![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
15 Cards in this Set
- Front
- Back

Hx:73 yo F underwent TKA 10 years ago. She sustained a prox tibial shaft periprosthetic fx p/ a ground level fall. xrays show that the fx involves the tibial component's stem w/loosening of the tibial component. Which is the most appropriate tx? 1- ORIF of the tibia; 2-Ex-Fx; 3-IM rod fix; 4-Revision with a long stem tibial component that bypasses the fx; 5-Fx bracing
|
Revision with a long stem tibial component that bypasses the fracture is an appropriate treatment for tibial shaft fracture at the level of the implant with evidence of implant loosening.
Haidukewych et al present a Level 5 review that states a periprosthetic fracture that involves the stem of a component with evidence of loosening requires revision. This most commonly is with a long stem, press fit component that bypasses the fracture by at least two cortical diameters.Ans4 |
|

A PCL retaining TKA is contraindicated in all of the following pts EXCEPT? 1-52yo F w/ severe RA of the knee; 2-73-yo M w/ post-traumatic arthritis of the knee and prior patellectomy; 3-67yo M w/DJD and 10 deg valgus deformity; 4-55yo M w/ post-traumatic arthritis of the knee 20 yrs p/ bicruciate ligament rupt; 5-63yo F w/ chronic hx of steroid tx of SLE and DJD knee
|
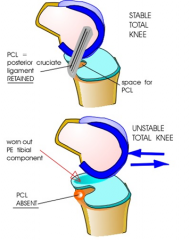
Posterior cruciate retaining knees require a functional PCL to produce femoral rollback during knee flexion. Posterior-stabilized knees rely in the component to produce femoral rollback. Contraindications to using a posterior cruciate retaining knee include any condition that may render the PCL incompetent at the time of surgery or in the future including prior PCL rupture, inflammatory arthritis, patellectomy, and over-release of the PCL during surgery. Valgus deformity is not a contraindication.Ans3
|
|

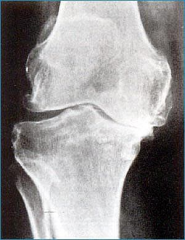
A 55-year-old patient is scheduled for total knee arthroplasty. A radiograph is provided in Figure A. Each of the following are risk factors for heterotopic ossification EXCEPT? 1-Valgus knee deformity; 2-Male gender; 3-Obesity; 4-Hx of trauma; 5-Presence of preoperative osteophytes (hypertrophic arthrosis)
|

Heterotopic bone ossification (HO) following TKA has not been associated with valgus knee deformity. HO formation can be problematic both after a THA and TKA, but unlike the hip, it rarely becomes a clinical problem. The overall incidence of HO after TKA varies greatly among published studies, ranging from 15-50%. In the study by Dalury et al, they noted a 15% HO incidence. Among those with HO, 95% had osteoarthritis and 5% had a history of inflammatory arthritis. In their study, obese and male patients also had a higher incidence of developing post-operative HO. Toyoda et al in their study showed a significantly higher rate of HO in patients with osteoarthritis and pre-operative osteophyte formation (hypertrophic arthrosis). Overall, the signficant risk factors include hypertrophic arthrosis (often seen with trauma), male gender, and obesity.Ans1
|
|

All of the following are risk factors for post-operative total knee arthroplasty periprosthetic supracondylar femur fractures EXCEPT? 1-RA; 2- Parkinson's dz; 3-Chronic steroid therapy; 4-Revision knee arthroplasty; 5-Male gender
|

Rheumatoid arthritis, Parkinson's disease, chronic steroid therapy, osteopenia, and female gender have all been found to be risk factors for post-operative periprosthetic supracondylar femur fractures. Male gender has not been found to be a risk factor. Su et al discuss risk factors for supracondylar periprosthetic femoral fractures which include rheumatoid arthritis, neurologic disorders such as Parkinson's disease, chronic steroid therapy, and revision knee arthroplasty. Analysis of the Mayo Clinic joint registry by Berry found that females are at increased risk of post-operative periprosthetic fracture, likely due to the increased incidence of osteoporosis.Ans 5
|
|

Hx:62yo F underwent a primary TKA of the L knee 10 days ago. She presents to clinic with skin necrosis of the midline incision. There is no deep infection present upon aspiration of the knee jn. She undergoes superficial I & D and is left with exposed patellar tendon as shown in Figure A. What is the next step in management? 1-Split thickness skin grafting; 2-BID wet-to-dry dressing changes with Dakin's solution until healing by secondary intention; 3-Latissimus dorsi free flap transfer; 4-Vacuum-assisted closure device until healing by secondary intention 5- Medial gastrocnemius muscle flap transfer and skin grafting
|

Medial gastrocnemius muscle flap transfer and skin grafting is the most appropriate choice of the options listed (postoperative image shown in Illustration A).
Level 4 evidence by Ries describes 7 patients that developed necrosis over the patellar tendon or tibial tubercle, of whom 6 were treated with medial gastrocnemius flap coverage. Two patients developed necrosis over the patella, both of whom were treated with local wound care and skin grafting. Successful wound healing and salvage of the TKA was achieved in all cases. Ries concluded that necrosis of the proximal wound including the area over the patella can be treated by local wound care and skin grafting. However, skin necrosis over the tibial tubercle or patellar tendon requires muscle flap coverage to prevent extensor mechanism disruption and deep infection.Ans5 |
|
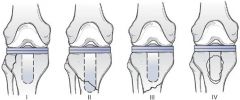
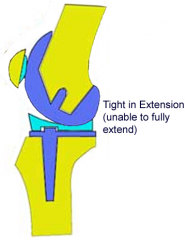
While performing a revision TKA the surgeon decides to upsize the fem component with use of posterior fem augments. Which of the following intraoperative exam findings would have led to this decision? 1-A knee that is balanced in ext and tight in flex; 2-A knee that is balanced in exten and loose in flex 3-A knee that is tight in extension and tight in flexion; 4-A knee that is loose in exten and loose in flex; 5-A knee that is loose in extension and balanced in flexion.
|
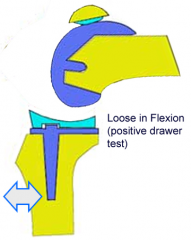
Increasing the size of the femoral component posteriorly will balance a flexion-extension mismatch where the knee is loose in flexion and stable/balanced in extension. The referenced article by Peters discusses multiple different soft tissue balancing techniques used for trialing scenarios as well as for varus or valgus instability, and knees with flexion contractures. A knee tight or loose on both flexion and extension can be corrected by decreasing or increasing the size of the polyethylene, respectively. A knee that is tight in flexion/balanced in extension can be corrected by decreasing the AP diameter of the femoral component.Ans2
|
|
Hx:62yo M undergoes TKA Preop xrays Fig A. Following bone resections and placement of trial implants, the knee is stable in flexion, but cannot achieve full extension. Which of the following interventions will most likely result in a knee that is balanced in flexion and extension? 1-Resect more distal femur; 2-Resect more distal femur and downsize the femoral component; 3-Resect more proximal tibia; 4-Decrease polyethelene liner thickness; 5-Place posterior femoral augments
|

The radiograph demonstrates a varus osteoarthritic knee suitable for a standard total knee arthroplasty. In this scenario, the knee is balanced in flexion, but tight in extension. Resecting more distal femur opens up the extension gap without changing the flexion gap resolving the problem.
Resecting more tibia alters both extension and flexion gaps and would cause laxity in flexion. Downsizing the femoral component opens up the flexion gap and would also cause laxity in flexion. Converting to a decreased polyethylene thickness would change both the flexion and extension gaps. Placing posterior femoral augments would tighten the flexion gap and have no effect on the extension gap.Ans1 |
|
While trialing components during a routine TKA, the flexion gap is felt to be loose and the extension gap is stable. Which of the following are possible ways to treat this intraoperative instability? 1-Move the femoral component posterior; 2-Increase the size of the polyethylene component; 3-Downsize the femoral component; 4-Move the femoral component anterior and augment the distal femur
5-Externally rotate both the femoral component and tibial components |
Flexion and extension gaps during TKA must be balanced to provide a knee that is stable throughout its range of motion. Changes to the tibia, such as modifying the size of the polyethylene insert, affect both the flexion gap and the extension gap. Conversely, changes to the femur typically affect either the flexion gap or the extension gap, but not both. Moving the femoral component anterior or posterior increases or decreases the flexion gap respectively. In a similar manner, moving the femoral component proximally or distally increases or decreases the extension gap respectively. In this question, the patient is loose in flexion and stable in extension. This can be addressed by either moving the femoral component posterior, or upsizing the femoral component which will only increase the AP diameter of the prosthesis. Ans1
|
|

A patient undergoes the procedure depicted in Figures A and B with standard components (non-gender specific). Which of the following outcomes most appropriately describes the difference in females compared to males for this procedure? 1. Greater implant survivorship
2. Decreased WOMAC scores 3. Increased rate of extensor mechanism rupture 4. Increased postoperative pain 5. Increased component osteoloysis |

Females undergoing total knee arthroplasty with standard (non-gender specific) components show improved implant survivorship compared to males.
MacDonald et al performed a Level 2 study of 3817 patients who underwent 5279 primary total knee replacements (3100 female, 2179 male) with a minimum of 2 years followup. They found that women demonstrated greater implant survivorship, greater improvement in WOMAC scores, equal improvements in SF-12 scores, and less improvement in only the Knee Society function and total scores.Ans1 |
|

A 65-year-old male undergoes a primary total knee arthroplasty. His preoperative radiographs are seen in figures A and B. Postoperative examination reveals an inability to dorsiflex his ankle or extend his toes. Sensation is decreased along the dorsum of his foot as well as between the 1st and 2nd toes. All of the following are risk factors for this complication following total knee arthroplasty EXCEPT 1. Aberrant retractor placement
2. Postoperative epidural analgesia 3. Correction of a 20 degree preoperative valgus deformity 4. Excessive medial release 5. Preoperative diagnosis of neuropathy |
Peroneal nerve palsy following a total knee arthroplasty has been shown to be associated with postoperative epidural analgesia, correction of large valgus deformities, and preoperative diagnosis of neuropathy in the involved extremity (either centrally or peripherally). One may also sustain peroneal nerve palsies following aberrant retractor placement intraoperatively.
Idusuyi et al performed a retrospective review and found a significant increase in the relative risk of developing a peroneal nerve palsy following total knee arthroplasty in patients who received postoperative epidural analgesia, had prior lumbar laminectomies, and had preoperative valgus deformities of greater than 12 degrees.Ans4 |
|
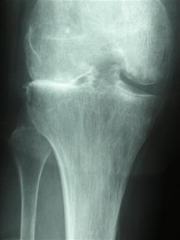
Hx:55-year-old patient is scheduled for total knee arthroplasty. A radiograph is provided in Figure A. Each of the following are risk factors for heterotopic ossification EXCEPT? 1. Valgus knee deformity; 2. Male gender; 3. Obesity; 4. History of trauma; 5. Presence of preoperative osteophytes (hypertrophic arthrosis)
|
Heterotopic bone ossification (HO) following TKA has not been associated with valgus knee deformity. HO formation can be problematic both after a THA and TKA, but unlike the hip, it rarely becomes a clinical problem. The overall incidence of HO after TKA varies greatly among published studies, ranging from 15-50%. In the study by Dalury et al, they noted a 15% HO incidence. Among those with HO, 95% had osteoarthritis and 5% had a history of inflammatory arthritis. In their study, obese and male patients also had a higher incidence of developing post-operative HO.Ans1
|
|

During trialing for a cruciate-retaining total knee arthroplasty, the surgeon is unable to fully extend the knee and is left with a 15 degree flexion contracture. The flexion gap is well balanced. Which of the following options will create a knee that is balanced in both flexion and extension? 1. Recess the PCL; 2. Increase the tibial slope; 3. Decrease the size of the femoral component; 4. Resect more distal femur; 5. Resect more proximal tibia
|
Flexion/extension gap balancing is crucial to the success in total knee arthroplasty. The inability to achieve full extension suggests extension tightness. This can be improved by either resecting more distal femur or releasing the posterior capsule from the femoral insertion. While resecting more proximal tibia will improve the extension gap, it will loosen the flexion gap and require either upsizing of the femoral component with placement of posterior augments or translation of the femoral component posteriorly. Recessing the PCL and increasing the tibial slope would be appropriate for flexion not extension tightness. In their review, Ries et al discuss flexion/extension balancing, focusing on revision total knee arthroplasty.Ans4
|
|
|
The bending rigidity of the implant shown in Figure A is proportional to what power of the measured radius of the implant? 1. 2; 2. 3; 3. 4 ; 4. 5; 5. 6
|
The bending rigidity of an intramedullary nail is related to the fourth power of the nail’s radius. For example, increasing the nail diameter froma a sized 10mm to a sized 11mm nail would increase the bending rigidity by 50%.
The rigidity of a fracture plate is proportional to the plate thickness to the third power. Thus, doubling the fracture plate thickness increases its bending stiffness 8 times. The bending rigidity of an external fixator pin is proportional to the fourth power of the pin diameter. The bending stiffness of each pin is proportional to the third power of the bone-rod distance. However, the most important factor external fixator stability is for the the fracture ends to come into contact with each other.Ans3 |
|
|
All of the following are acceptable indications for use of a constrained acetabular component EXCEPT: 1. Recurrent dislocations due to abductor insufficiency; 2. Recurrent dislocations due to unsalvageable capsular attenuation 3. Recurrent dislocations due to severe polyethylene wear
4. Recurrent late dislocations without component loosening or malposition 5. Recurrent dislocations due to cognitive or neuromuscular disease |
Instability due to polyethylene wear alone is not a reason to use a constrained component, though revision of the acetabular component may be necessary.
Indications for the use of a constrained acetabular component include: 1) recurrent dislocations due to unrepairable soft-tissue insufficiency from lack of abductor function or capsular attenuation; 2) severe cognitive disorders; 3) late dislocations with well positioned components.As3 |
|
|
The schematic shown in Figure A displays a ceramic-on-ceramic total hip arthroplasty articulation with impingement. Which of the following modifications would increase the primary arc range of motion? 1. Addition of a collar on the femoral head ;2. Exchanging the ceramic liner with a hooded polyethylene liner; 3. Increasing the femoral head size; 4. Increasing the femoral offset
5. Increasing the acetabular anteversion |
DISCUSSION: The assessment of hip stability involves four major areas: component design, component alignment, soft tissue tensioning, and soft tissue function. The primary determinant of primary arc range is the head-neck ratio, which is defined as the ratio of the femoral head diameter to the femoral neck diameter. Increasing the size of the femoral head will increase the excursion distance of the femoral head to dislocate, thus making the hip more stable. Illustration A shows how a greater head-to-neck ratio may improve range of motion before impingement. Increasing femoral component offset increases the abductor moment arm and reduces the resulting hip joint reactive force but does not affect primary arc range of motion impingement.Ans3
|

