by its brand name of Adriamycin)? MoI of Doxorubincin? comes from where? used to tx? what is a anthracyclines ? 6-MCComplication of:Ifosfamide & MoA, Cyclophosphamide, methotrexate Bleomycin ? MoA of methotrexate & Cis-platnum 7-1 rad = ? Typical dose is XRT/day, uncomplicated tissue healing XRT Total dose? tissue will likely not heal w/ XRT Total dose?risk factors for post radiation fracture? |
1-Indications for ORIF of metastatic lesions ie prophylactic fixation of impending pathologic fracture.
(1)Life expectancy greater than 1 - 2 months (2)Persistent pain after radiotherapy (3)Lesion > 2.5 cm diameter in metaphysis (50 - 75 % destruction) (4)Destruction of 50% or >of the diaphyseal cortex of a long bone (5)Adequate bone quality (6)Procedure would enhance mobilization and independence (7)Permeative destruction of the subtrochanteric femoral region 2-Score/ 1 2 3 Site/ upper limb lower limb peritrochanteric Pain/ mild moderate functional Lesion type/ blastic mixed lytic Size < 1/3 1/3 to 2/3 > 2/3 score > 8 suggests prophylactic fixation 3-re: life expectency, lung cancer and melanoma have the worst median survival (<6 months) and 5 year survival (<5%) when bone metastases are present. 4-MC long bone associated with metastatic disease=femur -MC site for pathologic fx 2^ to metastatic carcinoma is =proximal femur2^ to the fact that the femur is the MC long bone assoc w/ metastatic dz and the stress risers around the proximal femur make it easy to fracture. -MC site of all bone metastasis=spine however is the most common site of all bone metastasis. 5-MC side effect Doxorubicin=cardiac toxicity, cardiomyopathy -interacts with DNA by intercalation and inhibition of macromolecular biosynthesis.[34][35] This inhibits the progression of the enzyme topoisomerase II, which relaxes supercoils in DNA for transcription.[36] Doxorubicin stabilizes the topoisomerase II complex after it has broken the DNA chain for replication, preventing the DNA double helix from being resealed and thereby stopping the process of replication. - obtained from the bacterium Streptomyces peucetius -Tx-lung , breast, stomach, Hodgkin and Non-Hodgkin lymphoma 6-Ifosfamide= major neurological toxicity like encephalopathy. MoI=DNA alkalting agent Cyclophosphamide =myelosuppression & urotoxicity. methotrexate=neurotoxic seizures Bleomycin=pulmonary fibrosis. methotrext= competitively inhibits dihydrofolate reductase (DHFR), an enzyme that participates in the tetrahydrofolate synthesis cis-platnum= crosslinks DNA in several different ways, interfering with cell division by mitosis. The damaged DNA elicits DNA repair mechanisms, which in turn activate apoptosis when repair proves impossible. 7-1 rad = 1 centiGray XRT= 180-200 cGy/day; -uncomplicated tissue healing=45 - 55 Gray TD NO healing=>60 Gray TD -age, F, osteoporosis anterior femoral compartment resection, periosteal stripping radiation dose >60 Gy |
|
|
15-1=MC site of bony metastasis, MC reason for a destructive bone lesion in in older patients (> 40 yrs)? mc carcinomas mets that commonly spread to bone -mnemonic
2-top 3 MC site for metastatic disease ? MC site of fx secondary to metastatic bone lesions? MoI of mets causing osteolytic bone lesions? 3-osteoblastic bone metastases are due to tumor-secreted ? which 2 mets typrs are blastic & lytic 4-Undifferentiated Pleomorphic Sarcoma aka 5-Endothelin 1 is known to be involved in, MSTS (Enneking) Staging System 6-which mets get bx?, tx of a met? |
1-MC=thoracic spine is most common site of bony metastasis
-MC destructive bone lesion in adults=mets "Boners Penetrate Ladies That Kiss " MC- Breast and Prostate B- Breast (Both blastic and lytic)=24 months P- Prostate (blastic)=40 months L- Lung (Lytic)=6 months T- Thyroid=48 months 4yrs K- Kidneys=variable depending on medical condition but may be as short as 6 months 2-(behind lung and liver) bone -proximal femur - caused= tumor induced activation of osteoclasts, ex=RANK, RANK ligand (RANKL), osteoprotegrin pathway PTHrP (+) breast cancer cells activate osteoblastic RANKL production -osteoblastic bone metastases are due to tumor-secreted=endothelin 1 -blastic-breast & prostate lytic=breast & lumg 4-MFH malignant fibrous histiocytoma, undifferentiated pleomorphic sarcoma (UPS) 5-Osteoblastic bone metastases Stage:Grade:Site (1):Metastasis IA Low Grade T1 - intracompartmental M0 (none) IB Low Grade T2 - extracompartmental M0 (none) IIA High Grade T1 - intracompartmental M0 (none) IIB High Grade T2 - extracompartmental M0 (none) III Metastatic T1 - intracompartmental M1 (regional or distant) III Metastatic T2 - extracompartmental M1 (regional or distant) 6 all until history of biopsy proven metastatic, ALL get XRT, if IM XRT entire bone |
|
|
16-1 what do these common forms of spinal cord monitoring abbreviate- Mechnical Electromyography (spontaneous) SEP MEP, adv & disadv each
2 mnemonic for Afferent vs. efferent neurons columns in spinal cord ? 3-indications & CI for bisphonates? mn vaule needing treatment? mn for group ob bisphonates 4-mn for coagulation cascade? Virchow's triad? vit k dep factors 5-highest risk of bleeding and thrombocytopenia? pencil in cup seformity & nail pitting |
1-most common forms are Mechnical Electromyography (spontaneous)-monitor integrity of specific spinal nerve roots, contact alone of a surgical instrument to the nerve root will lead to "burst activity" which carries no clinical significance
more significant injury or traction to a nerve root will lead to "sustained train" activity, which may carry clinical significance Electrical Electromyography (triggered)-allows detection of a breached pedicle screw SEP (somatosensory evoked potentials), MEP (motor evoked potentials) 2-SAME SAD DAVE Cortispinal "My SAME friend DAVE Corticospinal got pain bc/kick in the Behind & Moved when he was kicked in the front": D-Dorsal A-Afferent component is the "sensation" of pain coming in behind. V-Ventral E-Efferent component is the "motor" action, he screamed (which is done at front of body). Spinal cord: afferent vs. efferent neurons="SAME" S-Sensory A-Afferent-> Arrive M-Motor E-Efferent-> Exit Advantages reliable and unaffected by anesthetics Disadvantages not reliable with respect to monitoring the integrity of the anterior spinal cord pathways reports exist in literature of an ischemic injury leading to paralysis despite normal SEP monitoring during surgery 3-MOM's PET POIson RottweiLer M-mets O-Osteoporosis M-Multiple myeloma P-Paget's E-Early stages of AVN T-total joint arthoplasty to prevent osteolysis P-polyostotic fibrous dysplasia O-osteogeneis I-imperfecta, cyclical IV pamidronate R-Renal dz severe L-Lumbar fusion following -bone mineral density 2.5 or more -NON TECATP Die=no nitrogen Tiludronate Etidronate/Didronel, Clodronate, ATP die 4-12, 11, 9, 8 X 7 10 lovenox/enxiparen Arixtra 5 2 1 -venous stasis, endotheleal damage, hypercoagulable state 4-2,7,9,10 5-Unfractionated heparin. psoriatic arthtitis |
|
|
17-1 Virchow's triad & risk factors for DVT/PE? mn
2-AAOS risk for: MAJOR bleed (3)& PE(2) & if getting THA or TKA? 3-classic finding of PE on EKG? mn ABG, nl values pH = PaCO2 = HCO3 = PO2 = classic CXG finding of PE (2) |
1-H-Hypercoagulable state
I-Intimal Injury S-Stasis venous E-Ex DVT previously, EPO, Ex-fix M-malignancy B-Baby? pregnancy O-Osetrogen, BCP, L- Large, obesity wt > 20% of nl wt, (overweight =BMI(25-30)) OBESE BMI>30 I-Immune Dz=antiphospholipid antibody conditions lupus anticoagulant, anticardiolipin antibody, 3 antithrombin III deficiency , 5-factor V Leiden mutation, C-CLot S- Stoppers S-Surgery previously or trauma M-Mobilization lack of 2-AAOS risk factors for major bleeding: (1)bleeding disorders, (2)hx of a recent GI bleed (3)hx of a recent hemorrhagic stroke/cVA AAOS risk factors for PE (1)hypercoagulable state (2)previous documented PE AAOS TKA & THA(low to high risk of either bleeding or pulmonary embolism)=pneumatic compression devices (MECHANICAL devices) 3- sinus tachycardia, right axis deviation and right bundle branch block. ***SI QIII TIII pattern - deep S wave in lead I, Q wave in III, inverted T wave in III. (S1 Q3 T3 Which means deep S wave in Lead I, Appearance of Q wave and T wave inversion in Lead III) This “classic” finding is found in only 20% of patients with PE. 3-ROME [Respiratory Opposite, Metabolic Equal] - meaning, In a Resp disorder, pH and PCO2 go in opp directions, and in Metab disorder pH and HCO3 go in the same direction (this may be fairly obvious) pH = 7.35 -7.45 —> 7.4 PaCO2 = 33-44 —> 40 HCO3 = 22 -28 —> 24 PO2 = 75-105 Most patients are hypoxic (Pao2 < 80 mm Hg), hypocapnic (Paco2 < 35 mm Hg), and have a high A-a gradient (> 20 mm Hg). CXR=Westermark Sign, is a sign that represents a focus of oligemia (leading to collapse of vessel) seen distal to a pulmonary embolism (PE) & Hampton's hump (a wedge shaped, pleural based consolidation associated with pulmonary infarction), has a low sensitivity (11%) and high specificity (92%) |
|
|
18-1Bones that receive tenuous blood supply (4)?mn
-centrifugal, centripetal flow of Arterial Flow and venous in mature/immature bone? -direction of flow Periosteal System in Haversion system & Volkman's artery?mn -risk of hepatitis B, C & HIV disease transmission in musculoskeletal fresh-frozen allograft transplantation 2-Which of the following bone graft substitutes has the fastest resorption characteristics? what is tested for in allografts?(5) 3-explain calcitonin "keeps the bone IN" & role of IL-10, IL-1, calcitonin and bisphonates 4-explain the story of osteocytes, osteoblasts, osteoclast, osteoprogenitor cells 5-metatarsal MC fractured, MC fx in ballet dancers, MC location of stress fracture, how much wt bearing does 1 MT experience? 6=gold standard test r/o dvt, 4-Major criteria for fat emboli syndrome? TX, types of immunologic reactions-mn |
1-tenuous blood supply (NOT FOST but S L O W healing)
F-Femoral head O-Odontoid S-Scaphoid T-Talus Arterial Flow:centrifugal (inside to outside) centrifuge in lab spinning->Mature bone Arterial Flow & Venous Flow centripetal (outside to inside)->Gravites affect on asteroid passing by the earth->Immature bone -HaverSioN system -North South or parallel to long axis Volkman's artery-WolkmEn-East West or perpendicular axis. -B=1:63,000, C=1:100,000, HIV=1:1,000,000 2-Calcium sulfate , Hepatitis B,C HIV, syphilis, HTLV-I/II, 3-calcitonin & bisphosphonates & IL-10->keep the bone IN by inhibiting osteo-CLAST, bisphosphonates=prevents osteoclasts from forming ruffled border and producing acid hydrolases) 4- 5-5th MT, base of 2nd metatarsal in ballet dancers, 2nd, bears 30-50% of weight during gait 6= Venous ultrasonography, Major (1) hypoxemia (PaO2 < 60), CNS depression (changes in mental status), petechial rash-axillary region conjunctivae, oral mucosa; pulmonary edema; Tx=PEEP -mn=ACID-AEGMD-s Type I - A-Anaphylaxis-E-allEgic, anaphalEctic dEath Type II - C-Cytotoxic-IgG-Global most abundant M-iMMediately appears Type III -I-Immune complex mediated-IgG,M Type IV - D-Delayed type of hypersensitivity-T-cells A-sAliva & teArs=secetions, D-unknown |
|
|
4-collegen types in articular cartilage
5-MoA=Aspirin (ASA), ibuprofen, indomethacin 6-w/u for mets, who am I cortical metastasis, lesions distal to elbow and knee? pre-op embolization? 7-who w/mets get surgery? 2 signs on cxr suggestive of PE? |
4-mjr 2:::5,6:::9,10,11
5-Aspirin (ASA) salicylate that irreversibly binds a serine COX enzyme residue half life >1 week binds to COX and blocks active site inhibits thromboxane A2 blocking platelet aggregation ibuprofen reversible competitive COX inhibitor indomethacin acts on the lipoxygenase side of the arachidonic metabolic pathway inhibibits leukotriene inflammatory mediators 6-imaging=xray in 2 planes of affected limb=cortical metastasis are common in lung cancer, lung, thyroid, and renal are primarily lytic 60% of breast CA is blastic 90% of prostate CA is blastic CT of chest / abdomen / pelvis, technetium bone scan to detect extent of dz, myeloma and thyroid carcinoma are often cold on bone scan - evaluate with a skeletal survery IF metastatic lesions to the spine THEN MRI labs=CBC with differential, ESR, basic metabolic panel, LFTs, Ca, Phos, alkaline phosphatase serum and urine immunoelectrophoresis (SPEP, UPEP) biopsy =in patients where a primary carcinoma is NOT identified, obtaining a bx is necessary to r/o a primary bone lesion, should not treat a bone lesion without tissue diagnosis of the lesion metastatic adenocarcinoma not identified by CT of the chest, abdomen, and pelvis is most likely from a small lung primary tumor -cortical metastasis are common in lung cancer & lesions distal to elbow and knee are usually from lung or renal primary -renal cell carcinoma or thyroid carcinoma prior to operative intervention 7-metastatic lesions to spine with neurologic deficits in patients with life expectancy of > 6 months=neurologic decompression, spinal stabilization, and postoperative radiation |
|
|
1-a higher modulus of elasticity indicates ?
what's in titanium, stainless steel, Cobalt alloy components 2-2 ex's of oncogenes, function 3-mn-carcinoembryonic antigen (CEA) =>? mn-carbohydrate antigen 19-9 (CA-19-9)=>? mn-carbohydrate antigen 125 (CA-125)=> mn-cancer antigen 15-3 (CA-15-3) => mn-alpha fetoprotein (AFP) =>MC -Tumor Suppressor Genes 2 ex's what their role in Cancer? mn & me |
1-a higher modulus of elasticity indicates a stiffer material
2- Ti-6Al-4V'= 6% aluminium, 4% vanadium, 0.25% (maximum) iron, 0.2% (maximum) oxygen, and the remainder titanium Stainless Steel (316L)=primarily iron-carbon alloy with lesser elements of chromium, molybdenum manganese Cobalt alloy=cobalt, chromium, molybdenum 2-FAK=focal adhesion kinase) Erb-2=epidermal growth factor variant 3-carcinoembryonic antigen (CEA) /CIA up your ASS & CEA & CIA 3 letters colorectal carcinoma carbohydrate antigen 19-9 (CA-19-9) hey the balloon took the pan for a ride pancreatic cancer carbohydrate antigen 125 (CA-125) football star a woman? ovarian cancer cancer antigen 15-3 (CA-15-3) 3 treasure chests full of breast cancer alpha fetoprotein (AFP)=MC seen in hepatocellular carcinomas Tumor Suppressor Genes=therefore a mutation interfering with normal function causes leads to uncontrolled cell growth retinoblastoma protein (pRB-1) abnormal state is phosphorylated and unable to bind to DNA to regulate& p53 normal protein prevents entrance into S-phase of cell cycle when DNA is damaged, my research with Dr. Shirley now MIT on tumor, suppressor gene mutations prevents p53-dependent growth suppression. Commonly seen in osteosarcoma (20-65%) chondrosarcoma |
|
|
Genetic Pearls of Skeletal Dysplasia
Achondroplasia Apert Syndrome CMT Pseudoachondroplasia SED congenita Kniest's Syndrome MED - Type I MED - Type II Type IX collagen Jansen's metaphyseal chondrodysplasia Functional defect in parathyroid hormone Schmid's metaphyseal chondrodysplasia Cleidocranial dysplasia Osteogenesis Imperfecta (Type I, IV) Autosomal Recessive Diastophic dysplasia Friedreich's Ataxia Osteo. Imperfecta (Type II, III) McKusick metaphyseal Unknown X Linked Recessive SED tarda CMT (10-20%) Disease Translocation Gene mn Ewing's sarcoma Rhabdomyosarcoma Myxoid liposarcoma Synovial sarcoma Clear cell sarcoma Chondrosarcoma (Myxoid Variant) |
Achondroplasia=FGFR-3, Inhibition of chondrocytes proliferation
Apert Syndrome=FGFR-2, Inhibition of chondrocytes proliferation CMT (80-90%) =PMP22 Nerve demyelination Pseudoachondroplasia =COMP, Abnormal cartilage formation SED congenita=COL2A1 / Type II collagen, Defect in cartilage matrix formation Kniest's Syndrome=Type II collagen MED - Type I =COMP, Type II collagen MED - Type II Type IX collagen Jansen's metaphyseal chondrodysplasia=PTHrP Functional defect in parathyroid hormone Schmid's metaphyseal chondrodysplasia Type X Collagen, Defect in cartilage matrix formation Cleidocranial dysplasia=CBFA-1 Impaired intramembranous ossification Osteogenesis Imperfecta (Type I, IV)= COL1A1/COL1A2, Type I collagen Autosomal Recessive Diastophic dysplasia=DTD (Sulfate Transport Protein), Defect in sulfaction of proteoglycan Friedreich's Ataxia =Frataxin Osteo. Imperfecta (Type II, III) COL1A1/COL1A2 Type I collagen McKusick metaphyseal Unknown X Linked Recessive SED tarda=COL2A1, Type II collagen CMT (10-20%)=connexin gene, Nerve demyelination Disease Translocation Gene mn= mn-Patrick Ewing's sarcoma=t (11:22),Fusion protein (EWS-FLI1) mn-2 muscles cut by mirror Rhabdomyosarcoma, t (2:13), Pax3-FKHR mn fat footballs found in the treasure chest dancing in the mix Myxoid liposarcoma, t (12:16) TLS-CHOP mn-synovial trucker ran me over. Synovial sarcoma, t (X:18), SYT-SSX1, 2or4 fusion prtn mn- the clear football was caught by the nun for winning touchdown-Clear cell sarcoma, t (12:22), Fusion protn EWS-ATF1 mn-big ballon landed on the nun huring her cartilage in her knees. Chondrosarcoma (Myxoid Variant), t (9:22), Fusion protein EWS-CHN |
|
|
1-Western blot detects ? mn-
Southern blot detects ? mn- Northern blot detects? mn- Southwestern blot ? mn- 2-RT-PCR? laboratory tools is used to detect genetic translocations for prenatal screening? 3-composition ligament? 4-absolute rigidity construct healing is? indications for locked plate? locking plate vs. fixed angle plate? 5-what % of strain present for 1^ & 2^ healing? define strain & stiffness in fracture healing? 6 define Oligotrophic nonunion, MoI/pathology and other types of non union 7-strain theory? |
Western blot near Pacific Ocean detects Protein
Southern blot detects Delaware DNA Red neck state Northern blot detects Rhode Island & Brown Univ in North RNA Southwestern blot detects Delawre Rednecks Pisssing on sidewalk DNA binding proteins RT-PCR =reverse transcription PCR, detects low copy number of Rhode Islanders RNA Cytogenetic analysis performed for prenatal testing involves analyzing entire chromosomes, obtained from the nucleus of the cell, to determine changes in chromosomal size and number (e.g. Down Syndrome, trisomy 21) 3-Type I collage 4-lag screw + neutralization plate healing is by primary (Haversian) -1) indirect fracture reduction, as they can tolerate imperfect reduction 2) diaphyseal/metaphyseal fractures in osteoporotic bone; 3) the bridging of severely comminuted fractures to minimize soft tissue damage; 4) the plating of fractures where, due to anatomic constraints, a compression plate may not be placed on the tension side of the fracture. -Locking plates = the fixed angle to ensure stability of the construct, conventional plates = the plate/bone friction, as well as fracture end contact to ensure stability 5-Strain < (2%) for primary bone healing to occur, =10-30% for secondary bone healing to occur. Strain in fractures = dividing the interfragmentary movement by the size of the fracture gap. Stiffness refers the ability of the construct to resist movement under applied loads. 6-callus is absent but intact blood supply MoP-internal fixation w/o accurate apposition of fragments 7-strain theory states that for two given fracture segments, the healing interface will possess a force-generated motion potential that is contingent on the stability of the original fixation construct. Mathematically, the strain for any given force is equal to the change in the interface length divided by the original interface length. Therefore, with an unstable construct, the healing gap may undergo excessive motion with resultant increasing strain. Perren’s strain theory.(With a small fracture gap, any movement will result in a relatively large change in length (i.e. high strain). If this exceeds the strain tolerance of the tissue, healing will not take place. If a larger fracture gap is subject to the same movement, the relative change in length will be smaller (i.e...) Strain is the deformation of a material (eg, granulation tissue within a gap) when a given force is applied. Normal strain is the change in length (Δ l) in comparison to original length (l)when a given load is applied. Thus, it has no dimensions and is often expressed as a percentage. The amount of deformation that a tissue can tolerate and still function varies greatly. Intact bone has a normal strain tolerance of 2% (before it fractures), whereas granulation tissue has a strain tolerance of 100%. Bony bridging between the distal and proximal callus can only occur when local strain (ie, deformation) is less than the forming woven bone can tolerate. Thus, hard callus will not bridge a fracture gap when the movement between the fracture ends is too great [22]. Nature deals with this problem by expanding the volume of soft callus. This results in a decrease in the local tissue strain to a level that allows bony bridging. This adaptive mechanism is not effective when the fracture gap has been considerably narrowed so that most of the interfragmentary movement occurs at the gap, producing a high-strain environment. Thus, overloading of the fracture with too much interfragmentary movement later in the healing process is not well tolerated [23]. |
|
|
level of evidence?
Level 1 Level 2 Level 3 Level 4 Level 5 2-what is (DNA) do? which base pairs? mn Gene define, define Transcription & Translation 4 stages of mitosis 3-One hallmark of cancer is the cell's 4- death receptors ??? and ??? trigger apoptosis upon engagement by their cognate death ligands. 5-bending rigidity plate proportional to thickness to the ??? power, rod stiffness, define stiffness 6-load-bearing device that is most effective when placed on the???? side 7-what kind of property is a plate, nail to the bone? |
(antenna) RCT Level 1=Randomized controlled trial (RCT) a study in which patients are randomly assigned to the treatment or control group and are followed prospectively, Meta-analysis of randomized trials with homogeneous results
- level 2 two elevators side by to compare Level firward we go=Prospective comparative study (therapeutic) a study in which patient groups are separated non-randomly by exposure or treatment, with exposure occurring after the initiation of the study, Meta-analysis of Level 2 studies or Level 1 studies with inconsistent results, "less than 80% follow-up, no blinding, or improper randomization" are lesser-quality studies and qualify as Level 2 evidence -traffic light looking back retro Level 3=Retrospective cohort study, a study in which patient groups are separated non-randomly by exposure or treatment, with exposure occurring before the initiation of the study -4 Case-control study a study in which patient groups are separated by the current presence or absence of disease and examined for the prior exposure of interest Meta-analysis of Level 3 studies horse running in series Level 4=Case series a report of multiple patients with the same treatment, but no control group or comparison group 5-one star on case repot-Level 5=Case report (a report of a single case) Expert opinion Personal observation 2-regulates cell division, mRNA is produced from DNA, double stranded, strands linked together by phosphate groups -At The Girl's Club = AT + GC Adenine pairs with Thymine Guanine pairs with Cytosine -Gene=segment of DNA that contains the information needed to synthesize a protein -Transcription DNA => mRNA, Translation mRNA => protein -PMAT: The four stages of mitosis (in order): For: Prophase, Metaphase, Anaphase, Telophase 2)ProMote Another Tadpole 3-One hallmark of cancer is the cell's loss of apoptosis 4- death receptors Fas and tumor necrosis factor receptor 1 (TNFR1) trigger apoptosis upon engagement by their cognate death ligands. 5-ridgity=thickness ^3 r=^4, -stiffness= the ability of the construct to resist movement under applied loads. 6-load bearing best=TENSION side 7-plate=load-bearing device, naol=load-sharing device |
|
|
1=center of gravity of human ?
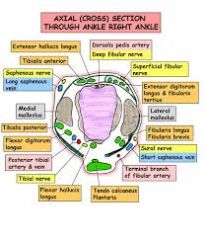
-coefficient of friction of human joints is & ice ? TJA (metal on PE) is? 2-Vector=?scalar quantities= 3 (classic triad)=paroxysmal pain exquisite tenderness to touch, cold intolerance think which tumor,& Tx 4-MC ankle w/ ER 5-PE finding of syndesmosis? 6-nl =tib-fib clear space, tib-fib overlap on AP & mortis, medial clear space? 7-anatomically where are the following tubercles= chopart's, Volkman's, Wagstaffe, which is the strongest lig of syndesmosis |
1-center of gravity = anterior to S2
-coefficient of friction of human joints is .002 to .04 ice=.005 TJA (metal on PE) is .05 to .15 2-Vector=a quantity that contains both direction and magnitude scalar quantities do not have direction 3-glomus tumtor, Tx- Ben=marginal excision is curative 4-syndesmosis injury, high ankle sprain 5-(+) squeeze test (hopkins) & ER test 6-AP and mortise ankle radiographs tibiofibular clear space shoulde be < 6 mm tibiofibular overlap for AP view > 6 mm med clear space<4 mm Chopart's Tub=(AITF) Ant Inf tib-fib lig attachment on tibia Wagstaffe's=(AITF) Ant Inf Tib fib lig attachment on the fibula Volkman's Tub=(PITF) Pos Inf Tib fib lig attach on the tibia stongest lig=PITF lig |
|
|
25-1 what is Simmon angle, dx of what?, Meary angle?
- calcaneal pitch how change w/ PTTI, nl=? abn=? 2-young male with young males with mild pes planus may have one of the following 2 conditions? w/o? stage of PTTI IF (+) single-limb heel rise IF xray (+) DJD of subtalar arthritis =? IF talar tilt =?, "too many toes" sign=? 3-what jnt are fused in a triple? what is cotton osteotomy 4-Berndt and Harty Radiographic Classification of? 5-MC fx of ballerina, criteria to ORIF a MT fx(3)? 6-MC injury in a dancer? MC lig injury in low ankle fx, how to Dx? 7-Ottawa ankle rules, goal of PT, single best predictor for return to play |
1-seen AP foot=increased talo-first metatarsal angle, seen pts w/ PTTI, stages 2-4
-seen lat foot=increased talo-first metatarsal angle, seen id PTTI, >4 deg & stages 2-4 -seen Lat foot=decreased calcaneal pitch =PTTI, nl is = 17-32°, indicates loss of arch height=PTTI 2-young male with pes planus=Ddx=seronegative spondyloarthropathy, inflammatory arthropathy w/o=(ESR) or the C-reactive protein (CRP) level is elevated in approximately 75% of patients blood test HLA-B27 –positive -PTTI=(+) can do SLS= stage 1 CAN NOT do THEN=2 "too many toes" sign=2B (+) DJD of subtalar arthritis =3 talar tilt = 4 with deltoid ligament out 3-triple arthrodesis= talocalcaneal (TC), talonavicular (TN), and calcaneocuboid (CC) joints cotton O=Plantarflexion opening wedge medial cuneiform osteotomy 4-Osteochondral Lesions of the Talus 5-base of 2nd MT=ballerina -sagittal plane deformity >10 deg, >4mm translation, multiple fractures 6-ankle sprain, MC lig ATFL, Ant. drawl test in PF 7-cannot wb after injury bony tenderness=medial or lateral malleolus , 5 MT, navicular PT-no swelling, Full ROM THEN neurmuscular training and proprioception training RTP->neg squez test neg synd inj |
|
|
1-define cotton test? hopkins test
2-b/l seasmoiditis what dx? 3-what is the deformity in Hallux valgus defornity, MC complication with navicular fx, tx of nav fx 4-only BMP withOUT osteo inductive property? 5-only BMP associated with Fibrodysplasia ossificans progressiva 6-antalgic gait associated with knee arthritis findings? MC pediatric prosthesis? 7-pt in WC how much increase in Energy is required compared to ambulation in normal subjects? |
1-cotton test=lateral translation of talus in the mortise
hopkin's= squeeze test 2- 3-valgus + pronation, MC COmlpl-> risk AVN, >risk delayed union and non-union, tx SLC NWB x 6-8 wks 4-BMP-3 5-BMP-4 6-knee flexed, toe walking, shortened stride, constant friction (single axis) knee 7-Wheelchair propulsion=9% increase in energy expenditure |
|
|
27-1 what kind of gait did Guy have with his crutches?
2- what is used to initiate platelet activation in the prepared sample of PRP 3-PRP= 4-MCC hypoparathyroidism, findings, Tx? 5-MC etiology of neuropathic shoulder arthropathy, MCC of foot and ankle neuropathic joints? Tx? 6-MoA of myasthenia gravis & botox ? 7-describe 2 muscle fiber types-mn, which cell are first cells to appear following acute muscle injury? |
1-swing-to-gait not swing through gait unless he was moving quickly.
2-calcium chloride used to initiate platelet activation in the prepared sample of PRP 3prp=Platelet rich plasma (PRP) 4-MCC hypoparathroidism=thyroidectomy (including parathyroid), sx-hypocalcemia, neuromuscular irritability, Chvostek's sign,seizures tetany:::Tx-Vit D CA 5-syringomyelia, DM -tx-arthrodesis NOT TJA 6-myasthenia gravis patient has shortage of Ach receptors botox blocks release of Ach from end plate 7-"1 slow fat red ox" & "2 fast skinny white breasts": -slow twitch -lipid accumulation -red fibers -oxidative · Type 2: "2 fast skinny white breasts": -fast twitch -low lipid -white fibers, like chicken breasts 7=MC cells early on after acute muscle injury=neutrophils |
|
|
1=risk of hiv w/blood transfusion?
2=risk of transmission of (HIV) to a health care worker after percutaneous exposure to HIV-infected blood has been estimated as???percent. 3-type of collagen in annulus fibrosis & nucleus pulposus, meniscus & bone 4-nerve which innervates the superficial fibers of annulus? 5-what the aging effect on the ratio of keratin sulfate to chondroitin sulfate? 6-intervertebral discs are biologically responsive and increase their production why? 7-what are predominant cell type in tendon? tendon repairs are weakest at????days |
1=1/500,000 per unit transfused
2-0.3% risk hiv needle stick 3- annulus fibrosis -1 nucleus pulposus-2 meniscus & bone=1 4-DRG gives rise to the sinuvertebral nerve which innervates the superficial fibers of annulus 5-aging increases the ratio of keratin sulfate to chondroitin sulfate 6-when stimulated by interleukin-1 beta 7-fibroblasts are predominant cell type; tendon repairs are weakest at 7-10 days |
|
|
1-Which of the following diagnoses is most likely to result in a malpractice claim?
2-give examples of 5 levels of evidence. 3-mn-AD disorders 4-mn AR disorders 5-mn x-linked recessive 6- example of 2 x-linked Dominate dz 7-mn 50S & 30S Abx, Mannerfelt syndrome, Tx |
1-femoral fracture
2-1=RCT or meta homo 1, 2=(forward) prospective, meta 2; 3=(back) retrospective/meta3/case control;4=case series 5=case report, expert opinion, my expiere 3-AD=>DOMINANT D-Danlos Ehlers syndrome, Dysostosis Cleidocranial:::O-Osteogensis Imperfecta 1&4, Osteochondromatosis, Osteopetrosis (tarda, mild form:::M-Marfan's synd-fibrilin, Metaphyseal chondrodysplasia (Schmid and Jansen types), Malignant hyperthermia, MED (COMP gene - Type II collagen) I- Intermittent Porphyria N-Noonans Symdrome A-Achondroplasia (FGFR3) N-Neuofibromatosis,Neurofibromin 1:::T-Tuberous sclerosis 4-A, B, C, D, E, F, G, H. . . O,P, S, T, W A-alpha 1 antitrypsin deficiency::: B-B thalessemia. C-Cystic fibrosis, CFTR gene, D-Diastrophic Dysplasia (sulfate transporter gene) E-Enzyme deficiencies (glycogen storage and lysosomal storage) F-Friedrich's ataxia, frataxin:::G-Gaucher dz, H-Hypo-phosphasia. . .O-Ostogenis imperfecta 2&3 Osteopetrosis P-PKU S-Sickle Cell Dz, SMA T-Tay Sachs Dz, W- wilson's dz 5-XLR=Less hCG is Detected Clinically in A Fragile Women" Less : lesch nyhan syndrome. h : hemophilia a , hunter syndrome. C : chronic granulomatous disease. G is : g6pd degiciency Detected : duchene DO NOT MAKE muscular dystrophy, diabetes insipidus Becker's MD BADLY MADE less Clinically in : color blindness. A : agammaglobulinemia Fragile : fragile x syndrome Women : wiskott aldrich syndrome 6-Hypo-phospatasia rickets, Leri-Weill dyschondrosteosis (bilateral Madelung's deformity) 7-CLEAn TAG CLEAn-50S C-Chloramphenicol L-Lincomycin (CL=CLindamycin) E-Erythromycin A-Azithromycin TAG-30S T-Tetraclycine A-AminoGlycosides CLEAn-50S C-Chloramphenicol L-Lincomycin (CL=CLindamycin) E-Erythromycin A-Azithromycin TAG-30S T-Tetraclycine A-AminoGlycosid Mannerfelt syndrome=rupture of FPL (most common flexor rupture) in carpal tunnel due to scaphoid osteophytes treatment FDS to FPL tendon transfer |
|
|
1-bacteriostatic vs. bactericidal mn
2-(3) MoA of Abx? 3-Genetic mutation of ??? gene encoding a penicillin-binding protein (PBP) 4-s/p Splenectomy patients require the following vaccines and/or antibiotics (4)??mn 5-Which of the following species of bacteria are known to produce mecA? MoA of mecA gene? 6- Which class of antibiotics inhibit early fracture healing through toxic effects on chondrocytes? 7-What is an appropriate choice of prophylactic antibiotics to be taken prior to dental work if he has no allergies? |
1-bacteriostatic=We're ECSTaTiC about bacterioSTATIC (6)
E-Erythromycin, C-Clindamycin, S-Sulphonamides, T-Tetratcyclines, T-Trimethoprim, C-Chloramphenicol) bactericidal=Very Finely Proficient At Cell Murder (6) V-Vancomycin, F-Fluoroquinolones, P-Penicillins, A-Aminoglycosides, C-Cephalosporins, M-Metronidazole) 2-(1)CELL WALL synthesis & cell membrane synthesis:Beta-lactamase Inhibitors= (bactericidal: blocking cross linking), vanco= (bactericidal: disrupts peptioglycan cross-linkage) bacitraicin, (2)Bacterial PROTEIN synthesis:50s Macrolides (bacteriostatic: reversibly binds 50S), Chloramphenico & 30s=Aminoglycosides (bactericidal: irreversible binding to 30S) & Tetracyclines=(bacteriostatic: blocks tRNA) (3)NUCLEIC ACID sythnesis:DNA gyrace(Quinolones), RNA polymerase (Rafampin), Folic Acid=S & Mycolic Acid Inhib=Ison 3-Genetic mutation of mecA=>encoding a penicillin-binding protein. 4=s/p Splenectomy patients require the following vaccines and/or antibiotics ?? s/p spenectomy=PIMPE P-(1)Pneumococcal immunization I-(2)haemophilus Influenza type B vaccine M-(3)Meningococcal group C conjugate vaccine P-(4)Lifelong prophylactic antibiotics (oral phenoxymethylpenicillin (Penicillin/Beta-lactamase) or Erythromycin=(Very Finely Proficient At Cell Murder & ECSTaTiC-bacteriostatic NOT Hepatitis A vaccine. 5- Methicillin-Resistant Staphylococcus Aureus,(MRSA) -bacterial gene which encodes for a penicillin-binding protein that alters the efficacy of beta-lactam antibiotics penicillians 6-quinolones 7-beta lactam/penecillian, 2 grams of Amoxicillin, Cephalexin, or Cephadrine, by mouth one hour prior to the dental procedure. IV antibiotics are very rarely used in dental offices. If allergic to penicillin, clindamycin would be the next best alternative. |
|
|
1-mn-DMARDs, mn bactericidal & bactericidal
2-MoA & classification of: Vancomycin- Beta-lactamase Inhibitors Aminoglycosides Tetracyclines Macrolides Lincosamide Metronidazole Rifampin Trimethoprim/Sulfonamides Linezolid 3-mn rheumatoid arthritis 4-Management mn-RA 5-MC form of inflammatory arthritis 6-primary cellular mediator of tissue destruction in RA 7-most common flexor rupture w/RA, Tx? |
1-DMARDs (Disease-Modifying Anti-Rheumatic Drugs),
-We're ECSTaTiC about bacterioSTATIC (6) & Very Finely Proficient At Cell Murder (6) V-Vancomycin =(bactericidal: disrupts peptioglycan cross-linkage) F-Fluoroquinolones=(NUCLEIC ACID sythnesis:DNA gyrace(Quinolones) Beta-lactamase Inhibitors=(bactericidal: blocking cross linking) Aminoglycosides=(bactericidal: irreversible binding to 30S) Tetracyclines=(bacteriostatic: blocks tRNA) 30s Macrolides=(bacteriostatic: reversibly binds 50S) Lincosamide=(bacteriostatic: inhibits peptidyl transferase by interfering with amino acyl-tRNA complex) 50s Metronidazole=(bacteridical: metabolic biproducts disrupt DNA) Rifampin=(bactericidal: inhibits RNA transcription by inhibiting RNA polymerase) Trimethoprim/Sulfonamides=(bacteriostatic: inhibition with PABA) Linezolid binds to the 23S portion of the 50S subunit and acts by preventing the formation of the initiation complex between the the 30S and 50S subunits of the ribosome. 2-: RHEUMATISM R Rheumatoid factor (RF) +ve in 80%/Radial deviation of wrist H HLA-DR1 and DR-4 E ESR/Extra-articular features (restrictive lung disease, subcutaneous nodules) U Ulnar deviation of fingers M Morning stiffness/MCP+PIP joint swelling A Ankylosis/Atlanto–axial joint subluxation/Autoimmune/ANA +ve in 30% T T-cells (CD4)/TNF I Inflammatory synovial tissue (pannus)/IL-1 S Swan-neck deformity, Boutonniere deformity, Z-deformity of thumb M Muscle wastage of small muscles of hand 3-Management DMARDs (Disease-Modifying Anti-Rheumatic Drugs) Mnemonic: Most Sufferers Can Get Appropriate Pain Control M-Methotrexate S- Sulfasalazine C- Ciclosporin G- Gold A- Azathioprine P- Penicillamine C HydroxyChloroquine 5-RA 6-B cell 7-Mannerfelt syndrome=rupture of FPL in carpal tunnel due to scaphoid osteophytes tx FDS to FPL tendon transfer |
|
|
1-Vaughan-Jackson syndrome, tx?
2-Caput-ulna syndrome, tx? 3-classic xray findings shoulder w/ RA vs OA (3) 4-what is the most significant risk factor for development of SSI surgical site infection 5-surgery should be performed in RA when immunosuppressive agents are at what level, ex ?? 6-Type I:& Type II: errors 7-Dietary requirements CA ??mg/day for lactating women ???mg/day for pregnant women, postemenopausal woman, and patients with a healing bone fracture ?//mg/day for adolescents and young adults ???mg/day for adults ??/ mg/day for children Dietary intake PO4=??/ mg/day active hormone form vit d? mn |
1=EDM out, describes the rupture of the hand digital extensor tendons which occur from the ulnar side of the wrist first then moves radially
tx=EIP to EDC transfer and distal ulna resection 2-Caput-ulna syndrome=synovitis in the DRUJ > ECU subsheath stretching > ECU subluxation > supination of the carpal bones away from the head of the ulna > volar subluxation of the carpus away from the ulna > increased pressure over the extensor compartments > tendon rupture tx=distal ulna resection (Darrach) must also relocate ECU dorsally with a retinacular flap or perform ECU stabilization of ulna Sauvé-Kapandji ulnar pseudoarthrosis has advantage of preserving the TFCC good option for younger patients 3=classic xray=central glenoid wear, periarticular osteopenia, cystsvs OA=Joint space narrowing and development of osteophytes posterior & inferior wear 4-hx of prior surgical site infection (SSI) 5-surgery should be performed when immunosuppressive agents are at their lowest levels=etanercept should be discontinued 3 days prior to surgical procedures adalimumab should be discontinued 10 days prior to surgery the lowest level of infliximab is found 2 weeks prior to the next scheduled infusion 6-Type I: "I falsely think hypothesis is true" (one false) Type II: "I falsely think hypothesis is false" (two falses) accepting the null hypothesis when it is in fact not true 7-Dietary requirements (knees 2x nl + almost a child 750 x2 + 500 ) 2000 mg/day for lactating women (tail x2 nl adult) 1500 mg/day for pregnant women, post-menopausal woman, and pts w/ a healing bone fx (dummy)1300 mg/day for adolescents and young adults (coal or 1/2 prge)750 mg/day for adults (shore) 600 mg/day for children -Dietary intake po4=1400 1000-1500 mg/day -1,25-(OH)2-vitamin D3 (3,2,1)=600 IU for those 1-70 years of age and pregnant or breastfeeding women, and 800 IU for those over 71 years of age. |
|
|
1-bugs killed, Mokill
2-examples of drugs in categories 3-unique quality |
1
|
|
|
34-1 anatomic pathway of the ilioinguinal nerve?
2Passes under the inguinal ligament and over the sartorius muscle into the thigh, where it divides into an anterior and a posterior branch 3 Perforates the posterior part of the transversus abdominis and divides the obliquus internus abdominis branching into a lateral and an anterior cutaneous branch 4-mn lumbar plexes (6) 5-Thigh: innervation by compartment-mn 6-Sacral plexus: posterior components-mn 7-10 types of acetabular fx, piriformis will provide a landmark leading to the ??? see on xray, MC w/each |
1-Pierces the obliquus internus and then accompanies the spermatic cord or round ligament through the superficial inguinal ring
2-lateral femoral cutaneous nerve. 3-iliohypogastric nerve. 4-I 2x Get Laid On Fridays" "2 from 1, 2 from 2, 2 from 3": Iliohypogastric [L1] Ilioinguinal [L1] Genitofemoral [L1, L2] Lateral femoral cutaneous [L2, L3] Obtruator [L2, L3, L4] Femoral [L2, L3, L4] 5-MAP OF Sciatic": Medial comp: Obturator Anterior comp: Femoral Posterior comp: Sciatic 6-Sacral plexus: posterior components "Common GLUttons For Punishment": C-Common fibular GLU-Gluteals (superior and inferior) F-Femoral cutaneous (Posterior) P-Piriformis nerve 7-AC/AW/PC/PW/Tr "T"/Tr+PW/PE + PC/AC +1/2 Tr-Pos/ AC+PC=BC -piriformis will provide a landmark ->greater sciatic notch |
|
|
1-if it is cut and retracts into the pelvis, then treat by flipping patient, open abdomen, and tie off internal iliac artery?
2-at risk of injury with release of gluteus maximus insertion? 3-at risk with failure to protect anterior aspect of the acetabulum, or with placement of retractors anterior to the iliopsoas muscle? 4-excessive retraction and injury must be avoided to prevent damage to medial circumflex artery 5-Structures passing through greater sciatic foramen below pyriformis muscle? mn 6-highest rate of heterotopic bone formation of all pelvic approaches? 7-Permanent hip abductor weakness is expected? which fx see gull sign & spur sign on Obturator oblique view of pelvis |
1-Inferior gluteal artery
2-First perforating branch of profunda femoris 3-Femoral vessels 4-Quadratus femoris 5-" PIN & PINS " Structures passing through greater sciatic foramen below pyriformis muscle: P-Posterior cutaneous nerve of thigh I-Inferior gluteal vessels and nerves N-Nerve to quadratus femoris P-Pudendal nerve I-Internal pudendal vessels N-Nerve to obturator internus S-Sciatic nerve 6-Extensile (extended iliofemoral) 7-Extensile (extended iliofemoral gull-post wall spur-both column |
|
|
1-Internervous plane anterior approach hip?
2-name of anterior approach to hip? 3-indication for medial approach to hip? 4-3 names of posterior approach to hip/acetabulum? 5-vessel most at risk with medial approach to hip? 6-MC acetebular fx seen in elderly from standing fall? MC fx with gull sign? MC fx with spur sign? only fx that is not both columns? MC fx pattern to need combined approach? MC to injure the sup. gluteal nerve 7-if see basal ganglion calcification think what dz? |
1-femoral n & superior gluteal nerve
2-smith Peterson approach 3-ORIF of congenital hip dislocation psoas release 4-Southern/Moore approach and the Kocher-Langenbeck- 5- medial femoral circumflex artery 6-Ant Colm, Post wall on OOV, Both columnm, PC & PW, T pattern, PC 7-hypoparathrodism |
|
|
1 name the 4 approaches to acetabulem? risk w each? when do you use it/them?
2-effects of hypo-parathyroidism? 3-Proliferative Zone of physis effected? 4-Reserve Zone of physis effected? 5-Primary Spongiosa (metaphysis) of physis effected? 6-which approach puts the lateral femoral circumflex artery and medial femoral circumflex artery at risk? 7- A patient with chronic renal disease would expect which of the following endocrine abnormalities? |
1-modified Stoppa app-medial wall quadrilater plate, risk corona mortis
-illio Inguinal app-Anterior-RISK=corna mortis, FN, LFCN, FA-thrombos;AC/AW/X/X/X X/X/X/Ac +1/2Tr-P/B -Kocher-Langenback-POSTERIOR -RISK=HO, SN, MFCA:X/X/PC/PW/Tr "T"/X/X/X/X -Extended iliofemoral -RISK=MASSIVE HO, GM necrosis:X/X/X/X/Tr "T"/X/X/X/B 2-decreased-PTH, calcium, 1,25-Vit D, urinary calcium nl-alk phos 3-Achondroplasia, Gigantism, MHE 4-Gaucher's, diastrophic dysplasia, Kneist* Pseudoachondroplasia* 5-Metaphyseal "corner fracture" in child abuse Scurvy 6-MFCA-Medial app when performing Tenotomy of iliopsoas muscle LFCA=Anterior-Smith-Petersen approach to the hip 7- Increased production of PTH |
|
|
38-1When approaching a proximal diaphyseal radius fracture via the (volar) approach, the forearm is supinated to minimize injury to what structure? AKA appr
2- Which approaches for THA is reported to have the lowest prosthetic dislocation rate? 3-Hip Direct Lateral Approach, AKA? at risk structures? 4-Hip Posterior Approach AKA-3? at risk structures? 5-Does the mini-incision approach shows no long-term benefits to hip function 6- Where is the origin of the muscle located between the anterior acetabulum and iliac vessels? 7-The medial femoral circumflex artery and first perforating branch of the profunda femoris artery anastamose at which of the following locations? |
1-Posterior interosseus nerve, Henry App
2-Harding app, Transgluteal has lower rate of THA dislocations, 3-Harding app -SGN split fibers of gluteus medius do not extend more than 3-5 cm above greater trochanter to prevent injury to superior gluteal nerve -Femoral nerve=most lateral structure in neurovascular bundle of anterior thigh, keep retractors on bone with no soft tissue under to prevent iatrogenic injury 4-Hip Posterior App AKA (Moore, Southern, Kocher-Langenbeck=more extensile exposure used for complicated acetabular work) 5-NO 6- Lumbar transverse processes 7- Medial to the gluteus maximus insertion |
|
39-1-what nerve and A are located above joint runs between EDL and EHL, crosses behind EHL at level of the joint
2-(5) at risk with Ankle Posterolateral Approach? 3-What is the active form of Vit D? 4-delays differentiation of chondrocytes in the zone of hypertrophy involved what transcription factor? 5-mn-mn for proliferative Zoneof physis? 6-primary ossification centers form (at?? wks) 7-what kind of bone healing :casting and bracing, Ex-fix, IM nailing, ridge fixation define ??? |
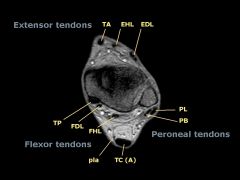
1-Deep pereonal N & anterior tibial artery)
2-(1)care must be taken not to release the PITFL off the fragment, devitalizes posterior malleolar fragment, can lead to post-fixation syndesmotic instability (2)Superficial peroneal N=at risk with superficial dissection proximally (3)Posterior tibial vessels=should remain protected behind FHL (4)Tibial N-should remain protected behind FHL (5)Sural nerve=at risk with further dissection distally 3--D3 or 1,25-dihydroxy-cholecalciferol (calcitriol) 1,25-dihydroxyvitamin D 4-PTHrP 5-MAGy get BIG andPROLIFERATES=M-MHE A-Acholdroplasia, G-Gigantism 6-1^O cntr=(at ~ 8 weeks) 7-Cast/brace=Secondary: enchondral ossification Ex-fix=Secondary: enchondral ossification IM nailing=Secondary: enchondral ossification & intramembranous Compression plate =Primary: Haversian remodeling |
|
|
40-1-groove of Ranvier. What is this region of the growth plate responsible for?
2-Salter-Harris type I fractures typically occur through which zone of the physis? 3-What region of the physis does collagen type X play a prominent role? MCC w/ distal 1/3 tibia fx 4-MC long bone fx, risk of ??? with oblique fracture patterns, risk of ??? with midshaft tibia fx & an intact fibula 5-reamed nails associated w/ (3) advantages? 6-most important predictor of infection w/ open fx?, -most important predictor of eventual amputation is? 7-which treatment has been shown to have 92-96% union rate after open tibial fractures initially treated with external fixation; best treatment of nonunion atrophic tibia non-invasive & invasative, hypertrophic nonunion |
1-Appositional bone growth
2-MC- zone of provisional calcification 3-10-hypertrophioc zone--Rickets zone, rational malunion 4-tibia fx, oblique fx=shorting, intact fibula tib fx=varus malunion 5-reamed nails associated w/ 1decreased hardware failure, 2superior union rate, 3decrease time to union 6-most important predictor of infection is transfer to definitive trauma center -most important predictor of eventual amputation is the severity of ipsilateral extremity soft tissue injury 7-compression plating; non-invasive techniques (electrical stimulation, US), BMP-7 (OP-1) has been shown equivalent to autograft hypertrophic nonunion=exchanged reamed nail |
|
|
41:1-MC malunion after IM nailing of distal 1/3 fx?
how to assess tibial rotation 2-compartment pressure, what is most sensitive diagnostic test? 3-MC reason for successful malpractice litigation against orthopaedic surgeons 4-CC-common complication seen p/ closed nailing, how to ***** nerve injury in tibia? 5-MCC w/ long plate on tibia, pts c/o of what clinically? 6-Which of the following tibial injuries is most commonly treated with staged open reduction and internal fixation with free flap soft tissue reconstruction? 7-How to differentiate ulnar tunnel syndrome from cubital tunnel syndrome? |
1-rotational, by obtaining perfect lateral fluoroscopic image of knee, then rotating c-arm 105-110 degrees to obtain mortise view of ipsilateral ankle
2-most sensitive diagnostic test=compartment pressure within 30mm Hg of diastolic BP is 3-failure to recognize and tx compartment syndrome 4-transient peroneal nerve palsy, EHL weakness and 1st dorsal webspace decreased sensation 5-SPN, c/o of numbness along the dorsum of her medial and lateral foot. 6-Type IIIB intra-articular distal tibia fracture 7-How to differentiate ulnar tunnel syndrome from cubital tunnel syndrome cubital tunnel demonstrates less clawing sensory deficit to dorsum of the hand motor deficit to ulnar-innervated extrinsic muscles Tinel sign at the elbow positive elbow flexion test |
|
42:1-what is Wartenberg sign, Allen test
2-Jeane's sign 3-Froment sign 4-Commonly known as "wind knocked out" AKA, Tx? 5-MCC of death because of an abdominal injury? MC organ injured in the abdomen as the result of blunt trauma? 6-MC organ blount trauma need urgent surgery? 7-(Kehr's sign), CI to surgicaly tx Pitcher's Elbow |
1-abduction posturing of the little finger, Allen test
helps diagnose ulnar artery thrombosis 2-Jeane's sign=a compensatory thumb MCP hyperextension and thumb adduction by EPL (radial n.), compensates for loss of IP extension and thumb adduction by adductor pollicis 3-Froment sign =IP flexion compensating for loss of thumb adduction when attempting to hold a piece of paper, loss of MCP flexion and adduction by adductor pollicis (ulnar n.) compensatory IP hyperflexion by FPL (AIN) 4-Diaphragmatic Spasm, observ 5-Spleen Injuries x2 6-renal, extensive bleeding with renal fx or vascular pedicle injury 7-Splenic injuries may present with pain referred to the shoulder, CI=valgus instability of elbow |
|
|
43:1-MC location of injury in pitchers elbow, which side of the olecranon fossa?
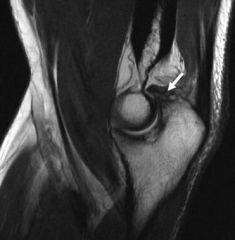
2-incidence ??? % infection rate following traumatic fracture 3-define involulcrum & sequestrum 4-"flake sign" on lateral view of elbow=? 5-how does TSA differ from THA? 6-#1 factor for successful TSA? 7-when is glenoid resurfacing is CI |
1-osteophyte formation in the posteromedial olecranon fossa
2-16% 3-involulcrum-envelope, reactive bone surrounding active infection sequestrum-dead bone 4=tricepts rupture 5-glenoid is less constrained-leads to greater sheer stresses and is more susceptible to mechanical loosening 6-#1=rotator cuff intact and functional, but an isolated supraspinatus tear without retraction can proceed with TSA 7-CI=if glenoid is eroded down to coracoid process |
|
|
44:1 Walch classification if for & describe?
2-CI to TSA?(7) 3-MCC in TSA, how to ***** for it? 4-limiting factor in early posto rehabilitation p/ TSA 5-MCCC of TSA failure (30% of primary OA revisions) 6- nl version of the glenoid=??? total shoulder the goal should be to place the glenoid component in??? 7-Common organism unique to cause indolent infection in TSA? |
1-Walch Classification of Glenoid Wear
Type A well-centered, A1 minor erosion, A2 deeper central erosion Type B head subluxated posteriorly, B1 posterior wear, B2 severe biconcave wear Type C glenoid retroversion of> 25 deg (dysplastic in origin) 2-CI=(1)insufficient glenoid bone stock, if glenoid is eroded down to coracoid process; (2)rotator cuff arthropathy;(3) deltoid dysfunction(4)irreparable RC (hemiarthroplasty or revTSA are preferable) (5) risk of loosening of the glenoid prosthesis is high ("rocking horse" phenomenon)(6)active infection (7)brachial plexus palsy 3-axillary nerve injury, Hornblower's test indicates teres minor pathology=shoulder placed in 90 deg of abd, 90 deg of ER, positive if patient falls into internal rotation lack of sensation over the lateral deltoid -risk of injury to the subscapularis tendon repair, Limit passive external rotation, weak belly-press test 5-MCCC=glenoid loosening 6- nl version of the glenoid=0-3 deg of retroversion, TSA= neutral to slight anteversion 7-Propionibacterium acnes (P. acnes) high bacterial burden around the shoulder common cause of indolent infections and implant failures |
|
|
45:1-Irreparable rotator cuff tear Tx
2-indication for PS TKA 3-GCS-mn, when to intubate? 4-Green Classification for 5-MC location of trigger finger? 6-TUBS-mn 7-Anterior static shoulder stability is provided by 3 lig? |
1-hemi, RTA NOT TSA bc/ superior glenoid (the "rocking horse” phenomenon) which may loosen the glenoid componen, BUT IF THE CUFF is repairable TSA is not a CI
2-previous patellectomy, RA/inflammA, NO PCL 3- If they're <8, they intubate! GCS (4 eyes V roman numeral 5 Motor 6cyclders) E.Y.E.S. = 4 letters E = Eyes shut (negative response) Y = "Y" is shaped like a spike or a barb (pain) E = Explosion (sound) 4-S = Spontaneous eye opening Vocal --> V -->( V.O.W.E.L. = 5 letters) V = Voiceless O = Ouhmnmh... (sounds; moaning; no words) W = Words (random words) E = Erratic/incomprehensible speech-(confused; misunderstands reality L5 = Legit speech M.O.B.I.L.E. = 6 letters M = Motionless O2 = Overextends to pain (decErebrate response - extended arms, legs; toes pointing downward; head arching backward) DECEREBRATE posturing, it is abnormal extension. Their hands look like the flippers of a seal - Think DESEALEBRATE! B = Bends/flexes to pain (decorticate response - flexed arms, clenched fists, extended legs) I = Ilude & Withdraw from pain L = Localizes pain 6E = Executes/obeys command 4-trigger finger, Grade I Palm pain and tenderness at A-1 pulley Grade II Catching of digit Grade III Locking of digit, passively correctable Grade IV Fixed, locked digit 5- ring finger 6-TUBS (Traumatic Unilateral dislocations with a Bankart lesion requiring Surgery) 7-Anterior static shoulder stability is provided by ant band of IGHL=provides static restraint with arm in 90° of abduction and external rotation MGHL=provides static restraint with arm in 45° of abd & ER SGHL=provides static restraint with arm at the side |
|
|
46-1-Bristow and Latarjet Procedure describe, indication
2-putti-plat procedure & Magnuson-Stack 3- Bankart lesion(mn), or avulsion of the ?? which part of the glenohumeral ligament is adjacent to the? 4-nl glenoid retroversion 5-primary restriction motion during PT after (TSA) is?? 6-what causes the "rocking horse” phenomenon after a TSA |
1-Bristow and Latarjet Procedure-h detachment of the tip of the coracoid and its transfer to the glenoid, bony deficiencies with >20% glenoid deficiency
2-Putti-Platt is performed by lateral advancement of subscapularis and medial advancement of the shoulder capsule Magnuson-Stack is performed with lateral advancement of subscapularis (lateral to bicipital groove and at times to greater tuberosity 3- mn-bankart is boney glenoid and below glenoid, Bankart lesion, or avulsion of the anteroinferior fibrocartilaginous labrum adjacent to the -IGH, 1st-time traumatic shoulder dislocation with Bankart lesion confirmed by MRI in athlete younger than 25 years of age 4-0-3 deg 5-primary restriction after (TSA) is passive ER, as well as active IR, to protect the subscapularis repair during the first 6 weeks. 6-irreparble cuff tear causing sup. migration of the prosthesis head levering on the superior glenoid loosing of the component |
|
|
47-1-which type of tibial Plateau fx MC injury to:
med men tear, lat men tear, ACL, comp syndrome? 2-which Plateau is proximal, which is distal 3-Hohl and Moore Classification of proximal tibia fracture-dislocations, when is it useful for? why use it? 4-lipohemarthrosis 5-ORIF indications tibial pleateau fx (5) & worse out expected if (3)6 how far from jnt surface are wires with tib pleat ex fix? 6-fill metaphyseal void with tib pleauteau fx? 7-most significantly increase rate of DJD in the long-term? |
1-MC mmt-->Schatzker 4
lmt->Schatzker 2 peripheral meniscal tears. ACL-Schatzker 5 & 6 comp syndrmd=4 high E 2-lat-proximal & convex med-distal & concave 3-Type I Coronal split fx Type II Entire condylar fx Type III Rim avulsion fracture of lateral plateau Tpe IV Rim compression fracture Type V Four-part fracture Classification useful for 1) true fracture-dislocations & fractures associated with knee instability 2) fracture patterns that do not fit into the Schatzker classification (10% of all tibial plateau fractures) 4-lipohemarthrosis on CT=fat in blood = fracture 5-(1)articular stepoff > 3mm (2)condylar widening > 5mm (3)varus/valgus instability (4)all medial plateau fxs (5)all bicondylar fxs -worse results=ligamentous instability, meniscectomy, alteration of limb mechanical axis > 5 deg 5-must keep wires >14mm from joint or 1.4 cm 6-fill metaphyseal void w/ calcium phosphate cement has high compressive strength for filling metaphyseal void 7-most significantly increase rate of DJD=Alteration of limb mechanical axis >5 inc DJD (27%) |
|
|
48-1-what is Jones classification used for?
2-treatment of tibia hemiamiliea is 1^ based on what? what direction is the bowing of the leg? 3-in tibia hemiamilia how is the foot affected? 4- how to tell difference between triplaner and tillaux fx, Tx of Tillaux Fractures, MoI? 5-what is the Meyers and McKeever Classification used for? MCC with surgery 6-define & Tx-Maisonneuve fx, Tillaux fx, Pott's fx, Cotton's fx, Snowboarder's fx 7-MCC w/tibial tubericale fx? Ogden Classification (modification of Watson-Jones) |
1-Jones class=complete abs of tibia & partial absence of tibia further divided= proximal, distal, ankle diastasis
2 1^ if the quad intact extensor mechanism minimal flexion contracture TX with mod syme amputation tib/fib synostosis vs NO KNEE EXTENSION then knee disarticulation followed by prosthestic fitting -bow is Ant/lat 3-foot deformity=there is often a rigid equinovarus and supination deformity of the foot, sole of foot faces perineum 4-tillaux=lack of fracture component in the coronal plane distinguishes this fracture from a triplane injury Tx-if <2 mm THEN CR w/ LLC x 4 wks, SLC x 2-3 weeks RARE MC Tx IF > 2 mm THEN ORIF MoI=AITF avultion salter 3 NO coronal fx 5-tibial eminence fx, attachment of ACL, MCC=arthrofibosis Type I Nondisplaced Type II Minimally displaced with intact posterior hinge Type III Completely displaced 6-Maisonneuve fx=med mal with prox fibula fx, ORIF syndesmosis injury present Tillaux fx=salter harris 3, avulsion of AITF fx, ORIF >2 mm Pott's fx-bi malleolar fx, ORIF Cotton's fx-3 malleolar(trimalleolar) fx ORIF Snowboarder's fx-2^ dorsiflexion and inversion of the ankle -> Lateral Talar Process Fx ND fx in SLC x 4-6 wks; most ORIF need CT order to see fx, difficult to see on xray 7-recurrent anterior tibial artery can be torn with these injuries 2^ compartment syndrome Ogden Classification (modification of Watson-Jones) Type I fx of the secondary ossification center near the insertion of the patellar tendon Type II fx propagates to proximal to the junction with the primary ossification center Type III fx extend posteriorly to cross the primary ossification center Modifier: A (nondisplaced), B (displaced) Type 4 is a fracture through the entire proximal tibial physis Type 5 is a periosteal avulsion of the extensor mechanism from the secondary ossification center |
|
|
49-1 Tibial Plafond Fractures, aka?
2-name the 3 fragments typical in pilon & name of intact ankle ligaments in pilon fx 3- regarding brake travel time after surgical treatment of complex lower extremity trauma-both long bone and articular fractures of the right lower extremity? 4-aspirate WBC count >??? with > ??% PML should raise suspicion infection in TKA? 5-Overall incidence??? o fTKA infection 6-common complication w/ with PCL-retaining designs TKA, Tx of patellar tendon rupture? 7-preoperative valgus and/or flexion deformity higher risk of? Most import factor for prediciting post-op stiffness? |
1 plafond=pilon fractures
2-3 fragments typical with intact ankle lig, medial malleolar (deltoid ligament), anterolateral/Chaput fragment (anterior inferior tibiofibular ligament) mn-Kick the Cat then Later Chop it, posterolateral/Volkmann fragment (posterior inferior tibiofibular ligament), 3- Brake travel time is significantly increased until 6 weeks after patient begins weight bearing 4-aspirate WBC count> 11,000 PML>60% 5-1% 6-flexion gap, tx CR TKA; reconstruction with an Achilles tendon/bone allograft 7-valgus>12 deg,m increased risk for peroneal nerve palsy, preoperative stiffness, preoperative motion +/- 10° |
|
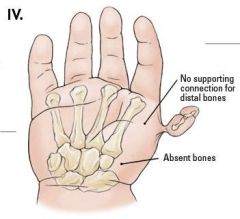
50-1=MC offending agent hypersensitivity reaction p/ TKA
2-stress fracture locations has the greatest likelihood of delayed healing or developing a non-union? 3-4 what test should be order if pt w/congential hyopplastic thumb ? what does VAC-TER-L 4-Treatment algorithm of hyplastic thumb depends on what? what is name of the classification system for thumd hypo, describe 5- who get tx w/ pollitization? 6-characteristics of toddler's fracture & Tx, MC complication |
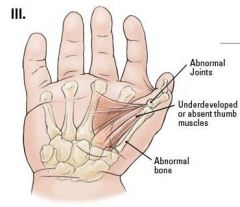
1-nickel-> cobalt-chromium alloys is the MC offending agent
2- Anterior cortex of tibia 3-US kidneys R/o VACTERL= V-Vertebral anomalies, A-Anal atresia, C-Cardiac defects, T-Tracheoesophageal fistula and/or E-Esophageal atresia, R-Renal & Radial anomalies and L-Limb defects. echocardiography r/o Holt-Oramm, CBC r/o thrombocytopenia-absent radius (TAR), CBC r/o Fanconi anemia chromosomal challenge test 4-CMC jnt, Blauth Classification 5-IIIB, IV, V hypoplasia 6-ND tibia spiral/oblique fx with intact fibula in children< 3 years > 1 yr 12 months; LLC w/knee flexed, complication=varus NOT fibula fx, valgus if fibula fx'ed |
|
|
51-1 activities that are ok p/TJR & effect of TKR on golf game?
2-MC & Commn technique to reduces risk of intraoperative fx? 3-intraoperative longitudinal calcar split Tx? 4-THA w/ fx loose vs stable vs comminuted? classification-mn 5-Acetabular Screw Placement and Safe Zones 6-Leaving the anterior rim of the acetabular component proud above the native acetabulum may result in ?? 7-Smith-Peterson approach to the hip uses a surgical plane between which of the following superficial muscles? |
1-ok p/ TJA=Walking, Swimming, Golf, Yoga, Doubles Tennis, Rowing, Weightlifting, Cycling, Calisthenics help build up strength while increasing flexibility. These include crunches, push-ups, and lunges, Elliptical Machines, Bowling, Dancing.
-(1)TKA and found that they invariably experienced a significant rise in their handicap (mean +4.6 strokes) (2)decrease in the length of their drives. (3)Approxiy 15% experienced a mild ache while playing, & (5) that statistically significant increased pain ratings occur in golfers with a TKA on the target-side knee. & (4)golfers with Left TKA's had > difficulty with pain during and after play than did golfers with R TKA's. (6)almost 90% of the patients in this study utilized a cart while playing post-operatively. 2-MC preop templating & adequate surgical exposure, special care when using cementless prosthesis in poor bone (RA, osteoporosis) 3-stem removal, cabling, and reinsertion 4-(mn B2 LOOSE then TWO Tx= ( bone + LONG stem uncemented extensively porous coated femoral component). must bypass the most distal cortical deficiency by two cortices. B1 (stable- ONE Tx=the bone fracture only) ORIF using cerclage cables and locking plates B3 (LOOSE/comminuted=(Tx all 3 (bone + LONG stem + biplanar strut grafts or megaprosthesis) or osteoporotic- prox fem (Allograft & strut graft)/proximal femoral replacement/long, cementless revision stem with biplanar strut grafts 5PS-post sup-safe zone-elevating the hip center in revisions can place sciatic nerve at risk in this quadrant PI-Pos Inf-caution Zone->if screw > 20mm the following structures are at risk: sciatic nerve inferior gluteal nerve and vessles; internal pudendal nerve and vessels AI-danger zone=obturator nerve, artery, and vein at risk AS-death zone=external iliac vessels at risk 6-Leaving the anterior rim of the acetabular component proud above the native acetabulum =>t in anterior iliopsoas tendon impingement 7-Sartorious and tensor fascia lata |
|
|
52-1-Who is credited with the design of the first hemiarthroplasty?
2-is there proven cancer link metel on metal THA? what pt's are Metal on metal CI? (3) 3-best wear properties of all bearing surfaces? 4-DISH stands for? define Dish, aka? DDx? 5-Mortality, for cervical spine trauma in DISH 6-? for those treated operatively 7-? for those treated nonoperatively |
1st hemiarthroplasty=Austin-Moore
2-no proven cancer link, CI= in pregnant women, renal disease, and metal hypersensitivity due to metal ions 3-ceramic on ceramic 4-DISH (Diffuse Idiopathic Skeletal Hyperostosis) -defined by presence of non-marginal syndesmophytes at three successive levels (involving 4 contiguous vertebrae) absence of facet-joint ankylosis; absence of SI joint erosion, sclerosis or intraarticular osseous fusion -"Flowing candle wax"=DISH; "Bamboo spine" AS 5-Mortality for cervical spine trauma in DISH 15% for those treated operatively 67% for those treated nonoperatively AKA Forestier dz |
|
|
53-1- talus serves as origin of the ??? muscle belly
2-(most important and main supply of the talus? 3-Hawkins sign (lucency) indications???, no hawkins =? 4-which nerve MC affected (80%) in THA complication? 5--risk factors, for motor nerve palsies= pt factors & technical(6) 6-% recover full strength after complete sciatic palsy 7-what is MC reason for litigation following THA?, increasing neck length & increasing femoral offset effect on LLD? |
1- talus =EDB muscle belly
2-posterior tibial artery->via artery of tarsal canal 3-Hawkins sign (lucency)=> revascularizatio NO hawkins=AVN 4-peroneal division of sciatic nerve affected (80%) 5--risk factors, for motor nerve palsies= pt factors-(1) DDH, (2) F gender (3) post-traumatic DJD technical- (1)revision surgery, (2)limb lengthening , (3)surgeon self-rated procedure as difficult 6-only 35% to 40% recover full strength after complete palsy 7-LLD,: increasing neck length >LLD increasing femoral offset = NO increase LLD |
|
|
54-1-risk factors for HO after THA?
2-if pt trendelenburg gate which side involved, which approach MCC? 3-create cement mantle at least ???mm thick 4-optimal characteristics of porous coating 5-hydroxyapatite (HA) chemical formula? 6-Terrible Triad Injury of Elbow define medial or lateral, how to Tx? 7-which bundle most important to stability, restraint to valgus and posteromedial rotatory instability -which ligament in elbow restraint to varus and posterolateral rotatory instability |
1-risk factors=prolonged surgical time,
excessive soft tissue handling during procedure hypertrophic osteoarthritis, male gender 2-Insufficiency of the gluteus medius to support the torso in an erect position, indicating weakness in the muscle of decreased innervation.modified Hardinge approach 3-2mm 4-preferably 50-150um 5-Ca10(PO4)6 (OH)2 6- unstable radial head fx, a type III coronoid fx, & an assoc elbow dislocation w/ LCL rupture tx= radial head arthroplasty, coronoid open reduction internal fixation, and lateral collateral ligament repair 7anterior bundle, lateral collateral ligament |
|
|
55-1-immobilize elbow in??? with forearm ??? to provide stability against posterior subluxation
2- At the elbow, the anterior bundle of the medial collateral ligament inserts at which site? 3-Horner's sign define, PE finding? mn 4-radial n-mn? 5-motor strength will be affected how after transfer of tendon, goal transfer muscle power? 6-muscles innervated by Ulnar nerve? mn 7-Bridle procedure used to treat what condition? how to perform? |
1-immobilize elbow in flexion with forearm pronation to provide stability against posterior subluxation
2-Anteromedial process of the coronoid 3-Horner's sign correlates with C8-T1 avulsion, severe pain in anesthetic limb, indication of root avulsion loss of rhomboid function Horner's syndrome componentsSPAM: Sunken eyeballs/ Symphathetic plexus (cervical) affected Ptosis Anhydrosis Miosis 4-Radial nerve: muscles innervated "Try A Big Chocolate Chip Sundae, Double Dip Cherries And Peanuts Preferably Included": BEST T Triceps A Anconeus B-Brachioradialis C-ext. Carpi radialis longus C ext. Carpi radialis brevis S Supinator D-ext. Digitorum D-ext.Digiti minimi C-ext. Carpi ulnaris A Abductor poll. longus P-ext. Poll. brevis P-ext. P poll. longus I ext. Indicis 5-motor strength will decrease one grade after transfer, should transfer motor grade 5 6-MAFFIA M-med 2 lumbricals, A-Add pollicis F-FCU, F-FDP, I-Interossia, A-abd digi mini 7-Bridle procedure foot drop 2^peroneal N dysfunction consists of a PTT transfer through the interosseous membrane to the dorsum of the foot with a dual anastomosis to the tendon of the ATT & a rerouted peroneus longus in front of the lateral malleolus. all 11 feet were brace-free from foot drop peroneal nerve palsy |
|
|
56-1- predominant cell type in tendon, composition
2-tendons contain ??? collagen and????viscoelastic than ligaments 3-Stages of Soft Tissue Healing (including tendons)(4) 4-tendon repairs are weakest at___ days 5-most of strength by ____ days 6-maximum strength at___months 7-final strength only reaches ___of normal even years after repair |
1-fibroblasts, collagen 1 3 proteoglycan
2-tendons contain MORE collagen and are LESS viscoelastic than ligaments 3-hemostasis- minutes, inflammation-1 wk, Organogenesis<3 wks remodeling-18 mths 4-tendon repairs are weakest at 1 wk 7-10 days 5-most of strength = 3-4 wks( 21-28 days) 6-maximum strength at 6 months 7-final strength only reaches 66% 2/3 of normal even years after repair |
|

57-1-MCC & 2nd MCC for revision THA? MC direction
2-MC MoI for post vs ant dislocation of hip? 3-11 risk factors for dislocation surgeon 4 & pt 7 4-xray finding impeding dislocation of hip? 5-Hawkins Classification of which bone?, significance? describe? 6- Varus malalignment after a talar neck fracture with medial comminution causes a decrease in what motion? 7-MC Complication after talar neck fx |
1 MCC-rev THA=infection #2 MCC-dislocation
-dir=posterior 2-post flex & IR Ant-ext & ER 3-surgeon-mal position-AV >15 adb >40, < fem neck.< fem offset, post approach, pt- female, neuromuscular/spastic/parkinsons, >70 yo, prior surgery, alcoholic/druggy, RA, AVN 4-eccentric wear on xray of femoral head as an indication of polyethylene wear and risk for impending dislocation 5- hawkins gives risk of AVN (1)-ND fx neck 10-13% (2)subtalar dislocation-50% (3)-subtalar & tibio talar dislocation-100% (4)-subtalar.tibio talar, talonavicular, dislocation-100% 6- Subtalar eversion 7-MC-DJD #2 MC-avn |
|
|
58-1-MC tarsal coalition & tx
2-subtalar joint moves the foot to___and ___ in late stance 3-"anteater" sign=? 4-Sangeorzan Classification of ___ Body Fx & describe 5-MCCompltn w/ navicular fx 6-Risk factors for thromboembolism, Virchow's triad mn 7-Prophylaxis in ALL hip & knee replacement |
1- CNC, calcealnavicular coalition young pts 8-12
tx-SLC x 4wks 1st if no previous treatment greater than 50% involvement of the subtalar joint. Triple arthrodesis involves fusion of the subtalar, calcaneocuboid, and talonavicular joints and is the most effective procedure for fixed hindfoot and forefoot deformities. Subtalar fusion can be performed in select cases with no significant hindfoot deformity. 2-subtalar joint moves the foot to IR & varus in late stance 3-calcaneonavicular coalition seen on oblique view, elongated anterior process of calcaneus 4-Sangeorzan Classification navicular 1-Transverse fracture of dorsal fragment that involves < 50% of bone. NO FOOT DEFORMITY 2ADD deformity Oblique fracture, usually from dorsal-lateral to plantar-medial. 3ABD deformity of foot, Central or lateral comminution. 5-delayed union, non union and high risk of AVN 6-stasis, hypercoagulable, intimal tear EMBOLISM E-ex DVT PREVIOUS***, & recombinant Erythropoeitin M-Malignancy B-pregnancy, O-oestrogen, L-Large obesity I-Immune system=****S,C.5 deficiency, thrombocytosis, HYPERCOAGULABLE STATE3 S- surgery recently M-mobilization lack of 7-mechanical prophalaxis-compressive stockings recommended pneumatic compression devices |
|
|
59-1-clinical presentation of PE?
2-EKG find of PE, aka 3-Paget-Schroetter syndrome 4-3 provocative tests for thoracic outlet syndrome 5-when repairing an elbow with terrible triad what part of the repair creates the most stability? 6-At the elbow, the anterior bundle of the medial collateral ligament inserts at which site? 7-most important against valgus stresses in elbow, AKA |
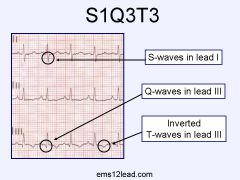
1-acute onset pleuritic pain and dyspnea, tachypnea
tachycardia 2-S1Q3T3 large S wave in lead I, a Q wave in lead III, and an inverted T wave in lead III indicates acute right heart strain. and is termed the "McGinn-White sign" after the initial describers but is only found in about 10-20% of people with a PE PE are sinus tachycardia, right axis deviation and right bundle branch block. 3-thoracic outlet syndrome with compression of subclavian vein in the developed athlete due to scalene muscle hypertrophy, weightlifting, rowing, swimming 4-PE-provocative test(1) Wright test=ABDuction of arm/should ER turn head AWAY from the side of interest ***** pulse to see if it disappears (2)Adson test=extend neck, turn towards side ***** if pulse disappears (3)roos-hold hands open and close them for 3 min 5-repair of LCL 6- Anteromedial process of the coronoid aka the sublime tubercle 7-anterior bundle of the MCL, AKA ulnar collateral band |
|
|
60-1 turnbuckle splinting
2-panner dz vs ocd 3- describe adson's test vs Wright's test 4-primary THA ___ vs revision THA ___incidence of dislocation? 5- HIGHEST risk of dislocation of THA 6- nl anteversion of cup and stem 7-mnemonic for ASAI (A-E) |
1-Static progressive splinting is useful treatment for certain patients with post-traumatic elbow stiffness. Generalized accepted indications are flexion contractures greater than 30 degrees, or flexion less than 130 degrees after a failed trial of physical therapy.
2-panners dz 0-10 same pathology OCD older pts 10-20 adolescent 2^ repetitive trauma 3 wright test-hyper abduction Ext Rot of shoulder w/ arm in extension turn head away from shoulder ***** pulse still present Adson's test extended should/arm look up and away check if pulse present 4-primary THA 1% vs. revision THA 5%-7% 5-pt >80 yo with failed orif of femur neck converted to THA 6- anteversion of cup= 20-30 & stem -10-15 7-ASIA A-Awful complete, ASIA E Excellent->normal ASIA B-BAD motor -zero ASAI C-motor<3, ASAI D motor >3 |
|
|
61-1which bust fx can be tx w/ brace only?
2-MC location of thoracic disk herniation? 3-2 causes of horner's syndrome 4-under representation of _____gene sequence in females with ACL ruptures 5-Calcium____ cement of high compressive strength 6-Triple arthrodesis involves fusion of the ___ joints |

1-PLL intact-mri, no neurologic/no weakness involvement <30 kyphosis, <50 body height loss, < 50 canal compromise
2-MC-T11-12 3-brachial plexus injury w/ nerve root involvement, thoracic disk herniation T2-T5 4-CC genotype of a COL5A1 5-Calcium PHOSphate 7-Triple arthrodesis subtalar, calcaneocuboid, and talonavicular joints |
|

62-1 Elbow Arthroscopy which portal not used, why
2-MC:condition to cause nerve injury w/ elbow scope? MC nerve injured w/ scope? MC portal to cause sinus tract? 3-MC direction of elbow dislocation? longest period of immobilization or consequence? 4-3 dynamic stabilizers of elbow? mn-3 5-elbow terrible triad? safe zone in elbow? 6-if LCL is disrupted vs MCL than usually more stable in __? 7-MC sequelae after closed treatment of a simple elbow dislocation? MoI for Varus Posteromedial instability? |
1 posterior medial->injury to ulnar nerve
2-MC condition- RA & joint contracture & stiffness MC nerve inj-ulnar Nerve MC portal sinus- poster lateral 3-Pos-lat -3 immobilization>3 wks-->joint contracture & stiffness 4-anconeus, brachialis, triceps (mn-ABT) 5-lig-LCL, radial head fx coronoid type 3 fx + dislocation -a 90° arc in the radial head that does not articulate with the proximal ulna) the "safe zone" can be identified by its relationship to Lister's tubercle and the radial styloid, zone is approximately 90 deg and lies between a longitudinal line along the radial styloid and a longitudinal line along Lister's tubercle (with the wrist in neutral rotation); - safe zone is anterolateral in neutral position and posterolateral in full supination; 6--if LCL -> more stable =pronation MCL-supination 7-loss of terminal extension of elbow, -anteromedial facet of the coronoid fx + LCL injury |
|
|
63-1 Syringomyelia define MCC of __?
2-define little league elbow? 3-#1 & #2 MC nerve palsy seen with supracondylar humerus fx? PE finding? 4-age of ossification/appearance and age of ossification/appearance 5-anterior humeral line 6-when performing a CR (extension-type) Supracondylar Fracture - Pediatric what direction for posteromedial fragments: __& posterolateral fragments:____ 7-floating elbow" define |
1-a cyst or cavity forms within the spinal cord. This cyst, called a syrinx.
MCC-neuropathic shoulder and elbow 2-Repetitive contraction of the flexor-pronator mass stresses the chondro-osseous origin, leading to medial apophysitis. 3-#1 (both extension & flexion) MC-AIN-> ulnar nerve, cannot make ok sign bc/unable to flex the interphalangeal joint of his thumb and the distal interphalangeal joint of his index finger #2 MC radial n, CANNOT inability to extend wrist or digits may be present due to radial nerve injury neurapraxia 4-age of ossification/appearance=Capitellum=1, Radius=4, Medial epicondyle=6, Trochlea=8, Olecranon=10, Lateral epicondyle= 12 age of ossification/appearance=fuses at age ~ 14 years (is the last to fuse) 5-anterior humeral line should intersect the middle third of the capitellum 6- forearm supinated with hyperflexion posteromedial fragments: forearm pronated with hyperflexion OPPOSITE posterolateral fragments: forearm supinated with hyperflexion 7-floating elbow"=ipsilateral supracondylar humerus and forearm fractures necessitate immediate pinning of both fractures to decrease risk of compartment syndrome |
|
|
64-1 Homan's sign
2-gold standard test for DVT 3-proximal DVTs (proximal to trifurcation) best test w/ highest sensitivity & specificity? 4-mn for causes of DVT 5-main indication of stoppa approoach 6-suprascapular neurapathy may occur in 2 locations, effect? 7-Jobe test =? |
1 pain and swelling in calf w/ DVT
2-Contrast venography is the gold standard BUT NOT used venous duplex ultrasound is gold standard 3-venous duplex ultrasound is 96% sensitive, 98% specific 4-EMBOLISM E-had DVT before M-malignancy B-baby pregnancy O-oestrogen bcp L-large obesity I-immunity prtn C,S,3; C lot & S toppers forming of clots S-surgery M-mobilization 5-quadrilateral plate ORIF 6-spinoglenoid notch entrapment-infraspinatus suprascapular notch entrapment- infraS & SS 7- weak SSM |
|
|
65-1-MRI showing a cyst in the suprascapular notch. Which of the following muscles is most likely to show weakness? PE findings?
2-His exam is noted to have a normal "empty can" and "belly press" tests. Resisted external rotation with the arm at the side does exhibit weakness. PE findings? 3-elderly patients from a low-energy subtrochanteric fx think what? 4-deforming forces on the Subtrochanteric Fractures proximal fragment are & distal frag? which muscles? reduction technique for prox frag & distal frag? 5-Russel-Taylor Classification used for? describe 6-fixation with a construct using tension band 3 principles criteria? 7-Concepts of application tension band 3 principles criteria? examples? |
1-SS & IS=>IS=weakness to external rotation with elbow at side & weakness seen with shoulder abduction to 90 degree, 30 degrees forward flexion, and with internal rotation (Jobe test positive=>SS
2- Spinoglenoid cyst decompression with posterior labral repair 3-R/o pathologic or atypical femur fx bisphosphonate use, particularly alendronate, 4- prox frag->(1)ER-short ER muscle, (2)flex-iliopsoas, (3)abd-gluteus medius and gluteus minimus dist frag->add->adductors & prox-(8)Adductor brevis Adductor longus, Adductor magnus, Adductor minimus, adductor magnus, pectineus, gracilis Obturator externus (obturator nerve) The proximal fragment=extended, adducted, and internally rotated to obtain a proper reduction. 5-subtraochanteric fx? 1- No extension into piriformis fossa,Tx-nail 2- w/ extension into GT & PF Tx-fixed angle device his 6-tension band principles=(1) the bone must be eccentrically loaded, (2) the construct must be applied on the tensile side, on the convex side of a curved bone.(3) the opposite cortex must be able to withstand compressive forces. 7-tension band principle with wire loops is often applied to articular fractures converting tension from muscle pull into compressive force on the articular side of the fracture. In addition, small avulsion fractures may benefit from the principles of tension band fixation. ex=1-patella, 2-olecranon, 3-med malleolus, 4-grt tuberosity humerios, 5-non union of fem or tibia w angular deformity, ex fix applied to tension side. |
|
|
66-1 Coxa Saltans define, MC form?
|
1-snapping hip
-internal snapping hip caused by iliopsoas tendon sliding over femoral head, prominent iliopectineal ridge, exostoses of lesser trochanter, iliopsoas bursa |
|
|
67-1 Spinal Cord Monitoring disadvantage of SEP (somatosensory evoked potentials) & Motor Evoked Potential (MEP)?
2- what is Mechnical Electromyography (spontaneous) 3-MC sarcoma in children, stageing of STS? give ex 4-classic sx for soft tissue sarcoma (STS)? MC site of metastasis of STS? (6) common types of STS 5- what is the significance of getting an MRI to evaluate a ST Mass? following resection the MC location for recurrence of a low grade, soft tissue sarcoma is___? 6 describe the expected histo finding in 6 MC STS? is MRI required to eval STS why why not? 7-standard of care in most cases of STS, standard dose? if give pre-op XRT vs post op XRT what is the risk of wound complication? why give XRT? |
1-not reliable with respect to monitoring the integrity of the anterior spinal cord pathways, ischemic injury leading to paralysis despite normal SEP monitoring during surgery
(MEP)-often unreliable due to effects of anesthesia 2-monitor integrity of specific spinal nerve roots 3-Rhabdomyosarcoma grade (G), grade is a sign of how likely it is the cancer will spread.Differentiation — cancer cells are given a score of 1 to 3, with 1 being assigned when they look similar to normal cells and 3 being used when the cancer cells look very abnormal Mitotic count — how many cancer cells are seen dividing under the microscope; given a score from 1 to 3 (a lower score means fewer cells were seen dividing) Tumor necrosis — how much of the tumor is made up of dying tissue; given a score from 0 to 2 (a lower score means there was less dying tissue present). T Tumor (T)stands for the size of the Tumor. T1: The sarcoma<5 cm (2 inches) T1a: The tumor is superficial − near the surface of the body. T1b: The tumor is deep in the limb or abdomen. N stands for spread to near by lymph Nodes (small bean-shaped collections of immune system cells found throughout the body that help fight infections and cancers). M is for Metastasis (spread to distant organs). stage= the tumor, its grade, lymph nodes, and metastasis is combined by a process called stage grouping. The stage is described by Roman numerals from I to IV and the letters A or B. The stage is useful in selecting treatment, but other factors, such as where the sarcoma is located, also influence treatment planning and outlook. ex.=Stage IA T1, N0, M0, G1 or GX: The tumor is not larger than 5 cm (2 inches) across (T1). It has not spread to lymph nodes (N0) or more distant sites (M0). The cancer is grade 1 (or the grade cannot be assessed). 4-enlarging painless mass over 6 mths, MC loc for STS mets=lung 4-lipo-S, rhabdo-S, fibro-S, leiomyo-S, synovial-S; angio-S 5- if MRI is diagnostic=lipoma, neurilemoma (schwanoma), intramuscular myxoma THEN the mass is BENIGN and symptomatic, then it can be removed w/OUT a bx if MRI is indeterminate or suggestive of sarcoma, then a core needle or open biopsy must be obtained before further treatment is initiated soft tissue sarcomas can look similiar to hematomas so be cautious of a "hematoma" which occurs w/OUT trauma -if recurrence=local 6-(6)=L-Lipo-S, F-Fibro-S, S-Synovial-S;(LFS) & L-Leiomyo-S, A-Angio-S, R-Rhabdo-S (LAR) (1)L-LipoS=immature lipoblasts (signet ring-type cells) mature adipocytes (2)F-FibroS=atypical spindle cells, HERRINGBONE pattern, variable levels of collagen production (3)S-Synovial S-classical =biphasic appearance with two typical cell types=spindle cells (fibrous type of cells) & L-Leiomyo-S, A-Angio-S, R-Rhabdo-S (LAR) (4) L-Leiomyo-S=cigar-shaped nuclei, cells arranged into fascicles along with myofibrils running parallel relatively small and uniform and found in sheets of malignant appearing cells with minimal cytoplasm and dark atypical nuclei & epithelial cells gland, nest, or cyst like cells (5)A-Angio-S=vascular channels, variable degree of anaplasia, malignant cells associated with vascular structures (6)R-RhabdoS=Embryonal=small rounds blue cell tumor, skeletal muscle-like cross-striations can occur based on the stage of neoplastic cell development MRI mandatory to evaluate STS in the extremities =determine tx algorithm if r/o benign vs malignant if benign NO bx necessary 7-XRT & wide surgical resection & NO chemotherapy:::XRT=50-60 Gy is the standard dose for soft-tissue sarcomas, radiotherapy may be given pre- or post-operatively -pre-op XRT= 30% risk for wound complications post op XRT= > induced morbidity & > risk for XRT induced sarcoma -give XRT to reduces the risk of local recurrence |
|
|
68-1 MC organism for epidural abscess TX
2-preoperative degree of neurologic deficits is most important indicator ___? 3-imaging modality of choice for diagnosis of spinal epidural abscess? why use it? define pathognomonic for abscess 4-If epidural abscess what is risk of permanent neurologic deficit? risk of death? 5-stand for (SONK) 6-MC loc of SONK & OCD 7-MC form incomplete SCI*** |
1-staph aureus Tx=an antistaphylococcal penicillin, a third-generation cephalosporin, and an aminoglycoside
2-preop deg of neurologic deficits is most important indicator of clinical outcome 3-MRI w/ gadolinium -gadolinium allows differentiation of pus from CSF a ring enhancing lesion is pathognomonic for abscess 4-22%***** permanent & 5% death 5-Spontaneous Osteonecrosis of the Knee (SONK) 6-epiphysis of MFC crescent shaped in older females OCD-lat aspect of MFC on adol Males 7-MC SCI incomplete=central cord= |
|
|
69-1 (2) MCC permanent loss of the bulbocavernous reflex
2-SCI above ___ likely to require intubation 3-MC reason for missed injury to the cervical spine? define trauma series of c-spine 4-(6) incomplete SCI 5-COMPLETE defined as ASAI=? (4):::INCOMPLETE defined as?? 6-Determine neurological level in ASIA? metastatic CA patients with < 6 mos life expectancy how to determine <6 MTL ((6) correspond to short life expectancy) 7-Tx of SCI, Indications tx SCI & CI (5)? why use steroids |
1-MC- conus medullarus injury, caudaul equina syndrome
2-SCI aT C4 or above C5 3-inadequate xrays, cervical spine xray series: must include top of T1 vertebra, includes:AP/lat/open-mouth odontoid view 4-anterior cord syndrome Brown-Sequard syndrome central cord syndrome posterior cord syndrome conus medullaris syndroms cauda equina syndrome 5-(1)0/2 distal sensory scores ****(no perianal sensation)AND (2) 0/5 distal motor AND (3) no voluntary anal contraction (sacral sparing) AND (4) bulbocavernosus reflex present (patient not in spinal shock) -INCOMPLETE=voluntary anal contraction (sacral sparing), anal wink and perianal sensation 6-lowest segment where motor and sensory function is normal on both sides -6=multiple spinal mets, multiple extraspinal mets unresectable lesions in major organs, SCI (complete or incomptete); aggresive CA: lung, osteosarcoma, pancrease, critiically ill 7-high dose methylprednisone 30 mg/kg bolus followed by a 5.4 mg/kg/hr infusion x 24 hours if started < 3 hrs after injury for 47 hours if started 3-8 hours after injury Indic=nonpenetrating SCI <8 hrs of injury (5)CI to Tx SCI=pregnancy & <13 yo & GSW; >8 hrs, brachial plexus injury, -outcomes=leads to improved root function at level of injury, may or may not lead to spinal cord function improvement |
|
|
1-transfer for C5 or C6 SCI
2-retained bullet fragment within the thecal sac observe or remove, why? -are any potentially fatal complications w/ SCI 3-goals during rehab w/ SCI 4-what level SCI IF::: A-Initially ventilator dependent, but can become independen, Elect WC? - Electric wheelchair with head or chin control, -Independent ADL’s; electric wheelchair with hand control, -nl WC w/sliding board transfers -nl WC with independent transfers -lowest level still need a WC? -with extensive bracing walking MAY be possible***? -Walking with minimal or no assistance 5-most important tumor-related factor has been shown to be most important for five-year disease-free survival in patients with subcutaneous sarcomas? vs. Which treatment factor has been shown to be most important for five-year disease-free survival in patients with subcutaneous sarcomas? 6-child w/SCIWORA). What is the most important predictor of her neurologic outcome? 7 which level needs: Electric WC chin vs hand, nl WC, still need WC, no WC + walk with braces, nl walk Various return of B/B and sexual function |
1- Deltoid to triceps
2-REMOVE, CSF leads to the breakdown of lead products that may lead to lead poisoning -yes autonomic dysregulation-HA, foley clogged, bowls impacted 3-headache, agitation, hypertension 4-E-WC w/chin=C3-4 E-WC w/ chin control=C4 -E-WC w/ hand controls & ADL=c5 -nl WC w/ slide board for transfers=c6 -nl WC & indep transf=C7 -yes to WC=T2-T6 (beer bad for WC) but nl UE, good trunk control control-YES WALK T7**** (7th heaven) -nl walking S1 -S5 5-size of tumor ie >5 cm vs tx, The size of the operative margin is the most important treatment-related factor 6-severity of initial neurologic injury, inherent elasticity in pediatric cervical spine can allow severe spinal cord injury to occur in absence of x-ray findings; HOWEVER “real” SCIWORA or spinal cord injury without neuroimaging abnormality is less common. However, the term SCIWORA is still commonly used to describe patients with neurologic findings suggestive of spinal cord injury with normal anatomic alignment and no bony abnormalities seen on plain film and/or CT. today MRI p/u spine pathology. 7-E-WC w/chin=C4 vs E-WC w/hand=C5: nl WC=C6 yes needs WC= T6, No WC walk w/braces=T12 nl walking= S1 |
|
|
71-1-the most influential factor affecting postoperative function in shoulder hemiarthroplasty?
2-what name xray view true AP of shoulder, how to do, what looking for? name 2nd xray view helpful in evalu shoulder pain? 3-distance from top of prosthesis head to upper border of pectoralis major should in hemi? 4-MCC of failure for fx treated with hemiarthroplasty? effect of migration 5-SLAP lesion mn, best view to see? 6-how does SLAP lesion increases the strain in shoulder and thus compromises stability of shoulder 7-describe the 3 provocative tests for SLAP tear? MC finding on MRI with SLAP tear |
1-status of the RC
2-Grashey, 30-40 degrees oblique to the coronal plane of the body , extent of glenohumeral arthritis axillary view-posterior glenoid wear. 3-53mm 4-tuberosity migration, lesser tuberosity is needed for ER subscapularis 5-Superior Labrum from Anterior to Posterior tears, coronal view 6-SLAP lesion increases the strain ->ant band of the IGHL 7-active compression test (O'Brien's test) Crank test, Dynamic labral shear test MC MRI finding-spinoglenoid notch cyst |
|
|
1-SLAP Classification
2-medial winging caused by, lateral wing caused by? 3-what is the difference bt/ mesh partial-thickness dermal tissue vs full-thickness dermal tissue, how does nutrition occur? CI to skin graft 4-MC organism to cause septic arthritis adult? MC organ seen in patients after dog or cat bite |
1-I-Labral and biceps fraying, anchor intact
II-Labral fraying with detached biceps tendon anchor III-Bucket handle tear, intact biceps tendon anchor (biceps separates from bucket handle tear) 4-IV Bucket handle tear with detached biceps tendon anchor (remains attached to bucket handle tear) V-SLAP lesion and anterior labral tear (Bankart lesion) VI-Superior flap tear VII-SLAP lesion with capsular injury 3-meshed grafts provide a greater surface area meshed grafts have a lower incidence of hematoma formation and infection leading to better "take" of the graft full thickness of dermis and epidermis, containing hair follicles and sweat glands, subcutaneous fat is not included because it decreases vascular ingrowth and survival, -nutrition is obtained by diffusion from the wound bed -Contraindications=wounds with exposed bone, nerves, or blood vessels 4-staphylococcus species MC cat-pasteurella multocida |
|
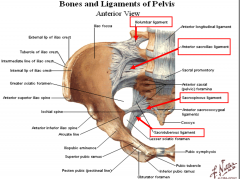
73-1-What is nl nerve root anatomy?mn
2-inlet view, purpose to see? outlet? 3-what nerve is at risk with insertion of SI, where is it, what view to make sure its ok? sx of nerve root injury? 4-Crescent Fractures definition, classification 5-4 SI joint is stabilized by the posterior pelvic ligaments 6-windswept pelvis define, classification 7-LC Type I, During placement of percutaneous iliosacral screws, the outlet radiograph is obtained. What purpose does this view serve? 7-MC injured with fx pattern: superior gluteal A MC APC vs LC internal pudendal A APC vs LC obturator A APC vs LC |

1C1-ABOVE (because of C8)
T1 below & L1 below EXCEPT Lum far lateral which is ABOVE 2-into and down the pelvis to see-> posterior displacement of SI or open pubic symphysis outlet to see vertical shear injury 3- L5 nerve root, it draps of saral ala, best seen on sacral lateral or inlet view, -L5 lateral leg numbness, weak DF to great toe and cannot toe walk 4-combination of ligamentous injury at inferior portion of SI joint, and verticle fracture of the posterior ilium which extends thru iliac crest; - posterior superior iliac spine remain attached to the sacrum; when ilium fragment remains with sacrum it is termed a crescent fracture LC2 5-sacrospinous, sacrotuberous, anterior sacroiliac posterior sacroiliac 6-=LC3=lateral compression type III pelvic fracture occurs when the internal rotation of the right iliac wing causes a sacral compression fracture, while the same forces cause an external rotation of the opposite hemipelvis (e.g. diastasis of SI joint). This causes classic “wind-swept pelvis” appearance. aka-Ipsilateral lateral compression and contralateral APC (windswept pelvis). 7-LC Type I=oblique ramus fracture and ipsilateral anterior sacral ala compression fracture. superior gluteal most common (posterior ring injury, APC pattern) -Best visualization of sacral neural foramina internal pudendal (anterior ring injury, LC pattern) obturator (LC pattern) |
|
|
1-Injection of ___ml of saline will diagnose 99% of knee arthrotomies
2-What is Seebauer Classification used for, describe it 3-snowcap sign is? 4-Following open pectoralis maj transfer to address chronic subscapularis insufficiency, which of the following movements would most likely show weakness if an iatrogenic nerve injury occurred during the pectoralis transfer? 5-define a large med, small rotator cuff tear? 6-rate-limiting step for recovery is biologic healing of RTC tendon _______, which is believed to take 8-12 weeks 7-latissimus dorsi transfer vs pectoralis major transfer |
1-175ml vs 155= 95%
2-Seebauer classification= Rotator Cuff Arthropathy 1 A=centralization & stable, see femoralization 1 B=medialization & stable, see medialization, stable 2 A=superior migration unstable 2B-ant sup escape & unstable 3-AVN or subchondral sclerosis seen in RC arthopathy 4-flexion @ elbow 2^ musculocutaneous nerve inj 5-small<1 med <3 large <5 massive> 5 6-rate-limiting step for recovery is biologic healing of RTC tendon to greater tuberosity, which is believed to take 8-12 weeks 7-latissimus dorsi transfer=indicated in large supraspinatus and infraspinatus tears best candidate is young laborer, irreparable posterosuperior rotator cuff tear with 100 degrees of forward elevation and -10 degrees of external rotation, lack of advanced glenohumeral arthritis, has an intact subscapularis function to stabilize the humeral head after latissimus transfer, and who maintains some active forward elevation. pectoralis major transfer=indicated in chronic subscapularis tears, transferring pectoralis major under the conjoined tendon leads more closely resembles the vector forces of the native subscapularis |
|
|
75-1- MC injury pattern w/ scapulothoracic dissociation? mortality rate? functional outcome is dependent on ___? tx ?
2-the chromosomal translocation t(X;18)(p11;q11) is characteristically found in which malignancy? 3-MC STS in the foot, and a sarcoma which commonly shows calcification on plain xray is? |
1-neurologic injuries MC than vascular injuries, ipsilateral brachial plexus injury
subclavian artery MC injured axillary artery -10% mortality rate -functional outcome is dependent on neurologic injury, if no return then Tx is amputation 2-Synovial sarcoma 3-synovial cell sarcoma |

