![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
62 Cards in this Set
- Front
- Back
|
There are some main things to talk about including ACTH- we often use this as
|
derivatives other others. not usually giving it directly as therapy
|
|
|
for the corticosteroids- there are two different main ones
|
glucocorticoids- metabolic regulating
mineralocorticoids- Na K balances |
|
|
ACTH stimulates the synthesis and release of
does an acute and chronic mechanism |
adrenocortical hormones
acute: making cholesterol available chronic: raises txn CYP450's which is needed for some key steps in the adrenal cortex |
|
|
There are different zones in the adrenal cortex--
in the ___ zone in response to ___ and ___ there's increased secretion of a CYP450 for aldosterone |
outer zone angiotensin II and high K+ stimulates aldosterone
|
|
|
ACTH acts in the ___ zone to increase secretion of glucocorticoid ___
In the ___ zone it increases the androgen precursor ___ |
middle zone to secrete CYP450's for cortisol
inner zone for DHEA- so in females or prepuberty males with facial hair, could be a problem |
|
|
What is regulating ACTH?
|
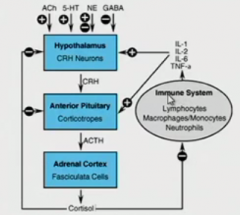
hypothalamus ->
pituitary which puts out corticotropes like ACTH -> adrenal cortex for cortisol -> feeds back to hypothalamus and ant. pituitary NT are acting on hypothalamus as well as cytokines |
|
|
endogenous and synthetic corticosteroids vary in terms of what effects (3)
|
anti-inflammatory potency
Na retaining potency duration of effect |
|
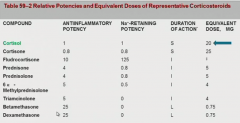
what are you reading?
|
these are comparing to cortisol. Some are antiinflammatory, some are Na retaining, some are both.
|
|
|
How do corticosteroids act mechanistically?
|
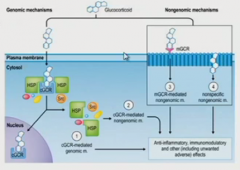
It goes right though membrane since it's hydrophobic and goes into nuclear receptors and it goes to the genes
nongenomic events can happen too |
|
|
what are the consequence of glucocorticoids activation?
|
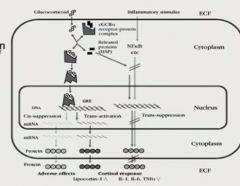
the genes being changed are metabolic
it's inhibiting activation of NFkB, so is anti-inflammatory what we want is to do the anti-inflammatory without any of the metabolic changes, so we want selective GR ligands that won't affect that pathway |
|
|
what are mineralocorticoids doing?
|
it goes to mineralocorticoid receptor and so aldosterone is upregulating epithelium Na channels
|
|
|
the different glucocorticoid receptors for corticosteroids and mineralocorticoid have ___ affinity for the different steroids
so how does that work? |
the same
cortisol would choose one just the same as the other and glucocorticoid receptors are everywhere but the mineralocorticoid receptor has restricted expression (kidney, colon, salivary, sweat) |
|
|
What other way are the corticosteroids regulated?
|
an isozyme 11BetaHSD2 will convert cortisol to an inactive form (though 11BetaHSD1 can go the other way- like in liver and fat)
|
|
|
Why is pear shape better than apple shape?
|
Belly fat has more 11BHSD1 turning cortisone into cortisol
|
|
|
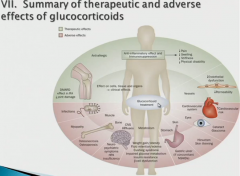
so the point of corticosteroids-- schematic of what they're doing
|
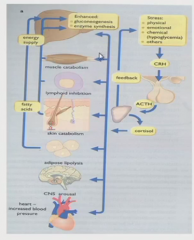
stress -> need to react
break down all sorts of stuff (muscle, lymphoid system, fat breakdown) for materials in liver for gluconeogenesis |
|
|
So breaking down the metabolic effects of corticosteroids:
in terms of glc |
in the liver.. ups the enzymes there getting that glc out
lowers glc uptake in muscle and adipose fat breakdown goes up net result- raises plasma glucose |
|
|
corticosteroids
how they affect electrolytes/water |
stimulates reabsorption of Na from tubular fluid
|
|
|
corticosteroids:
cardiovascular system |
if you have excessive mineralocorticoids (primary aldosteronism) changes in Na excretion and hypertension, can affect heart and cause cardiac fibrosis
glucocorticoids: induce hypertension |
|
|
corticosteroids: CNS
|
indirect changes from blood pressure, electrolytes, glc concentrations
also direct effects... if too much can push pt to psychosis but if low levels, lethargy issues |
|
|
corticosteroids: immune system and inflammatory cells
|
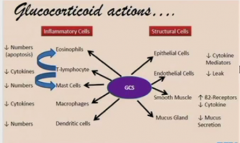
they inhibit leukocyte trafficking-- inhibits the trafficking receptors (so I'm guessing selectins?)
the ones that get into site, can't express proinflammatory cytokines other humoral factors the numbers go down from cells not getting there or not being able to mature |
|
|
the glucocorticoids act ___ on your immune cells
on macrophages/monocytes at what factors lymphocytes? |
NFkB to COX2 to arachidonic acid and its metabolites
cytokines like IL-1 IL-6 TNFalpha lymphocytes: IL1 2 3 6 TNFalpha, GM-CSF, interferon gamma |
|
|
toxicities from ___ of steroid therapy or continued use at supraphysiological doses is bad because
|
withdrawal
their HPA axis is not functioning, so you have to taper off or only put pt on for 2-4 weeks |
|
|
What complications arise when you're trying to get a pt off corticosteroid therapy/replacement?
|
disease flare-up, HPA axis not coming back on, and pts vary widely in how fast they can stop
|
|
|
What kinds of things have to be addressed if pt has continued use of supraphysiological doses? 7
|
hyperglycemia: controll with diet and/or insulin
immune suppression problems: thrush infection on tongue (opportunistic infection) or TB peptic ulcers: especially if on NSAIDS myopathy: muscles might be bad already like in lungs for COPD and now you're pulling from them behavioral changes-- insomnia, psychosis, all sorts of stuff cataracts- duration and dosage influences osteronecrosis: femoral head, starts with joint pain and stiffness |
|
|
How does osteoporosis tie in to adrenocortical steroids? (1 + 4)
|
already set up because autoimmune diseases more common in older women just like osteoporosis
the glucocorticoids are decreasing steroid hormones, Ca absorption, bone formation, and raising bone breakdown |
|
|
So how do you approach adrenocortical steroid use in osteroporosis potential problems? 5
|
do bone densitometry at beginning
recommend Ca and vitamin D supplements. bisphosphonate use, weight bearing exercises |
|
|
associated risk factors of glucocorticoids varies based on ___ given
|
dose
|
|
|
how do the adrenocortical steroids affect growth?
|
if given to children, growth deficiency noted during puberty and difference is sustained. a minor amount but definitively present.
|
|
|
When do we use glucocorticoids?
|
replacement therapy
acute inflammation neoplastic disorders (makes them apoptose) chronic inflammation |
|
|
use of glucocorticoids is largely ___
what do you look to see how the pt is doing? |
empirical
you just kind of guess how much a pt needs and use trial and error- look at blood pressure, mood, sleeping |
|
|
most of the time the goal of glucocorticoid treatment is as ___ agents except in the cases of-
|
pallative
replacement therapy or Rhem. Arth. |
|
|
What strategies do you use in glucocorticoid treatments to avoid the undesireable side effects?
|
use intermediate acting steroids
alternate treatment days pulse therapy- of high doses for a few days for really intense diseases like lupus |
|
|
To help with bone density issues for glucocorticoids the idea is that or with pain
|
you use lower doses or intermediate ones in the morning to try to mirror cortisol circadian rhythms
use modified release, so the inflammation in the morning isn't so bad |
|
|
over treatment with corticosteroids gets symptoms similar to ___ including
|
cushings
striae, belly fat, buffalo hump, moon face, thinning limbs |
|
|
if pts are on glucocorticoids for a long time you also have to consider adjusting the ____ of other things depending on
|
dosages
other drugs or if they have stress of another illness or surgery |
|
|
rheumatic disorders. often treated with
|
glucocorticoids as part of aggressive management-prednisone specifically
|
|
|
there are controversies about the high dosages of something like prednisone for rheumatic disorders
|
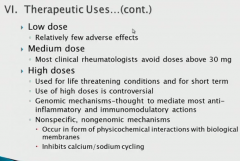
the high doses have more genomic side effects, but they seem to work- usually in life threatening situations
the non-specific issues have to do with Ca/Na cycling |
|
|
in the case of rheumatic treatments, they saw it wasn't just pallative but
|
actually helping as there is less damage and may be inhibiting progression of the disease
|
|
|
what are some advantages to using intermediate level glucocorticoids?
|
they're easier to taper and control
|
|
|
in non-inflammatory degenerative joint disorders- these are things like
you use what does that do? |
tendonitis, tennis elbow, etc
triamcinolone injections to joint slows down accumulation of inflammatory cells, so pain relief |
|
|
what is the artery problem that you can use with glucocorticoid?
what does pt experience how do you treat |
Giant cell arteritis or temporal arteritis where u get inflammation in med or large arteries (older white women). They get distended, occluded- rapidly relieved by corticoidsteroids Pt might have visual disturbances that bring them in. You don't want them to go blind, so you treat immediately with aggressive treatment
|
|
|
skin diseases and glucocorticoids
how to give side effects? different classes |
use topically though can do topically. Goes in better with some lotion. thinner skin use a bit less. side effects aren't too much of an issue.
they put them in classes, 1 being the most potent and a 7 being weak |
|
|
how do you measure the potency of topical corticosteroids?
|
look at blanching or suppression of edema
|
|
|
what's our favorite intralesional preparation for skin?
|
triamcinolone- has a prolonged duration of action
|
|
|
for systemic cases need for dermatological illnesses like ____ you would use morning dosing with ___
|
allergic contact dermatitis (poison ivy)
prednisone |
|
|
bowels and glucocorticoids
which diseases? |
Iinflammatory bowel diseases
ulcerative colitis and crohn's disease you use these at the moderate to severe IBD levels. Give them some prednisone until they go into remission |
|
|
there are three classes of pts generally speaking when it comes to glucocorticoids
|
steroid-responsive- you treat them, they get better, you stop, they go home
steroid-dependent- respond but if you stop treating, their illness returns steroid-unresponsive- do whatever you want, pts won't respond |
|
|
what other way could you treat IBD?
|
do a hydrocortisone enema to directly apply
buesonide: good for intermediate level IBD. It's enteric coated with 11% bioavailability- it's going to treat bowel, but liver will clear most of the rest. |
|
|
using glucocorticoids for asthma
what's the problem how do you treat |
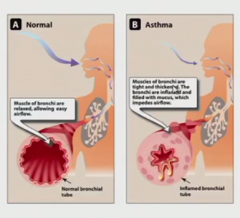
the mucous builds up, the smooth muscles contract, and path is small
gc. they're the best ones. Use budesonide to inhale. low bioavailability and directly delivered- so great. |
|
|
bleh
|
|
|
Sometimes we want to inhibit adrenocortical steroids and their actions.
what are two drugs we can use to inhibit the biosynthesis of gc? |
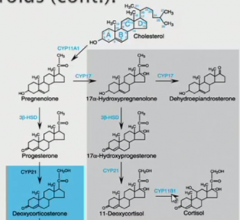
ketoconazole- normally an antifungal, but dose higher to lose selectivity and inhibit CYP17. Also for Cushing's
metyrapone- inhibits CYP11B. Good measure of HPA axis |
|
|
what's the mineralocorticoid drug that is a mr antagonist?
|
it's a replacement therapy for aldosterone
|
|
|
what are some drugs being developed?
|
selective glucocorticoid receptor agonists- but they've been working on this for a while
nitro-steroids where you combo NO and glucocorticoid since both anti-inflammatory for RA and IBD longer lasting liposomal gc |
|
|
summary drug list
budesonide potency? used to treat? how? anti-inflammatory/Na retain |
intermediate
asthma and IBD local administration low bioavailability |
|
|
summary drug list
dexamethasone potency? anti inflam/Na retain what does it treat? |
very potent
all anti inflam/no na retain brain edema or transplant- something crazy |
|
|
summary drug list
cortisol anti inflam/Na retain potency? duration? |
1:1 ratio
intermediate short lasting |
|
|
so the intermediate GC agonist drugs are
|
budesonide
prednisone triamcinolone |
|
|
summary drug list
prednisone will treat? dosage size for what goal? anti inflam/Na retain |
RA
low/med doses for maintenance therapy or pulse therapy intermed anti inflam/very low Na retain |
|
|
summary drug list
triamcinolone how did we administer? anti inflam/Na retain |
injected directly into joint
intermed anti-inflam/ no Na retain |
|
|
summary drug list
metyrapone treatment mechanism? |
inhibits CYP450's making cortisol
used to treat high cortisol |
|
|
summary drug list
ketoconazole treatment mechanism? |
inhibits CYP450's making cortisol
used to treat high cortisol |
|
|
summary drug list
aldosterone mechanism? what drug do you use to replace? anti inflam/Na retain |
mineralocorticoid receptor agonist
fludrocortisone anti inflam/ridiculous high Na retaining |

