![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
76 Cards in this Set
- Front
- Back
|
Blank
|
Blank
|
|
|
Describe Ectopic pregnancy, including placenta previa:
|
Ectopic pregnancy - zygote implants outside the uterine cavity - not viable.
Placenta previa - placenta is attached to the uterine wall close to or covering the cervix. |
|
|
Describe Oligohydramnios and “associated conditions for oligohydramnios”
|
Deficiency of amniotic fluid.
Causes - renal agenesis and placental insufficiency. Complications - cord compression, musculoskeletal abnormalities such as facial distortion and clubfoot, lung hypoplasia and intrauterine growth restriction. |
|
|
Describe Polyhydramnios and “associated conditions for polyhydramnios”
|
Excess of amniotic fluid.
Causes - maternal diabetes mellitus, meroanencephaly, multiple pregnacny and esophageal atresia. |
|
|
Describe the Ovarian Cycles and Describe the Menstrual Cycles:
|
Ovarian Cycles:
The Follicular (proliferative) Phase - growth of the uteral lining from an ovarian follicle leading up to ovulation. Luteal (secretory) phase - post ovulation with falling progesterone levels. Menstrual Cycles: -menstrual phase (menstruation) -proliferative phase -ovulatory phase (ovulation) -luteal phase (also known as secretory phase) -ischemic phase -follicular phase |
|
|
Explain how the Ovarian and Menstrual cycles are linked:
|
The Ovarian Cycle is part of the Menstrual Cycle.
-The ovarian cycle involves changes in the ovaries: a. The follicular phase b. Ovulation occurs around day 14 of the cycle c. The luteal phase -The uterine cycle involves changes in the uterus: a. The proliferative phase b. The secretory phase |
|
|
Explain how the date for delivery is calculated from the last menstrual cycle:
|
Naegele's Rule - from the first day of the woman's LMP add 1 year, subtract three months and add seven days (approximately 280 days (40 weeks) from the LMP.)
Parikh's Formula - add 9 months to LMP, subtract 21 days, then add duration of previous cycles. |
|
|
Describe the clinical significance of the sperm count:
|
[sperm] in ejaculate to confirm infertility.
Abnormalities: Aspermia: absence of semen Azoospermia: absence of sperm Hypospermia: low semen volume Oligozoospermia: low sperm count Asthenozoospermia: poor sperm motility -Teratozoospermia: sperm carry more morphological defects than usual |
|
|
Describe the phases of fertilization:
|
fertilized egg → blastocyst → embryo → fetus.
1) passage of a sperm through the corona radiata of the oocyte. 2) penetration of the zona pellucida 3) fusion of the plasma cell membranes of the oocyte and sperm. 4) Completion of the second meiotic division of the ocyte. 5) Formation of the male promucleus. 6) Break down of the promuclear membranes. |
|
|
Results of Fertilization:
|
1) Stimulates the secondary oocyte to complete the second meiotic division, producing the second polar body
2) Restores the normal diploid number of chromosomes (46) in the zygote 3) Results in variation of the human species through mingling of maternal and paternal chromosomes 4) Determines the chromosomal sex of the embryo 5) Causes metabolic activation of the oocyte, which initiates cleavage (of the zygote) |
|
|
Discuss cleavage of the zygote and formation of the blastocyst:
|
Cleavage consists of repeated mitotic divisions of the zygote, resulting in a rapid increase in the number of cells beginning approximately 30hours after fertilization.
Formation of the blastocyst: -Morula: The name of the embryo at the 16 to 32 cell stage. -Blastocyst: At about day 5 after implantation. -Cells are divided into the inner cell mass and trophoblast. •Inner Cell Mass: The cells on the inside. •Trophoblast: The cells surrounding the outside. |
|
|
Describe early implantation of the blastocyst:
|
Begins at the end of the 1st embryonic week.
The inner cell mass gives rise to the embryo proper, the amnion, yolk sac and allantois, while the trophoblast will eventually form the placenta. |
|
|
Describe Implantation of the blastocyst:
|
-Implantation: The trophoblast differentiates into two distinct layers:
Inner - the cytotrophoblast Outer - the syncytiotrophoblast The syncytiotrophoblast implants the blastocyst in the endometrium (innermost epithelial lining) of the uterus by forming finger-like projections called chorionic villi that make their way into the uterus, and spaces called lacunae that fill up with the mother's blood. |
|
|
Discuss the differentiation of the trophoblast:
|
The trophoblast proliferates and differentiates into 2 cell layers at approximately 6 days after fertilization for humans
1) Inner layer- Cytotrophoblast - a single celled, inner layer of the trophoblast. 2) Outer layer- Syncytiotrophoblast - the thick layer that lacks cell boundaries and grows into the endometrial stroma. It secretes hcg in order to maintain progesterone secretion and sustain a pregnancy. Intermediate trophoblast (IT); Location- implantation site, chorion, villi (dependent on subtype) - Anchor placenta (implanation site IT), unknown (chorionic & villus IT) |
|
|
Discuss the formation of lacunar networks:
|
Lacunae fill with maternal blood from ruptured endometrial capillaries and cellular debris from the uterine glands.
The fluid in the lacunae (Embryotroph) diffuses to the embryonic disc. Communication of the eroded uterine vessels with the lacunae represents the beginning of uteroplacental circulation. |
|
|
What is meant by the term "implantation bleeding" and is this the same as menses (menstrual fluid)?
|
Implantation bleeding - loss of blood from implantation site of a blastocyst, occurs a few days after the expected time of menstruation.
No, it is not menses; it is blood from the intervillous space of the developing placenta. Blood lose could be the results from the rupture of chorionic arteries, veins, or both. |
|
|
Can an ectopic pregnancy occur in a woman who has an intrauterine device?:
|
An intrauterine device does not physically block a sperm from entering the uterine tube and fertilizing an oocyte, if one is present, only making the endometrium hostile to implantation. A blastocyst could develop and implant in the uterine tube.
15% to 20% chance for ectopic pregnancy. |
|
|
What is the characteristic of 'LIGHT MEROMYOSIN' (LMM) filaments?
|
MAKE UP THE 'RODLIKE' BACKBONE OF THE 'MYOSIN' FILAMENTS
|
|
|
Can a blastocyst that implants in the abdomen develop into a full-term fetus?:
|
-Yes, however...Very uncommon. It is believed to result from ectopic implantation of a blastocyst that spontaneously aborts from the uterine tube and enters the peritoneal cavity. If the patient is free of of systoms, the pregnancy may be allowed to continue until the viability of the fetus is ensured (e.g., 32 weeks), at which time it would be delivered by cesarean section.
|
|
|
Can drugs and other agents cause congenital anomalies of the embryo if they are present in the mother's blood during the third week? If so, what organs would be most susceptible?:
|
Certain drugs can produce congenital anomalies, if administered during the third week after the last normal menstual period.
-Can produce severe skeletal and neural tube defects in the embryo, such as acrania and meroencephaly (partial absence of the brain). |
|
|
Describe the formation of the placenta:
|
Formed from a network of villi (trophoblast cells):
◦Primary Villus: Cytotrophoblast + a layer of syncytiotrophoblast grow into the lacunae. ◦Secondary Villus: Extraembryonic mesoderm grows into the primary villus. ◦Tertiary Villus: Extraembryonic mesoderm gives rise to blood vessels. Exchange of nutrients is now possible with mother. |
|
|
Describe the formation of the Three Germ Layers:
|
Form by migration of epiblast cells through the primitive streak:
◦First Migration: Epiblasts migrate toward the midline and fold under, as they displace the hypoblast layer. This forms the true endoderm. (comes from migration of 1st epiblast layer -- not from the hypoblast) ◦Second Migration: More epiblasts migrate to form mesoderm. ◦The epiblasts that remain on the dorsal surface form the ectoderm. |
|
|
Describe the process of gastrulation:
|
The cellular mass flattens and the three primary germ layers segregate.
By the process of gastrulation, the embryo differentiates into three types of tissue: - the ectoderm, producing the skin and nervous system; - the mesoderm, from which develop connective tissues, the circulatory system, muscles, and bones; and - the endoderm, which forms the digestive system, lungs, and urinary system. |
|
|
Describe the development of the notochord and induction of the neural plate:
|
Notochord Formation:
•Notochordal Process forms from mesoderm. •Neurenteric canal is a transient opening between the amniotic cavity and the yolk sac. •Notochordal plate reforms a tube now known as the notochord. Concurrent Ectodermal Changes: - Formation of the Neural Plate and Neural Crest Cells. •Notochord induces ectodermal formation of the neural plate. •As neural plate invaginates medially, forming the midline neural groove and laterally placed neural folds. •Neural Tube forms as the fusion of the neural folds. |
|
|
Describe the establishment of a primordial uteroplacental circulation:
|
maternal blood flows into the lacunae, oxygen and nutritive substances become available to the extraembryonic tissues ove the large surface of the syncytiotrophoblast.
Oxygenated blood passes into the lacunae from the spiral endometrial arteries in the enometrium; deoxygenated blood is removed from the lacunae through endometrial veins. |
|
|
What is the most common cause of spontaneous abortion during the first week of development?
|
Chromosomal abnormality.
|
|
|
When does the Primitive Streak take place?
|
Beginning of the 3rd Week
|
|
|
Describe the development of sacrococcygeal teratoms?
|
Remnants of the primitive streak may persist and give rise to a large tumor known as a sacrococcygeal teratoma.
-Usually surgically removed, and prognosis is good. |
|
|
During the 3rd week of development, Failure of the neural folds to fuse and form the neural tube results in what?
|
meroencephaly and spina bifida cystica.
|
|
|
Describe the formation of early embryonic blood vessels:
|
Formed during the 3rd week, called Vasculogenesis.
|
|
|
When does the fetus heart begin to beat?
|
Day 21 or 22.
|
|
|
Which organ system is fully functional in a fetus?
|
The Cardiovascular system is the first organ system to reach a functional state on day 21 or 22.
|
|
|
What is choriocarcinomas?
|
Malignant trophoblastic lesions.
|
|
|
Describe the folding of the embryo?
|
Describe the folding of the embryo?
-Folding results from rapid growth of the embryo, by folding the flat trilaminar embryonic dsc into a somewhat cylindar embryo. |
|
|
Describe a hydatiform mole and its association with choriocarcinoma?
|
-Hydatiform moles form when the embryo dies and the chorionic villi do not complete their development. Little or no embryonic tissue is present though the trophoblast developes well. They look like a bunch of grapes and turns into choriocarcinomas.
|
|
|
Describe the fate of the intraembryonic mesoderm:
|
Mesodermal Structures:
•Paraxial Mesoderm: Somites. •Intermediate Mesoderm: Urogenital system. •Lateral Plate Mesoderm: Primitive gut, posterior and lateral body wall. It differentiates into two layers: -◦Somatic Mesoderm: (Amniotic side) -◦Splanchnic Mesoderm: (Yolk side) |
|
|
Describe the development of the somites:
|
Somites establish the segmental nature of the body. They differentiate into three layers.
•Sclerotome: Forms the vertebral bone. This originates from paraxial mesoderm. •Dermamyotome, consisting of myotome (medial part) and dermatome (most lateral part) Early Somite Development: •Chorioamnionic Membrane forms, merging the chorion and amnion cavities. •Folding (flexion) of the embryo repositions the somites from the ventral-medial position to a dorsolateral position. |
|
|
Describe how the amniotic fluid is produced:
|
Weeks 1-11: Maternal tissue fluid diffuses across the amniochorionic membrane.
Weeks 11+: fetus contributes to the "AF" by expelling urine into the amniotic cavity. |
|
|
Describe how the amniotic fluid circulates:
|
An exchange of fluid w/fetal blood occurs thru the umbilical cord & at the site where the amnion adheres to the chorionic plate on the fetal surface of the placenta.
|
|
|
What is a Sacrococcygeal Teratoma?
|
A benign tumor left over from the primitive streak.
|
|
|
What is a Chordoma?
|
Slow growing malignant tumor which invades bone. Occurs at the base of the scull or the lumbrosacral region. Remnant of the notochord.
|
|
|
What is Gastroschisis?
|
Gut herniates through a poorly formed anterior abdominal wall. Causes heat loss from exposed bowel. Good prognosis after surgery.
Caused by a problem with lateral folding. |
|
|
What is Ectopic Cordis?
|
Heart lies outside the thoracic cavity due to lesion in sternum. Very poor prognosis (usually accompanied by other cardiac defects.
Caused by a problem with Lateral folding. |
|
|
What does the neural tube give rise to?
|
CNS
Somatic PNS Pre-ganglionic component of visceral motor portion of PNS (sym and para) |
|
|
What do neural crest cells give rise to?
|
Ganglion cells of PNS (all neurons of the PNS with soma in somantic sensory and autonomic ganglia)
- Sensory neurons of spinal nerves - Sympathetic and parasympathetic post-ganglionics Schwann Cells Meninges Suprarenal medulla |
|
|
What are the two kinds of spina bifida?
|
Spina bifida occulta:
No bulge, tuft of hair, no neurological deficencies. Spina bifida cystica -With meningocoele - bulge over defect that contains meninges and CSF, no neurological defects With meningomyelocoele - bulge over defect containing meninges, cord and spinal nerves With Myeloschisis - open cord, failure of caudal neuropore to close and neural tube did not form. |
|
|
What is the primary yolk sac/Exocoelomic cavity?
|
First site of blood formation, gives rise to primordial gut and germ cells.
|
|
|
What is Amniotic Band Syndrome?
|
Amniotic bands can amputate limbs (premature rupture of amnion)
|
|
|
What two parts make up the placenta?
|
Maternal - Decidua basalis (rough)
Fetal - Chorion frondosum (smooth) |
|
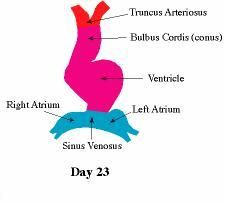
What are the fates of the following structures of the primitive heart?
Trancus Arteriosus Bulbus Cordis Ventricle Atrium Sinus Venosus space between Bulbus Cordis and Left Atrium |
Truncus Arteriosus - asc aorta, pulm trunk
Bulcus Cordis - aortic vestibule & conus arteriosus Ventricle - out free walls of both ventricles Atrium - auricles and pectinate muscle area of both atria Sinus Venosus - coronary sinus & sinus venarum Space - transverse sinus |
|
|
What is dextrocardia?
|
Heart folds in opposite direction giving a mirror image
|
|
|
What is probe patency?
|
Failure of anatomical closure resulting in functional closure only, allowing a "prove" to pass through the foramen. Generally asymptomatic
|
|
|
What are the three areas involved in Atrial Septal Defects and what problems are associated with them?
|
Problem: Persistent foramen causing a left to right shunt. All are correctable by surgery. Can result in common atrium.
Ostium Secondum defect - patent foramen secundum - failure of septum primum and secundum to meet and fuse (most common ASD) Endocardial Cushion defect - patent foramen primum Sinus Venosus defect - defect in upper atrium due to incomplete sunus venosus and/or incomplete development of septum secundum. |
|
|
Which septum is supposed to partition the truncus arteriosus?
|
Aorticopulmonary septum
|
|
|
Describe the transposition of the great vessels
|
Faulty migration of neural crest cells results in absence of spiral to the aorticopulmonary septum.
If complete transposition you have a R - L shunt (cyanotic) Cyanosis is less if ASD, VSD or PDA is present to allow L - R missing Deoxy blood from RV directly enters system circulation. |
|
|
Describe the Tetrology of Fallot
|
Failure of migration of neural crest cells where the aorticopulmonary septum forms symmetrically.
Must have: Pulmonary stenosis causing Right ventricular hypertrophy VSD Overriding aorta. Results in a cyanotic R - L shunt. |
|
|
Describe a Persistent Truncus Arteriosus
|
Failure of migration of neural crest cells
Part or all of truncus arteriosus does not develop Aorticopulmonary septum resulting in a common passageway part or all the way up. Always accompanied by VSD. Not a true R - L shut but systemic circulation gets blood from both ventricles and is cyanotic. |
|
|
Describe two prenatal cardiac shunts - foramen ovale and ductus arteriosus
|
Foramen Ovale - allows oxy blood from IVC entering RA - LA to systemic circulation
Ductus Arteriosus - deoxy blood from SVC enters RA, RV, Pulm Trunk - distal aorta arch via ductus arteriosus |
|
|
What is a Patent Ductus Arteriosus?
|
Persistence of duct beyond 1 month of due date
Premature infants usually have PDA Most common anomaly with maternal ruvella infection L - R Shunt (acyanotic) |
|
|
Summarize which shunts are R - L
|
Tetrology of Fallot
Transpotion of Great Vessels Persistent Truncus Arteriosus |
|
|
Summarize which shunts are L - R
|
ASD
VSD PDA |
|
|
What is a Tracheoesophageal fistula?
|
Faulty development of the traacheoesphogeal septum
Abnormal communication between trachea and esophagus May be associated with esophagus atresia Infants will cough and choke when swallowing fluid May cause pneumonia In utero - may result in polyhdramnios as the amniotic fluid can't go to gut for absorption do to esophageal atresia |
|
|
Lung development and fetal viability
|
Canalicular period (26 weeks) Type II aveolar cells may produce sufficient surfactant to respire w/o respirator
Terminal Sac Stage (26+) - fetus is viable |
|
|
Factors influencing normal development of the lungs
|
Amniotic fluid volume - Oligohydramnios = hypoplasia
Fetal breathing movements: stimulate lung development by causing aspiration of amniotic fluid (at birth still partially filled, which is quickly absorbed) Space in thorax for growth: infants with congenital disphragmatic hernia, lung is unable to develop normally as space is reduced |
|
|
Normal development of the diaphragm
|
From 4 embryonic components:
Pleuroperitoneal membranes invaded by myoblasts and contribute to muscular portion Septum Transversum remains membranous and becomes central tendon Lateral body wall contributes some muscle to the periphery of the diaphragm |
|
|
Normal development of pleural and pericardial cavities
|
• bronchial buds grow from laryngotracheal diverticulum
• buds grow into surrounding splanchnic mesoderm • plueropericardial folds grow in from lateral walls • folds enlarge to become pleuropericardial membranes • membranes separate heart from developing lungs • pleuropericardial membranes fuse posterior to heart, forming the pericardial sac, while lungs continue to grow around sac |
|
|
What are the possible defects in the development of the diaphragm?
|
Retrosternal/parasternal hernia
Congenital diaphragmatic hernia Eventration of the diaphragm |
|
|
What is a retrosternal/parasternal hernia?
|
Deficiency of pleuroperitoneal membrane
Hiatus between sternocostal parts Gut may be herniated into pericardial sac |
|
|
What is a congenital diaphragmatic hernia?
|
Failure of pleuroperitoneal membranes to fully develop or properly fuse with other elements of the diaphragm
Flattened abdomen Gut enters thorax through posterolateral defect in diaphragm |
|
|
What is Eventration of diaphragm?
|
Defective muscle development from body wall and only aponeurotic/membranous sheet is present
As diaphragm contracts, muscular part descends, non-muscular portion balloons into throwax pushed by abdominal viscera Relatively rare |
|
|
What are the fates of the aortic arches?
|
First - gives rise to maxillary artery (disappears)
Second - gives rise to hyoid and stapedial arteries (disappears) Third, Fourth, Sixth - major vessels Fifth - disappears |
|
|
What happens if the distal portion of the right fourth arch persists?
|
Double aortic arches
They enclose the esophagus so swallowing is difficult |
|
|
What happens if the right 4th arch disappears leaving part of the 7th?
|
The right 7th becomes the right subclavian. It follows the left around and eventually passes behind it and the trachea to reach its destination
|
|
|
What problems are possible during descent of the testis?
|
Hydrocoeles
Incomplete indirect inguinal hernia Indirect inguinal hernia Direct inguinal hernia Cryptorchid (undescended) Ectopic testis |
|
|
What problems are possible during development of the GI tract?
|
Congenital omphalocoele
Anomalies of Rotation - nonrotation - reversed rotation - subhepatic cecum - midgut volvulus Omphaloenteric duct (yolk sac) anomalies Problems with epithelia lining of gut - bowel stenosis - bowel atresia Hirsprung disease (megacolon) |
|
|
What problems are possible during development of the kidneys?
|
Renal agenesis
Discoid (pancake) kidney Problems with ascent of kidney - horshoe kidney (fuses, hits inf mesenteric artery on ascent) - pelvic kidney (fails to ascend) - Migration to opposite side with possible fushion - 3 ureters Lobulated kidney |

